Hyperhomocysteinemia in Patients with Newly Diagnosed Primary Hypertension in Can Tho City, Vietnam
Abstract
1. Introduction
2. Materials and Methods
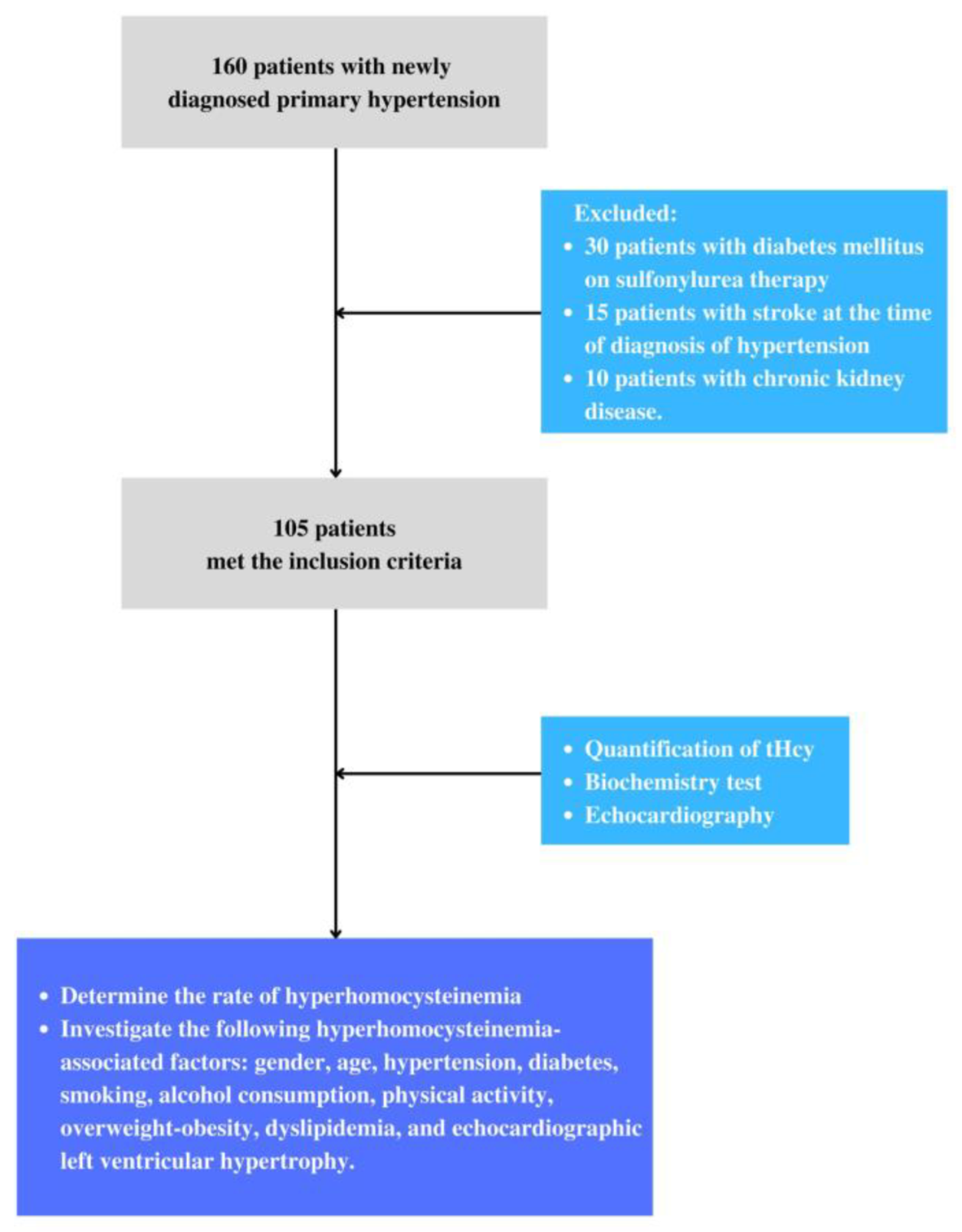
2.1. Study Population
2.1.1. Materials
2.1.2. Inclusion Criteria
2.1.3. Exclusion Criteria
2.2. Methods
2.2.1. Study Design
2.2.2. Sample Size
2.3. Data Collection
2.3.1. Data Analysis
2.3.2. Measurements
2.3.3. Statistical Analysis
3. Results
3.1. Baseline Subject Characteristics
3.2. Prevalence of Hyperhomocysteinemia in Patients with Primary Hypertension
3.3. Some Factors Associated with Hyperhomocysteinemia in Patients with Primary Hypertension
4. Discussion
4.1. Prevalence of Hyperhomocysteinemia in Patients with Primary Hypertension
4.2. Some Factors Associated with Hyperhomocysteinemia in Patients with Newly Diagnosed Primary Hypertension
Limitations
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| ADA | American Diabetes Association |
| AHA | American Heart Association |
| BMI | Body mass index |
| CRP | C-Reactive Protein |
| ESC | European Society of Cardiology |
| THcy | Total Homocysteine |
| JNC | Joint National Committee |
| SD | Standard deviation |
References
- Leung, A.; Daskalopoulou, S.; Dasgupta, K.; McBrien, K.; Butalia, S.; Zarnke, K.B.; Nerenberg, K.; Harris, K.C.; Nakhla, M.; Canada, H.; et al. Hypertension Canada’s 2017 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults. Can. J. Cardiol. 2017, 33, 557–576. [Google Scholar]
- Son, P.T.; Quang, N.N.; Viet, N.L.; Khai, P.G.; Wall, S.; Weinehall, L.; Bonita, R.; Byass, P. Prevalence, awareness, treatment and control of hypertension in Vietnam—Results from a national survey. J. Hum. Hypertens. 2012, 26, 268–280. [Google Scholar] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar]
- Begum, R.; Bhuiyan, M.M.A.; Ferdoushi, S.; Rahim, K.A.; Adhikari, D.K.; Rahman, S.M.R.; Pramanik, A.K.; Rahman, S.; Khan, F.I.; Islam, M.S.; et al. Raised Serum Homocysteine Level is Associated with Coronary Artery Disease in Young Patients. Arch. Clin. Biomed. Res. 2022, 6, 575–586. [Google Scholar]
- Paganelli, F.; Mottola, G.; Fromonot, J.; Marlinge, M.; Deharo, P.; Guieu, R.; Ruf, J. Hyperhomocysteinemia and cardiovascular diseases: Is the Adenosinergic System the Missing Link? Int. J. Mol. Sci. 2021, 22, 1690. [Google Scholar] [CrossRef] [PubMed]
- Koklesova, L.; Mazurakova, A.; Samec, M.; Biringer, K.; Samuel, S.M.; Büsselberg, D.; Kubatka, P.; Golubnitschaja, O. Homocysteine metabolism as the target for predictive medical approach, disease prevention, prognosis, and treatments tailored to the person. EPMA J. 2021, 12, 477–505. [Google Scholar]
- Zhang, Z.-Y.; Gu, X.; Tang, Z.; Guan, S.-C.; Liu, H.-J.; Wu, X.-G.; Zhao, Y.; Fang, X.-H. Homocysteine, hypertension, and risks of cardiovascular events and all-cause death in the Chinese elderly population: A prospective study. J. Geriatr. Cardiol. 2021, 18, 796. [Google Scholar]
- Zhao, W.; Gao, F.; Lv, L.; Chen, X. The interaction of hypertension and homocysteine increases the risk of mortality among middle-aged and older population in the United States. J. Hypertens. 2022, 40, 254–263. [Google Scholar] [CrossRef]
- Sheps, S.G. Overview of JNC VI: New directions in the management of hypertension and cardiovascular risk. Am. J. Hypertens. 1999, 12, 65S–75S. [Google Scholar] [CrossRef]
- Visseren, F.L.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Williams, B.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [PubMed]
- Kim, J.; Kim, H.; Roh, H.; Kwon, Y. Causes of hyperhomocysteinemia and its pathological significance. Arch. Pharmacal Res. 2018, 41, 372–383. [Google Scholar] [CrossRef]
- DeSouza, C.; Keebler, M.; McNamara, D.B.; Fonseca, V. Drugs affecting homocysteine metabolism. Drugs Context 2002, 62, 605–616. [Google Scholar]
- Cheng, M.; Xue, H.; Li, X.; Yan, Q.; Zhu, D.; Wang, Y.; Shi, Y.; Fu, C. Prevalence of hyperhomocysteinemia (HTHcy) and its major determinants among hypertensive patients over 35 years of age. Eur. J. Clin. Nutr. 2022, 76, 616–623. [Google Scholar]
- Verma, M.; Rajput, M.; Kishore, K.; Kathirvel, S. Asian BMI criteria are better than WHO criteria in predicting Hypertension: A cross-sectional study from rural India. J. Fam. Med. Prim. Care 2019, 8, 2095. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care 2017, 40 (Suppl. S1), S11–S24. [Google Scholar]
- American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes—2021. Diabetes Care 2021, 44 (Suppl. S1), S15–S33. [Google Scholar]
- Evaluation Expert Panel on Detection. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef] [PubMed]
- Devereux, R.B. Detection of left ventricular hypertrophy by M-mode echocardiography. Anatomic validation, standardization, and comparison to other methods. Hypertens. Res. 1987, 9, 19–26. [Google Scholar] [CrossRef]
- Stergiou, G.S.; Palatini, P.; Parati, G.; O’Brien, E.; Januszewicz, A.; Lurbe, E.; Persu, A.; Mancia, G.; Kreutz, R. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J. Hypertens. 2021, 39, 1293–1302. [Google Scholar] [CrossRef]
- Misra, A.; Dhurandhar, N.V. Current formula for calculating body mass index is applicable to Asian populations. Nutr. Diabetes 2019, 9, 3. [Google Scholar]
- Alam, S.F.; Kumar, S.; Ganguly, P. Measurement of homocysteine: A historical perspective. J. Clin. Biochem. Nutr. 2019, 65, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Mitra, K.; Ghosh, A.B.; Sarkar, A.; Saha, N.; Dutta, A.K. Colorimetric estimation of human glucose level using γ-Fe2O3 nanoparticles: An easily recoverable effective mimic peroxidase. Biochem. Biophys. Res. Commun. 2014, 451, 30–35. [Google Scholar] [CrossRef]
- Bragdon, J.H. Colorimetric determination of blood lipides. J. Biol. Chem. 1951, 190, 513–517. [Google Scholar] [CrossRef]
- Schnedl, W.J.; Krause, R.; Halwachs-Baumann, G.; Trinker, M.; Lipp, R.W.; Krejs, G.J. Evaluation of HbA1c determination methods in patients with hemoglobinopathies. Diabetes Care 2000, 23, 339–344. [Google Scholar] [CrossRef]
- Tran, S.K.; Huynh, H.T.N.; Ngo, T.H.; Nguyen, A.T.P.; Vo, C.T.; Nguyen, T.; Van Huynh, M. Effectiveness of combination of perindopril and indapamide on ambulatory arterial stiffness index in Vietnamese patients with primary hypertension. Pharm. Sci. Asia 2022, 49, 478–485. [Google Scholar] [CrossRef]
- Tsuda, K. Associations among plasma total homocysteine levels, circadian blood pressure variation, and endothelial function in hypertension. Am. J. Hypertens. 2018, 31, e1–e2. [Google Scholar] [CrossRef] [PubMed]
- Sutton-Tyrrell, K.; Bostom, A.; Selhub, J.; Zeigler-Johnson, C. High homocysteine levels are independently related to isolated systolic hypertension in older adults. Circulation 1997, 96, 1745–1749. [Google Scholar] [CrossRef]
- Morris, M.S.; Selhub, J.; Jacques, P.F. Vitamin B-12 and folate status in relation to decline in scores on the Mini-Mental State Examination in the Framingham Heart Study. J. Am. Geriatr. Soc. 2012, 60, 1457–1464. [Google Scholar] [PubMed]
- Lin, T.-Y.; Chen, Y.-J.; Chen, W.-L.; Peng, T.-C. The relationship between nonalcoholic fatty liver disease and retinopathy in NHANES III. PLoS ONE 2016, 11, e0165970. [Google Scholar] [CrossRef]
- De Bree, A.; Van Der Put, N.M.J.; IMennen, L.; Verschuren, W.M.M.; Blom, H.; Galan, P.; Bates, C.J.; Herrmann, W.; Ullrich, M.; Dierkes, J.; et al. Prevalences of hyperhomocysteinemia, unfavorable cholesterol profile and hypertension in European populations. Eur. J. Clin. Nutr. 2005, 59, 480–488. [Google Scholar] [PubMed]
- Onyemelukwe, O.U.; Maiha, B.B. Hyperhomocysteinemia and folate levels in normal healthy Nigerians living in Zaria: Subanalysis of ABU homocysteine cross-sectional survey. Ann. Afr. Med. 2019, 18, 143. [Google Scholar] [CrossRef]
- Poduri, A.; Kaur, J.; Thakur, J.S.; Kumari, S.; Jain, S.K.; Khullar, M. Effect of ACE inhibitors and β-blockers on homocysteine levels in essential hypertension. J. Hum. Hypertens. 2008, 22, 289–294. [Google Scholar] [CrossRef]
- Raza, S.T. Genetic Risk Factors in the Development of Hyperhomocysteinemia. In Nutritional Management and Metabolic Aspects of Hyperhomocysteinemia; Springer: Berlin/Heidelberg, Germany, 2021; pp. 99–113. [Google Scholar]
- Davis, J.; Juarez, D.; Hodges, K. Relationship of ethnicity and body mass index with the development of hypertension and hyperlipidemia. Ethnicity 2013, 23, 65–70. [Google Scholar]
- Karatela, R.; Sainani, G. Plasma homocysteine in obese, overweight and normal weight hypertensives and normotensives. Indian Heart J. 2009, 61, 156–159. [Google Scholar]
- Li, N.; Yi, F.X.; Rute, E.; Zhang, D.X.; Slocum, G.R.; Zou, A.P. Effects of homocysteine on intracellular nitric oxide and superoxide levels in the renal arterial endotheliu. Am. J. Physiol.-Heart Circ. Physiol. 2002, 283, H1237–H1243. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Wang, T.; Gao, J.; Wang, Y.; Chen, Y.; Kaliannan, K.; Li, X.; Xiao, J.; Ma, T.; Shao, Z.; et al. Associations of homocysteine status and homocysteine metabolism enzyme polymorphisms with hypertension and dyslipidemia in a Chinese hypertensive population. Clin. Exp. Hypertens. 2020, 42, 52–60. [Google Scholar] [CrossRef]
- Arina, C.A.; Amir, D.; Siregar, Y.; Sembiring, R.J. Correlation between homocysteine and dyslipidemia in ischaemic stroke patients with and without hypertension. In IOP Conference Series: Earth and Environmental Science; IOP Publishing: Medan, Indonesia, 2018; p. 012005. [Google Scholar]
- Deng, Y.; Li, Z.; An, X.; Fan, R.; Wang, Y.; Li, J.; Yang, X.; Liao, J.; Xia, Y. Hyperhomocysteinemia Promotes Cardiac Hypertrophy in Hypertension. Oxidative Med. Cell. Longev. 2022, 2022, 1486157. [Google Scholar] [CrossRef] [PubMed]
- Muzurović, E.; Kraljević, I.; Solak, M.; Dragnić, S.; Mikhailidis, D.P. Homocysteine and diabetes: Role in macrovascular and microvascular complications. J. Diabetes Complicat. 2021, 35, 107834. [Google Scholar]
- Henry, O.R.; Benghuzzi, H.; Taylor, H.A.; Tucci, M.; Butler, K.; Jones, L. Suppression of homocysteine levels by vitamin B12 and folates: Age and gender dependency in the Jackson Heart Study. Am. J. Med. Sci. 2012, 344, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Lim, U.; Cassano, P.A. Homocysteine and blood pressure in the third national health and nutrition examination survey, 1988–1994. Am. J. Epidemiol. 2002, 156, 1105–1113. [Google Scholar] [CrossRef]
- Wu, H.; Wang, B.; Ban, Q.; Chen, L.; Yan, D.; Yu, Y.; Song, Y.; Liu, C.; Cao, J.; Zhang, J.; et al. Association of total homocysteine with blood pressure in a general population of Chinese adults: A cross-sectional study in Jiangsu province, China. BMJ Open 2018, 8, e021103. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Kang, K.; Xue, Q.; Chen, Y.; Wang, W.; Cao, J. Value of plasma homocysteine to predict stroke, cardiovascular diseases, and new-onset hypertension: A retrospective cohort study. Medicine 2020, 99, e21541. [Google Scholar]
- Weber, G.J.; Pushpakumar, S.; Tyagi, S.C.; Sen, U. Homocysteine and hydrogen sulfide in epigenetic, metabolic and microbiota related renovascular hypertension. Pharmacol. Res. 2016, 113, 300–312. [Google Scholar]
- Joshi, R.R.Y. Effect of Antihypertensive Drugs on Homocysteine level among Hypertensive Patients. Age 2018, 20, 31–40. [Google Scholar]
- Onyemelukwe, O.U.; Maiha, B.B. Relationship between plasma homocysteine and blood pressure in hypertensive Northern-Nigerians. Afr. Health Sci. 2020, 20, 324–337. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Mean ± SD or n (%) |
|---|---|
| Age (years) | 63.07 ± 9.32 |
| BMI | 23.46 ± 3.23 |
| Total homocysteine (µmol/L) | 17.88 ± 6.03 |
| Male | 29 (27.6) |
| Grade 1 hypertension | 64 (60.9) |
| Grade 2 hypertension | 18 (17.1) |
| Grade 3 hypertension | 23 (21.9) |
| Age ≥ 60 | 72 (68.6) |
| Diabetes | 49 (46.7) |
| Overweight-obesity | 60 (57.1) |
| Dyslipidemia | 94 (89.5) |
| Left ventricular hypertrophy on echocardiogram | 25 (23.8) |
| Antiplateles | 15 (14.29) |
| Statin | 94 (89.5) |
| Metformin | 33 (31.43) |
| Factor | Hyperhomocysteinemia | OR | 95% CI | p * | ||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Gender | Male | 26 (89.7) | 3 (10.3) | 4.00 | 1.10–14.52 | 0.026 |
| Female | 52 (68.4) | 24 (31.6) | ||||
| Age ≥ 60 | Yes | 56 (77.8) | 16 (22.2) | 2.87 | 1.15–7.19 | 0.021 |
| No | 22 (66.7) | 11 (33.3) | ||||
| Diabetes | Yes | 32 (65.3) | 17 (34.7) | 0.41 | 0.17–1.01 | 0.049 |
| No | 46 (82.1) | 10 (7.9) | ||||
| Overweight-obesity | Yes | 46 (76.7) | 14 (23.3) | 1.34 | 0.55–3.22 | 0.519 |
| No | 32 (71.1) | 13 (28.9) | ||||
| Dyslipidemia | Yes | 69 (73.4) | 25 (25.6) | 0.61 | 0.12–3.04 | 0.725 |
| No | 9 (81.8) | 2 (18.2) | ||||
| Hypertension | Grade 1 | 37 (57.8) | 27 (42.2) | - | - | <0.001 |
| Grade 2 | 18 (100) | 0 (0.0) | ||||
| Grade 3 | 23 (100) | 0 (0.0) | ||||
| Left ventricular hypertrophy on echocardiogram | Yes | 22 (88.0) | 3 (12.0) | 3.14 | 0.86–11.49 | 0.072 |
| No | 56 (70.0) | 24 (30.0) | ||||
| Metformin therapy | Yes | 20 (60.6) | 13 (39.4) | 2.693 | 1.08–6.69 | 0.03 |
| No | 58 (80.6) | 14 (19.4) | ||||
| Factor | OR | 95% CI | p | |
|---|---|---|---|---|
| Gender | Male | 5.143 | 0.894–29.575 | 0.067 |
| Female | ||||
| Elder | Yes | 12.455 | 0.793–195.669 | 0.073 |
| No | ||||
| Diabetes | Yes | 0.25 | 0.079–0.796 | 0.019 |
| No | ||||
| Hypertension | Grade 1 | - | - | - |
| Grade 2 | - | - | 0.998 | |
| Grade 3 | - | - | 0.998 | |
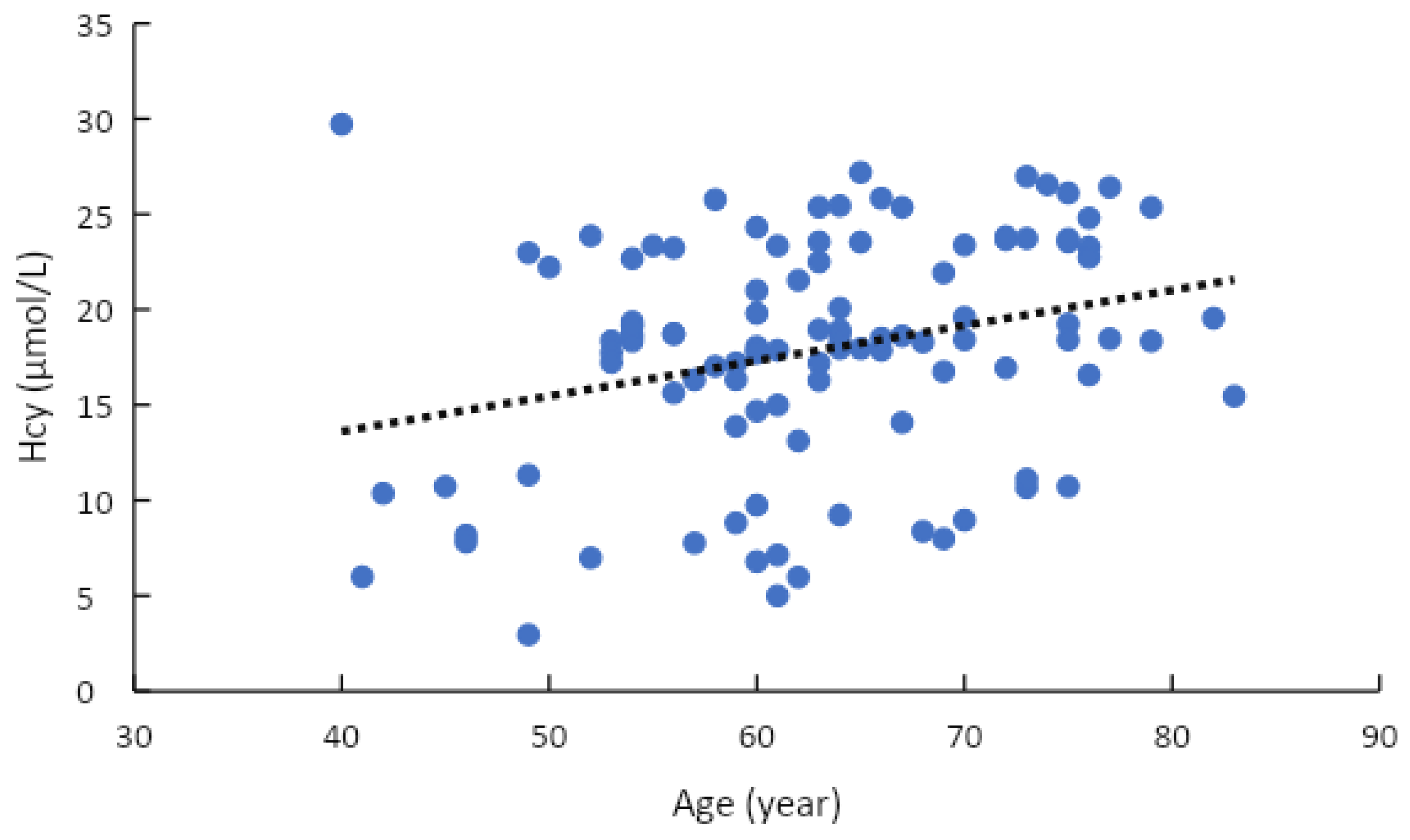
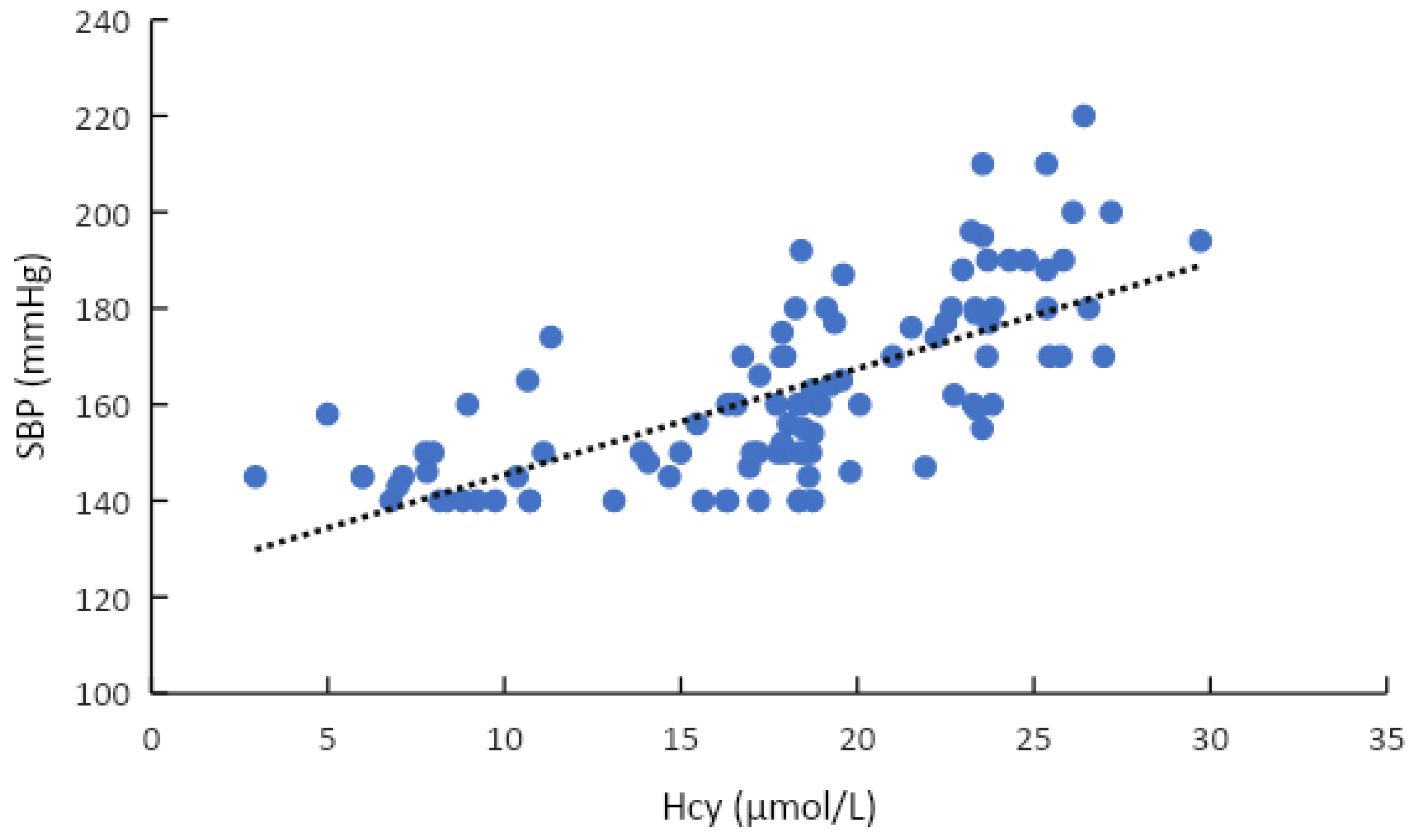
| Factor | r | p |
|---|---|---|
| SBP * | 0.696 | <0.001 |
| DBP * | 0.585 | <0.001 |
| Age * | 0.286 | 0.003 |
| Fasting blood glucose * | −0.046 | 0.642 |
| HbA1c * | −0.095 | 0.335 |
| Metformin therapy ** | −0.086 | 0.381 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, S.K.; Ngo, T.H.; Nguyen, P.H.; Truong, A.B.; Truong, G.K.; Tran, K.D.D.; Vo, P.M.; Nguyen, P.T.; Nguyen, T.T.; Nguyen, P.N.T.; et al. Hyperhomocysteinemia in Patients with Newly Diagnosed Primary Hypertension in Can Tho City, Vietnam. Healthcare 2023, 11, 234. https://doi.org/10.3390/healthcare11020234
Tran SK, Ngo TH, Nguyen PH, Truong AB, Truong GK, Tran KDD, Vo PM, Nguyen PT, Nguyen TT, Nguyen PNT, et al. Hyperhomocysteinemia in Patients with Newly Diagnosed Primary Hypertension in Can Tho City, Vietnam. Healthcare. 2023; 11(2):234. https://doi.org/10.3390/healthcare11020234
Chicago/Turabian StyleTran, Son Kim, Toan Hoang Ngo, Phi Hoang Nguyen, An Bao Truong, Giang Khanh Truong, Khoa Dang Dang Tran, Phuong Minh Vo, Phi The Nguyen, Thuan Tuan Nguyen, Phu Ngoc Thien Nguyen, and et al. 2023. "Hyperhomocysteinemia in Patients with Newly Diagnosed Primary Hypertension in Can Tho City, Vietnam" Healthcare 11, no. 2: 234. https://doi.org/10.3390/healthcare11020234
APA StyleTran, S. K., Ngo, T. H., Nguyen, P. H., Truong, A. B., Truong, G. K., Tran, K. D. D., Vo, P. M., Nguyen, P. T., Nguyen, T. T., Nguyen, P. N. T., Nguyen, K. T., & Tran, H. D. (2023). Hyperhomocysteinemia in Patients with Newly Diagnosed Primary Hypertension in Can Tho City, Vietnam. Healthcare, 11(2), 234. https://doi.org/10.3390/healthcare11020234






