Participation and Outcomes among Disabled and Non-Disabled People in the Diabetes Pay-for-Performance Program
Abstract
1. Introduction
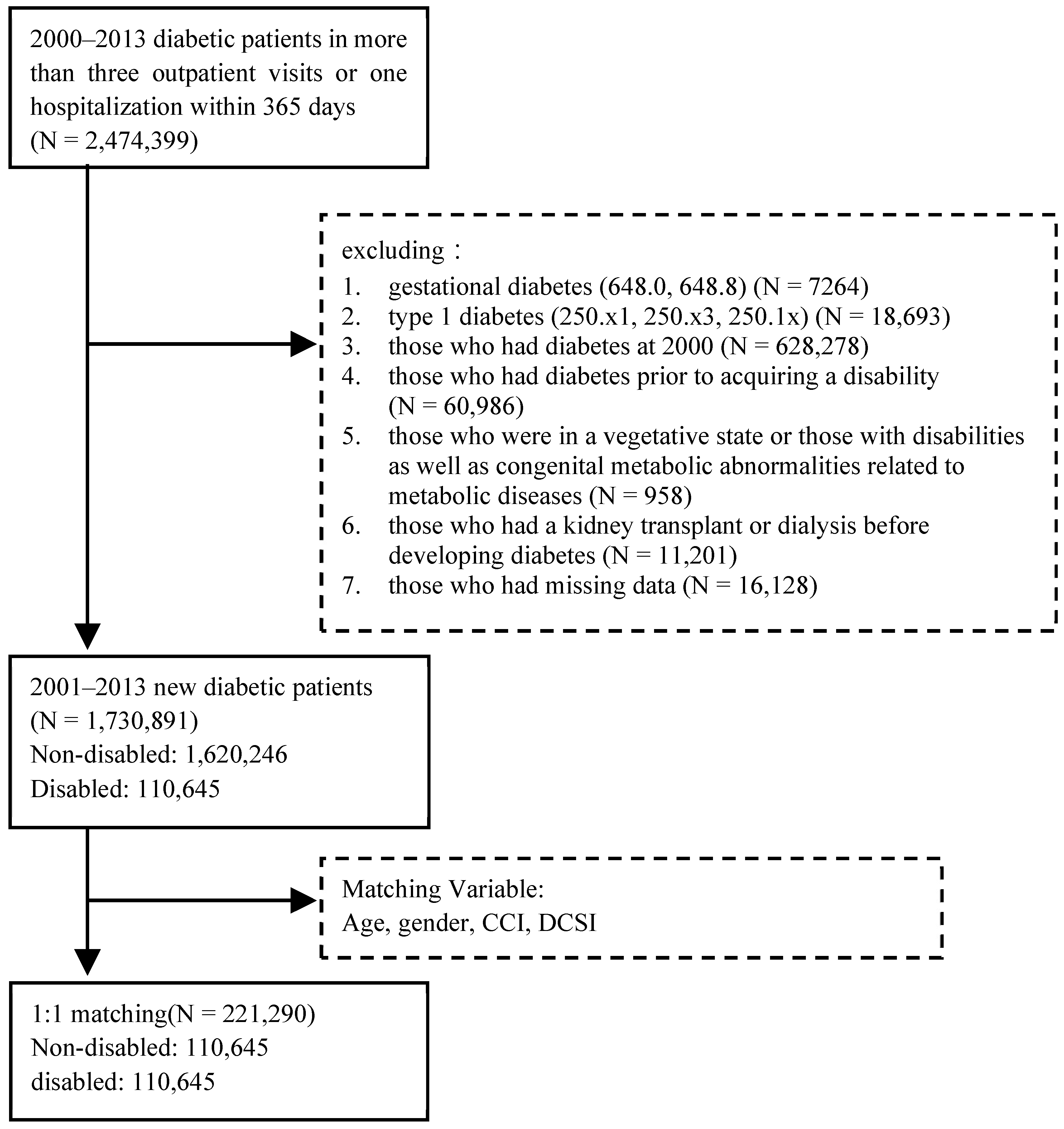
2. Materials and Methods
2.1. Data Sources and Participants
2.2. Description of Variables
2.3. Statistical Analysis
3. Results
3.1. Results of Matching between Disabled and Non-Disabled Diabetic Patients
3.2. Comparison of Enrollment in the P4P Program among Diabetic Patients with and without Disabilities
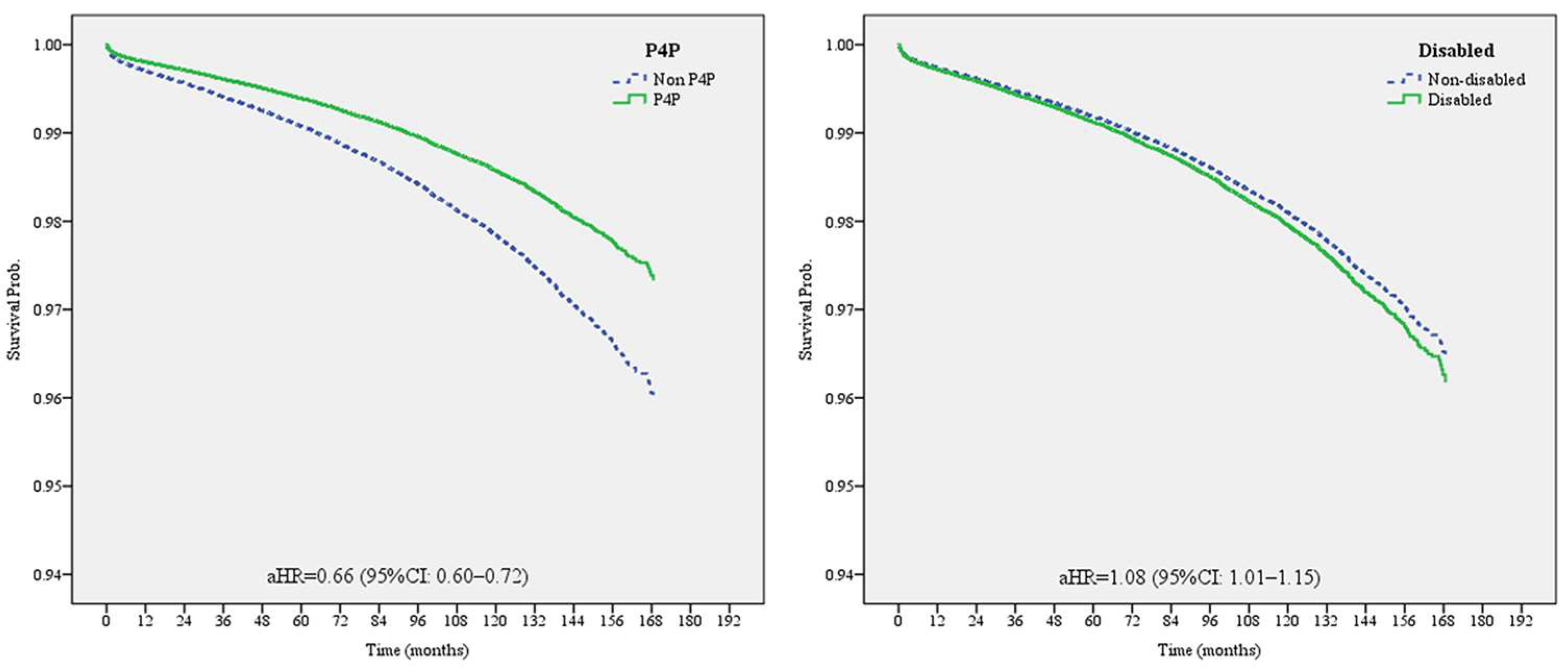
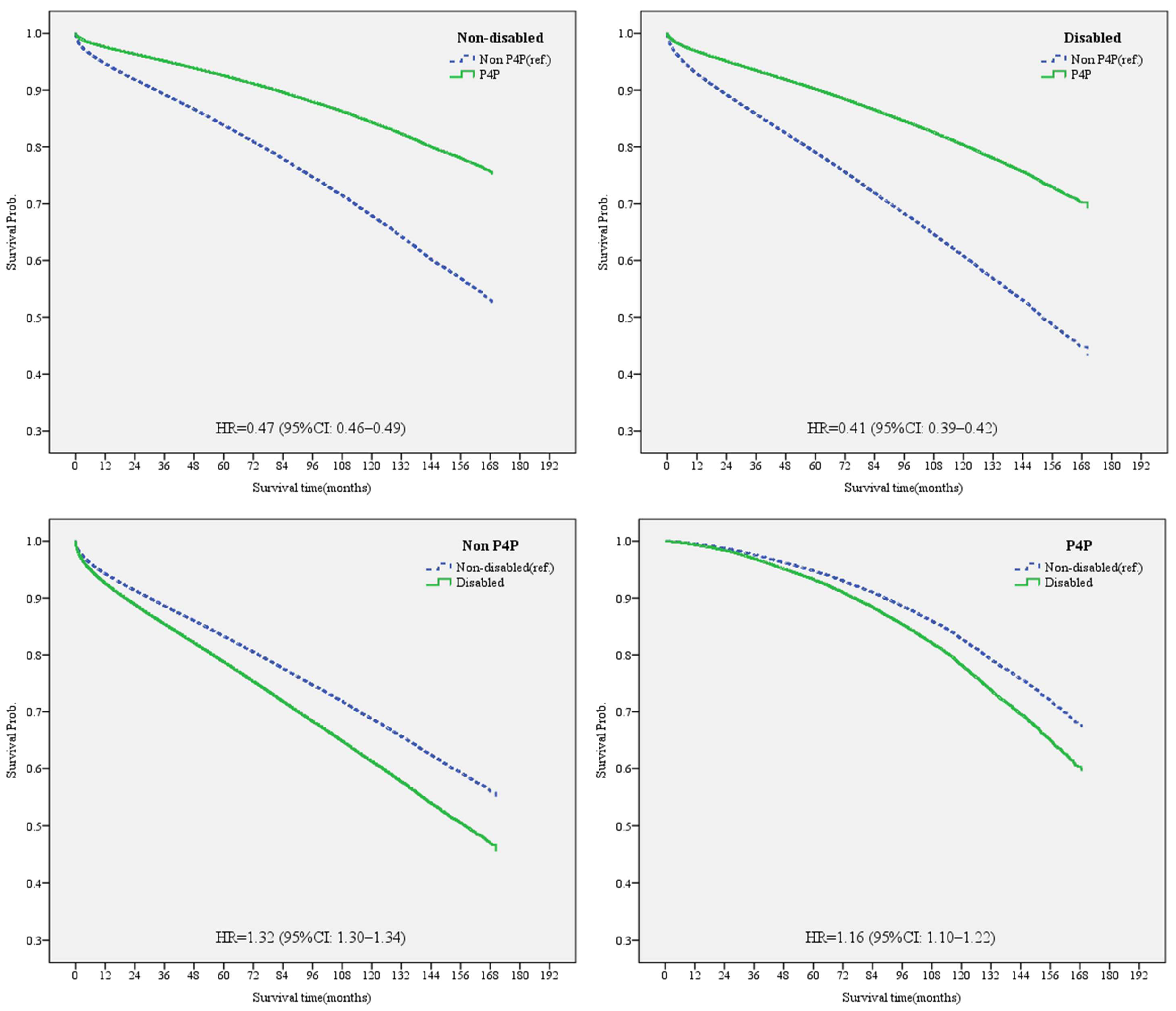
3.3. Effects of Enrollment in the DM P4P Program on the Risk of Dialysis in Disabled and Non-Disabled Diabetic Patients
3.4. Effects of the DM P4P Program on the Mortality in Disabled and Non-Disabled Diabetic Patients
4. Discussion
4.1. Disabled People Had a Lower Rate of Enrollment in the P4P Program than Non-Disabled People
4.2. The Similar Effects of the P4P Program on Reducing the Risk of Dialysis among DM Patients with Disabilities and Those without Disabilities
4.3. P4P Program Enrollment Reduced the Risk of Death More for Disabled Individuals than for Non-Disabled
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Hornick, T.; Aron, D.C. Preventing and managing diabetic complications in elderly patients. Clevel. Clin. J. Med. 2008, 75, 153. [Google Scholar] [CrossRef] [PubMed]
- United States Renal Data System. 2020 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2020.
- Dyck, R.F.; Jiang, Y.; Osgood, N.D. The long-term risks of end stage renal disease and mortality among First Nations and non-First Nations people with youth-onset diabetes. Can. J. Diabetes 2014, 38, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Lok, C.E.; Oliver, M.J.; Rothwell, D.M.; Hux, J.E. The growing volume of diabetes-related dialysis: A population based study. Nephrol. Dial. Transplant. 2004, 19, 3098–3103. [Google Scholar] [CrossRef] [PubMed]
- Graciani, A.; Banegas, J.R.; López-García, E.; Rodríguez-Artalejo, F. Prevalence of disability and associated social and health-related factors among the elderly in Spain: A population-based study. Maturitas 2004, 48, 381–392. [Google Scholar] [CrossRef]
- Parish, S.L.; Huh, J. Health care for women with disabilities: Population-based evidence of disparities. Health Soc. Work 2006, 31, 7–15. [Google Scholar] [CrossRef][Green Version]
- Wisdom, J.P.; McGee, M.G.; Horner-Johnson, W.; Michael, Y.L.; Adams, E.; Berlin, M. Health disparities between women with and without disabilities: A review of the research. Soc. Work Public Health 2010, 25, 368–386. [Google Scholar] [CrossRef]
- Executive Yuan, R.O.C. Important Gender Statistics Database—Actual Coverage Rate of National Health Insurance. Available online: https://www.gender.ey.gov.tw/gecdb/Stat_Statistics_Query.aspx?sn=OU8Vo8ydhvbx1qKbUarVHw%3d%3d&statsn=u4ceyDJ9iGzBYUGlJC0z7w%3d%3d (accessed on 26 July 2023).
- Chang, R.E.; Lin, S.P.; Aron, D.C. A pay-for-performance program in Taiwan improved care for some diabetes patients, but doctors may have excluded sicker ones. Health Aff. 2012, 31, 93–102. [Google Scholar] [CrossRef]
- Kung, F.P.; Tsai, C.F.; Lu, C.L.; Huang, L.C.; Lu, C.H. Diabetes pay-for-performance program can reduce all-cause mortality in patients with newly diagnosed type 2 diabetes mellitus. Medicine 2020, 99, e19139. [Google Scholar] [CrossRef]
- Taiwan National Health Insurance Administration. 2019–2020 National Health Insurance Annual Report; Taiwan National Health Insurance Administration: Taichung, Taiwan, 2019.
- Adler, R.; Vasiliadis, A.; Bickell, N. The relationship between continuity and patient satisfaction: A systematic review. Fam. Pract. 2010, 27, 171–178. [Google Scholar] [CrossRef]
- Cheng, S.H.; Lee, T.T.; Chen, C.C. A longitudinal examination of a pay-for-performance program for diabetes care: Evidence from a natural experiment. Med. Care 2012, 50, 109–116. [Google Scholar] [CrossRef]
- Villagra, V.G.; Ahmed, T. Effectiveness of a disease management program for patients with diabetes. Health Aff. 2004, 23, 255–266. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Campbell, S.; Reeves, D.; Kontopantelis, E.; Middleton, E.; Sibbald, B.; Roland, M. Quality of primary care in England with the introduction of pay for performance. New Engl. J. Med. 2007, 357, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.-S.; Tsai, W.-C.; Lin, C.-L.; Chen, L.; Lang, H.-C.; Hsieh, H.-M.; Shin, S.-J.; Chen, T.; Huang, C.-T.; Hsu, C.-C. Trend and factors associated with healthcare use and costs in type 2 diabetes mellitus: A decade experience of a universal health insurance program. Med. Care 2015, 53, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-C.; Cheng, S.-H. Does pay-for-performance benefit patients with multiple chronic conditions? Evidence from a universal coverage health care system. Health Policy Plan. 2016, 31, 83–90. [Google Scholar] [CrossRef]
- Pan, C.C.; Kung, P.T.; Chiu, L.T.; Liao, Y.P.; Tsai, W.C. Patients with diabetes in pay-for-performance programs have better physician continuity of care and survival. Am. J. Manag. Care 2017, 23, e57–e66. [Google Scholar] [PubMed]
- Chiu, T.; Sun, H.-Y. Definition and Categorization of Disability in Taiwan: A Historical Review. Dev. Soc. 2017, 46, 179–194. [Google Scholar]
- Taiwan Ministry of Health and Welfare. The Disabled Population. Available online: https://dep.mohw.gov.tw/dos/cp-5224-62359-113.html (accessed on 26 June 2023).
- Havercamp, S.M.; Scandlin, D.; Roth, M. Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in North Carolina. Public Health Rep. 2004, 119, 418–426. [Google Scholar] [CrossRef]
- Shireman, T.I.; Reichard, A.; Nazir, N.; Backes, J.M.; Greiner, K.A. Quality of diabetes care for adults with developmental disabilities. Disabil. Health J. 2010, 3, 179–185. [Google Scholar] [CrossRef]
- Taggart, L.; Coates, V.; Truesdale-Kennedy, M. Management and quality indicators of diabetes mellitus in people with intellectual disabilities. J. Intellect. Disabil. Res. 2013, 57, 1152–1163. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention; National Center on Birth Defects and Developmental Disabilities; Division of Human Development and Disability. Disability and Health Data System (DHDS); CDC: Atlanta, GA, USA, 2019.
- McGuire, B.; Daly, P.; Smyth, F. Lifestyle and health behaviours of adults with an intellectual disability. J. Intellect. Disabil. Res. 2007, 51, 497–510. [Google Scholar] [CrossRef]
- Temple, V.A.; Walkley, J.W. Physical activity of adults with intellectual disability. J. Intellect. Dev. Disabil. 2003, 28, 342–353. [Google Scholar] [CrossRef]
- Ewing, G.; McDermott, S.; Thomas-Koger, M.; Whitner, W.; Pierce, K. Evaluation of a cardiovascular health program for participants with mental retardation and normal learners. Health Educ. Behav. 2004, 31, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Mookhoek, E.J.; de Vries, W.A.; Hovens, J.E.; Brouwers, J.R.; Loonen, A.J. Risk factors for overweight and diabetes mellitus in residential psychiatric patients. Obes. Facts 2011, 4, 341–345. [Google Scholar] [CrossRef]
- Cohen, D. Atypical antipsychotics and new onset diabetes mellitus. Pharmacopsychiatry 2004, 37, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sugai, T.; Suzuki, Y.; Yamazaki, M.; Shimoda, K.; Mori, T.; Ozeki, Y.; Matsuda, H.; Sugawara, N.; Yasui-Furukori, N.; Minami, Y. High prevalence of obesity, hypertension, hyperlipidemia, and diabetes mellitus in Japanese outpatients with schizophrenia: A nationwide survey. PLoS ONE 2016, 11, e0166429. [Google Scholar] [CrossRef] [PubMed]
- Austin, D. Disabilities are risk factors for late stage or poor prognosis cancers. In Changing Concepts of Health & Disability: State of the Science Conference & Policy Forum; Oregon Health and Science University: Portland, OR, USA, 2003; pp. 52–55. [Google Scholar]
- Caban, M.E.; Nosek, M.A.; Graves, D.; Esteva, F.J.; McNeese, M. Breast carcinoma treatment received by women with disabilities compared with women without disabilities. Cancer 2002, 94, 1391–1396. [Google Scholar] [CrossRef]
- Diab, M.E.; Johnston, M.V. Relationships between level of disability and receipt of preventive health services. Arch. Phys. Med. Rehabil. 2004, 85, 749–757. [Google Scholar] [CrossRef]
- Chen, T.T.; Chung, K.P.; Lin, I.C.; Lai, M.S. The unintended consequence of diabetes mellitus pay-for-performance (P4P) program in Taiwan: Are patients with more comorbidities or more severe conditions likely to be excluded from the P4P program? Health Serv. Res. 2011, 46, 47–60. [Google Scholar] [CrossRef]
- Lee, I.-T.; Hsu, C.-C.; Sheu, W.H.-H.; Su, S.-L.; Wu, Y.-L.; Lin, S.-Y. Pay-for-performance for shared care of diabetes in Taiwan. J. Formos. Med. Assoc. 2019, 118, S122–S129. [Google Scholar] [CrossRef]
- Tan, E.C.-H.; Pwu, R.-F.; Chen, D.-R.; Yang, M.-C. Is a diabetes pay-for-performance program cost-effective under the National Health Insurance in Taiwan? Qual. Life Res. 2014, 23, 687–696. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Tu, S.-T.; Sheu, W.H.-H. 2019 diabetes atlas: Achievements and challenges in diabetes care in Taiwan. J. Formos. Med. Assoc. 2019, 118, S130–S134. [Google Scholar] [CrossRef] [PubMed]
- Sheen, Y.-J.; Kung, P.-T.; Sheu, W.H.-H.; Kuo, W.-Y.; Tsai, W.-C. Impact of Liver Cirrhosis on Incidence of Dialysis Among Patients with Type 2 Diabetes. Diabetes Ther. 2020, 11, 2611–2628. [Google Scholar] [CrossRef] [PubMed]
- Tsai, W.-C.; Huang, K.-H.; Chen, P.-C.; Chang, Y.-C.; Chen, M.S.; Lee, C.B. Effects of individual and neighborhood social risks on diabetes pay-for-performance program under a single-payer health system. Soc. Sci. Med. 2023, 326, 115930. [Google Scholar] [CrossRef] [PubMed]
- Parsons, L. Performing a 1: N Case-Control Match on Propensity Score SAS. In Proceedings of the Conference Proceedings: SAS Users Group International, Montreal, QC, Canada, 9–12 May 2004; p. 165-29. [Google Scholar]
- Deyo, R.A.; Cherkin, D.C.; Ciol, M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef]
- Young, B.A.; Lin, E.; Von Korff, M.; Simon, G.; Ciechanowski, P.; Ludman, E.J.; Everson-Stewart, S.; Kinder, L.; Oliver, M.; Boyko, E.J. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am. J. Manag. Care 2008, 14, 15. [Google Scholar]
- Liu, C.Y.; Hung, Y.T.; Chuang, Y.L.; Chen, Y.J.; Weng, W.S.; Liu, J.S.; Liang, K. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar] [CrossRef]
- Cho, K.H.; Nam, C.M.; Choi, Y.; Choi, J.-W.; Lee, S.-H.; Park, E.-C. Impact of continuity of care on preventable hospitalization of patients with type 2 diabetes: A nationwide Korean cohort study, 2002–2010. Int. J. Qual. Health Care 2016, 28, 478–485. [Google Scholar] [CrossRef][Green Version]
- Chen, P.-C.; Tsai, C.-Y.; Woung, L.-C.; Lee, Y.-C. Socioeconomic disparities in preventable hospitalization among adults with diabetes in Taiwan: A multilevel modelling approach. Int. J. Equity Health 2015, 14, 31. [Google Scholar] [CrossRef]
- Raymaker, D.M.; McDonald, K.E.; Ashkenazy, E.; Gerrity, M.; Baggs, A.M.; Kripke, C.; Hourston, S.; Nicolaidis, C. Barriers to healthcare: Instrument development and comparison between autistic adults and adults with and without other disabilities. Autism 2017, 21, 972–984. [Google Scholar] [CrossRef]
- Saqr, Y.; Braun, E.; Porter, K.; Barnette, D.; Hanks, C. Addressing medical needs of adolescents and adults with autism spectrum disorders in a primary care setting. Autism 2018, 22, 51–61. [Google Scholar] [CrossRef]
- Veltman, A.; Stewart, D.E.; Tardif, G.S.; Branigan, M. Perceptions of primary healthcare services among people with physical disabilities. Part 1: Access issues. Medscape Gen. Med. 2001, 3, 18. [Google Scholar]
- Champaneri, S.; Wand, G.S.; Malhotra, S.S.; Casagrande, S.S.; Golden, S.H. Biological basis of depression in adults with diabetes. Curr. Diabetes Rep. 2010, 10, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Kan, C.; Silva, N.; Golden, S.H.; Rajala, U.; Timonen, M.; Stahl, D.; Ismail, K. A systematic review and meta-analysis of the association between depression and insulin resistance. Diabetes Care 2013, 36, 480–489. [Google Scholar] [CrossRef]
- Pan, A.; Keum, N.; Okereke, O.I.; Sun, Q.; Kivimaki, M.; Rubin, R.R.; Hu, F.B. Bidirectional association between depression and metabolic syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care 2012, 35, 1171–1180. [Google Scholar] [CrossRef]
- Chen, Y.C.; Lee, C.T.-C.; Lin, B.J.; Chang, Y.-Y.; Shi, H.Y. Impact of pay-for-performance on mortality in diabetes patients in Taiwan: A population-based study. Medicine 2016, 95, e4197. [Google Scholar] [CrossRef]
- Lee, T.T.; Cheng, S.H.; Chen, C.C.; Lai, M.S. A pay-for-performance program for diabetes care in Taiwan: A preliminary assessment. Am. J. Manag. Care 2010, 16, 65–69. [Google Scholar] [PubMed]
- Wu, Y.F.; Chen, M.Y.; Chen, T.H.; Wang, P.C.; Peng, Y.S.; Lin, M.S. The effect of pay-for-performance program on infection events and mortality rate in diabetic patients: A nationwide population-based cohort study. BMC Health Serv. Res. 2021, 21, 78. [Google Scholar] [CrossRef]
- Gillani, S.W.; Sulaiman, S.A.S.; Abdul, M.I.M.; Saad, S.Y. A qualitative study to explore the perception and behavior of patients towards diabetes management with physical disability. Diabetol. Metab. Syndr. 2017, 9, 58. [Google Scholar] [CrossRef]
| Before Matching | SMD * | After 1:1 Matching | SMD | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total (N = 1,730,891) | Non-Disabled (n = 1,620,246) | Disabled (n = 110,645) | Total (N = 221,290) | Non-Disabled (n = 110,645) | Disabled (n = 110,645) | ||||||||||
| N | % | n | % | n | % | N | % | n | % | n | % | ||||
| Sex | |||||||||||||||
| Female | 803,979 | 46.45 | 755,536 | 46.63 | 48,443 | 43.78 | −0.057 | 96,886 | 43.78 | 48,443 | 43.78 | 48,443 | 43.78 | 0.000 | |
| Male | 926,912 | 53.55 | 864,710 | 53.37 | 62,202 | 56.22 | 0.057 | 124,404 | 56.22 | 62,202 | 56.22 | 62,202 | 56.22 | 0.000 | |
| Age (years) | |||||||||||||||
| <45 | 289,012 | 16.70 | 275,097 | 16.98 | 13,915 | 12.58 | −0.124 | 27,826 | 12.57 | 13,911 | 12.57 | 13,915 | 12.58 | 0.000 | |
| 45~54 | 448,953 | 25.94 | 427,542 | 26.39 | 21,411 | 19.35 | −0.168 | 42,825 | 19.35 | 21,414 | 19.35 | 21,411 | 19.35 | 0.000 | |
| 55~64 | 438,980 | 25.36 | 416,713 | 25.72 | 22,267 | 20.12 | −0.134 | 44,534 | 20.12 | 22,267 | 20.12 | 22,267 | 20.12 | 0.000 | |
| 65~74 | 325,298 | 18.79 | 301,210 | 18.59 | 24,088 | 21.77 | 0.079 | 48,176 | 21.77 | 24,088 | 21.77 | 24,088 | 21.77 | 0.000 | |
| ≥75 | 228,648 | 13.21 | 199,684 | 12.32 | 28,964 | 26.18 | 0.357 | 57,929 | 26.18 | 28,965 | 26.18 | 28,964 | 26.18 | 0.000 | |
| Average age (SD) | 58.26 (14.15) | 57.92 (13.98) | 63.27 (15.57) | 0.897 | 62.24 (15.29) | 62.10 (15.09) | 63.27 (15.57) | 0.102 | |||||||
| CCI | |||||||||||||||
| 0 | 911,154 | 52.64 | 872,021 | 53.82 | 39,133 | 35.37 | −0.378 | 78,266 | 35.37 | 39,133 | 35.37 | 39,133 | 35.37 | 0.000 | |
| 1 | 428,741 | 24.77 | 401,390 | 24.77 | 27,351 | 24.72 | −0.001 | 54,702 | 24.72 | 27,351 | 24.72 | 27,351 | 24.72 | 0.000 | |
| 2 | 197,119 | 11.39 | 179,242 | 11.06 | 17,877 | 16.16 | 0.149 | 35,754 | 16.16 | 17,877 | 16.16 | 17,877 | 16.16 | 0.000 | |
| ≥3 | 193,877 | 11.20 | 167,593 | 10.34 | 26,284 | 23.76 | 0.363 | 52,568 | 23.76 | 26,284 | 23.76 | 26,284 | 23.76 | 0.000 | |
| DCSI | |||||||||||||||
| 0 | 1,390,678 | 80.34 | 1,316,387 | 81.25 | 74,291 | 67.14 | −0.327 | 148,583 | 67.14 | 74,292 | 67.14 | 74,291 | 67.14 | 0.000 | |
| 1 | 170,318 | 9.84 | 159,034 | 9.82 | 11,284 | 10.20 | 0.013 | 22,568 | 10.20 | 11,284 | 10.20 | 11,284 | 10.20 | 0.000 | |
| 2 | 132,930 | 7.68 | 114,382 | 7.06 | 18,548 | 16.76 | 0.303 | 37,096 | 16.76 | 18,548 | 16.76 | 18,548 | 16.76 | 0.000 | |
| ≥3 | 36,965 | 2.14 | 30,443 | 1.88 | 6522 | 5.89 | 0.209 | 13,043 | 5.89 | 6521 | 5.89 | 6522 | 5.89 | 0.000 | |
| Total | Non-Disabled | Disabled | Non-Disabled | Disabled | P4P Program Participation | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Total | Non P4P | P4P | Non P4P | P4P | |||||||||||||
| N | % | N | % | n | % | n | % | n | % | n | % | aOR | 95% CI | p Value | ||||
| Total | 221,290 | 110,645 | 100.00 | 110,645 | 100.00 | 84,954 | 76.78 | 25,691 | 23.22 | 88,391 | 79.89 | 22,254 | 20.11 | |||||
| Non-disabled | 110,645 | 110,645 | 100.00 | - | - | - | - | - | - | - | - | - | - | 1.00 | ||||
| Disabled | 110,645 | - | - | 110,645 | 100.00 | - | - | - | - | - | - | - | - | 0.89 | 0.87 | 0.91 | <0.001 | |
| P4P | ||||||||||||||||||
| Non-P4P | 173,345 | 84,954 | 76.78 | 88,391 | 79.89 | 84,954 | 76.78 | 25,691 | 23.22 | - | - | - | - | |||||
| P4P | 47,945 | 25,691 | 23.22 | 22,254 | 20.11 | - | - | - | - | 88,391 | 79.89 | 22,254 | 20.11 | |||||
| Sex | ||||||||||||||||||
| Female | 96,886 | 48,443 | 43.78 | 48,443 | 43.78 | 37,349 | 77.10 | 11,094 | 22.90 | 38,866 | 80.23 | 9577 | 19.77 | 1.00 | ||||
| Male | 124,404 | 62,202 | 56.22 | 62,202 | 56.22 | 47,605 | 76.53 | 14,597 | 23.47 | 49,525 | 79.62 | 12,677 | 20.38 | 1.07 | 1.05 | 1.1 | <0.001 | |
| Age (years) | ||||||||||||||||||
| <45 | 27,826 | 13,911 | 12.57 | 13,915 | 12.58 | 9528 | 68.49 | 4383 | 31.51 | 9795 | 70.39 | 4120 | 29.61 | 1.00 | ||||
| 45~54 | 42,825 | 21,414 | 19.35 | 21,411 | 19.35 | 14,913 | 69.64 | 6501 | 30.36 | 15,205 | 71.01 | 6206 | 28.99 | 0.92 | 0.89 | 0.95 | <0.001 | |
| 55~64 | 44,534 | 22,267 | 20.12 | 22,267 | 20.12 | 15,989 | 71.81 | 6278 | 28.19 | 16,657 | 74.81 | 5610 | 25.19 | 0.81 | 0.78 | 0.84 | <0.001 | |
| 65~74 | 48,176 | 24,088 | 21.77 | 24,088 | 21.77 | 18,652 | 77.43 | 5436 | 22.57 | 19,779 | 82.11 | 4309 | 17.89 | 0.74 | 0.71 | 0.77 | <0.001 | |
| ≥75 | 57,929 | 28,965 | 26.18 | 28,964 | 26.18 | 25,872 | 89.32 | 3093 | 10.68 | 26,955 | 93.06 | 2009 | 6.94 | 0.43 | 0.41 | 0.46 | <0.001 | |
| Average age (SD) | 63.11 (15.3) | 62.95 (15.09) | 63.27 (15.57) | 64.44 (15.25) | 58.03 (13.43) | 64.92 (15.65) | 56.71 (13.38) | |||||||||||
| Monthly salary (TWD) | ||||||||||||||||||
| ≤17,280 | 15,874 | 5307 | 4.8 | 10,567 | 9.55 | 4109 | 77.43 | 1198 | 22.57 | 8486 | 80.31 | 2081 | 19.69 | 1.00 | ||||
| 17,281~28,800 | 149,309 | 72,199 | 65.25 | 77,110 | 69.69 | 56,284 | 77.96 | 15,915 | 22.04 | 62,041 | 80.46 | 15,069 | 19.54 | 1.12 | 1.08 | 1.17 | <0.001 | |
| 28,801~45,800 | 35,743 | 20,432 | 18.47 | 15,311 | 13.84 | 14,844 | 72.65 | 5588 | 27.35 | 11,557 | 75.48 | 3754 | 24.52 | 1.21 | 1.15 | 1.27 | <0.001 | |
| 45,801~57,800 | 6787 | 4152 | 3.75 | 2635 | 2.38 | 3099 | 74.64 | 1053 | 25.36 | 2135 | 81.02 | 500 | 18.98 | 1.12 | 1.04 | 1.2 | 0.004 | |
| ≥57,801 | 13,442 | 8504 | 7.69 | 4938 | 4.46 | 6581 | 77.39 | 1923 | 22.61 | 4107 | 83.17 | 831 | 16.83 | 1.02 | 0.96 | 1.08 | 0.605 | |
| Missing | 135 | 51 | 0.05 | 84 | 0.08 | |||||||||||||
| Urbanization of residence area | ||||||||||||||||||
| Level 1 | 51,731 | 30,061 | 27.17 | 21,670 | 19.59 | 23,437 | 77.96 | 6624 | 22.04 | 17,690 | 81.63 | 3980 | 18.37 | 1.00 | ||||
| Level 2 | 62,011 | 32,674 | 29.53 | 29,337 | 26.51 | 24,822 | 75.97 | 7852 | 24.03 | 22,902 | 78.07 | 6435 | 21.93 | 1.19 | 1.15 | 1.22 | <0.001 | |
| Level 3 | 34,346 | 17,565 | 15.88 | 16,781 | 15.17 | 13,482 | 76.75 | 4083 | 23.25 | 13,367 | 79.66 | 3414 | 20.34 | 1.17 | 1.13 | 1.21 | <0.001 | |
| Level 4 | 38,983 | 17,010 | 15.37 | 21,973 | 19.86 | 12,788 | 75.18 | 4222 | 24.82 | 17,501 | 79.65 | 4472 | 20.35 | 1.36 | 1.31 | 1.41 | <0.001 | |
| Level 5 | 7981 | 3251 | 2.94 | 4730 | 4.27 | 2613 | 80.38 | 638 | 19.62 | 3887 | 82.18 | 843 | 17.82 | 1.14 | 1.07 | 1.22 | <0.001 | |
| Level 6 | 14,344 | 5603 | 5.06 | 8741 | 7.90 | 4390 | 78.35 | 1213 | 21.65 | 6950 | 79.51 | 1791 | 20.49 | 1.28 | 1.22 | 1.35 | <0.001 | |
| Level 7 | 11,894 | 4481 | 4.05 | 7413 | 6.700 | 3422 | 76.37 | 1059 | 23.63 | 6094 | 82.21 | 1319 | 17.79 | 1.21 | 1.14 | 1.28 | <0.001 | |
| Catastrophic illness | ||||||||||||||||||
| No | 153,669 | 85,478 | 77.25 | 68,191 | 61.63 | 63,988 | 74.86 | 21,490 | 25.14 | 53,093 | 77.86 | 15,098 | 22.14 | 1.00 | ||||
| Yes | 67,621 | 25,167 | 22.75 | 42,454 | 38.37 | 20,966 | 83.31 | 4201 | 16.69 | 35,298 | 83.14 | 7156 | 16.86 | 0.87 | 0.85 | 0.9 | <0.001 | |
| CCI | ||||||||||||||||||
| 0 | 78,266 | 39,133 | 35.37 | 39,133 | 35.37 | 27,541 | 70.38 | 11,592 | 29.62 | 28,479 | 72.77 | 10,654 | 27.23 | 1.00 | ||||
| 1 | 54,702 | 27,351 | 24.72 | 27,351 | 24.72 | 20,694 | 75.66 | 6657 | 24.34 | 21,566 | 78.85 | 5785 | 21.15 | 1.08 | 1.04 | 1.13 | <0.001 | |
| 2 | 35,754 | 17,877 | 16.16 | 17,877 | 16.16 | 14,245 | 79.68 | 3632 | 20.32 | 14,892 | 83.30 | 2985 | 16.70 | 1.13 | 1.07 | 1.19 | <0.001 | |
| ≥3 | 52,568 | 26,284 | 23.76 | 26,284 | 23.76 | 22,474 | 85.50 | 3810 | 14.50 | 23,454 | 89.23 | 2830 | 10.77 | 1.01 | 0.95 | 1.07 | 0.875 | |
| DCSI | ||||||||||||||||||
| 0 | 148,583 | 74,292 | 67.14 | 74,291 | 67.14 | 55,188 | 74.29 | 19,104 | 25.71 | 57,123 | 76.89 | 17,168 | 23.11 | 1.00 | ||||
| 1 | 22,568 | 11,284 | 10.2 | 11,284 | 10.2 | 8454 | 74.92 | 2830 | 25.08 | 8871 | 78.62 | 2413 | 21.38 | 1.05 | 1.01 | 1.09 | 0.009 | |
| 2 | 37,096 | 18,548 | 16.76 | 18,548 | 16.76 | 15,652 | 84.39 | 2896 | 15.61 | 16,470 | 88.80 | 2078 | 11.20 | 0.92 | 0.88 | 0.97 | <0.001 | |
| ≥3 | 13,043 | 6521 | 5.89 | 6522 | 5.89 | 5660 | 86.80 | 861 | 13.20 | 5927 | 90.88 | 595 | 9.12 | 0.85 | 0.79 | 0.92 | <0.001 | |
| Hypertension | ||||||||||||||||||
| No | 44,134 | 22,603 | 20.43 | 21,531 | 19.46 | 17,385 | 76.91 | 5218 | 23.09 | 17,135 | 79.58 | 4396 | 20.42 | 1.00 | ||||
| Yes | 177,156 | 88,042 | 79.57 | 89,114 | 80.54 | 67,569 | 76.75 | 20,473 | 23.25 | 71,256 | 79.96 | 17,858 | 20.04 | 1.21 | 1.18 | 1.25 | <0.001 | |
| Hyperlipidemia | ||||||||||||||||||
| No | 86,266 | 37,485 | 33.88 | 48,781 | 44.09 | 32,923 | 87.83 | 4562 | 12.17 | 44,085 | 90.37 | 4696 | 9.63 | 1.00 | ||||
| Yes | 135,024 | 73,160 | 66.12 | 61,864 | 55.91 | 52,031 | 71.12 | 21,129 | 28.88 | 44,306 | 71.62 | 17,558 | 28.38 | 2.65 | 2.58 | 2.72 | <0.001 | |
| Physician volume | ||||||||||||||||||
| Low (<Q1) | 9027 | 4401 | 3.98 | 4626 | 4.18 | 3280 | 74.53 | 1121 | 25.47 | 3579 | 77.37 | 1047 | 22.63 | 1.00 | ||||
| Median (Q3~Q1) | 60,701 | 29,614 | 26.76 | 31,087 | 28.1 | 23,120 | 78.07 | 6494 | 21.93 | 25,078 | 80.67 | 6009 | 19.33 | 1.00 | 0.95 | 1.06 | 0.977 | |
| High (>Q3) | 151,562 | 76,630 | 69.26 | 74,932 | 67.72 | 58,554 | 76.41 | 18,076 | 23.59 | 59,734 | 79.72 | 15,198 | 20.28 | 1.09 | 1.03 | 1.15 | 0.002 | |
| Healthcare organization level | ||||||||||||||||||
| Medical center | 44,734 | 23,619 | 21.35 | 21,115 | 19.08 | 18,983 | 80.37 | 4636 | 19.63 | 17,177 | 81.35 | 3938 | 18.65 | 1.00 | ||||
| Regional hospital | 67,861 | 32,044 | 28.96 | 35,817 | 32.37 | 24,019 | 74.96 | 8025 | 25.04 | 27,963 | 78.07 | 7854 | 21.93 | 1.31 | 1.27 | 1.35 | <0.001 | |
| District hospital | 51,314 | 23,008 | 20.79 | 28,306 | 25.58 | 18,121 | 78.76 | 4887 | 21.24 | 23,688 | 83.69 | 4618 | 16.31 | 1.01 | 0.98 | 1.05 | 0.540 | |
| Community clinic | 52,800 | 30,408 | 27.48 | 22,392 | 20.24 | 22,553 | 74.17 | 7855 | 25.83 | 16,934 | 75.63 | 5458 | 24.37 | 0.90 | 0.87 | 0.93 | <0.001 | |
| Missing | 4581 | 1566 | 1.42 | 3015 | 2.72 | |||||||||||||
| Healthcare organization type | ||||||||||||||||||
| Public | 8715 | 4805 | 4.34 | 3910 | 3.53 | 3264 | 67.93 | 1541 | 32.07 | 2630 | 67.26 | 1280 | 32.74 | 1.00 | ||||
| Non-public | 212,575 | 105,840 | 95.66 | 106,735 | 96.47 | 81,690 | 77.18 | 24,150 | 22.82 | 85,761 | 80.35 | 20,974 | 19.65 | 0.57 | 0.54 | 0.61 | <0.001 | |
| Total | Non Dialysis | Dialysis | p Value | Risk of Dialysis # | ||||||||
| N | % | n | % | n | % | aHR | 95% CI | p Value | ||||
| Total | 221,290 | 100.00 | 217,255 | 98.18 | 4035 | 1.82 | ||||||
| Status | 0.898 | |||||||||||
| Non-disabled | 110,645 | 50.00 | 108,632 | 98.18 | 2013 | 1.82 | 1.00 | |||||
| Disabled | 110,645 | 50.00 | 108,623 | 98.17 | 2022 | 1.83 | 1.08 | 1.01 | 1.15 | 0.026 | ||
| P4P | <0.001 | |||||||||||
| Non P4P | 173,345 | 78.33 | 170,000 | 98.07 | 3345 | 1.93 | 1.00 | |||||
| P4P | 47,945 | 21.67 | 25,323 | 52.82 | 690 | 1.44 | 0.66 | 0.6 | 0.72 | <0.001 | ||
| Status × P4P interaction term | 0.839 | |||||||||||
| Total | Survival | Death | p Value | Risk of Death # | ||||||||
| N | % | n | % | n | % | aHR | 95% CI | p Value | ||||
| Total | 221,290 | 100.00 | 148,275 | 67.00 | 73,015 | 33.00 | ||||||
| Status | <0.001 | |||||||||||
| Non-disabled | 110,645 | 50.00 | 79,645 | 71.98 | 31,000 | 28.02 | 1.00 | |||||
| Disabled | 110,645 | 50.00 | 68,630 | 62.03 | 42,015 | 37.97 | 1.34 | 1.32 | 1.36 | <0.001 | ||
| P4P | <0.001 | |||||||||||
| Non P4P | 173,345 | 78.33 | 106,230 | 61.28 | 67,115 | 38.72 | 1.00 | |||||
| P4P | 47,945 | 21.67 | 42,045 | 87.69 | 5900 | 12.31 | 0.45 | 0.43 | 0.47 | <0.001 | ||
| Status × P4P interaction term | <0.001 | 0.87 | 0.82 | 0.92 | <0.001 | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuo, W.-Y.; Tsai, W.-C.; Kung, P.-T. Participation and Outcomes among Disabled and Non-Disabled People in the Diabetes Pay-for-Performance Program. Healthcare 2023, 11, 2742. https://doi.org/10.3390/healthcare11202742
Kuo W-Y, Tsai W-C, Kung P-T. Participation and Outcomes among Disabled and Non-Disabled People in the Diabetes Pay-for-Performance Program. Healthcare. 2023; 11(20):2742. https://doi.org/10.3390/healthcare11202742
Chicago/Turabian StyleKuo, Wei-Yin, Wen-Chen Tsai, and Pei-Tseng Kung. 2023. "Participation and Outcomes among Disabled and Non-Disabled People in the Diabetes Pay-for-Performance Program" Healthcare 11, no. 20: 2742. https://doi.org/10.3390/healthcare11202742
APA StyleKuo, W.-Y., Tsai, W.-C., & Kung, P.-T. (2023). Participation and Outcomes among Disabled and Non-Disabled People in the Diabetes Pay-for-Performance Program. Healthcare, 11(20), 2742. https://doi.org/10.3390/healthcare11202742







