Professional Accountability of Caring for Patients with COVID-19: A Phenomenographic Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Rationale and Aims
2.2. Recruitment, Criteria, and Sampling
2.3. Data Analysis
2.4. Ethical Considerations
3. Results
3.1. Characteristics of Participants
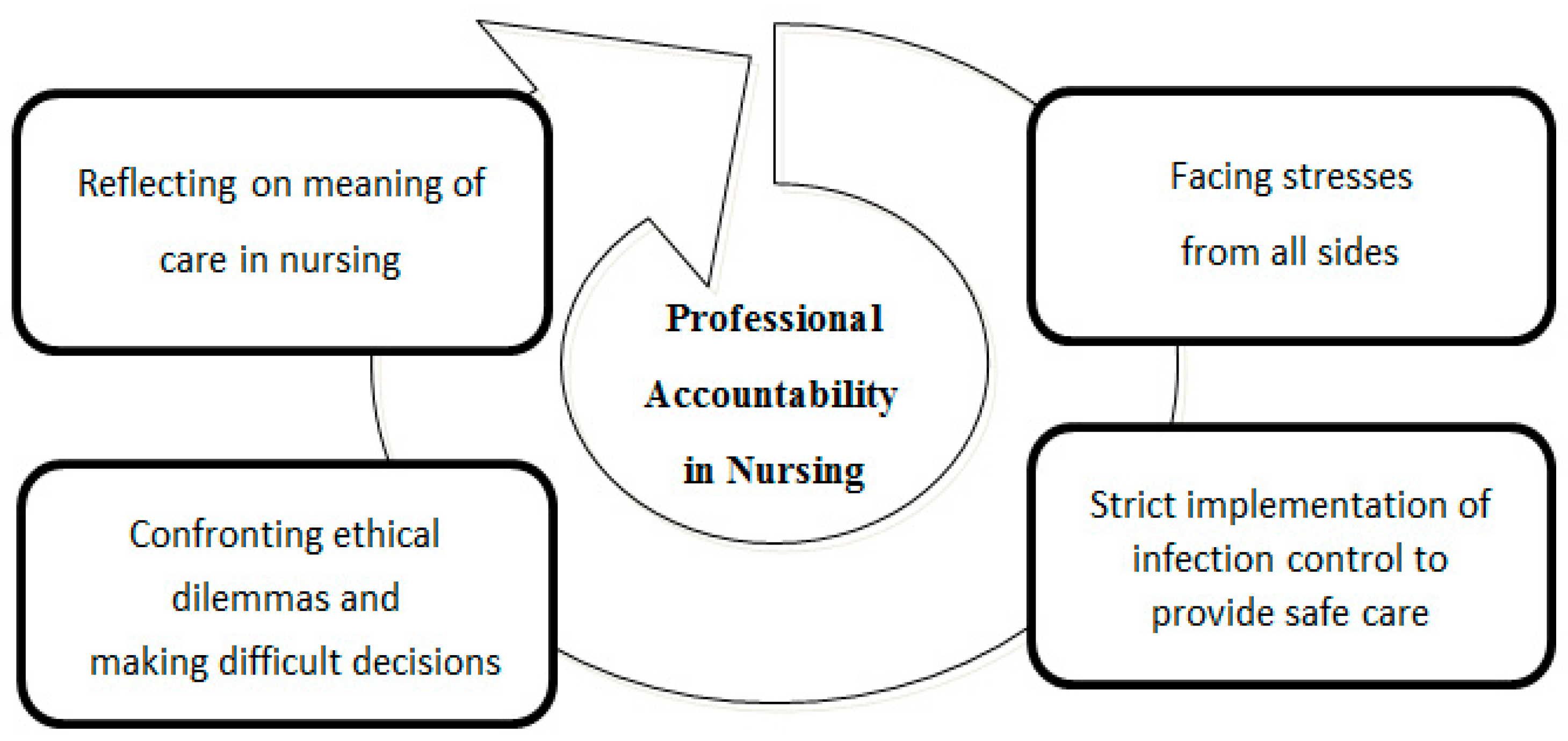
3.2. Categories of Desctiption
3.2.1. Categories of Description One: Caring for Patients with COVID-19 as Facing Stresses from All Sides
RN5: I was extremely scared. I’ve never met a disease like this before, and I’ve scrubbed my hands to the point that they crack… and was soaked in sweat from head to toe after the shift without realizing this happened.
P12: …made sure I’d put on the protective clothing correctly at work. In the summer, I was soaked in sweat from head to toes after my shift. Perhaps because I was so scared about contracting the disease, I didn’t realize I was all wet.
RN18: I had nightmares for days when I first started caring for them, and I’ve had dreams about getting infected myself.
RN4: I heard from my mother that the neighbors stay away (from my family) like they are avoiding the plague. All I could do was console my parents. I feel so guilty about the potential COVID-19 exposure risk to my family.
RN7: For some time, I’ve intentionally made up reasons for not going home because I was worried about the consequences of bringing the virus into my home and infecting my kids.
RN16: I had nightmares for days when I first started caring for them, and I’ve had dreams about getting infected myself (smiling wryly).
3.2.2. Categories of Description Two: Caring for Patients with COVID-19 as Strict Infection Control to Provide Safe Care
RN15: …hospitals quickly offered online lessons about infection control strategy. No one liked online learning, but we all participated and discussed the lessons with each other whenever there was a problem. We just wanted to practice well infection control intervention in the care process, as this ensured not only the safety of patients but everyone else.
RN6: I was assigned to work here (in the negative pressure isolation unit) from the surgical ward. I saw that everyone had put on the PPE (personal protective equipment) properly without any complaints, even when our hands cracked or we had deep marks on our faces made by N95 masks. This was done so that the patients and colleagues were not exposed to the risk of being infected.
3.2.3. Categories of Description Three: Caring for Patients with COVID-19 as Confronting Ethical Dilemmas and Making Difficult Decisions
RN4: I’ve come across two beds (patients) that needed assistance at the same time, and I had to decide which one to go to first. They were really difficult decisions to make. I had to “gear up” and get into the negative pressure room within such a short time.
RN15: It stay imprinted in my mind because she was the index patient and transmitted the disease to several of her family members. At the final moment when she was in critical condition, her family was forbidden by law from being present and said their final goodbyes via the screen. And then, her body had to be cremated within the mandatory time.
RN21: I’ve never seen patients deteriorate so quickly in such a short time… and I have to immediately decide what I need to do. When their family members were also in isolation, crying over the phone or through the screen and asking us what to do, we were also grieving internally despite responding to them calmly. They couldn’t be with their dying loved ones.
3.2.4. Categories of Description Four: Caring for Patients with COVID-19 as Reflecting on the Meaning of Nursing
RN17: An older (sick) man waited while I put on PPE (personal protective equipment) before going to the isolation room. He only wanted to use the bathroom and needed help. He was in tears and said “thank you” many times… he told me he didn’t want to soil the bed sheet. I was so moved and understood the meaning of caring.
RN11: …always made sure that everything was well prepared before going into the negative pressure room so that I could tend to all the patient needed. It takes a long time putting on the PPE and I couldn’t keep the patient in pain, waiting for so long… I was the only person who could help (him).
3.3. The Outcome Space: Professional Accountability in Nursing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. The Interview Guide
- What was work like today?
- Could you describe your working situation when the COVID-19 pandemic started?
- Did you care for any patients with COVID-19 today?
- Could you provide some examples of how you care for patients with COVID-19?
- Could you talk about your feelings or thoughts while caring for the patients with COVID-19?
- Have you had any difficulty while caring for the patients with COVID-19?
- Do you have any suggestions for caring for the patients with COVID-19?
- Is there anything you would like to add?
References
- Catton, H. Global challenges in health and healthcare for nurses and midwives everywhere. Int. Nurs. Rev. 2020, 67, 4–6. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2022. Available online: https://covid19.who.int/ (accessed on 3 August 2022).
- Chen, W.; Huang, Y. To protect health care workers better, to save more lives with COVID-19. Anesth. Analg. 2020, 131, 97–101. [Google Scholar] [CrossRef]
- Luo, Y.; Feng, X.; Wang, D.; Qiao, X.; Xiao, X.; Jia, S.; Zheng, M.; Reinhardt, J.D. Experience of clinical nurses engaged in caring for patients with COVID-19: A qualitative systematic review and meta-synthesis. J. Clin. Nurs. 2023, 32, 5258–5273. [Google Scholar] [CrossRef] [PubMed]
- Shahoei, R.; Nemati, S.M.; Valiee, S. Exploring the experience of nurses in providing care to patients with COVID-19: A qualitative study. J. Nurs. Res. 2022, 30, e217. [Google Scholar] [CrossRef] [PubMed]
- Çınar, D.; Akça, N.K.; Bahçeli, P.Z.; Bağ, Y. Perceived stress and affecting factors related to COVID-19 pandemic of emergency nurses in Turkey. Nurs. Manag. 2021, 29, 1916–1923. [Google Scholar] [CrossRef]
- Moore, C.; Kolencik, J. Acute depression, extreme anxiety, and prolonged stress among COVID-19 frontline healthcare workers. Psychosociol. Issues Hum. Resour. Manag. 2020, 8, 55–60. [Google Scholar] [CrossRef]
- Bogoch, I.I.; Watts, A.; Thomas-Bachli, A.; Huber, C.; Kraemer, M.U.G.; Khan, K. Pneumonia of unknown aetiology in Wuhan, China: Potential for international spread via commercial air travel. Travel Med. 2020, 27, taaa008. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Gómez-Ochoa, S.A.; Franco, O.H.; Rojas, L.Z.; Raguindin, P.F.; Roa-Díaz, Z.M.; Wyssmann, B.M.; Guevara, S.L.R.; Echeverría, L.E.; Glisic, M.; Muka, T. COVID-19 in health-care workers: A living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am. J. Epidemiol. 2021, 190, 161–175. [Google Scholar] [CrossRef]
- Mukhtar, S. Psychological health during the coronavirus disease 2019 pandemic outbreak. Int. J. Soc. Psychiatry 2020, 66, 512–516. [Google Scholar] [CrossRef]
- Shaw, S.C.K. Hopelessness, helplessness and resilience: The importance of safeguarding our trainees’ mental wellbeing during the COVID-19 pandemic. Nurse Educ. Pract. 2020, 44, 102780. [Google Scholar] [CrossRef] [PubMed]
- Doom, D.J.; Han, M.A.; Park, J.; Ryu, S.Y. Post-traumatic stress and related factors among hospital nurses during the COVID-19 Outbreak in Korea. Psychiatr. Q. 2021, 92, 1381–1391. [Google Scholar] [CrossRef]
- Dos Santos, M.A.; Pereira, F.H.; DESouza Caliari, J.; Oliveira, H.C.; Ceolim, M.F.; Andrechuk, C.R.S. Sleep and Professional Burnout in Nurses, Nursing Technicians, and Nursing Assistants During the COVID-19 Pandemic. J. Nurs. Res. 2022, 30, e218. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Nazari, N.; Sadeghi, M.; Samusenkov, V.; Aligholipour, A. Retraction note: Factors associated with insomnia among frontline nurses during COVID-19: A cross-sectional survey study. BMC Psychiatry 2022, 22, 498. [Google Scholar] [CrossRef]
- Roberts, N.J.; McAloney-Kocaman, K.; Lippiett, K.; Ray, E.; Welch, L.; Kelly, C. Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respir. Med. 2021, 176, 106219. [Google Scholar] [CrossRef]
- Slettmyr, A.; Arman, M.; Andermo, S.; Malmberg, C.; Hällström, Å.; Hugelius, K.; Schandl, A. Intensive care nurses’ lived experience of altruism and sacrifices during the COVID-19 pandemic: A phenomenological study. J. Adv. Nurs. 2023, 79, 244–253. [Google Scholar] [CrossRef]
- Trachtenberg, S.; Tehan, T.; Shostak, S.; Snydeman, C.; Lewis, M.; Romain, F.; Cadge, W.; McAuley, M.E.; Matthews, C.; Lux, L.; et al. Experiences of moral distress in a COVID-19 intensive care unit: A qualitative study of nurses and respiratory therapists in the United States. Nurs. Inq. 2023, 30, e12500. [Google Scholar] [CrossRef]
- Pozo-Herce, P.D.; Garrido-García, R.; Santolalla-Arnedo, I.; Gea-Caballero, V.; García-Molina, P.; de Viñaspre-Hernández, R.R.; Rodríguez-Velasco, F.J.; Juárez-Vela, R. Psychological impact on the nursing professionals of the Rioja Health Service (Spain) due to the SARS-CoV-2 Virus. Int. J. Environ. Res. Public Health 2021, 18, 580. [Google Scholar] [CrossRef]
- Lee, M.C.; Chen, C.H.; Hsieh, P.H.; Ling, C.H.; Yang, C.C.; Chang, Y.C.; Yeh, L.Y.; Hung, H.C.; Yeh, T.F. Psychological impact, coping behaviors, and traumatic stress among healthcare workers during COVID-19 in Taiwan: An early stage experience. PLoS ONE 2022, 17, e0276535. [Google Scholar] [CrossRef]
- Kuo Fang, P.H.; Hsu, H.T.; Su, C.Y.; Chen, C.H.; Yeh, I.J.; Wu, Y.H.; Chen, L.C. Survey on perceived work stress and its influencing factors among hospital staff during the COVID-19 pandemic in Taiwan. Kaohsiung J. Med. Sci. 2020, 36, 944–952. [Google Scholar] [CrossRef]
- Marton, F. Phenomenography—Describing conceptions of the world around us. Instr. Sci. 1981, 10, 177–200. [Google Scholar] [CrossRef]
- Barnard, A.; McCosker, H.; Gerber, R. Phenomenography: A qualitative research approach for exploring understanding in health care. Qual. Health Res. 1999, 9, 212–226. [Google Scholar] [CrossRef] [PubMed]
- Åkerlind, G.S. Academics awareness of their own growth and development—Five dimensions of variation. In Proceedings of the Symposium on Current Issues in Phenomenography, Canberra, Australia, November 2002. [Google Scholar]
- Marton, F. Phenomenography—A research approach to investigating different understandings of reality. J. Thought 1986, 21, 28–49. [Google Scholar]
- Dahlgren, L.O.; Fallsberg, M. Phenomenography as a qualitative approach in social pharmacy research. Res. Soc. Adm. Pharm. 1991, 8, 150–156. [Google Scholar]
- Sjöström, B.; Dahlgren, L.O. Applying phenomenography in nursing research. J. Adv. Nurs. 1996, 40, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Brailas, A. Using drawings in qualitative interviews: An introduction to the practice. Qual. Rep. 2020, 25, 4447–4460. [Google Scholar] [CrossRef]
- Sandberg, J. Are phenomenographic results reliable? High. Educ. Res. Dev. 1997, 16, 203–212. [Google Scholar] [CrossRef]
- Benbenishty, J.; Ashkenazy, S.; Avital, I.L.; Jakobson, L.; Kolpak, O.; Ganz, F.D. Nurses’ perceptions of social rejection, resilience and well-being during COVID-19: A national comparative study. J. Clin. Nurs. 2022, 31, 2189–2197. [Google Scholar] [CrossRef]
- Jung, H.; Jung, S.Y.; Lee, M.H.; Kim, M.S. Assessing the presence of post-traumatic stress and turnover intention among nurses post-Middle East Respiratory Syndrome: The importance of supervisor support. Workplace Health Saf. 2020, 68, 337–345. [Google Scholar] [CrossRef]
- Tsukuda, M.; Kayano, T.; Ito, Y. Experiences of COVID-19-related stigma: A qualitative study on nurses caring for patients with COVID-19. J. Nurs. Res. 2022, 30, e241. [Google Scholar] [CrossRef] [PubMed]
- Widiasih, R.; Emaliyawati, E.; Hendrawati, S.; Susanti, R.D.; Sutini, T.; Sari, C.W.M. Nurses’ actions to protect their families from COVID-19: A descriptive qualitative study. Glob. Qual. Nurs. Res. 2021, 29, 23333936211014851. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.L.; Chen, K.L.; Lee, L.H.; Yang, C.I. Working in a danger zone: A qualitative study of Taiwanese nurses’ work experiences in a negative pressure isolation ward. Am. J. Infect. Control 2016, 44, 809–814. [Google Scholar] [CrossRef] [PubMed]
- Dalky, H.F.; Hamdan-Mansour, A.M.; Amarneh, B.H.; AlAzzam, M.; Yacoub, N.R.; Khalifeh, A.H.; Aldalaykeh, M.; Dalky, A.F. Social discrimination perception of health-care workers and ordinary people toward individuals with COVID-19. Soc. Influ. 2020, 15, 65–79. [Google Scholar] [CrossRef]
- Aldohyan, M.; Al-Rawashdeh, N.; Sakr, F.M.; Rahman, S.; Alfarhan, A.; Salam, M. The perceived effectiveness of MERS-CoV educational programs and knowledge transfer among primary healthcare workers: A across-sectional survey. BMC Infect. Dis. 2019, 19, 273. [Google Scholar] [CrossRef]
- Chersich, M.F.; Gray, G.; Fairlie, L.; Eichbaum, Q.; Mayhew, S.; Allwod, B.; English, R.; Scorgie, F.; Luchters, S.; Simpson, G.; et al. COVID-19 in Africa: Care and protection for frontline healthcare workers. Glob. Health 2020, 16, 46. [Google Scholar] [CrossRef]
- Carnesten, H.; Wiklund Gustin, L.; Skoglund, K.; von Heideken Wågert, P. Caring through barriers-Newly graduated registered nurses’ lived experiences in emergency departments during the COVID-19 pandemic. J. Adv. Nurs. 2023, 79, 2269–2279. [Google Scholar] [CrossRef]
- Firouzkouhi, M.; Alimohammadi, N.; Kako, M.; Abdollahimohammad, A.; Bagheri, G.; Nouraie, M. Ethical challenges of nurses related COVID-19 pandemic in inpatient wards: An integrative review. Ethics Med. Public Health 2021, 18, 100669. [Google Scholar] [CrossRef]
- Gebreheat, G.; Teame, H. Ethical challenges of nurses in COVID-19 pandemic: An integrative review. J. Multidiscip. Healthc. 2021, 14, 1029–1035. [Google Scholar] [CrossRef]
- Chiang, H.H.; Chen, M.B.; Sue, I.L. Ethical dilemmas in Caring for patient with SARS. J. Nurs. 2006, 53, 28–34. (In Chinese) [Google Scholar] [CrossRef]
- Chesterton, L.; Tetley, J.; Cox, N.; Jack, K. A hermeneutical study of professional accountability in nursing. J. Clin. Nurs. 2021, 30, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Royal College of Nursing. Accountability and Delegation. Available online: https://www.rcn.org.uk/professional-development/accountability-and-delegation (accessed on 16 April 2022).


| Variables | n (%) | Mean ± SD | Range |
| Gender | |||
| Male | 2 (5.88) | ||
| Female | 32 (94.12) | ||
| Age | 30 ± 4.83 | 22–42 | |
| Education | |||
| Associate diploma | 6 (17.65) | ||
| Bachelor’s degree | 28 (82.35) | ||
| Department (site of recruitment) | |||
| Medical | 18 (52.94) | ||
| ICU | 8 (23.53) | ||
| ER | 8 (23.53) | ||
| Nursing experience (years) | 7.61 ± 4.60 | 1–21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, L.-C.; Yeh, S.-L.; Lee, H.-L.; Lin, C.-C.; Goopy, S.; Han, C.-Y. Professional Accountability of Caring for Patients with COVID-19: A Phenomenographic Study. Healthcare 2023, 11, 2269. https://doi.org/10.3390/healthcare11162269
Chen L-C, Yeh S-L, Lee H-L, Lin C-C, Goopy S, Han C-Y. Professional Accountability of Caring for Patients with COVID-19: A Phenomenographic Study. Healthcare. 2023; 11(16):2269. https://doi.org/10.3390/healthcare11162269
Chicago/Turabian StyleChen, Li-Chin, Shu-Ling Yeh, Hui-Ling Lee, Chun-Chih Lin, Suzanne Goopy, and Chin-Yen Han. 2023. "Professional Accountability of Caring for Patients with COVID-19: A Phenomenographic Study" Healthcare 11, no. 16: 2269. https://doi.org/10.3390/healthcare11162269
APA StyleChen, L.-C., Yeh, S.-L., Lee, H.-L., Lin, C.-C., Goopy, S., & Han, C.-Y. (2023). Professional Accountability of Caring for Patients with COVID-19: A Phenomenographic Study. Healthcare, 11(16), 2269. https://doi.org/10.3390/healthcare11162269






