Virtual Reality Simulation for Advanced Infection Control Education in Neonatal Intensive Care Units: Focusing on the Prevention of Central Line-Associated Bloodstream Infections and Ventilator-Associated Infections
Abstract
1. Introduction
1.1. Study Aims
1.2. Research Hypotheses
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Research Tools
2.3.1. General Characteristics
2.3.2. Infection Control Knowledge
2.3.3. Confidence in Infection Control
2.3.4. Presence
2.3.5. Empathy
2.3.6. Program Satisfaction
2.4. VR_AICENICU Program Development
2.4.1. Step 1: Validation of the Infection Control and Development Procedures
2.4.2. Step 2: Modeling and Construction for VR Implementation
2.4.3. Step 3: VR Program Equipment and Software
2.5. Study Procedures
2.5.1. Pre-Survey
2.5.2. Experimental Treatment
2.5.3. Post-Survey
2.6. Data Analysis
2.7. Ethical Considerations
3. Results
3.1. Homogeneity Testing of General Characteristics and Study Variables
3.2. Program Effectiveness Testing
3.2.1. Hypothesis 1
3.2.2. Hypothesis 2
3.3. VR Simulation Program-Related Presence, Empathy, and Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, A.-R.; Kim, E.-J.; Kim, C.-S.; Park, M.-S.; Park, J.-Y.; Shim, G.-H.; Eun, B.-W.; Lee, B.; Chang, M.-Y.; Choi, S.-H.; et al. Perspective of Nationwide Surveillance System for Healthcare associated-Infection in Neonatal Intensive Care Units. Korean J. Healthc. Assoc. Infect. Control Prev. 2020, 25, 154–156. [Google Scholar] [CrossRef]
- Korean National Healthcare-Associated Infections Surveillance System Korean National Healthcare Associated Infections Surveillance System (KONIS) Neonatal Intensive Care Units (NICU) Report: Data Summary from July 2020 to June 2021. Available online: http://konis.cafe24.com/xe/reports_nicu_y (accessed on 1 February 2023).
- Chang, Y.S. Moving Forward to Improve Safety and Quality of Neonatal Intensive Care in Korea. J. Korean Med. Sci. 2018, 33, e89. [Google Scholar] [CrossRef]
- Stoll, B.J.; Hansen, N.; Fanaroff, A.A.; Wright, L.L.; Carlo, W.A.; Ehrenkranz, R.A.; Lemons, J.A.; Donovan, E.F.; Stark, A.R.; Tyson, J.E.; et al. Late-Onset Sepsis in Very Low Birth Weight Neonates: The Experience of the NICHD Neonatal Research Network. Pediatrics 2002, 110, 285–291. [Google Scholar] [CrossRef]
- Kusuda, S.; Fujimura, M.; Sakuma, I.; Aotani, H.; Kabe, K.; Itani, Y.; Ichiba, H.; Matsunami, K.; Nishida, H. Neonatal Research Network, Japan Morbidity and Mortality of Infants with Very Low Birth Weight in Japan: Center Variation. Pediatrics 2006, 118, e1130-8. [Google Scholar] [CrossRef]
- Lee, S.M.; Chang, M.; Kim, K.-S. Blood Culture Proven Early Onset Sepsis and Late Onset Sepsis in Very-Low-Birth-Weight Infants in Korea. J. Korean Med. Sci. 2015, 30 (Suppl. 1), S67–S74. [Google Scholar] [CrossRef]
- Menon, G. Neonatal Long Lines. Arch. Dis. Child. Fetal Neonatal Ed. 2003, 88, F260–F262. [Google Scholar] [CrossRef]
- Erdei, C.; McAvoy, L.L.; Gupta, M.; Pereira, S.; McGowan, E.C. Is Zero Central Line-Associated Bloodstream Infection Rate Sustainable? A 5-Year Perspective. Pediatrics 2015, 135, e1485-93. [Google Scholar] [CrossRef]
- Zoutman, D.E.; Ford, B.D.; Gauthier, J. A Cross-Canada Survey of Infection Prevention and Control in Long-Term Care Facilities. Am. J. Infect. Control 2009, 37, 358–363. [Google Scholar] [CrossRef]
- Chung, M.S. Relationship between Knowledge and Performance of Infection Control among Nurses in the Neonatal Intensive Care Unit; University of Yonsei: Seoul, Republic of Korea, 2002. [Google Scholar]
- Kardong-Edgren, S.; Farra, S.L.; Alinier, G.; Young, H.M. A Call to Unify Definitions of Virtual Reality. Clin. Simul. Nurs. 2019, 31, 28–34. [Google Scholar] [CrossRef]
- Kneebone, R. Simulation in Surgical Training: Educational Issues and Practical Implications. Med. Educ. 2003, 37, 267–277. [Google Scholar] [CrossRef]
- Bailenson, J.; Patel, K.; Nielsen, A.; Bajscy, R.; Jung, S.-H.; Kurillo, G. The Effect of Interactivity on Learning Physical Actions in Virtual Reality. Media Psychol. 2008, 11, 354–376. [Google Scholar] [CrossRef]
- Ahn, M.K.; Lee, C.M. Development and effects of head-mounted display-based home-visits virtual reality simulation program for nursing students. J. Korean Acad. Nurs. 2021, 51, 465–477. [Google Scholar] [CrossRef] [PubMed]
- Ma, M.; Jain, L.C.; Anderson, P. Future Trends of Virtual, Augmented Reality, and Games for Health. In Virtual, Augmented Reality and Serious Games for Healthcare 1; Springer: Berlin/Heidelberg, Germany, 2014; pp. 1–6. [Google Scholar]
- Issenberg, S.B.; McGaghie, W.C.; Petrusa, E.R.; Lee Gordon, D.; Scalese, R.J. Features and Uses of High-Fidelity Medical Simulations That Lead to Effective Learning: A BEME Systematic Review. Med. Teach. 2005, 27, 10–28. [Google Scholar] [CrossRef] [PubMed]
- Verkuyl, M.; Hughes, M. Virtual Gaming Simulation in Nursing Education: A Mixed-Methods Study. Clin. Simul. Nurs. 2019, 29, 9–14. [Google Scholar] [CrossRef]
- Oh, I.S. The Effect of Cognitive Experience and Flow for VR Advertisements on Immersion and Behavioral Intention; Korea University: Seoul, Republic of Korea, 2018. [Google Scholar]
- Jung, D.H.; Song, J.S. A Study on the Satisfaction Survey for the Utilization of Augmented Reality of Mobile Historical Books. A J. Brand Des. Assoc. Korea 2020, 18, 89–100. [Google Scholar]
- Yoon, C.R. Development and Effectiveness of Virtual Reality-Based Learning Program for the New Nurses Caring Mechanical Ventilated Patients; University of Ulsan: Ulsan, Republic of Korea, 2021. [Google Scholar]
- Jung, H.; Chae, M. Experience the Core Fundamental Nursing Skills Practice of Nursing Students Using Virtual Reality. J. Humanit. Soc. Sci. 2020, 11, 703–716. [Google Scholar] [CrossRef]
- Yu, M.; Yang, M.; Ku, B.; Mann, J.S. Effects of Virtual Reality Simulation Program Regarding High-Risk Neonatal Infection Control on Nursing Students. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2021, 15, 189–196. [Google Scholar] [CrossRef]
- Kang, K.-A.; Kim, S.-J.; Lee, M.-N.; Kim, M.; Kim, S. Comparison of Learning Effects of Virtual Reality Simulation on Nursing Students Caring for Children with Asthma. Int. J. Environ. Res. Public Health 2020, 17, 8417. [Google Scholar] [CrossRef]
- Park, J.H. Adaptation of VR 360-Degree Intravenous Infusion Educational Content for Nursing Students. J. Converg. Cult. Technol. 2020, 6, 165–170. [Google Scholar]
- Borg Sapiano, A.; Sammut, R.; Trapani, J. The Effectiveness of Virtual Simulation in Improving Student Nurses’ Knowledge and Performance during Patient Deterioration: A Pre and Post Test Design. Nurse Educ. Today 2018, 62, 128–133. [Google Scholar] [CrossRef]
- Verkuyl, M.; Romaniuk, D.; Atack, L.; Mastrilli, P. Virtual gaming simulation for nursing education: An experiment. Clin. Simul. Nurs. 2017, 13, 238–244. [Google Scholar] [CrossRef]
- Yang, S.-Y.; Oh, Y.-H. The Effects of Neonatal Resuscitation Gamification Program Using Immersive Virtual Reality: A Quasi-Experimental Study. Nurse Educ. Today 2022, 117, 105464. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Kang, K.J. Effectiveness of a Role-Play Simulation Program Involving the Sbar Technique: A Quasi-Experimental Study. Nurse Educ. Today 2017, 53, 41–47. [Google Scholar] [CrossRef]
- Yu, M.; Kang, H.; Park, J.; Yang, M. Development of a High-Risk Neonatal Infection Control Competency Scale. J. Child Health Care 2021, 25, 393–411. [Google Scholar] [CrossRef]
- Chung, D.H.; Yang, H.C. Reliability and Validity Assessment in 3D Video Measurement. J. Broadcast Eng. 2012, 17, 49–59. [Google Scholar]
- Yu, M.; Yang, M.R. Effectiveness and Utility of Virtual Reality Infection Control Simulation for Children with COVID-19: Quasi-Experimental Study. JMIR Serious Games 2022, 10, e36707. [Google Scholar] [CrossRef] [PubMed]
- Sung, M.H.; Kim, N.Y.; Choi, H.Y. Factors Influencing Performance of the Nurses about the Management of Nosocomial Infection. Korean J. Occup. Health Nurs. 2007, 16, 5–14. [Google Scholar]
- Anderson, J.M.; Warren, J.B. Using Simulation to Enhance the Acquisition and Retention of Clinical Skills in Neonatology. Semin. Perinatol. 2011, 35, 59–67. [Google Scholar] [CrossRef]
- Benner, P. Using the Dreyfus Model of Skill Acquisition to Describe and Interpret Skill Acquisition and Clinical Judgment in Nursing Practice and Education. Bull. Sci. Technol. Soc. 2004, 24, 188–199. [Google Scholar] [CrossRef]
- Ragsdale, M.A.; Mueller, J. Plan, Do, Study, Act Model to Improve an Orientation Program. J. Nurs. Care Qual. 2005, 20, 268–272. [Google Scholar] [CrossRef]
- Cobbett, S.; Snelgrove-Clarke, E. Virtual versus Face-to-Face Clinical Simulation in Relation to Student Knowledge, Anxiety, and Self-Confidence in Maternal-Newborn Nursing: A Randomized Controlled Trial. Nurse Educ. Today 2016, 45, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Cant, R.P.; Cooper, S.J. Simulation-Based Learning in Nurse Education: Systematic Review: Simulation in Nursing. J. Adv. Nurs. 2010, 66, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J. Development and Application of Scenario-Based Admission Management VR Contents for Nursing Students. J. Korea Soc. Comput. Inf. 2021, 26, 209–216. [Google Scholar]
- Hyun, S.J.; Lee, Y.J. Clinical Competence, Confidence, Presence, and Learning Immersion: Analyzing Nursing Students’ Learning Experiences in Virtual Reality Simulation Transfusion Education. J. Healthc. Simul. 2020, 4, 42–51. [Google Scholar]
| Stage | Contents | Time (Min) | |
|---|---|---|---|
| Stage 1. Pre-briefing | Preparation | Lecture on infection control guidelines | 20 |
| Orientation | Presentation of the scenarios | ||
| VR-use-related demonstrations and precautions | |||
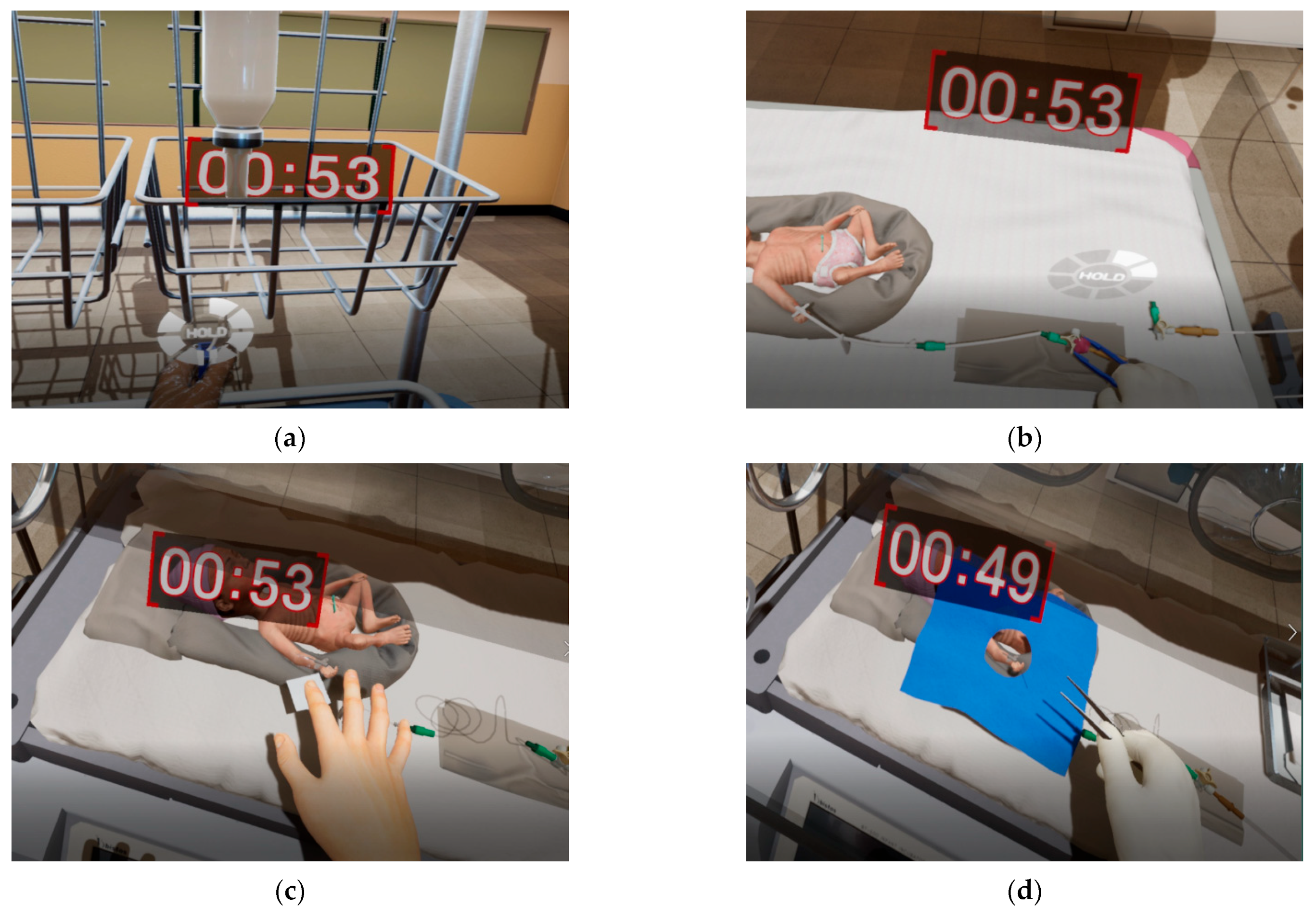
| Stage 2. VR Simulation | Scenario 1. Infection-prone intralipid infusion A high-risk newborn should be infused with intralipid for nutrition supply. The newborn has a PICC in the right arm and is currently connected to total parenteral nutrition. The user should additionally administer intralipid through a three-way catheter. The prescription infusion rate is 1 cc/h every 12 h. | 15 | |
| Scenario 2. Insertion site care of a preterm infant with a PICC line The injection site dressing appears loose, and a slight skin flare is observed in a 700 g premature newborn receiving intravenous nutrition through a PICC line. To prevent infection, aseptic techniques must be strictly followed when changing the dressing. | 15 | ||
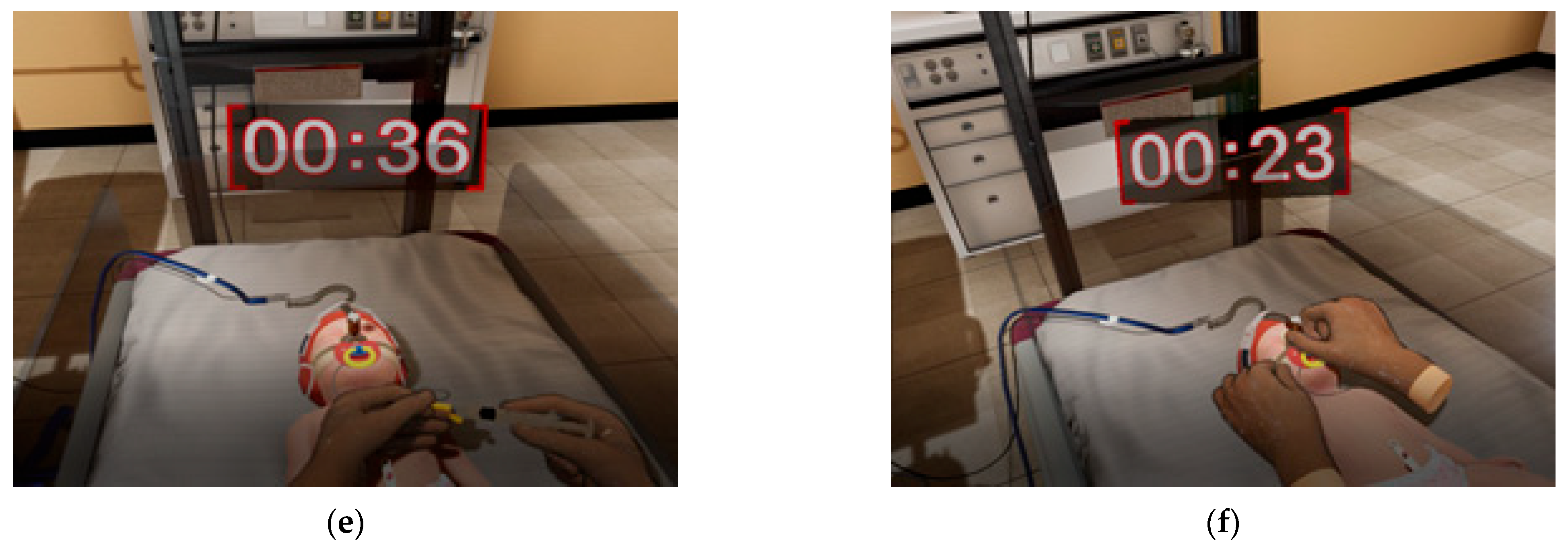
| Scenario 3. Care of a newborn on NCPAP A 2700 g high-risk newborn is under respiratory support with NCPAP. The user must perform routine checks on the proper functioning of the respiratory equipment, humidification temperature, skin condition around the nasal mask, and gastroesophageal reflux. (NCPAP setting: FiO2 0.4, Pressure 5 cmH2O, Flow 8 L/min, Humidifier: 37 °C) | 10 | ||
| Stage 3. Debriefing |
| 20 | |
| Total | 80 | ||
| Characteristic | Category | Total (%) | Group | χ2/t/Z † | p | |
|---|---|---|---|---|---|---|
| Control Group (n = 20) | Experimental Group (n = 20) | |||||
| Educational level | 3-year college | 13 (32.5) | 11 (55.0) | 2 (10.0) | 9.23 | 0.002 ** |
| 4-year college | 27 (67.5) | 9 (45.0) | 18 (90.0) | |||
| Infection control training | Yes | 25 (62.5) | 12 (60.0) | 13 (65.0) | 0.11 | 0.744 |
| No | 15 (37.5) | 8 (40.0) | 7 (35.0) | |||
| VR experience * | Yes | 1 (2.5) | - | 1 (5.0) | 1.000 | |
| No | 39 (97.5) | 20 (100.0) | 19 (95.0) | |||
| Infection control knowledge | Basic infection control | 9.60 ± 0.78 | 9.35 ± 0.99 | 9.85 ± 0.37 | −1.89 | 0.142 |
| Invasive procedure and equipment management | 4.65 ± 0.66 | 4.65 ± 0.59 | 4.65 ± 0.75 | −0.31 | 0.820 | |
| High-risk medication management | 7.70 ± 0.52 | 7.70 ± 0.47 | 7.70 ± 0.57 | −0.24 | 0.862 | |
| Total | 21.95 ± 1.15 | 21.70 ± 1.34 | 22.20 ± 0.89 | −1.09 | 0.314 | |
| Confidence in infection control | Basic infection control | 3.77 ± 0.25 | 3.61 ± 0.26 | 3.93 ± 0.10 | −4.13 | <0.001 *** |
| Invasive procedure and equipment management | 4.00 ± 0.00 | 4.00 ± 0.00 | 4.00 ± 0.00 | 0.00 | 1.000 | |
| High-risk medication management | 3.91 ± 0.17 | 3.84 ± 0.20 | 3.99 ± 0.06 | −3.12 | 0.013 ** | |
| Total | 3.87 ± 0.16 | 3.77 ± 0.17 | 3.97 ± 0.05 | −4.11 | <0.001 *** | |
| Variable | Category | Group | Pre-Test | Post-Test | Difference between Time | Program Effect |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Z (p) * | Z (p) † | |||
| Infection control knowledge | Basic infection control | Exp. | 9.35 ± 0.49 | 9.95 ± 0.22 | −2.33 (0.020) | −2.00 (0.045 **) |
| Cont. | 9.85 ± 0.39 | 9.85 ± 0.37 | 0.00 (1.000) | |||
| Invasive procedure and equipment management | Exp. | 4.65 ± 0.59 | 5.00 ± 0.00 | −2.33 (0.020) | −0.88 (0.495) | |
| Cont. | 4.65 ± 0.75 | 4.90 ± 0.31 | −1.41 (0.157) | |||
| High-risk medication management | Exp. | 7.70 ± 0.47 | 7.95 ± 0.22 | −1.89 (0.059) | −1.16 (0.327) | |
| Cont. | 7.70 ± 0.57 | 7.75 ± 0.44 | −0.30 (0.763) | |||
| Total | Exp. | 21.70 ± 1.34 | 22.90 ± 0.31 | −2.95 (0.003) | −1.86 (0.063) | |
| Cont. | 22.20 ± 0.89 | 22.50 ± 0.61 | −1.26 (.210) | |||
| Confidence for infection control | Basic infection control | Exp. | 3.61 ± 0.26 | 3.86 ± 0.21 | −2.24 (.015) | −2.95 (0.003 **) |
| Cont. | 3.93 ± 0.10 | 3.95 ± 0.11 | –0.79 (0.430) | |||
| Invasive procedure and equipment management | Exp. | 4.00 ± 0.00 | 3.99 ± 0.06 | −1.00 (0.317) | −0.04 (0.989) | |
| Cont. | 4.00 ± 0.00 | 3.98 ± 0.11 | −1.00 (0.317) | |||
| High-risk medication management | Exp. | 3.84 ± 0.20 | 3.91 ± 0.19 | −1.58 (0.115) | −1.37 (0.277) | |
| Cont. | 3.99 ± 0.06 | 4.00 ± 0.00 | −1.00 (0.317) | |||
| Total | Exp. | 3.77 ± 0.17 | 3.90 ± 0.16 | −2.27 (0.024) | −2.92 (0.004 **) | |
| Cont. | 3.97 ± 0.05 | 3.97 ± 0.07 | −0.92 (0.360) |
| Variable | Sub-Item | Range | Mean ± SD |
|---|---|---|---|
| Presence | Spatial involvement | 1–5 | 4.44 ± 0.45 |
| Temporal involvement | 1–5 | 4.08 ± 0.62 | |
| Dynamic immersion | 1–5 | 4.62 ± 0.35 | |
| Realistic immersion | 1–5 | 4.33 ± 0.46 | |
| Total | 4.39 ± 0.36 | ||
| Empathy | 1–5 | 4.33 ± 0.75 | |
| Program satisfaction | 1. I think this program will help me to work as a neonatal intensive care unit nurse | 1–5 | 4.90 ± 0.31 |
| 2. I would recommend this program to other nurses | 1–5 | 4.90 ± 0.31 | |
| 3. I think this education program is necessary for the nurse education curriculum | 1–5 | 4.90 ± 0.31 | |
| Total | 1–5 | 4.90 ± 0.31 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ryu, J.; Yu, M. Virtual Reality Simulation for Advanced Infection Control Education in Neonatal Intensive Care Units: Focusing on the Prevention of Central Line-Associated Bloodstream Infections and Ventilator-Associated Infections. Healthcare 2023, 11, 2296. https://doi.org/10.3390/healthcare11162296
Ryu J, Yu M. Virtual Reality Simulation for Advanced Infection Control Education in Neonatal Intensive Care Units: Focusing on the Prevention of Central Line-Associated Bloodstream Infections and Ventilator-Associated Infections. Healthcare. 2023; 11(16):2296. https://doi.org/10.3390/healthcare11162296
Chicago/Turabian StyleRyu, Jimin, and Mi Yu. 2023. "Virtual Reality Simulation for Advanced Infection Control Education in Neonatal Intensive Care Units: Focusing on the Prevention of Central Line-Associated Bloodstream Infections and Ventilator-Associated Infections" Healthcare 11, no. 16: 2296. https://doi.org/10.3390/healthcare11162296
APA StyleRyu, J., & Yu, M. (2023). Virtual Reality Simulation for Advanced Infection Control Education in Neonatal Intensive Care Units: Focusing on the Prevention of Central Line-Associated Bloodstream Infections and Ventilator-Associated Infections. Healthcare, 11(16), 2296. https://doi.org/10.3390/healthcare11162296






