Resilience, Perceived Stress from Adapted Medical Education Related to Depression among Medical Students during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measurements
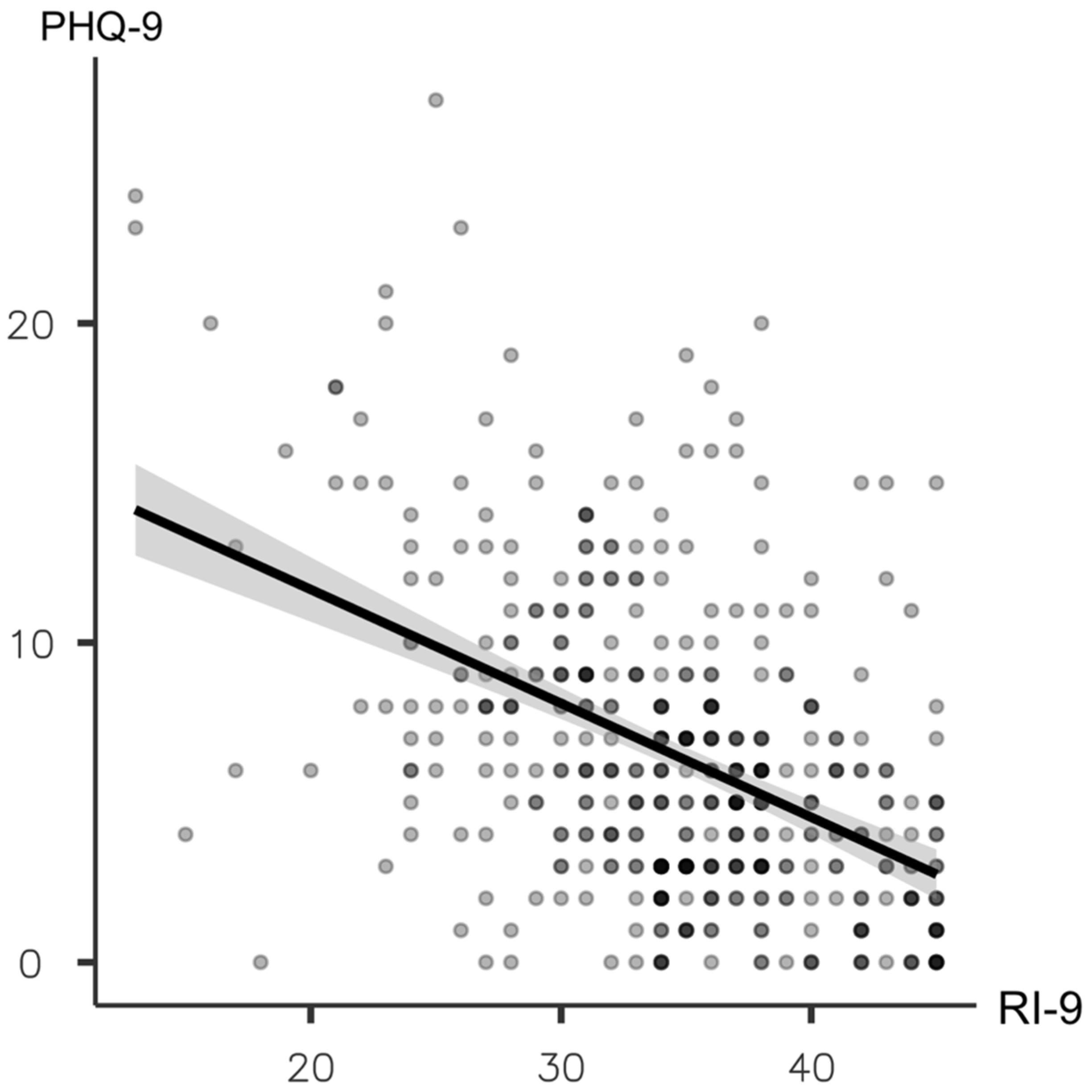
- The Resilience Inventory (RI-9) is a self-rating measurement consisting of nine items focused on individual recovery after encountering changing situation. Each question was scored on a 5-point Likert scale. The items have a response format with 5 options, where “1” means the statement “does not describe me at all” and “5” means “it describes me very well”. The minimum score is 9 and the maximum score is 45. Higher scores indicate greater levels of resilience. The psychometric properties of this measurement were tested in a sample of 140 university students and demonstrated good reliability and internal consistency [21]. The person reliability is 0.86 using Rasch analysis and the Cronbach’s alpha value is 0.90 in this study’s sample was 0.91.
- The Thai version of the Patient Health Questionnaire (PHQ-9) was used to measure depressive symptoms. The Thai version of PHQ-9 is a self-reported nine-question screening scale that uses a 4-point Likert scale to screen depressive symptoms. The 9 items describing the intensity of depressive symptoms was rated from 0 (“not at all”) to 3 (“nearly every day”). Scores on the Thai version of PHQ-9 are from 0 to 27, with scores ≥9 indicating significant depressive symptoms [22,23]. Higher scores represent greater depressive symptoms. The sensitivity at the cut-off value of 9 or greater was 0.84 and the specificity was 0.77. The internal consistency of the PHQ-9 in this study was acceptable (alpha coefficient = 0.79).
- Perceived stress related to AMEC was measured by a set of questions that asked about the extent of stress an individual perceived from lacking opportunities to complete their clinical practices in laboratories and their clinical works, in-person contact with peers, in-person communication with teachers, and completing examinations online. Participants responded to each question using a 4-Likert type of scale, ranging from 0 (no impact), 1 (mild impact), 2 (moderate impact), to 3 (severe impact) [7,8,9].
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Clinical Implications and Suggested Future Research
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rothan, H.A.; Byrareddy, S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020, 109, 102433. [Google Scholar] [CrossRef] [PubMed]
- Shen, K.; Yang, Y.; Wang, T.; Zhao, D.; Jiang, Y.; Jin, R.; Zheng, Y.; Xu, B.; Xie, Z.; Lin, L.; et al. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: Experts’ consensus statement. World J. Pediatr. WJP 2020, 16, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Țăran, A.-M.; Mustea, L.; Vătavu, S.; Lobonț, O.-R.; Luca, M.-M. Challenges and Drawbacks of the EU Medical System Generated by the COVID-19 Pandemic in the Field of Health Systems’ Digitalization. Int. J. Environ. Res. Public Health 2022, 19, 4950. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.-H.; Yang, H.-L.; Yang, Y.-Q.; Liu, D.; Li, Z.-H.; Zhang, X.-R.; Zhang, Y.-J.; Shen, D.; Chen, P.-L.; Song, W.-Q.; et al. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. J. Affect. Disord. 2020, 275, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.; Hu, T.; Hu, B.; Jin, C.; Wang, G.; Xie, C.; Chen, S.; Xu, J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020, 274, 1–7. [Google Scholar] [CrossRef]
- Ministry of Education, T. Ministry of Education of Thailand Action Plan, the Preparation for Education in Thailand in 1 July 2020. Available online: https://www.moe.go.th/การเตรียมความพร้อมของการจ/ (accessed on 12 December 2022).
- Shetty, S.; Shilpa, C.; Dey, D.; Kavya, S. Academic Crisis During COVID 19: Online Classes, a Panacea for Imminent Doctors. Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 45–49. [Google Scholar] [CrossRef]
- Puranachaikere, T.; Hataiyusuk, S.; Anupansupsai, R.; In-Iw, S.; Saisavoey, N.; Techapanuwat, T.; Arunrodpanya, F.; Charonpongsuntorn, C.; Wiwattanaworaset, P.; Siripongpan, A.; et al. Stress and associated factors with received and needed support in medical students during COVID-19 pandemic: A multicenter study. Korean J. Med. Educ. 2021, 33, 203–213. [Google Scholar] [CrossRef]
- Zhao, L.; Sznajder, K.; Cheng, D.; Wang, S.; Cui, C.; Yang, X. Coping Styles for Mediating the Effect of Resilience on Depression Among Medical Students in Web-Based Classes During the COVID-19 Pandemic: Cross-sectional Questionnaire Study. J. Med. Internet Res. 2021, 23, e25259. [Google Scholar] [CrossRef]
- Cheng, C.K.T.; Chua, J.H.; Cheng, L.J.; Ang, W.H.D.; Lau, Y. Global prevalence of resilience in health care professionals: A systematic review, meta-analysis and meta-regression. J. Nurs. Manag. 2022, 30, 795–816. [Google Scholar] [CrossRef]
- Labrague, L.J. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: A systematic review of quantitative studies. J. Nurs. Manag. 2021, 29, 1893–1905. [Google Scholar] [CrossRef]
- Ruengorn, C.; Awiphan, R.; Phosuya, C.; Ruanta, Y.; Wongpakaran, N.; Wongpakaran, T.; Thavorn, K.; Nochaiwong, S. Psychological Resilience and Adverse Mental Health Issues in the Thai Population during the Coronavirus Disease 2019 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 13023. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Jeste, D.V.; Savla, G.N.; Thompson, W.K.; Vahia, I.V.; Glorioso, D.K.; Martin, A.v.S.; Palmer, B.W.; Rock, D.; Golshan, S.; Kraemer, H.C.; et al. Older Age is Associated with More Successful Aging: Role of Resilience and Depression. Am. J. Psychiatry 2013, 170, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Lupe, S.E.; Keefer, L.; Szigethy, E. Gaining resilience and reducing stress in the age of COVID-19. Curr. Opin. Gastroenterol. 2020, 36, 295–303. [Google Scholar] [CrossRef]
- Zhao, F.; Guo, Y.; Suhonen, R.; Leino-Kilpi, H. Subjective well-being and its association with peer caring and resilience among nursing vs. medical students: A questionnaire study. Nurse Educ. Today 2016, 37, 108–113. [Google Scholar] [CrossRef]
- Kelifa, M.O.; Yang, Y.; Herbert, C.; He, Q.; Wang, P. Psychological resilience and current stressful events as potential mediators between adverse childhood experiences and depression among college students in Eritrea. Child Abus. Negl. 2020, 106, 104480. [Google Scholar] [CrossRef]
- Baste, V.S.; Gadkari, J.V. Study of stress, self-esteem and depression in medical students and effect of music on perceived stress. Indian J. Physiol. Pharmacol. 2014, 58, 298–301. [Google Scholar]
- Yu, J.H.; Chae, S.J. Differences in Academic Burnout and Achievement Goal Orientation by Perfectionism of Medical Students. J. Health Inform. Stat. 2016, 41, 88–95. [Google Scholar] [CrossRef]
- Lyons, Z.; Wilcox, H.; Leung, L.; Dearsley, O. COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australas Psychiatry 2020, 28, 649–652. [Google Scholar] [CrossRef]
- Hiranwong, T.; Sitthiprawiat, P.; Siritikul, S.; Jiwtrakul, J.; Klaychaiya, S.; Chaipinchana, P.; Kuntawong, P.; Wongpakaran, T.; Wongpakaran, N.; Deesomchok, A.; et al. Mental Strength and Challenges among Thai Medical Students in Their Clinical Years-Study Protocol. Healthcare 2021, 9, 305. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Lotrakul, M.; Sumrithe, S.; Saipanish, R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry 2008, 8, 46. [Google Scholar] [CrossRef] [PubMed]
- Cuttilan, A.N.; Sayampanathan, A.A.; Ho, R.C.-M. Mental health issues amongst medical students in Asia: A systematic review [2000–2015]. Ann. Transl. Med. 2016, 4, 72. [Google Scholar] [CrossRef]
- Pattanaseri, K.; Atsariyasing, W.; Pornnoppadol, C.; Sanguanpanich, N.; Srifuengfung, M. Mental problems and risk factors for depression among medical students during the COVID-19 pandemic: A cross-sectional study. Medicine 2022, 101, e30629. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Hegde, S.; Son, C.; Keller, B.; Smith, A.; Sasangohar, F. Investigating Mental Health of US College Students During the COVID-19 Pandemic: Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e22817. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.J. Moving forward: Embracing challenges as opportunities to improve medical education in the post-COVID era. Humanit. Soc. Sci. Commun. 2022, 9, 419. [Google Scholar] [CrossRef]
- Althwanay, A.; Ahsan, F.; Oliveri, F.; Goud, H.K.; Mehkari, Z.; Mohammed, L.; Javed, M.; Rutkofsky, I.H. Medical Education, Pre- and Post-Pandemic Era: A Review Article. Cureus 2020, 12, e10775. [Google Scholar] [CrossRef]
- Walter, G.; Soh, N.L.; Norgren Jaconelli, S.; Lampe, L.; Malhi, G.S.; Hunt, G. Medical students’ subjective ratings of stress levels and awareness of student support services about mental health. Postgrad. Med. J. 2013, 89, 311–315. [Google Scholar] [CrossRef]
- Siddique, M.A.B.; Ovi, M.R.; Ahammed, T.; Chowdhury, M.A.B.; Uddin, M.J. Mental health knowledge and awareness among university students in Bangladesh. Heliyon 2022, 8, e11084. [Google Scholar] [CrossRef]
- Peng, P.; Hao, Y.; Liu, Y.; Chen, S.; Wang, Y.; Yang, Q.; Wang, X.; Li, M.; Wang, Y.; He, L.; et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2022, 321, 167–181. [Google Scholar] [CrossRef]
- Yang, Q.; Kanjanarat, P.; Wongpakaran, T.; Ruengorn, C.; Awiphan, R.; Nochaiwong, S.; Wongpakaran, N.; Wedding, D. Fear of COVID-19 and Perceived Stress: The Mediating Roles of Neuroticism and Perceived Social Support. Healthcare 2022, 10, 812. [Google Scholar] [CrossRef] [PubMed]
- Rumas, R.; Shamblaw, A.L.; Jagtap, S.; Best, M.W. Predictors and consequences of loneliness during the COVID-19 Pandemic. Psychiatry Res. 2021, 300, 113934. [Google Scholar] [CrossRef] [PubMed]
- Nikčević, A.V.; Marino, C.; Kolubinski, D.C.; Leach, D.; Spada, M.M. Modelling the contribution of the Big Five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. J. Affect. Disord. 2021, 279, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Phomprasith, S.; Karawekpanyawong, N.; Pinyopornpanish, K.; Jiraporncharoen, W.; Maneeton, B.; Phinyo, P.; Lawanaskol, S. Prevalence and Associated Factors of Depression in Medical Students in a Northern Thailand University: A Cross-Sectional Study. Healthcare 2022, 10, 488. [Google Scholar] [CrossRef] [PubMed]
- Santabárbara, J.; Olaya, B.; Bueno-Notivol, J.; Pérez-Moreno, M.; Gracia-García, P.; Ozamiz-Etxebarria, N.; Idoiaga-Mondragon, N. Prevalence of depression among medical students during the COVID-19 pandemic. A systematic review and meta-analysis. Rev. Med. Chile 2021, 149, 1579–1588. [Google Scholar] [CrossRef]
- Chang, J.; Yuan, Y.; Wang, D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. J. South. Med. Univ. 2020, 40, 171–176. [Google Scholar] [CrossRef]
- Rachoin, J.-S.; Vilceanu, M.O.; Franzblau, N.; Gordon, S.; Hunter, K.; Cerceo, E. Influence of demographic and socio-economic factors in choosing hospitalist careers among US medical students. BMC Med. Educ. 2022, 22, 736. [Google Scholar] [CrossRef]
- Rajapuram, N.; Langness, S.; Marshall, M.R.; Sammann, A. Medical students in distress: The impact of gender, race, debt, and disability. PloS ONE 2020, 15, e0243250. [Google Scholar] [CrossRef]
- Torun, F.; Torun, S.D. The psychological impact of the COVID-19 pandemic on medical students in Turkey. Pak. J. Med. Sci. 2020, 36, 1355–1359. [Google Scholar] [CrossRef]
- Van Der Feltz-Cornelis, C.M.; Varley, D.; Allgar, V.L.; de Beurs, E. Workplace Stress, Presenteeism, Absenteeism, and Resilience Amongst University Staff and Students in the COVID-19 Lockdown. Front. Psychiatry 2020, 11, 588803. [Google Scholar] [CrossRef]
- Zhang, J.; Yang, Z.; Wang, X.; Li, J.; Dong, L.; Wang, F.; Li, Y.; Wei, R.; Zhang, J. The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: A cross-sectional study. J. Clin. Nurs. 2020, 29, 4020–4029. [Google Scholar] [CrossRef]
- Liu, Y.; Cao, Z. The impact of social support and stress on academic burnout among medical students in online learning: The mediating role of resilience. Front. Public Health 2022, 10, 938132. [Google Scholar] [CrossRef]
- Kerdcharoen, N.; Kolkijkovin, V.; Thaworn, J. Resilience, Mental Health Impact and COVID-19 Related Mental Health Determinants among Medical Students during COVID-19 Epidemic. Vajira Med. J. J. Urban Med. 2021, 65, S101–S116. [Google Scholar] [CrossRef]
- Angelopoulou, P.; Panagopoulou, E. Resilience interventions in physicians: A systematic review and meta-analysis. Appl. Psychol. Health Well-Being 2022, 14, 3–25. [Google Scholar] [CrossRef]
- Angevaare, M.J.; Roberts, J.; van Hout, H.P.J.; Joling, K.J.; Smalbrugge, M.; Schoonmade, L.J.; Windle, G.; Hertogh, C. Resilience in older persons: A systematic review of the conceptual literature. Ageing Res. Rev. 2020, 63, 101144. [Google Scholar] [CrossRef]
- Hendriks, T.; Graafsma, T.; Hassankhan, A.; Bohlmeijer, E.; de Jong, J. Strengths and virtues and the development of resilience: A qualitative study in Suriname during a time of economic crisis. Int. J. Soc. Psychiatry 2018, 64, 180–188. [Google Scholar] [CrossRef]
- Hiremath, P.; Suhas Kowshik, C.S.; Manjunath, M.; Shettar, M. COVID 19: Impact of lock-down on mental health and tips to overcome. Asian J. Psychiatry 2020, 51, 102088. [Google Scholar] [CrossRef]
- Abd Elwahab, S.M.; Cosgrave, J.; Doherty, E.; Lowery, A. Grit personality trait of doctors and medical students in level 4 acute hospital. Surgeon 2022, 20, 216–224. [Google Scholar] [CrossRef]
- Parikh, N.C.; Sharma, P.S.; Chaudhary, P.J.; Gandhi, H.A.; Banwari, G.H. Study of attitude of interns toward psychiatry: A survey of a tertiary level hospital in Ahmedabad. Ind. Psychiatry J. 2014, 23, 143–148. [Google Scholar] [CrossRef]
- DeMaranville, J.; Wongpakaran, T.; Wongpakaran, N.; Wedding, D. Meditation and Five Precepts Mediate the Relationship between Attachment and Resilience. Children 2022, 9, 371. [Google Scholar] [CrossRef]
- Wongpakaran, N.; Pooriwarangkakul, P.; Suwannachot, N.; Mirnics, Z.; Kövi, Z.; Wongpakaran, T. Moderating role of observing the five precepts of Buddhism on neuroticism, perceived stress, and depressive symptoms. PLoS ONE 2022, 17, e0277351. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.; Marques, A.; Gomes, P.V. Individual Resilience Interventions: A Systematic Review in Adult Population Samples over the Last Decade. Int. J. Environ. Res. Public Health 2021, 18, 7564. [Google Scholar] [CrossRef] [PubMed]
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A.; Harvey, S.B. Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018, 8, e017858. [Google Scholar] [CrossRef] [PubMed]
- Lattie, E.G.; Adkins, E.C.; Winquist, N.; Stiles-Shields, C.; Wafford, Q.E.; Graham, A.K. Digital Mental Health Interventions for Depression, Anxiety, and Enhancement of Psychological Well-Being Among College Students: Systematic Review. J. Med. Int. Res. 2019, 21, e12869. [Google Scholar] [CrossRef]
| Demographic Data | Depression (n = 118) N (%) | Non-Depression (n = 319) N (%) | pc | p d |
|---|---|---|---|---|
| Sex assigned at birth: Male | 73 (61.86) | 176 (55.17) | 0.21 a | |
| Presence of previous history of psychiatric disorder | 92 (77.97) | 296 (92.79) | <0.001 *a | <0.001 * |
| Income per month <395 USD e | 25 (21.19) | 59 (18.50) | 0.53 a | |
| Age (year), Mean (SD) | 21.3 (1.62) | 21.4 (1.67) | 0.77 b | |
| Educational level | 0.64 a | |||
| - Pre-clinical training | 64 (54.24) | 165 (51.72) | ||
| - Clinical training | 54 (45.76) | 154 (48.28) | ||
| - Living alone | 79 (66.95) | 184 (57.68) | 0.079 a | |
| Perceived stress of AMEC | ||||
| Loss of opportunities for clinical practice and experiments | <0.001 * | <0.001 * | ||
| Median (IQR) | ||||
| - No impact | 16 (13.56) | 74 (23.20) | ||
| - Mild | 57 (48.31) | 176 (55.17) | ||
| - Moderate | 36 (30.51) | 60 (18.81) | ||
| - Severe | 9 (7.63) | 9 (2.82) | ||
| Lack of in-person contact with peer. Median (IQR) | <0.001 * | <0.001 * | ||
| - No impact | 21 (17.80) | 85 (26.65) | ||
| - Mild | 36 (30.51) | 154 (48.28) | ||
| - Moderate | 45 (38.14) | 65 (20.38) | ||
| - Severe | 16 (13.56) | 15 (4.70) | ||
| Lack of face-to-face communication with teachers, Median (IQR) | <0.001 * | <0.001 * | ||
| - impact | 32 (27.12) | 160 (50.16) | ||
| - Mild | 56 (47.46) | 122 (38.24) | ||
| - Moderate | 24 (20.34) | 33 (10.34) | ||
| - Severe | 6 (5.08) | 4 (1.25) | ||
| Online examinations, Median (IQR) | <0.001 * | <0.001 * | ||
| - No impact | 25 (21.19) | 100 (31.35) | ||
| - Mild | 47 (39.83) | 141 (44.20) | ||
| - Moderate | 28 (23.73) | 62 (19.44) | ||
| - Severe | 18 (15.25) | 16 (5.02) | ||
| Resilience Inventory (RI-9), Mean (SD) | 30.9 (6.18) | 35.8 (5.68) | <0.001 * | <0.001* |
| Variables | OR | p Value | 95% CI |
|---|---|---|---|
| Previous history of psychiatric disorder | 2.89 | 0.003 | 1.42 to 5.51 |
| Lack of in-person contact with peers | 1.47 | 0.014 | 1.08 to 2.02 |
| Lack of in-person communication with teachers | 1.49 | 0.021 | 1.06 to 2.10 |
| Resilience Inventory (RI-9) | 0.88 | <0.001 | 0.84 to 0.92 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chakeeyanun, B.; Wongpakaran, N.; Wongpakaran, T.; Oon-arom, A. Resilience, Perceived Stress from Adapted Medical Education Related to Depression among Medical Students during the COVID-19 Pandemic. Healthcare 2023, 11, 237. https://doi.org/10.3390/healthcare11020237
Chakeeyanun B, Wongpakaran N, Wongpakaran T, Oon-arom A. Resilience, Perceived Stress from Adapted Medical Education Related to Depression among Medical Students during the COVID-19 Pandemic. Healthcare. 2023; 11(2):237. https://doi.org/10.3390/healthcare11020237
Chicago/Turabian StyleChakeeyanun, Boonyarit, Nahathai Wongpakaran, Tinakon Wongpakaran, and Awirut Oon-arom. 2023. "Resilience, Perceived Stress from Adapted Medical Education Related to Depression among Medical Students during the COVID-19 Pandemic" Healthcare 11, no. 2: 237. https://doi.org/10.3390/healthcare11020237
APA StyleChakeeyanun, B., Wongpakaran, N., Wongpakaran, T., & Oon-arom, A. (2023). Resilience, Perceived Stress from Adapted Medical Education Related to Depression among Medical Students during the COVID-19 Pandemic. Healthcare, 11(2), 237. https://doi.org/10.3390/healthcare11020237









