Describing Trends in Maternal Mortality in the State of São Paulo, Brazil, from 2009 to 2019
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
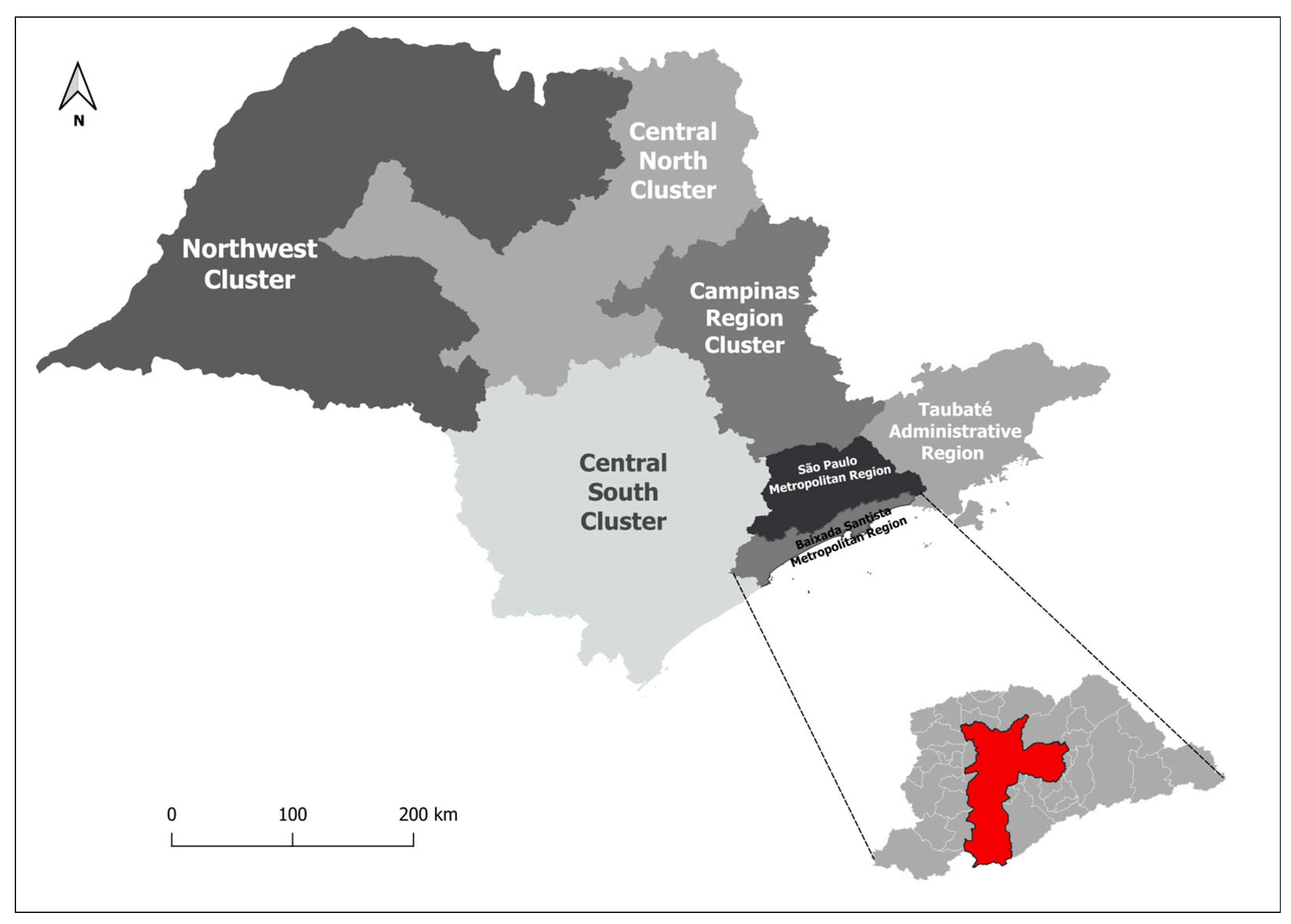
2.2. Study Location
2.3. Study Population
2.4. Inclusion and Exclusion Criteria
2.5. Data Collection
2.6. Instruments for Data Extraction
2.7. Study Variables
2.8. Statistical Analysis
2.9. Ethical and Legal Aspects of Research
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Maternal Mortality. Available online: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality (accessed on 2 June 2020).
- WHO. World Health Organization, UNICEF, UNFPA and The World Bank. Trends in Maternal Mortality: 1990 to 2010–WHO, UNICEF, UNFPA and The World Bank Estimates; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- UNICEF; UNFPA. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: Executive Summary; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- WHO World Health Organization; United Nations Children’s Fund; World Bank; United Nations; United Nations Population Division. Trends in Maternal Mortality: 1990 to 2015: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division [Internet]; World Health Organization: Geneva, Switzerland, 2015; 77p, Available online: https://apps.who.int/iris/bitstream/handle/10665/194254/9789241565141_eng.pdf (accessed on 10 April 2019).
- WHO World Health Organization (WHO). WHO Statement on cesarean section rates. Reprod. Health Matters 2015, 23, 149–150. [Google Scholar]
- United Nations. Development Goals the Millennium; Report; United Nations: New York, NY, USA, 2007. [Google Scholar]
- Laurenti, R.; Jorge, M.H.P.M.; Gotlieb, S.L.D. Maternal mortality in Brazilian State Capitals: Some characteristics and estimates for an adjustment factor. Rev. Bras. Epidemiol. 2004, 7, 449–460. [Google Scholar] [CrossRef]
- Ministério das Relações Exteriores. Transformando Nosso Mundo: A Agenda 2030 Para o Desenvolvimento Sustentável [Internet]; Nações Unidas: Rio de Janeiro, Brazil, 2016. Available online: https://www.mds.gov.br/webarquivos/publicacao/Brasil_Amigo_Pesso_Idosa/Agenda2030.pdf (accessed on 5 August 2020).
- Brasil. Ministério da Saúde [Homepage na Internet]; Indicadores e Dados Básicos: São Paulo, Brazil, 2012.
- Brasil; Ministério da Saúde. Manual dos Comitês de Morte Materna; Série A. Normas e Manuais Técnicos; Ministério da Saúde: Brasília, Brazil, 2007.
- RIPSA. Rede Interagência de Informações para a Saúde. Indicadores e Dados Básicos para o Brasil–2011. C. Indicadores de Mortalidade. Razão de Mortalidade Materna. Available online: http://tabnet.datasus.gov.br/cgi/idb2011/C03b.htm (accessed on 1 August 2020).
- Mota, S.M.M.; Gama, S.G.J.; Filha, M.M.T. Mortalidade materna e o Sistema de Informações sobre Mortalidade. Epidemiol. Rev. Saúde 2008, 17, 33–42. [Google Scholar]
- Calderon, M.G.; Santos, E.F.S.; Abreu, L.C.; Raimundo, R.D. Increasing prevalence, time trend and seasonality of gastroschisis in São Paulo state, Brazil, 2005–2016. Sci. Rep. 2019, 9, 14491. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- National Cancer Institute. Joinpoint Trend Analysis Software. Available online: https://surveillance.cancer.gov/joinpoint/ (accessed on 1 March 2022).
- Costa, A.A.R.; Ribas, M.S.S.S.; Amorim, M.M.R.; Santos, L.C. Mortalidade Materna na Cidade do Recife. Rev. Bras. Ginecol. Obs. 2002, 24, 455–462. [Google Scholar] [CrossRef]
- Ronsmans, C.; Graham, W.J. Maternal mortality: Who, when, where, and why. Lancet 2006, 368, 1189–1200. [Google Scholar] [CrossRef] [PubMed]
- Khab, K.S.; Wojdyla, D.; Say, L.; Gulmezoglu, A.M.; Van Look, P.F.A. Who analysis of causes of maternal death: A systematic review. Lancet 2006, 367, 1066–1074. [Google Scholar]
- Secretaria De Vigilância Em Saúde; Ministério da Saúde. Guia de Vigilância Epidemiológica do Óbito Materno; Ministério da Saúde: Brasília, Brazil, 2009.
- Instituto de Pesquisa Econômica Aplicada (IPEA). Objetivos de Desenvolvimento do Milênio: Relatório Nacional de Acompanhamento; IPEA: Brasília, Brazil, 2014. [Google Scholar]
- BRASIL; Ministério da Saúde (BR). Secretaria Executiva. Datasus. Informações de Saúde. Epidemiológicas e Morbidade [Internet]; Ministério da Saúde: Brasília, Brazil, 2014. Available online: http://www2.datasus.gov.br/DATASUS/index.php?area=0203 (accessed on 3 September 2015).
- Mendes, J.D.V.; Osiano, V.L.R.L. A Mortalidade Materna no Estado de São Paulo, Brasil. Bol. Epidemiol. Paul. 2013, 10, 17–29. [Google Scholar]
- Andreoni, S.; Silva, R.S.; Drezett, J. Who Is More Likely to Have Had an Induced Abortion? A Pooled Analysis of Three Studies in the World Health Organization; Mortalidad Materna: Nota Descriptiva 348; Organización Mundial de la Salud: Geneva, Switzerland, 2014. [Google Scholar]
- Fernandez, M.A.L.; Cavanillas, A.B.; Mateo, S. Excess of maternal mortality in foreign nationalities in Spain, 1999–2006. Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 149, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Kale, P.L.; Costa, A.J.L. Maternal Deaths in the City of Rio de Janeiro, Brazil, 2000–2003. Health Popul. Nutr. 2009, 27, 794–801. [Google Scholar] [CrossRef] [PubMed]
- Alves, S.V. Maternal Mortality in Pernambuco, Brazil: What Has Changed in Ten Years? Reprod. Health Matters 2007, 15, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Tharaux, C.D.; Carmona, E.; Colle, M.H.B.C.; Bréart, G. Postpartum Maternal Mortality and Cesarean Delivery. Obstet. Gynecol. 2006, 108, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Kongnyuy, E.J.; Mlaya, G.; Broek, N. Facility-Based Maternal Death Review in Three Districts in the Central Region of Malawi. An Analysis of Causes and Characteristics of Maternal Deaths. Women’s Health 2009, 19, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Calderon, I.M.P.; Cecatti, J.G.; Vega, C.E.P. Intervenções benéficas no pré-natal para prevenção da mortalidade materna. Rev. Bras. Gine Obs. 2006, 28, 310–315. [Google Scholar] [CrossRef]
- Brasil; Ministério da Saúde; Secretaria de Atenção à Saúde. Pacto Nacional pela Redução da Morte Maternal; Ministério da Saúde: Brasília, Brazil, 2004.
- MacKay, A.; Berg, C.J.; Duran, C.; Chang, J.; Rosenber, H. An assessment of pregnancy-related mortality in the United States. Paediatr. Perinat. Epidemiol. 2005, 19, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Carmo, L.M.; Pereira, A.P.; Domingues, R.M.; Theme-Filha, M.M.; Dias, M.A.; Nakamura-Pereira, M.; Bastos, M.H.; Gama, S.G. Obstetric interventions during labor and childbirth in Brazilian low-risk women. Cad Saúde Pública 2014, 30 (Suppl. 1), S1–S16. [Google Scholar]
- Diniz, D.; Medeiros, M. Itinerários e métodos do aborto ilegal em cinco capitais brasileiras. Ciências Saúde Coletiva 2012, 17, 1671–1681. [Google Scholar] [CrossRef] [PubMed]
- Singh, S. Hospital admissions resulting from unsafe abortion: Estimates from 13 developing countries. Lancet 2006, 368, 1887–1892. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Aquino, E.M.; Leal, M.D.C.; Monteiro, C.A.; Barros, F.C.; Szwarcwald, C.L. Maternal and child health in Brazil: Progress and challenges. Lancet 2011, 377, 1863–1876. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, L.Z.; Macedo, C.R.; Laignier, M.R.; Santos, B.B.; Sousa, L.V.A.; Ramos, J.L.S. Analysis of the perinatal mortality rate in the metropolitan region of Grande Vitória, Espírito Santo, Brazil, between 2008 and 2017. J. Hum. Growth Dev. 2023, 33, 250–259. [Google Scholar]
| Characteristics | Number of Maternal Deaths | Number of Live Births | % | Maternal Mortality Ratio * |
|---|---|---|---|---|
| Age group | ||||
| 10 to 14 years | 11 | 33,482 | 0.35 | 32.85 |
| 15 to 19 years | 293 | 882,005 | 9.52 | 332.19 |
| 20 to 29 years | 1140 | 3,251,041 | 37.03 | 35.06 |
| 30 to 39 years | 1351 | 2,321,948 | 43.93 | 58.18 |
| 40 to 49 years | 280 | 210,510 | 9.10 | 133.01 |
| Skin color/race | ||||
| White | 1729 | 4,142,023 | 56.22 | 41.74 |
| Black | 260 | 307,831 | 8.45 | 84.46 |
| Yellow | 11 | 35,251 | 0.35 | 31.20 |
| Mixed | 995 | 2,123,393 | 32.35 | 46.85 |
| Indigenous | 0 | 9712 | 0 | 0 |
| Ignored | 80 | 80,776 | 2.60 | 99.03 |
| Education | ||||
| None | 16 | 12,225 | 0.52 | 130.87 |
| 1–3 years | 193 | 94,529 | 6.27 | 204.17 |
| 4–7 years | 693 | 838,054 | 22.53 | 82.69 |
| 8–11 years | 1230 | 4,206,867 | 40 | 29.23 |
| 12 years or more | 380 | 1,507,636 | 12.36 | 25.20 |
| Ignored | 563 | 39,675 | 18.30 | 1419.02 |
| Marital status | ||||
| Single | 1549 | 2,901,981 | 50.37 | 53.37 |
| Married | 1050 | 2,744,176 | 34.14 | 38.26 |
| Widow | 22 | 12,358 | 0.71 | 178.02 |
| Judicially separated | 100 | 117,130 | 3.25 | 85.37 |
| Other | 247 | 778,756 | 8.03 | 31.71 |
| Ignored | 107 | 48,699 | 3.4 | 219.71 |
| Place of occurrence | ||||
| Hospital | 2854 | 6,650,684 | 92.81 | 42.91 |
| Another health facility | 92 | 25,246 | 2.99 | 364.41 |
| Home | 90 | 17,962 | 2.92 | 501.05 |
| Public highway | 5 | - | 0.16 | - |
| Other | 34 | 4943 | 1.10 | 687.84 |
| Ignored | 0 | 151 | 0 | 0 |
| Type of obstetric cause | ||||
| Direct obstetric | 1874 | - | 61.00 | - |
| Indirect obstetric | 1115 | - | 36.30 | - |
| Unspecified obstetric | 83 | - | 2.70 | - |
| Maternal death | ||||
| 2009 | 332 | 598,421 | 10.76 | 55.47 |
| 2010 | 259 | 601,289 | 8.40 | 43.07 |
| 2011 | 241 | 610,150 | 7.81 | 39.49 |
| 2012 | 219 | 616,545 | 7.10 | 35.52 |
| 2013 | 233 | 610,836 | 7.55 | 38.14 |
| 2014 | 254 | 625,590 | 8.23 | 40.60 |
| 2015 | 307 | 633,935 | 9.95 | 48.42 |
| 2016 | 299 | 601,393 | 9.69 | 49.71 |
| 2017 | 346 | 611,735 | 11.22 | 56.56 |
| 2018 | 302 | 606,065 | 9.79 | 49.82 |
| 2019 | 283 | 583,057 | 9.17 | 48.53 |
| Total | 3075 | 6,698,986 | 100 | 45.90 |
| Category CID 10 | N | % |
|---|---|---|
| Direct Obstetric Causes | ||
| O15 Eclampsia | 219 | 7.13 |
| O14 Gestational hypertension with significant proteinuria | 187 | 6.09 |
| O72 Postpartum hemorrhage | 181 | 5.89 |
| O88 Obstetric origin embolism | 126 | 4.10 |
| O85 Postpartum infection | 121 | 3.94 |
| O90 Postpartum complication NCOP | 115 | 3.74 |
| O62 Abnormalities of uterine contraction | 99 | 3.22 |
| O06 Abortion NE | 90 | 2.93 |
| O45 Premature detachment of the placenta | 79 | 2.57 |
| O00 Ectopic pregnancy | 75 | 2.44 |
| O23 Infection of the genitourinary tract in pregnancy | 71 | 2.31 |
| O75 Other complications of labor and childbirth NCOP | 62 | 2.02 |
| O13 Gestational hypertension without significant proteinuria | 39 | 1.27 |
| O16 Maternal hypertension NE | 35 | 1.14 |
| O44 Placenta previa | 35 | 1.14 |
| Other direct obstetric causes * | 340 | 11.07 |
| Indirect Obstetric Causes | ||
| O99 Other maternal illness COP compl grav childbirth puerp | 949 | 30.89 |
| O98 Inf paras mat disease COP compl grav childbirth puerp | 79 | 2.57 |
| O10 Hypertension pre-exist complic grav childbirth puerp | 66 | 2.15 |
| O24 Diabetes mellitus in pregnancy | 19 | 0.62 |
| O25 Desnutric in pregnancy | 2 | 0.07 |
| Unspecified Obstetric Causes | ||
| O95 Obstetric death NE | 83 | 2.70 |
| Total | 3072 | 100.00 |
| Category CID 10 | GSP | % | BSMR | % | TAR | % | CSC | % | NWC | % | CNC | % | CRC | % | Total | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Direct Obstetric Causes | ||||||||||||||||
| O15 Eclampsia | 121 | 7.36 | 9 | 4.35 | 13 | 12.15 | 13 | 6.63 | 14 | 5.6 | 22 | 8.24 | 27 | 6.84 | 219 | 7.13 |
| O14 Gestational hypertension w/proteinuria signif. | 90 | 5.47 | 16 | 7.73 | 6 | 5.61 | 13 | 6.63 | 14 | 5.6 | 21 | 7.87 | 27 | 6.84 | 187 | 6.09 |
| O72 Postpartum hemorrhage | 99 | 6.02 | 10 | 4.83 | 6 | 5.61 | 6 | 3.06 | 10 | 4 | 27 | 10.11 | 23 | 5.82 | 181 | 5.89 |
| O88 Obstetric orig embolism | 87 | 5.29 | 4 | 1.93 | 5 | 4.67 | 4 | 2.04 | 12 | 4.8 | 4 | 1.50 | 10 | 2.53 | 126 | 4.10 |
| O85 Puerperal infection | 69 | 4.19 | 6 | 2.90 | 3 | 2.80 | 8 | 4.08 | 6 | 2.4 | 13 | 4.87 | 16 | 4.05 | 121 | 3.94 |
| O90 Postpartum complication NCOP | 61 | 3.71 | 5 | 2.42 | 3 | 2.80 | 7 | 3.57 | 11 | 4.4 | 12 | 4.49 | 16 | 4.05 | 115 | 3.74 |
| O62 Abnormalities of uterine contraction | 42 | 2.55 | 9 | 4.35 | 3 | 2.80 | 10 | 5.10 | 11 | 4.4 | 8 | 3.00 | 16 | 4.05 | 99 | 3.22 |
| O06 Abortion NE | 71 | 4.32 | 1 | 0.48 | 1 | 0.93 | 1 | 0.51 | 6 | 2.4 | 5 | 1.87 | 5 | 1.27 | 90 | 2.93 |
| O45 Premature detachment of the placenta | 39 | 2.37 | 6 | 2.90 | 2 | 1.87 | 11 | 5.61 | 10 | 4 | 6 | 2.25 | 5 | 1.27 | 79 | 2.57 |
| O00 Ectopic pregnancy | 35 | 2.13 | 6 | 2.90 | 3 | 2.80 | 5 | 2.55 | 7 | 2.8 | 7 | 2.62 | 12 | 3.04 | 75 | 2.44 |
| O23 Infection of the genitourinary tract in pregnancy | 27 | 1.64 | 4 | 1.93 | 4 | 3.74 | 4 | 2.04 | 7 | 2.8 | 7 | 2.62 | 18 | 4.56 | 71 | 2.31 |
| O75 Other complications of labor and childbirth NCOP | 22 | 1.34 | 4 | 1.93 | 3 | 2.80 | 11 | 5.61 | 7 | 2.8 | 12 | 4.49 | 3 | 0.76 | 62 | 2.02 |
| O13 Gestational hypertension without proteinuria signif. | 19 | 1.16 | 5 | 2.42 | 1 | 0.93 | 4 | 2.04 | 3 | 1.2 | 4 | 1.50 | 3 | 0.76 | 39 | 1.27 |
| O16 Maternal hypertension NE | 15 | 0.91 | 3 | 1.45 | 3 | 2.80 | 2 | 1.02 | 4 | 1.6 | 4 | 1.50 | 4 | 1.01 | 35 | 1.14 |
| O44 Placenta previa | 19 | 1.16 | 1 | 0.48 | 2 | 1.87 | 2 | 1.02 | 4 | 1.6 | 5 | 1.87 | 2 | 0.51 | 35 | 1.14 |
| Other direct obstetric causes | 154 | 9.36 | 28 | 13.53 | 15 | 14.02 | 30 | 15.31 | 30 | 12 | 33 | 12.36 | 50 | 12.66 | 340 | 11.07 |
| Indirect Obstetric Causes | ||||||||||||||||
| O99 Other doenc mat COP compl grav childbirth puerp | 528 | 32.10 | 76 | 36.71 | 23 | 21.50 | 52 | 26.53 | 79 | 31.6 | 54 | 20.22 | 137 | 34.68 | 949 | 30.89 |
| O98 Inf paras mat disease COP compl grav childbirth puerp | 38 | 2.31 | 10 | 4.83 | 4 | 3.74 | 6 | 3.06 | 8 | 3.2 | 6 | 2.25 | 7 | 1.77 | 79 | 2.57 |
| O10 Hypertension pre-exist complic grav childbirth puerp | 47 | 2.86 | 2 | 0.97 | 1 | 0.93 | 1 | 0.51 | 3 | 1.2 | 3 | 1.12 | 9 | 2.28 | 66 | 2.15 |
| O24 Diabetes mellitus in pregnancy | 13 | 0.79 | 1 | 0.48 | 3 | 2.80 | 1 | 0.51 | 0 | 0 | 1 | 0.37 | 0 | 0.00 | 19 | 0.62 |
| O25 Malnutrition in pregnancy | 1 | 0.06 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0 | 1 | 0.37 | 0 | 0.00 | 2 | 0.07 |
| Unspecified Obstetric Causes | ||||||||||||||||
| O95 Cause obstetric death NE | 48 | 2.92 | 1 | 0.48 | 3 | 2.80 | 5 | 2.55 | 4 | 1.6 | 12 | 4.49 | 5 | 1.27 | 83 | 2.70 |
| Total | 1645 | 100 | 207 | 100 | 107 | 100 | 196 | 100 | 250 | 100 | 267 | 100 | 395 | 100 | 3072 | 100 |
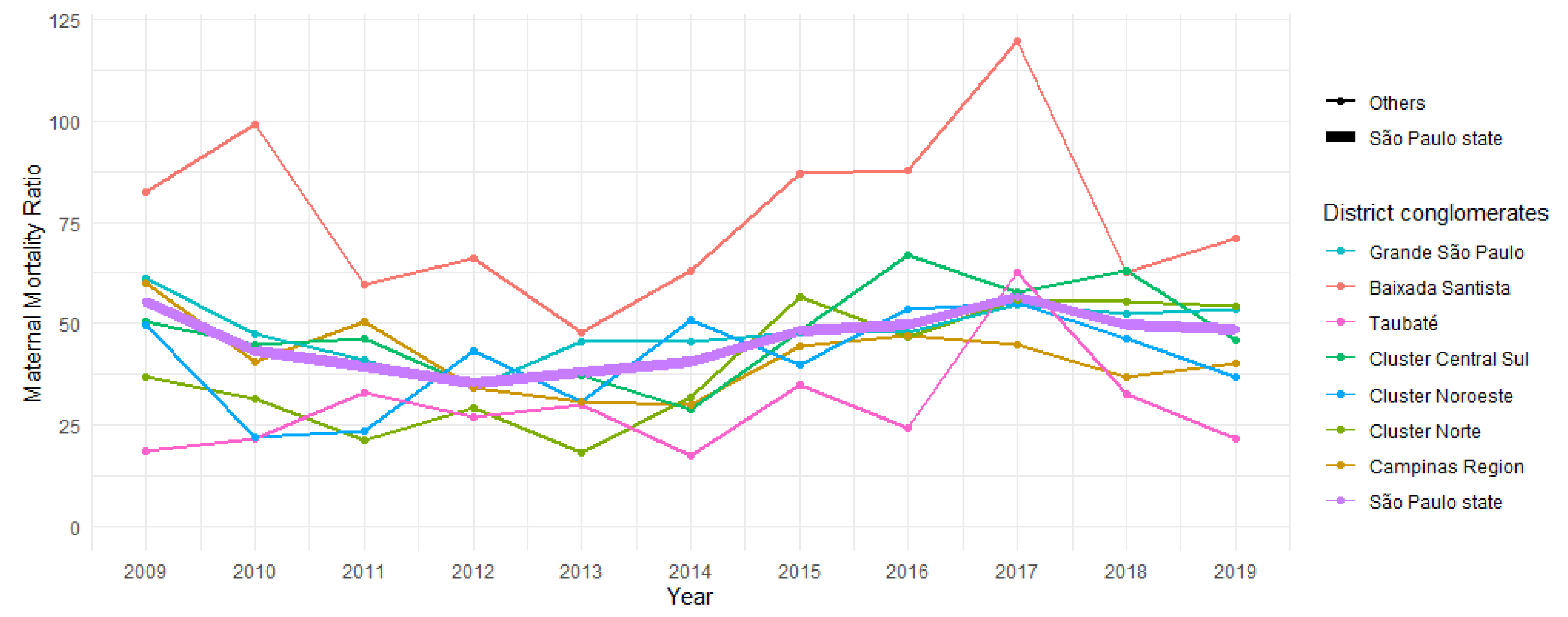
| District Conglomerates | Maternal Mortality Ratio | Range | APC (95% CI) | AAPC (95% CI) | ||
|---|---|---|---|---|---|---|
| 2009 | 2019 | 2009–2019 | ||||
| Baixada Santista | 82.6 | 71.2 | 77.0 | 2009–2019 | 0.7 (−4.9; 6.6) | 0.7 (−4.9; 6.6) |
| Cluster Campinas Region | 60.0 | 40.4 | 41.9 | 2009–2019 | −1.5 (−5.8; 3.0) | −1.5 (−5.8; 3.0) |
| Cluster Centro Norte | 36.7 | 54.4 | 39.8 | 2009–2019 | 8.9 (2.1; 16.1) ↑ | 8.9 (2.1; 16.1) ↑ |
| Cluster Centro Sul | 50.4 | 46.1 | 47.7 | 2009–2019 | 2.8 (−2.7; 8.6) | 2.8 (−2.7; 8.6) |
| Cluster Noroeste | 49.8 | 36.8 | 41.1 | 2009–2019 | 5.5 (0.4; 10.9) ↑ | 5.5 (0.4; 10.9) ↑ |
| Grande São Paulo | 61.2 | 53.5 | 48.3 | 2009–2011 | −20.9 (−44.9; 13.6) | −0.8 (−6.5; 5.3) |
| 2011–2019 | 5.0 (2.6; 7.4) ↑ | 4.3 (−1.8; 10.8) | ||||
| Taubaté | 18.7 | 21.8 | 29.5 | 2009–2019 | 4.3 (−1.8; 10.8) | |
| São Paulo State | 55.5 | 48.5 | 46.0 | 2009–2011 | −17.5 (−38.6; 10.9) | −0.1 (−5.3; 5.3) |
| 2011–2019 | 4.8 (0.9; 8.8) ↑ | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva Bueno, L.A.; Ribeiro, M.A.L.; Martins, C.B.; de Abreu, L.C.; de Almeida, A.D., Jr.; Correa, J.A. Describing Trends in Maternal Mortality in the State of São Paulo, Brazil, from 2009 to 2019. Healthcare 2023, 11, 2522. https://doi.org/10.3390/healthcare11182522
da Silva Bueno LA, Ribeiro MAL, Martins CB, de Abreu LC, de Almeida AD Jr., Correa JA. Describing Trends in Maternal Mortality in the State of São Paulo, Brazil, from 2009 to 2019. Healthcare. 2023; 11(18):2522. https://doi.org/10.3390/healthcare11182522
Chicago/Turabian Styleda Silva Bueno, Luciane Amorim, Mariane Albuquerque Lima Ribeiro, Camila Bertini Martins, Luiz Carlos de Abreu, Alvaro Dantas de Almeida, Jr., and João Antonio Correa. 2023. "Describing Trends in Maternal Mortality in the State of São Paulo, Brazil, from 2009 to 2019" Healthcare 11, no. 18: 2522. https://doi.org/10.3390/healthcare11182522
APA Styleda Silva Bueno, L. A., Ribeiro, M. A. L., Martins, C. B., de Abreu, L. C., de Almeida, A. D., Jr., & Correa, J. A. (2023). Describing Trends in Maternal Mortality in the State of São Paulo, Brazil, from 2009 to 2019. Healthcare, 11(18), 2522. https://doi.org/10.3390/healthcare11182522






