Assessments of and Attitudes towards Specialist Teleconsultations among Nephrology and Posttransplant Outpatients during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. Questionnaire
2.3. Statistical Analysis
3. Results
3.1. Population
3.2. Teleconsultations
3.3. Type of TCs
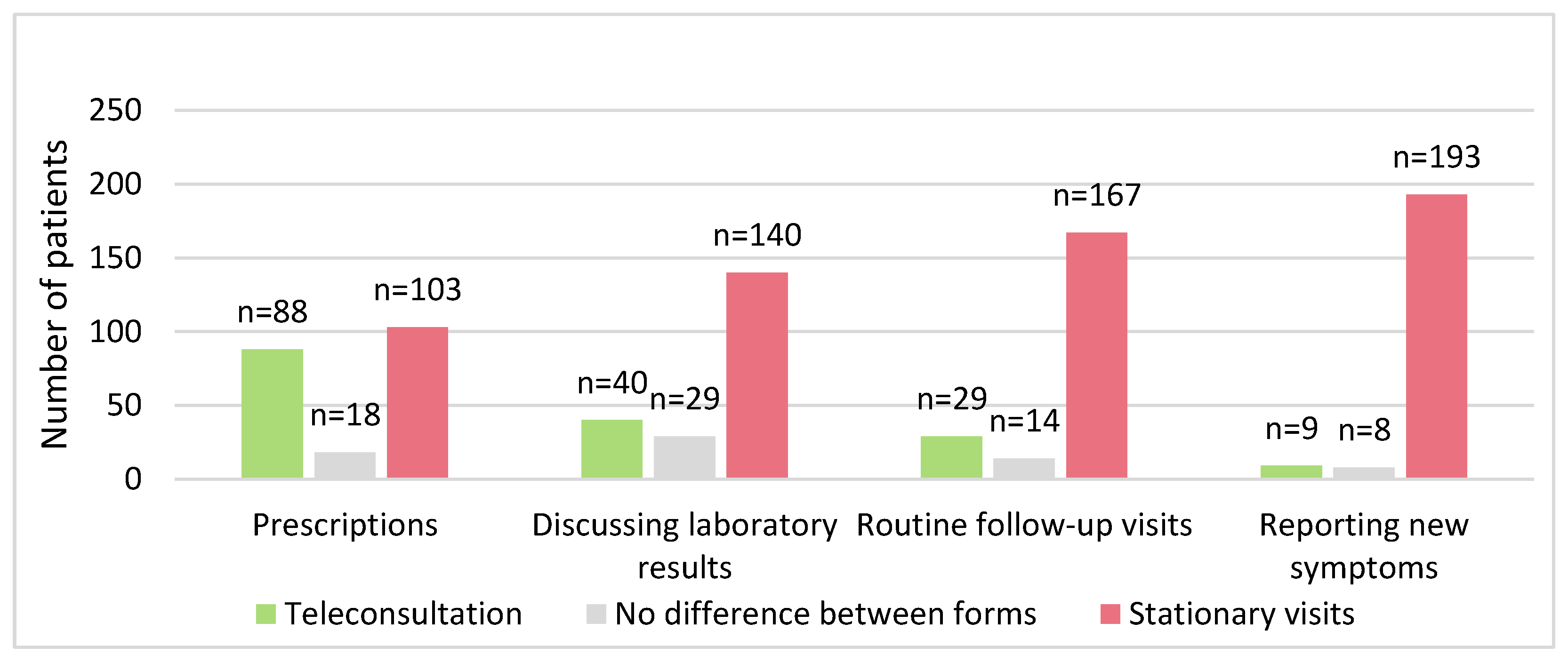
3.4. Attitude towards Telemedicine
3.5. Statistical Analysis
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Cao, B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Tedros Adhanom Ghebreyesus, Director General of WHO, declared COVID-19 a Pandemic 11th March 2020. Available online: https://news.un.org/en/story/2023/05/1136367 (accessed on 1 June 2023).
- Vagal, A.; Mahoney, M.; Allen, B.; Kapur, S.; Udstuen, G.; Wang, L.; Braley, S.; Makramalla, A.; Chadalavada, S.; Choe, K.A.; et al. Rescheduling Nonurgent Care in Radiology: Implementation During the Coronavirus Disease 2019 (COVID-19) Pandemic. J. Am. Coll. Radiol. 2020, 17, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, J. Quality of care in the COVID-19 era: A global perspective. IJQHC Communicat. 2022, 1, 1–3. [Google Scholar] [CrossRef]
- Regulation of the Minister of Health of 20th March 2020 on the Declaration of an Epidemic in the Territory of the Republic of Poland. Available online: https://www.covidlawlab.org/item/regulation-of-the-minister-of-health-of-20-march-2020-on-recalling-the-state-of-epidemic-threat-in-the-territory-of-the-republic-of-poland/ (accessed on 12 March 2023).
- Strehle, E.M.; Shabde, N. One hundred years of telemedicine: Does this new technology have a place in paediatrics? Arch. Dis. Child. 2006, 91, 956–959. [Google Scholar] [CrossRef] [PubMed]
- Deldar, K.; Bahaadinbeigy, K.; Tara, S.M. Teleconsultation and Clinical Decision Making: A Systematic Review. Acta Inform. Med. 2016, 24, 286–292. [Google Scholar] [CrossRef]
- Lambooy, S.; Krishnasamy, R.; Pollock, A.; Hilder, G.; Gray, N.A. Telemedicine for Outpatient Care of Kidney Transplant and CKD Patients. Kidney Int. Rep. 2021, 6, 1265–1272. [Google Scholar] [CrossRef]
- Zhao, B.; Zhang, L.; Ji, P.; Lin, J.; Han, J.; Li, J.; Chen, L. Bridging “Office-Based Care” With the “Virtual Practice Care Model”: Evolving Care for Chronic Kidney Disease Patients in the COVID-19 Pandemic—And beyond. Front. Med. 2020, 7, 1–10. [Google Scholar] [CrossRef]
- Tan, J.; Mehrotra, A.; Nadkarni, G.N.; He, J.C.; Langhoff, E.; Post, J.; Rohatgi, R. Telenephrology: Providing Healthcare to Remotely Located Patients with Chronic Kidney Disease. Am. J. Nephrol. 2018, 47, 200–207. [Google Scholar] [CrossRef]
- Regulation of the Polish Minister of Health of 4th November 2019. Available online: https://study.gov.pl/news/new-regulations-polish-government-are-announced-due-covid-19 (accessed on 25 February 2023).
- Mubaraki, A.A.; Alrabie, A.D.; Sibyani, A.K.; Aljuaid, R.S.; Bajaber, A.S.; Mubaraki, M.A. Advantages and disadvantages of telemedicine during the COVID-19 pandemic era among physicians in Taif, Saudi Arabia. Saudi Med. J. 2021, 42, 110–115. [Google Scholar] [CrossRef]
- Gajarawala, S.N.; Pelkowski, J.N. Telehealth Benefits and Barriers. JNP 2021, 17, 218–221. [Google Scholar] [CrossRef]
- Patient Service Department of National Health Fund of Poland: Patient Satisfaction Survey Report Using Teleconsultation with a Primary Care Physician Health Care during the COVID-19 Epidemic. 8 August 2020. Available online: https://www.gov.pl/attachment/a702e12b-8b16-44f1-92b5-73aaef6c165c (accessed on 28 September 2023).
- Beheshti, L.; Kalankesh, L.R.; Doshmangir, L.; Farahbakhsh, M. Telehealth in Primary Health Care: A Scoping Review of the Literature. Perspect. Health Inf. Manag. 2022, 19, 1–12. [Google Scholar] [PubMed]
- Jdiaa, S.S.; Mansour, R.; El Alayli, A.; Gautam, A.; Thomas, P.; Mustafa, R.A. COVID–19 and chronic kidney disease: An updated overview of reviews. J. Nephrol. 2022, 35, 69–85. [Google Scholar] [CrossRef] [PubMed]
- MacRae, C.; Mercer, S.W.; Guthrie, B.; Henderson, D. Comorbidity in chronic kidney disease: A large cross-sectional study of prevalence in Scottish primary care. Br. J. Gen. Pract. 2021, 71, e243–e249. [Google Scholar] [CrossRef]
- National Institutes of Health: Coronavirus Disease 2019 (COVID-19) Treatment Guidelines—Special Considerations in People Who Are Immunocompromised. 2022. Available online: https://files.covid19treatmentguidelines.nih.gov/guidelines/section/section_188.pdf (accessed on 19 January 2023).
- International Society of Nephrology: Recommendations for Prevention and Treatment of COVID-19. Available online: https://www.theisn.org/initiatives/covid-19/recommendations/#prevention-and-treatment-of-covid-19 (accessed on 19 January 2023).
- Duplaga, M. A Nationwide Natural Experiment of e-Health Implementation during the COVID-19 Pandemic in Poland: User Satisfaction and the Ease-of-Use of Remote Physician’s Visits. Nt. J. Environ. Res. Public Health 2022, 19, 8338. [Google Scholar] [CrossRef] [PubMed]
- Public Information Provided by the Health Care Services Division of the Polish National Health Fund; National Health Fund: Kingston, Jamaica, 2022.
- Reichheld, F.F. The one number you need to grow. Harv. Bus. Rev. 2003, 81, 46–54. [Google Scholar]
- Krol, M.W.; de Boer, D.; Delnoij, D.M.; Rademakers, J.J. The Net Promoter Score—An asset to patient experience surveys? Health Expect. 2014, 18, 3099–3109. [Google Scholar] [CrossRef] [PubMed]
- Ladino, M.A.; Wiley, J.; Schulman, I.H.; Sabucedo, A.J.; Garcia, D.; Cardona, J.M.; Echeverri, R.J. Tele-Nephrology: A Feasible Way to Improve Access to Care for Patients with Kidney Disease Who Reside in Underserved Areas. Telemed. e-Health 2016, 22, 650–654. [Google Scholar] [CrossRef]
- Nord, G.; Rising, K.L.; Band, R.A.; Carr, B.G.; Hollander, J.E. On-demand synchronous audio video telemedicine visits are cost effective. Am. J. Emerg. Med. 2019, 37, 890–894. [Google Scholar] [CrossRef]
- Almathami, H.K.Y.; Win, K.T.; Vlahu-Gjorgievska, E. Barriers and Facilitators That Influence Telemedicine-Based, Real-Time, Online Consultation at Patients’ Homes: Systematic Literature Review. J. Med. Internet Res. 2020, 22, e16407. [Google Scholar] [CrossRef]
- Blumen, H.; Fitch, K.; Polkus, V. Comparison of Treatment Costs for Breast Cancer, by Tumor Stage and Type of Service. Am. Health Drug Benefits 2016, 9, 23–32. [Google Scholar] [PubMed]
- George, K.; Subbiah, A.; Yadav, R.K.; Bagchi, S.; Mahajan, S.; Bhowmik, D.; Agarwal, S.K. Utility and patient acceptance of telemedicine in nephrology. J. Nephrol. 2022, 35, 2325–2331. [Google Scholar] [CrossRef]
- Alismail, A.; Schaeffer, B.; Oh, A.; Hamiduzzaman, S.; Daher, N.; Song, H.Y.; Tan, L.D. The Use of the Net Promoter Score (NPS) in an Outpatient Allergy and Pulmonary Clinic: An Innovative Look into Using Tablet-Based Tool vs Traditional Survey Method. Patient Relat. Outcome Meas. 2020, 11, 137–142. [Google Scholar] [CrossRef]
- Koladycz, R.; Fernandez, G.; Gray, K.; Marriott, H. The Net Promoter Score (NPS) for Insight into Client Experiences in Sexual and Reproductive intoth Clinics. Glob Health Sci. Pract. 2018, 6, 413–424. [Google Scholar] [CrossRef]
- Jaakkimainen, L.; Glazier, R.; Barnsley, J.; Salkeld, E.; Lu, H.; Tu, K. Waiting to see the specialist: Patient and provider characteristics of wait times from primary to specialty care. BMC Fam. Pract. 2014, 15, 1–13. [Google Scholar] [CrossRef]
- Devadula, S.; Langbecker, D.; Vecchio, P.; Tesiram, J.; Meiklejohn, J.; Benham, H. Tele-Rheumatology to Regional Hospital Outpatient Clinics: Patient Perspectives on a New Model of Care. Telemed J. e-Health 2020, 26, 912–919. [Google Scholar] [CrossRef] [PubMed]
- Adams, L.; Lester, S.; Hoon, E.; van Der Haak, H.; Proudman, C.; Hall, C.; Hill, C.L. Patient satisfaction and acceptability with telehealth at specialist medical outpatient clinics during the COVID-19 pandemic in Australia. Intern. Med. J. 2021, 51, 1028–1037. [Google Scholar] [CrossRef]
- Hoff, T.; Lee, D.R. Physician Satisfaction with Telehealth: A Systematic Review and Agenda for Future Research. Qual. Manag. Health Care 2022, 31, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Orrange, S.; Patel, A.; Mack, W.J.; Cassetta, J. Patient Satisfaction and Trust in Telemedicine During the COVID-19 Pandemic: Retrospective Observational Study. JMIR Hum. Factors 2021, 8, e28589. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization: Ageing and Health. 1 October 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 19 January 2023).
| Variables | All Respondents (n = 294) | TC Group (n = 212) |
|---|---|---|
| Age (years) | 57.06 ± 15.64 | 55.24 (44–68) |
| Gender (%) | ||
| male | 54.8 (n = 161) | 53.8 (n = 114) |
| female | 43.9 (n = 129) | 44.8 (n = 95) |
| No response | 1.3 (n = 4) | 1.4 (n = 3) |
| Occupation (%) | ||
| Student | 0.3 (n = 1) | 0.5 (n = 1) |
| Working | 35.7 (n = 105) | 38.7 (n = 82) |
| Unemployed | 2.4 (n = 7) | 2.8 (n = 6) |
| Retired/Pensioner | 61.6 (n = 181) | 58.0 (n = 123) |
| Level of education (%) | ||
| Primary | 5.5 (n = 16) | 5.6 (n = 12) |
| Secondary | 67.3 (n = 198) | 65.6 (n = 139) |
| University | 27.2 (n = 80) | 28.8 (n = 61) |
| Place of residence (%) | ||
| Rural | 28.6 (n = 84) | 30.7 (n = 65) |
| City < 10,000 inhabitants | 3.8 (n = 11) | 4.2 (n = 9) |
| City 10,000–50,000 inhabitants | 17.3 (n = 51) | 18.4 (n = 39) |
| City 50,000–100,000 inhabitants | 7.1 (n = 21) | 5.6 (n = 12) |
| City 100,000–500,000 inhabitants | 7.1 (n = 21) | 8.5 (n = 18) |
| City > 500,000 inhabitants | 36.1 (n = 106) | 32.6 (n = 69) |
| Variables | TC Group (n = 212) |
|---|---|
| Belonging to Outpatient Clinic (%) | |
| <6 months | 3.3 (n = 7) |
| 6 months–2 years | 11.8 (n = 25) |
| 2–5 years | 20.8 (n = 44) |
| >5 years | 59.0 (n = 125) |
| No response | 5.1 (n = 11) |
| Distance from Outpatient Clinic (%) | |
| Same city | 29.7 (n = 63) |
| <10 km | 3.8 (n = 8) |
| 10–50 km | 26.9 (n = 57) |
| >50 km | 37.3 (n = 79) |
| No response | 2.3 (n = 5) |
| Number of in-person visits to Outpatient Clinic (%) | |
| 0 | 4.7 (n = 10) |
| 1 | 5.2 (n = 11) |
| 2–4 | 27.4 (n = 58) |
| 5 or more | 57.1 (n = 121) |
| No response | 5.6 (n = 12) |
| Remote visit to another specialist outpatient clinic (%) | |
| No | 35.4 (n = 75) |
| 1 | 20.3 (n = 43) |
| 2 or more | 40.6 (n = 86) |
| No response | 3.7 (n = 8) |
| Number of in-person visits to family clinic (%) | |
| 0 | 23.1 (n = 49) |
| 1 | 9.9 (n = 21) |
| 2–4 | 36.8 (n = 78) |
| 5 or more | 29.7 (n = 63) |
| No response | (n = 0) |
| Number of in-person visits to family clinic (%) | |
| 0 | 9.9 (n = 21) |
| 1 | 14.2 (n = 30) |
| 2–4 | 42.5 (n = 90) |
| 5 or more | 29.7 (n = 63) |
| No response | 3.7 (n = 8) |
| Use of remote services (%) | |
| Yes | 65.1 (n = 138) |
| No | 34.0 (n = 72) |
| No response | 0.9 (n = 2) |
| Use of Patient Internet Account (%) | |
| Yes | 51.4 (n = 109) |
| No | 48.1 (n = 102) |
| No response | 0.5 (n = 1) |
| Advantages | TC Group (n = 212) | Disadvantages | TC Group (n = 212) |
|---|---|---|---|
| Not leaving home (%) | 61.3 (n = 130) | No physical examination (%) | 59.0 (n = 125) |
| Lower infection risk (%) | 54.2 (n = 115) | Higher risk of misdiagnosis (%) | 32.5 (n = 69) |
| Shorter waiting time (%) | 35.8 (n = 76) | Problems with describing symptoms (%) | 19.3 (n = 41) |
| No benefits (%) | 9.9 (n = 21) | Technical problems (%) | 19.9 (n = 38) |
| Other (%) | 0.9 (n = 2) | Not understanding doctors’ orders (%) | 4.7 (n = 10) |
| No disadvantages (%) | 22.6 (n = 48) | ||
| Other (%) | 0.9 (n = 2) |
| Variables | Telemedicine | |
|---|---|---|
| Positive Assessment | Future Participation | |
| Sex (M/F) | p = 0.326 | p = 0.327 |
| Use of remote services (Yes/No) | p = 0.351 | p = 0.128 |
| Use of Patient Internet Account (Yes/No) | p = 0.233 | p = 0.011 |
| Participations in TCs in primary health care (Yes/No) | p = 0.184 | p = 0.373 |
| Time of affiliation to a clinic (0–5) | p = 0.056 R = 0.138 | p = 0.110 R = 0.114 |
| Distance from clinic (0–3) | p = 0.078 R = 0.126 | p = 0.113 R = −0.111 |
| Number of TCs in studied clinics (0–2) | p = 0.092 R = 0.125 | p = 0.147 R = −0.105 |
| Participation in TCs in other specialist clinics (0–2) | p = 0.016 R = −2.429 | p = 0.802 R = 0.018 |
| Age | p = 0.638 R = −0.334 | p = 0.098 R = 0.115 |
| Place of residence (0–5) | p = 0.334 R = −0.069 | p = 0.077 R = 0.122 |
| Employment (0–4) | p = 0.579 R = 0.339 | p = 0.716 R = 0.023 |
| Level of education (0–3) | p = 0.339 R = 0.068 | p = 0.234 R = −0.083 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Edyko, K.; Edyko, P.; Nowicka, M.; Kurnatowska, I. Assessments of and Attitudes towards Specialist Teleconsultations among Nephrology and Posttransplant Outpatients during the COVID-19 Pandemic. Healthcare 2023, 11, 2737. https://doi.org/10.3390/healthcare11202737
Edyko K, Edyko P, Nowicka M, Kurnatowska I. Assessments of and Attitudes towards Specialist Teleconsultations among Nephrology and Posttransplant Outpatients during the COVID-19 Pandemic. Healthcare. 2023; 11(20):2737. https://doi.org/10.3390/healthcare11202737
Chicago/Turabian StyleEdyko, Krzysztof, Paweł Edyko, Maja Nowicka, and Ilona Kurnatowska. 2023. "Assessments of and Attitudes towards Specialist Teleconsultations among Nephrology and Posttransplant Outpatients during the COVID-19 Pandemic" Healthcare 11, no. 20: 2737. https://doi.org/10.3390/healthcare11202737
APA StyleEdyko, K., Edyko, P., Nowicka, M., & Kurnatowska, I. (2023). Assessments of and Attitudes towards Specialist Teleconsultations among Nephrology and Posttransplant Outpatients during the COVID-19 Pandemic. Healthcare, 11(20), 2737. https://doi.org/10.3390/healthcare11202737






