Association of Sociodemographic Factors with Physical Activity and Sleep Quality in Arab and Non-Arab Individuals of Both Sexes during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Study Variables
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aguilar-Farias, N.; Toledo-Vargas, M.; Miranda-Marquez, S.; Cortinez-O’Ryan, A.; Cristi-Montero, C.; Rodriguez-Rodriguez, F.; Martino-Fuentealba, P.; Okely, A.D.; del Pozo Cruz, B. Sociodemographic Predictors of Changes in Physical Activity, Screen Time, and Sleep among Toddlers and Preschoolers in Chile during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 18, 176. [Google Scholar] [CrossRef] [PubMed]
- Papageorge, N.W.; Zahn, M.V.; Belot, M.; van den Broek-Altenburg, E.; Choi, S.; Jamison, J.C.; Tripodi, E. Socio-Demographic Factors Associated with Self-Protecting Behavior during the Covid-19 Pandemic. J. Popul. Econ. 2021, 34, 691–738. [Google Scholar] [CrossRef]
- Da Silva, J.M.; Verlengia, R.; de Oliveira, J.J.; Ribeiro, A.G.S.V.; Barbosa, C.G.R.; Stotzer, U.S.; Crisp, A.H. Associations between Sociodemographic Factors and Physical Activity and Sedentary Behaviors in Adults with Chronic Diseases during COVID-19 Pandemic. Sports Med. Health Sci. 2020, 2, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Narici, M.; De Vito, G.; Franchi, M.; Paoli, A.; Moro, T.; Marcolin, G.; Grassi, B.; Baldassarre, G.; Zuccarelli, L.; Biolo, G.; et al. Impact of Sedentarism Due to the COVID-19 Home Confinement on Neuromuscular, Cardiovascular and Metabolic Health: Physiological and Pathophysiological Implications and Recommendations for Physical and Nutritional Countermeasures. Eur. J. Sports Sci. 2021, 21, 614–635. [Google Scholar] [CrossRef]
- Peçanha, T.; Goessler, K.F.; Roschel, H.; Gualano, B. Social Isolation during the COVID-19 Pandemic Can Increase Physical Inactivity and the Global Burden of Cardiovascular Disease. Am. J. Physiol.-Heart Circ. Physiol. 2020, 318, H1441–H1446. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451. [Google Scholar] [CrossRef]
- Yammine, K. The Prevalence of Physical Activity among the Young Population of UAE: A Meta-Analysis. Perspect. Public. Health 2017, 137, 275–280. [Google Scholar] [CrossRef]
- Dalibalta, S.; Majdalawieh, A.; Yousef, S.; Gusbi, M.; Wilson, J.J.; Tully, M.A.; Davison, G. Objectively Quantified Physical Activity and Sedentary Behaviour in a Young UAE Population. BMJ Open Sports Exerc. Med. 2021, 7, e000957. [Google Scholar] [CrossRef] [PubMed]
- Radwan, H.; Al Kitbi, M.; Hasan, H.; Al Hilali, M.; Abbas, N.; Hamadeh, R.; Saif, E.R.; Naja, F. Indirect Health Effects of COVID-19: Unhealthy Lifestyle Behaviors during the Lockdown in the United Arab Emirates. Int. J. Environ. Res. Public Health 2021, 18, 1964. [Google Scholar] [CrossRef]
- Shahidi, S.H.; Stewart Williams, J.; Hassani, F. Physical Activity during COVID-19 Quarantine. Acta Paediatr. 2020, 109, 2147–2148. [Google Scholar] [CrossRef]
- Abate Daga, F.; Agostino, S.; Peretti, S.; Beratto, L. The Impact of Physical Activity Rate on Subjective Well-Being among North-Western Italian Population during COVID-19 Nationwide Lockdown. J. Sports Med. Phys. Fit. 2022, 62, 1–25. [Google Scholar] [CrossRef]
- Trabelsi, K.; Ammar, A.; Masmoudi, L.; Boukhris, O.; Chtourou, H.; Bouaziz, B.; Brach, M.; Bentlage, E.; How, D.; Ahmed, M.; et al. Globally Altered Sleep Patterns and Physical Activity Levels by Confinement in 5056 Individuals: ECLB COVID-19 International Online Survey. Biol. Sport 2021, 38, 495–506. [Google Scholar] [CrossRef] [PubMed]
- Srivastav, A.K.; Sharma, N.; Samuel, A.J. Impact of Coronavirus Disease-19 (COVID-19) Lockdown on Physical Activity and Energy Expenditure among Physiotherapy Professionals and Students Using Web-Based Open E-Survey Sent through WhatsApp, Facebook and Instagram Messengers. Clin. Epidemiol. Glob. Health 2021, 9, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Trabelsi, K.; Ammar, A.; Masmoudi, L.; Boukhris, O.; Chtourou, H.; Bouaziz, B.; Brach, M.; Bentlage, E.; How, D.; Ahmed, M.; et al. Sleep Quality and Physical Activity as Predictors of Mental Wellbeing Variance in Older Adults during COVID-19 Lockdown: ECLB COVID-19 International Online Survey. Int. J. Environ. Res. Public Health 2021, 18, 4329. [Google Scholar] [CrossRef]
- Ferrara, M.; Langiano, E.; Falese, L.; Diotaiuti, P.; Cortis, C.; De Vito, E. Changes in Physical Activity Levels and Eating Behaviours during the COVID-19 Pandemic: Sociodemographic Analysis in University Students. Int. J. Environ. Res. Public Health 2022, 19, 5550. [Google Scholar] [CrossRef]
- Orlandi, M.; Rosselli, M.; Pellegrino, A.; Boddi, M.; Stefani, L.; Toncelli, L.; Modesti, P.A. Gender Differences in the Impact on Physical Activity and Lifestyle in Italy during the Lockdown, Due to the COVID-19 Pandemic. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2173–2180. [Google Scholar] [CrossRef]
- Wang, F.; Boros, S. The Effect of Physical Activity on Sleep Quality: A Systematic Review. Eur. J. Physiother. 2021, 23, 11–18. [Google Scholar] [CrossRef]
- Kredlow, M.A.; Capozzoli, M.C.; Hearon, B.A.; Calkins, A.W.; Otto, M.W. The Effects of Physical Activity on Sleep: A Meta-Analytic Review. J. Behav. Med. 2015, 38, 427–449. [Google Scholar] [CrossRef]
- Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelöv, S.; Riemann, D. Dealing with Sleep Problems during Home Confinement Due to the COVID-19 Outbreak: Practical Recommendations from a Task Force of the European CBT-I Academy. J. Sleep. Res. 2020, 29, e13052. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Adams Hillard, P.J.; Katz, E.S.; et al. National Sleep Foundation’s Updated Sleep Duration Recommendations: Final Report. Sleep. Health 2015, 1, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Dutil, C.; Featherstone, R.; Ross, R.; Giangregorio, L.; Saunders, T.J.; Janssen, I.; Poitras, V.J.; Kho, M.E.; Ross-White, A.; et al. Sleep Duration and Health in Adults: An Overview of Systematic Reviews. Appl. Physiol. Nutr. Metab. 2020, 45 (Suppl. 2), S218–S231. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Wong, S.L.; Michaud, I. Duration and Quality of Sleep among Canadians Aged 18 to 79. Health Rep. 2017, 28, 28. [Google Scholar] [PubMed]
- Gadie, A.; Shafto, M.; Leng, Y.; Kievit, R.A. How Are Age-Related Differences in Sleep Quality Associated with Health Outcomes? An Epidemiological Investigation in a UK Cohort of 2406 Adults. BMJ Open 2017, 7, e014920. [Google Scholar] [CrossRef] [PubMed]
- Štefan, L.; Sporiš, G.; Krističević, T.; Knjaz, D. Associations between Sleep Quality and Its Domains and Insufficient Physical Activity in a Large Sample of Croatian Young Adults: A Cross-Sectional Study. BMJ Open 2018, 8, e021902. [Google Scholar] [CrossRef]
- Spira, A.P.; Chen-Edinboro, L.P.; Wu, M.N.; Yaffe, K. Impact of Sleep on the Risk of Cognitive Decline and Dementia. Curr. Opin. Psychiatry 2014, 27, 478–483. [Google Scholar] [CrossRef]
- Targa, A.D.S.; Benítez, I.D.; Moncusí-Moix, A.; Arguimbau, M.; de Batlle, J.; Dalmases, M.; Barbé, F. Decrease in Sleep Quality during COVID-19 Outbreak. Sleep. Breath. 2021, 25, 1055–1061. [Google Scholar] [CrossRef]
- Bigalke, J.A.; Greenlund, I.M.; Carter, J.R. Sex Differences in Self-Report Anxiety and Sleep Quality during COVID-19 Stay-at-Home Orders. Biol. Sex. Differ. 2020, 11, 56. [Google Scholar] [CrossRef]
- Ono, B.H.V.S.; Souza, J.C. Sleep and Immunity in Times of COVID-19. Rev. Assoc. Med. Bras. 2020, 66 (Suppl. 2), 143–147. [Google Scholar] [CrossRef]
- Yousfi, N.; Bragazzi, N.L.; Briki, W.; Zmijewski, P.; Chamari, K. The COVID-19 Pandemic: How to Maintain a Healthy Immune System during the Lockdown—A Multidisciplinary Approach with Special Focus on Athletes. Biol. Sport 2020, 37, 211–216. [Google Scholar] [CrossRef]
- Kahan, D. Adult Physical Inactivity Prevalence in the Muslim World: Analysis of 38 Countries. Prev. Med. Rep. 2015, 2, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Henry, C.J.K.; Lightowler, H.J.; Al-Hourani, H.M. Physical Activity and Levels of Inactivity in Adolescent Females Ages 11–16 Years in the United Arab Emirates. Am. J. Hum. Biol. 2004, 16, 346–353. [Google Scholar] [CrossRef]
- Berger, G.; Peerson, A. Giving Young Emirati Women a Voice: Participatory Action Research on Physical Activity. Health Place 2009, 15, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Fatima, Y.; Doi, S.A.R.; Najman, J.M.; Mamun, A.A. Exploring Gender Difference in Sleep Quality of Young Adults: Findings from a Large Population Study. Clin. Med. Res. 2016, 14, 138–144. [Google Scholar] [CrossRef]
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender Differences in Depression in Representative National Samples: Meta-Analyses of Diagnoses and Symptoms. Psychol. Bull. 2017, 143, 783–822. [Google Scholar] [CrossRef] [PubMed]
- Dubinina, E.; Korostovtseva, L.S.; Rotar, O.; Amelina, V.; Boyarinova, M.; Bochkarev, M.; Shashkova, T.; Baranova, E.; Libis, R.; Duplyakov, D.; et al. Physical Activity Is Associated With Sleep Quality: Results of the ESSE-RF Epidemiological Study. Front. Psychol. 2021, 12, 705212. [Google Scholar] [CrossRef]
- Tomioka, K.; Iwamoto, J.; Saeki, K.; Okamoto, N. Reliability and Validity of the International Physical Activity Questionnaire (IPAQ) in Elderly Adults: The Fujiwara-Kyo Study. J. Epidemiol. 2011, 21, 459–465. [Google Scholar] [CrossRef]
- Backhaus, J.; Junghanns, K.; Broocks, A.; Riemann, D.; Hohagen, F. Test–Retest Reliability and Validity of the Pittsburgh Sleep Quality Index in Primary Insomnia. J. Psychosom. Res. 2002, 53, 737–740. [Google Scholar] [CrossRef]
- Sylvia, L.G.; Bernstein, E.E.; Hubbard, J.L.; Keating, L.; Anderson, E.J. Practical Guide to Measuring Physical Activity. J. Acad. Nutr. Diet. 2014, 114, 199–208. [Google Scholar] [CrossRef]
- National Institutes of Health, National Heart, Lung, and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report; National Institutes of Health: Bethesda, MD, USA, 1998.
- Craig, C.L.; Marshall, A.L.; Sjstrm, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Sember, V.; Meh, K.; Sorić, M.; Starc, G.; Rocha, P.; Jurak, G. Validity and Reliability of International Physical Activity Questionnaires for Adults across EU Countries: Systematic Review and Meta Analysis. Int. J. Environ. Res. Public Health 2020, 17, 7161. [Google Scholar] [CrossRef]
- Carpenter, J.S.; Andrykowski, M.A. Psychometric Evaluation of the Pittsburgh Sleep Quality Index. J. Psychosom. Res. 1998, 45, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Mielke, G.I.; da Silva, I.C.M.; Kolbe-Alexander, T.L.; Brown, W.J. Shifting the Physical Inactivity Curve Worldwide by Closing the Gender Gap. Sports Med. 2018, 48, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Nienhuis, C.P.; Lesser, I.A. The Impact of COVID-19 on Women’s Physical Activity Behavior and Mental Well-Being. Int. J. Environ. Res. Public Health 2020, 17, 9036. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, T.T.; Al-Thani, A.A.; Benjamin, K.; Al-Khater, A.H.; Fung, T.S.; Ahmedna, M.; Welch, A. Arab Female and Male Perceptions of Factors Facilitating and Inhibiting Their Physical Activity: Findings from a Qualitative Study in the Middle East. PLoS ONE 2018, 13, e0199336. [Google Scholar] [CrossRef]
- Elshahat, S.; Newbold, K.B. Physical Activity Participation among Arab Immigrants and Refugees in Western Societies: A Scoping Review. Prev. Med. Rep. 2021, 22, 101365. [Google Scholar] [CrossRef]
- Al Zahmi, F.; Habuza, T.; Awawdeh, R.; Elshekhali, H.; Lee, M.; Salamin, N.; Sajid, R.; Kiran, D.; Nihalani, S.; Smetanina, D.; et al. Ethnicity-Specific Features of COVID-19 Among Arabs, Africans, South Asians, East Asians, and Caucasians in the United Arab Emirates. Front. Cell. Infect. Microbiol. 2022, 11, 773141. [Google Scholar] [CrossRef]
- Grumbach, P.; Opel, N.; Martin, S.; Meinert, S.; Leehr, E.J.; Redlich, R.; Enneking, V.; Goltermann, J.; Baune, B.T.; Dannlowski, U.; et al. Sleep Duration Is Associated with White Matter Microstructure and Cognitive Performance in Healthy Adults. Hum. Brain Mapp. 2020, 41, 4397–4405. [Google Scholar] [CrossRef]
- Yaffe, K.; Nasrallah, I.; Hoang, T.D.; Lauderdale, D.S.; Knutson, K.L.; Carnethon, M.R.; Launer, L.J.; Lewis, C.E.; Sidney, S. Sleep Duration and White Matter Quality in Middle-Aged Adults. Sleep 2016, 39, 1743–1747. [Google Scholar] [CrossRef]
- Li, C.; Schreiber, J.; Bittner, N.; Li, S.; Huang, R.; Moebus, S.; Bauer, A.; Caspers, S.; Elmenhorst, D. White Matter Microstructure Underlies the Effects of Sleep Quality and Life Stress on Depression Symptomatology in Older Adults. Front. Aging Neurosci. 2020, 12, 578037. [Google Scholar] [CrossRef]
- Khalsa, S.; Hale, J.R.; Goldstone, A.; Wilson, R.S.; Mayhew, S.D.; Bagary, M.; Bagshaw, A.P. Habitual Sleep Durations and Subjective Sleep Quality Predict White Matter Differences in the Human Brain. Neurobiol. Sleep. Circadian Rhythm. 2017, 3, 17–25. [Google Scholar] [CrossRef]
- Sexton, C.E.; Zsoldos, E.; Filippini, N.; Griffanti, L.; Winkler, A.; Mahmood, A.; Allan, C.L.; Topiwala, A.; Kyle, S.D.; Spiegelhalder, K.; et al. Associations between Self-Reported Sleep Quality and White Matter in Community-Dwelling Older Adults: A Prospective Cohort Study. Hum. Brain Mapp. 2017, 38, 5465–5473. [Google Scholar] [CrossRef]
- Corbo, I.; Forte, G.; Favieri, F.; Casagrande, M. Poor Sleep Quality in Aging: The Association with Mental Health. Int. J. Environ. Res. Public Health 2023, 20, 1661. [Google Scholar] [CrossRef] [PubMed]
- Dinler, E.; Badat, T.; Kocamaz, D.; Yakut, Y. Evaluation of the Physical Activity, Sleep Quality, Depression, and Life Satisfaction of University Students During the COVID-19. Int. J. Disabil. Sports Health Sci. 2020, 3, 128–139. [Google Scholar] [CrossRef]
- Mahfouz, M.S.; Ali, S.A.; Bahari, A.Y.; Ajeebi, R.E.; Sabei, H.J.; Somaily, S.Y.; Madkhali, Y.A.; Hrooby, R.H.; Shook, R.N. Association Between Sleep Quality and Physical Activity in Saudi Arabian University Students. Nat. Sci. Sleep 2020, 12, 775–782. [Google Scholar] [CrossRef]
- Romdhani, M.; Rae, D.E.; Nédélec, M.; Ammar, A.; Chtourou, H.; Al Horani, R.; Ben Saad, H.; Bragazzi, N.; Dönmez, G.; Driss, T.; et al. COVID-19 Lockdowns: A Worldwide Survey of Circadian Rhythms and Sleep Quality in 3911 Athletes from 49 Countries, with Data-Driven Recommendations. Sports Med. 2022, 52, 1433–1448. [Google Scholar] [CrossRef]
- Hyun, S.; Hahm, H.C.; Wong, G.T.F.; Zhang, E.; Liu, C.H. Psychological Correlates of Poor Sleep Quality among U.S. Young Adults during the COVID-19 Pandemic. Sleep. Med. 2021, 78, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Sañudo, B.; Fennell, C.; Sánchez-Oliver, A.J. Objectively-Assessed Physical Activity, Sedentary Behavior, Smartphone Use, and Sleep Patterns Pre- and during-COVID-19 Quarantine in Young Adults from Spain. Sustainability 2020, 12, 5890. [Google Scholar] [CrossRef]
- Bentlage, E.; Ammar, A.; How, D.; Ahmed, M.; Trabelsi, K.; Chtourou, H.; Brach, M. Practical Recommendations for Maintaining Active Lifestyle during the COVID-19 Pandemic: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 6265. [Google Scholar] [CrossRef]
- Bani-Issa, W.; Radwan, H.; Saqan, R.; Hijazi, H.; Fakhry, R.; Alameddine, M.; Naja, F.; Ibrahim, A.; Lin, N.; Naing, Y.T.; et al. Association between Quality of Sleep and Screen Time during the COVID-19 Outbreak among Adolescents in the United Arab Emirates. J. Sleep. Res. 2023, 32, e13666. [Google Scholar] [CrossRef]
- Cheikh Ismail, L.; Osaili, T.M.; Mohamad, M.N.; Al Marzouqi, A.; Jarrar, A.H.; Abu Jamous, D.O.; Magriplis, E.; Ali, H.I.; Al Sabbah, H.; Hasan, H.; et al. Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study. Nutrients 2020, 12, 3314. [Google Scholar] [CrossRef] [PubMed]
- Rahi, S.; Ghani, M.A.; Ngah, A.H. A Structural Equation Model for Evaluating User’s Intention to Adopt Internet Banking and Intention to Recommend Technology. Accounting 2018, 4, 139–152. [Google Scholar] [CrossRef]
- Rääsk, T.; Mäestu, J.; Lätt, E.; Jürimäe, J.; Jürimäe, T.; Vainik, U.; Konstabel, K. Comparison of IPAQ-SF and Two Other Physical Activity Questionnaires with Accelerometer in Adolescent Boys. PLoS ONE 2017, 12, e0169527. [Google Scholar] [CrossRef] [PubMed]
- Milner, C.E.; Cote, K.A. Benefits of Napping in Healthy Adults: Impact of Nap Length, Time of Day, Age, and Experience with Napping. J. Sleep. Res. 2009, 18, 272–281. [Google Scholar] [CrossRef] [PubMed]
- Althubaiti, A. Information Bias in Health Research: Definition, Pitfalls, and Adjustment Methods. J. Multidiscip. Healthc. 2016, 9, 211–217. [Google Scholar] [CrossRef]
| Variable | n |
|---|---|
| Age, years | |
| <40 | 542 |
| ≥40 | 114 |
| Gender | |
| Female | 491 |
| Male | 147 |
| Nationality | |
| GCC | 370 |
| Non-Arab | 166 |
| Non-GCC Arab | 100 |
| BMI | |
| Underweight | 50 |
| Normal | 317 |
| Overweight | 172 |
| Obese | 97 |
| Occupation | |
| Student | 338 |
| Employed | 232 |
| Unemployed | 68 |
| Number of people per room | |
| 1–2 | 76 |
| 3–5 | 236 |
| >5 | 326 |
| Number of people per room | |
| 1–2 | 543 |
| ≥3 | 95 |
| History of smoking | |
| Yes | 68 |
| No | 570 |
| COVID-19 status | |
| Recovered | 149 |
| Not infected | 256 |
| Physical activity category | |
| Low | 313 |
| Moderate/high | 325 |
| Sleep quality | |
| Poor | 482 |
| Good | 156 |
| Variable | Physical Activity, n (%) | p Value | |
|---|---|---|---|
| Low | Moderate/High | ||
| Age, years | |||
| <40 | 253 (48.3) | 271 (51.7) | 0.400 |
| ≥40 | 60 (51.6) | 54 (47.4) | |
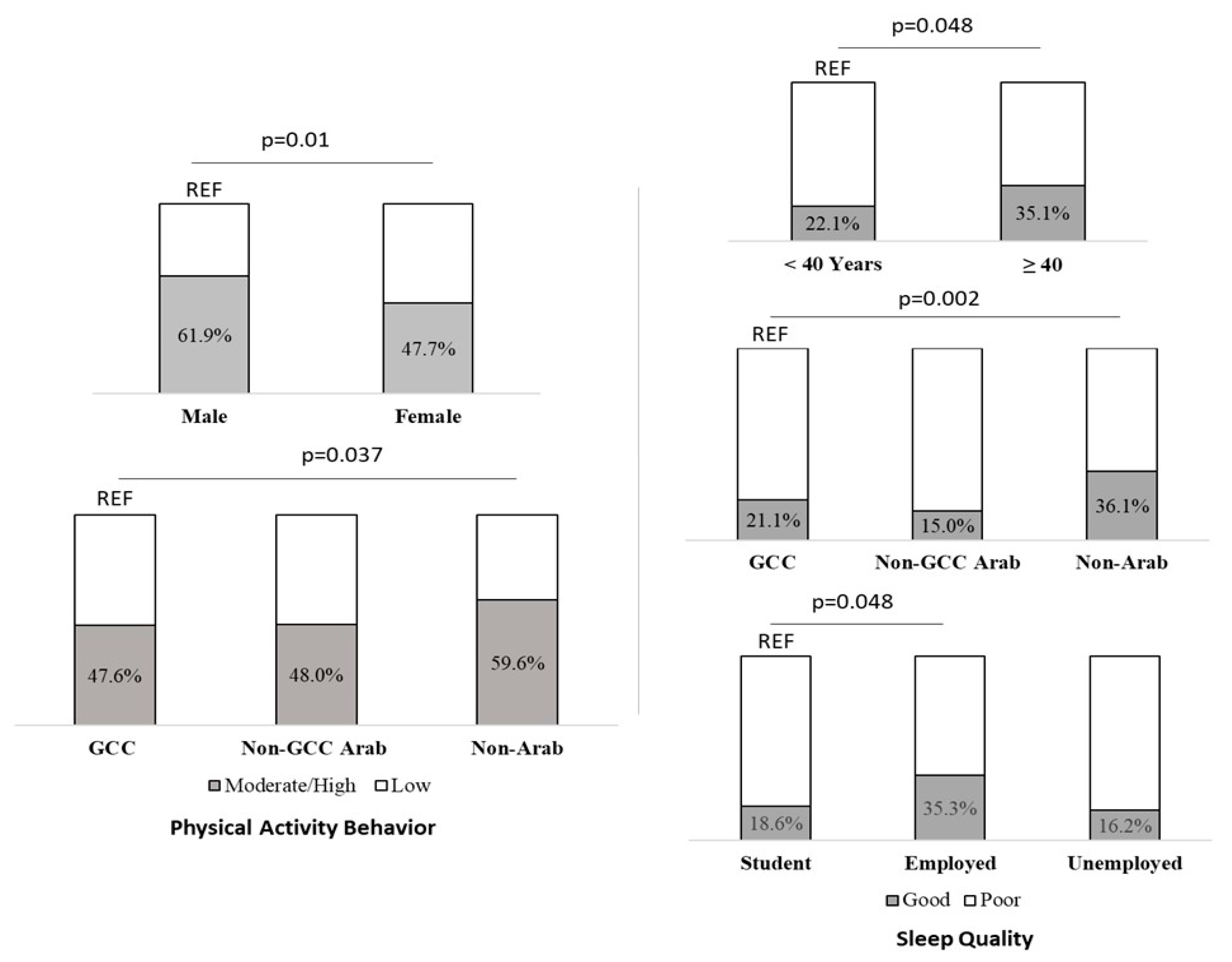
| Sex | |||
| Female | 257 (52.3) | 234 (47.7) | 0.002 |
| Male | 56 (38.1) | 91 (61.9) | |
| Nationality | |||
| GCC | 194 (52.4) | 176 (47.6) | |
| Non-GCC Arab | 52 (52) | 48 (48) | 0.029 |
| Non-Arab | 67 (40.4) | 99 (59.6) | |
| BMI | |||
| Underweight | 28 (56) | 22 (44) | |
| Normal | 152 (47.9) | 165 (52.1) | 0.391 |
| Overweight | 79 (45.9) | 93 (54.1) | |
| Obese | 53 (54.6) | 44 (45.4) | |
| Occupation | |||
| Student | 176 (52.1) | 162 (47.9) | |
| Employed | 100 (43.1) | 132 (56.9) | 0.071 |
| Unemployed | 37 (54.4) | 31 (45.6) | |
| History of smoking | |||
| Yes | 32 (47.1) | 36 (52.9) | 0.727 |
| No | 281 (49.3) | 289 (50.7) | |
| COVID-19 status | |||
| Yes | 74 (49.7) | 75 (50.3) | 0.866 |
| No | 239 (48.9) | 250 (51.1) | |
| Sleep quality | |||
| Poor | 245 (50.8) | 237 (49.2) | 0.116 |
| Good | 68 (43.6) | 88 (56.4) | |
| Variable | uaOR (95% CI) | aOR (95% CI) | p Value |
|---|---|---|---|
| Sex | |||
| Female (Reference, 1) | |||
| Male | 1.79 (1.22, 2.60) | 1.66 (1.13–2.44) | 0.010 |
| Nationality | |||
| GCC (Reference, 1) | |||
| Non-Arab | 1.63 (1.12, 2.36) | 1.49 (1.02–2.18) | 0.037 |
| Non-GCC Arab | 1.02 (0.65, 1.58) | 0.97 (0.62–1.51) | 0.896 |
| Variable | Sleep Quality, n (%) | p Value | |
|---|---|---|---|
| Good | Poor | ||
| Age, years | |||
| <40 | 116 (22.1) | 408 (77.9) | 0.004 |
| ≥40 | 40 (35.1) | 74 (64.9) | |
| Sex | |||
| Female | 109 (22.2) | 382 (77.8) | 0.016 |
| Male | 47 (32) | 100 (68) | |
| Nationality | |||
| GCC | 81 (21.1) | 289 (78.9) | |
| Non-GCC Arab | 15 (15) | 85 (85) | <0.001 |
| Non-Arab | 60 (36.1) | 106 (63.9) | |
| BMI | |||
| Underweight | 12 (24) | 38 (76) | |
| Normal | 84 (26.5) | 233 (73.5) | 0.705 |
| Overweight | 38 (22.1) | 134 (77.9) | |
| Obese | 22 (22.7) | 75 (77.3) | |
| Occupation | |||
| Student | 63 (18.6) | 275 (81.4) | |
| Employed | 82 (35.3) | 150 (64.7) | <0.001 |
| Unemployed | 11 (16.2) | 57 (83.8) | |
| Number of people per room | |||
| 1–2 | 133 (24.5) | 410 (75.5) | 0.953 |
| ≥3 | 23 (24.2) | 72 (75.8) | |
| History of smoking | |||
| Yes | 12 (17.6) | 86 (82.4) | 0.167 |
| No | 144 (25.3) | 426 (74.7) | |
| COVID-19 status | |||
| Yes | 124 (25.4) | 365 (74.6) | 0.335 |
| No | 32 (21.5) | 117 (78.5) | |
| Physical activity | |||
| Low | 68 (21.7) | 245 (78.3) | 0.116 |
| Moderate/High | 88 (27.1) | 237 (72.9) | |
| Variable | uaOR (95% CI) | aOR (95% CI) | p Value |
|---|---|---|---|
| Age, years | |||
| <40 (Reference, 1) | |||
| ≥40 | 1.90 (1.23, 2.94) | 1.70 (1.01–2.89) | 0.048 |
| Gender | |||
| Female (Reference, 1) | |||
| Male | 1.65 (1.10, 2.47) | 1.10 (0.69–1.70) | 0.725 |
| Nationality | |||
| GCC (Reference, 1) | |||
| Non-Arab | 2.02 (1.35, 3.02) | 1.95 (1.27–2.97) | 0.002 |
| Non-GCC Arab | 0.63 (0.35, 1.15) | 0.60 (0.32–1.11) | 0.101 |
| Occupation | |||
| Unemployed (Reference, 1) | |||
| Employed | 2.83 (1.41, 5.70) | 2.76 (1.32–5.76) | 0.007 |
| Student | 1.19 (0.59, 2.39) | 1.47 (0.68–3.18) | 0.329 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arumugam, A.; Murat, D.; Javed, A.; Ali, S.A.; Mahmoud, I.; Trabelsi, K.; Ammar, A. Association of Sociodemographic Factors with Physical Activity and Sleep Quality in Arab and Non-Arab Individuals of Both Sexes during the COVID-19 Pandemic. Healthcare 2023, 11, 2200. https://doi.org/10.3390/healthcare11152200
Arumugam A, Murat D, Javed A, Ali SA, Mahmoud I, Trabelsi K, Ammar A. Association of Sociodemographic Factors with Physical Activity and Sleep Quality in Arab and Non-Arab Individuals of Both Sexes during the COVID-19 Pandemic. Healthcare. 2023; 11(15):2200. https://doi.org/10.3390/healthcare11152200
Chicago/Turabian StyleArumugam, Ashokan, Danya Murat, Asma Javed, Sara Atef Ali, Ibrahim Mahmoud, Khaled Trabelsi, and Achraf Ammar. 2023. "Association of Sociodemographic Factors with Physical Activity and Sleep Quality in Arab and Non-Arab Individuals of Both Sexes during the COVID-19 Pandemic" Healthcare 11, no. 15: 2200. https://doi.org/10.3390/healthcare11152200
APA StyleArumugam, A., Murat, D., Javed, A., Ali, S. A., Mahmoud, I., Trabelsi, K., & Ammar, A. (2023). Association of Sociodemographic Factors with Physical Activity and Sleep Quality in Arab and Non-Arab Individuals of Both Sexes during the COVID-19 Pandemic. Healthcare, 11(15), 2200. https://doi.org/10.3390/healthcare11152200







