Estimation of a Structural Equation Modeling of Quality of Life Mediated by Difficulty in Daily Life in Survivors of Breast Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. FACT-B
2.4. HADS
2.5. SOC-13
2.6. WHODAS 2.0
2.7. CAOD
2.8. Analysis
2.9. Ethics Statement
3. Results
3.1. Participant Characteristics
3.2. Relationship between Each Assessment Scale
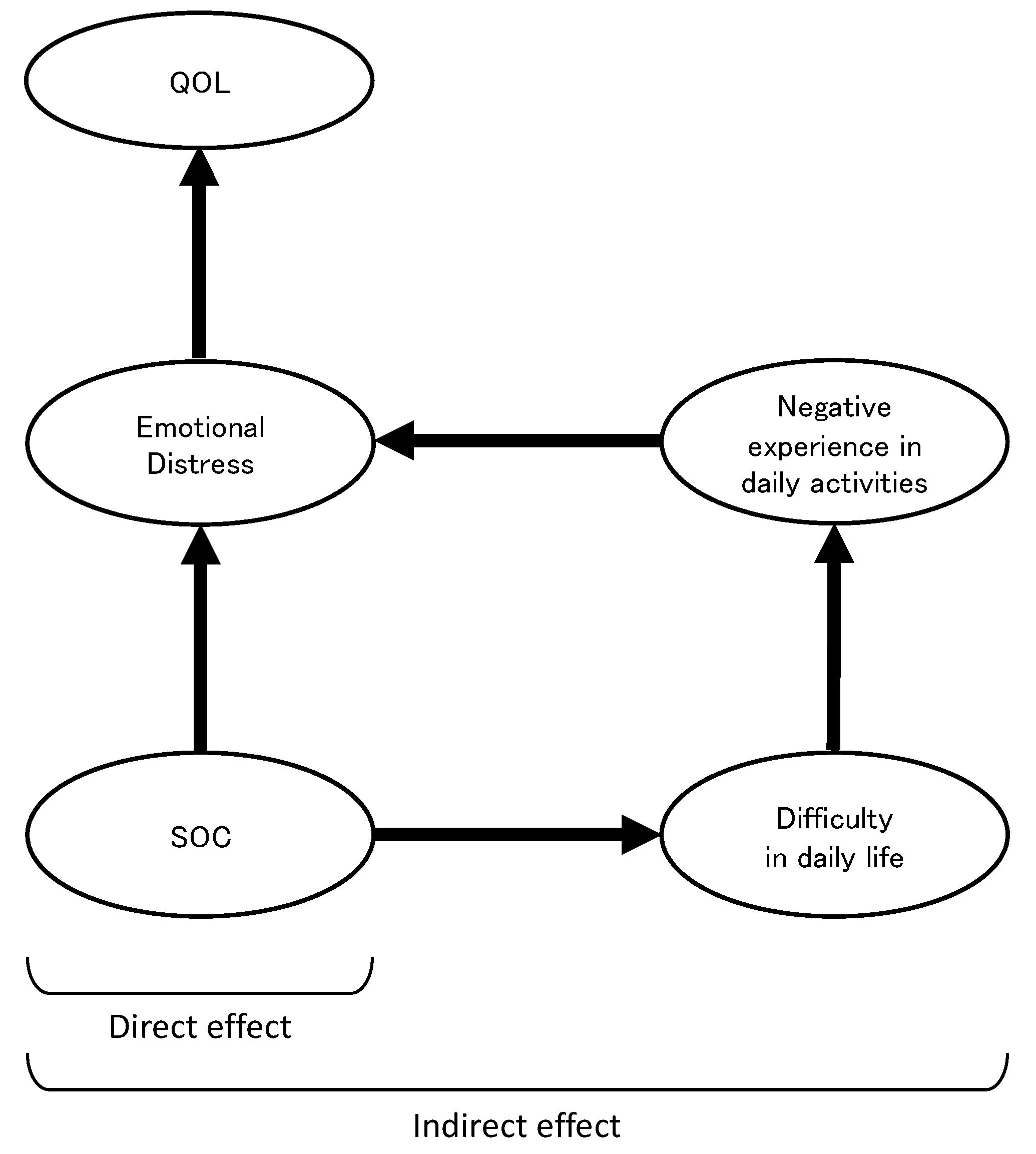
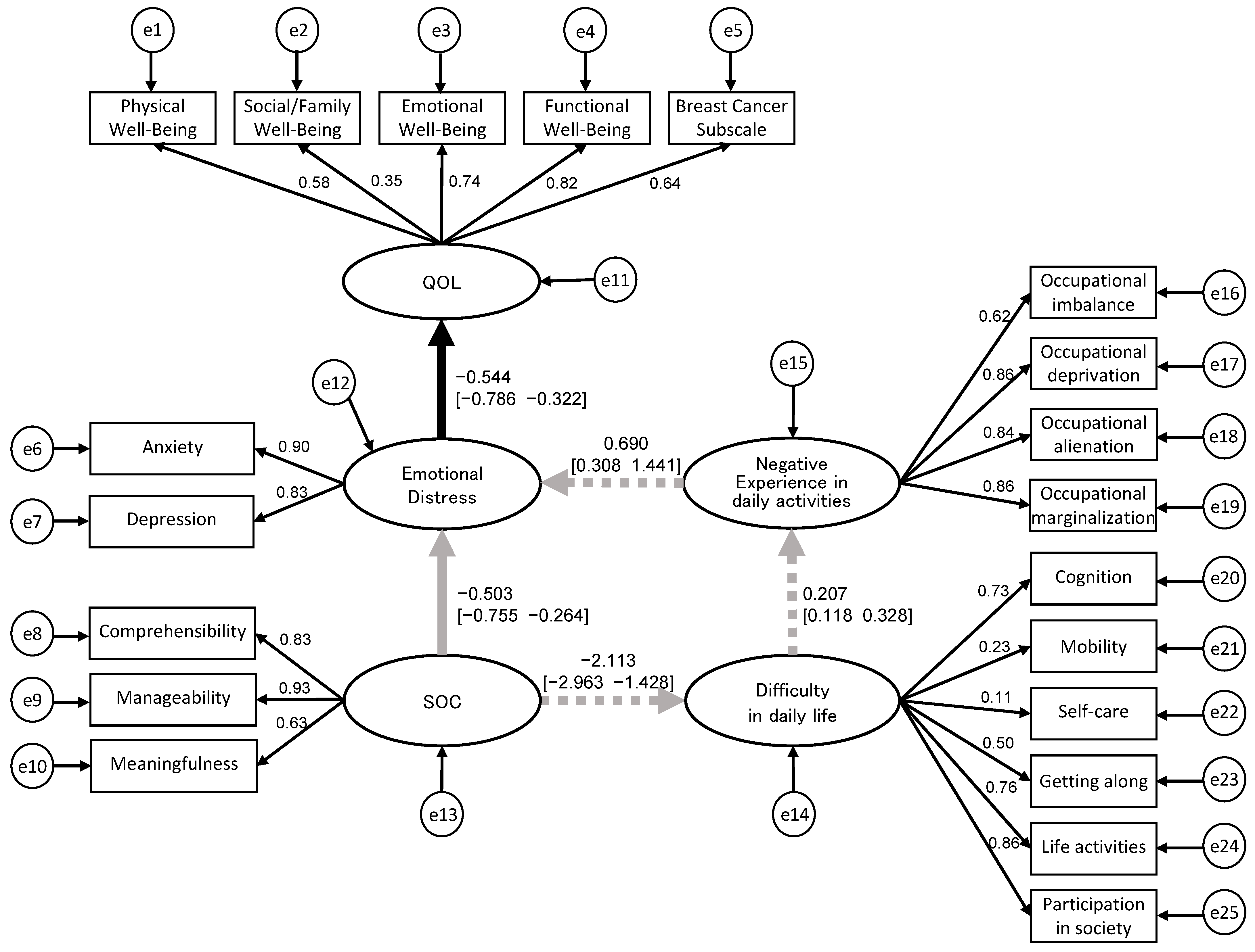
3.3. Structural Relationship of QOL, Emotional Distress, SOC, Difficulty in Daily Life, and Negative Experiences in Daily Activities
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burgess, C.; Cornelius, V.; Love, S.; Graham, J.; Richards, M.; Ramirez, A. Depression and anxiety in women with early breast cancer: Five year observational cohort study. BMJ 2005, 330, 702. [Google Scholar] [CrossRef] [PubMed]
- McNeely, M.L.; Campbell, K.L.; Rowe, B.H.; Klassen, T.P.; Mackey, J.R.; Courneya, K.S. Effects of exercise on breast cancer patients and survivors: A systematic review and meta-analysis. Can. Med. Assoc. J. 2006, 175, 34–41. [Google Scholar] [CrossRef]
- Nguyen, H.T.Y. Post-discharge Unmet Supportive Care Needs of Breast Cancer Patients: A Systematic Review. J. Health Sci. Med. Res. 2023, 41, e2022887. [Google Scholar] [CrossRef]
- Suzuki, K.; Hayashi, N.; Hayashi, E.; Fukawa, A. Sense of Coherence in Cancer Patients: A Literature Review. Osaka Med. Coll. J. Nurs. Res. 2017, 7, 3–13. (In Japanese) [Google Scholar]
- Antonovsky, A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well; Jossey-Bass: Hoboken, NJ, USA, 1987. [Google Scholar]
- Rohani, C.; Abedi, H.A.; Sundberg, K.; Langius-Eklöf, A. Sense of coherence as a mediator of health-related quality of life dimensions in patients with breast cancer: A longitudinal study with prospective design. Health Qual Life Outcomes 2015, 13, 1–9. [Google Scholar] [CrossRef]
- Kenne Sarenmalm, E.; Browall, M.; Persson, L.O.; Fall-Dickson, J.; Gaston-Johansson, F. Relationship of sense of coherence to stressful events, coping strategies, health status, and quality of life in women with breast cancer. Psychooncology 2013, 22, 20–27. [Google Scholar] [CrossRef]
- Drageset, J.; Eide, G.E.; Hauge, S. Symptoms of depression, sadness and sense of coherence (coping) among cognitively intact older people with cancer living in nursing homes-a mixed-methods study. PeerJ 2016, 4, e2096. [Google Scholar] [CrossRef]
- Üstün, T.B.; Chatterji, S.; Kostanjsek, N.; Rehm, J.; Kennedy, C.; Epping-Jordan, J.; Saxena, S.; von Korff, M.; Pull, C. Developing the World Health Organization disability assessment schedule 2.0. Bull. World Health Organ. 2010, 88, 815–823. [Google Scholar] [CrossRef]
- Tazaki, M.; Yamaguchi, T.; Yatsunami, M.; Nakane, Y. Measuring functional health among the elderly: Development of the Japanese version of the World Health Organization Disability Assessment Schedule II. Int. J. Rehabil. Res. 2014, 37, 48–53. [Google Scholar] [CrossRef]
- Lourenço, A.; Dantas, A.A.G.; de Souza, J.C.; Araujo, C.M.; Araujo, D.N.; Lima, I.N.D.F.; de Sousa Dantas, D. Sleep quality is associated with disability and quality of life in breast cancer survivors: A cross-sectional pilot study. Eur. J. Cancer Care 2021, 30, e13339. [Google Scholar] [CrossRef]
- Chachaj, A.; Małyszczak, K.; Pyszel, K.; Lukas, J.; Tarkowski, R.; Pudełko, M.; Andrzejak, R.; Szuba, A. Physical and psychological impairments of women with upper limb lymphedema following breast cancer treatment. Psychooncology 2010, 19, 299–305. [Google Scholar] [CrossRef]
- Zhao, H.P.; Liu, Y.; Li, H.L.; Ma, L.; Zhang, Y.J.; Wang, J. Activity limitation and participation restrictions of breast cancer patients receiving chemotherapy: Psychometric properties and validation of the Chinese version of the WHODAS 2.0. Qual. Life Res. 2013, 22, 897–906. [Google Scholar] [CrossRef]
- Pösl, M.; Cieza, A.; Stucki, G. Psychometric properties of the WHODASII in rehabilitation patients. Qual. Life Res. 2007, 16, 1521–1531. [Google Scholar] [CrossRef] [PubMed]
- Teraoka, M.; Kyougoku, M. Development of the Final Version of the Classification and Assessment of Occupational Dysfunction Scale. PLoS ONE 2015, 10, e0134695. [Google Scholar] [CrossRef] [PubMed]
- Townsend, E.; Wilcock, A.A. Occupationaljustice and client-centred practice: A dialogue in progress. Can. J. Occup. Ther. 2004, 71, 75–87. [Google Scholar] [CrossRef]
- Teraoka, M.; Kyougoku, M. Analysis of structural relationship among the occupational dysfunction on the psychological problem in healthcare workers: A study using structural equation modeling. PeerJ 2015, 3, e1389. [Google Scholar] [CrossRef]
- Teraoka, M.; Kyougoku, M. Causal relationship between occupational dysfunction and depression in healthcare workers: A study using structural equation model. PeerJ PrePrints 2015, 3, e787v1. [Google Scholar]
- Katz, A.H.; Bender, E.I. Self-help groups in Western society: History and prospects. J. Appl. Behav. Sci. 1976, 12, 265–282. [Google Scholar] [CrossRef]
- Ohmatsu, S. My Study Note—Peer Support in Cancer Patients Groups. Acta Med. Hyogo. 2014, 38, 41–45. [Google Scholar]
- Brady, M.J.; Cella, D.F.; Mo, F.; Bonomi, A.E.; Tulsky, D.S.; Lloyd, S.R.; Deasy, S.; Cobleigh, M.; Shiomoto, G. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J. Clin. Oncol. 1997, 15, 974–986. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Togari, T.; Yamazaki, Y.; Nakayama, K.; Yokoyama, Y.; Yonekura, Y.; Takeuchi, T. Nationally representative score of the Japanese language version of the 13-item 7-point sense of coherence scale. Jpn. J. Public Health 2015, 62, 232–237. (In Japanese) [Google Scholar]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. 2003, 8, 23–74. [Google Scholar]
- Vandenberg, R.J.; Lance, C.E. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organ Res. Methods 2000, 3, 4–70. [Google Scholar] [CrossRef]
- Deng, L.; Yang, M.; Marcoulides, K.M. Structural equation modeling with many variables: A systematic review of issues and developments. Front. Psychol. 2018, 9, 580. [Google Scholar] [CrossRef]
- Yarnell, C.J.; Granton, J.T.; Tomlinson, G. Bayesian analysis in critical care medicine. Am. J. Respir. Crit. Care Med. 2020, 201, 396–398. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Ko, Y.H.; Song, Y.; Kang, M.J.; Lee, H.; Kim, S.H.; Jeon, J.Y.; Cho, Y.U.; Yi, G.; Han, J. Pre-post analysis of a social capital-based exercise adherence intervention for breast cancer survivors with moderate fatigue: A randomized controlled trial. Support. Care Cancer 2020, 28, 5281–5289. [Google Scholar] [CrossRef]
- Cain, M.K.; Zhang, Z. Fit for a Bayesian: An evaluation of PPP and DIC for structural equation modeling. Struct. Equat. Model. 2019, 26, 39–50. [Google Scholar] [CrossRef]
- Zamanian, H.; Amini-Tehrani, M.; Jalali, Z.; Daryaafzoon, M.; Ramezani, F.; Malek, N.; Adabimohazab, M.; Hozouri, R.; Rafiei Taghanaky, F. Stigma and quality of life in women with breast cancer: Mediation and moderation model of social support, sense of coherence, and coping strategies. Front. Psychol. 2022, 18, 657992. [Google Scholar] [CrossRef]
- Rohani, C.; Abedi, H.A.; Omranipour, R.; Langius-Eklöf, A. Health-related quality of life and the predictive role of sense of coherence, spirituality and religious coping in a sample of Iranian women with breast cancer: A prospective study with comparative design. Health Qual. Life Outcomes 2015, 13, 40. [Google Scholar] [CrossRef]
- Forsberg, K.A.; Björkman, T.; Sandman, P.O.; Sandlund, M. Influence of a lifestyle intervention among persons with a psychiatric disability: A cluster randomised controlled trail on symptoms, quality of life and sense of coherence. J. Clin. Nurs. 2010, 19, 1519–1528. [Google Scholar] [CrossRef]
- Moen, V.P.; Eide, G.E.; Drageset, J.; Gjesdal, S. Sense of coherence, disability, and health-related quality of life: A cross-sectional study of rehabilitation patients in Norway. Arch. Phys. Med. Rehabil. 2019, 100, 448–457. [Google Scholar] [CrossRef]
- Watanabe, A.; Kawaguchi, T.; Sakimoto, M.; Oikawa, Y.; Furuya, K.; Matsuoka, T. Occupational dysfunction as a mediator between recovery process and difficulties in daily life in severe and persistent mental illness: A Bayesian structural equation modeling approach. Occup. Ther. Int. 2022, 2022, 2661585. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, M.S.; O’Mahony, J.; Karkada, S.N. Effectiveness and meaningfulness of breast cancer survivorship and peer support for improving the quality of life of immigrant women: A mixed methods systematic review protocol. Clin. Epidemiol. Global Health 2021, 10, 100678. [Google Scholar] [CrossRef]
- Arent, S.M.; Walker, A.J.; Arent, M.A. The effects of exercise on anxiety and depression. In Handbook of Sport Psychology; Wiley: Hoboken, NJ, USA, 2020; pp. 872–890. [Google Scholar]
- Zeppegno, P.; Krengli, M.; Ferrante, D.; Bagnati, M.; Burgio, V.; Farruggio, S.; Rolla, R.; Gramaglia, C.; Grossini, E. Psychotherapy with music intervention improves anxiety, depression and the redox status in breast cancer patients undergoing radiotherapy: A randomized controlled clinical trial. Cancers 2021, 13, 1752. [Google Scholar] [CrossRef]
- Knobf, M.T.; Cooley, M.E.; Duffy, S.; Doorenbos, A.; Eaton, L.; Given, B.; Mayer, D.K.; McCorkle, R.; Miaskowski, C.; Mitchell, S.; et al. The 2014–2018 Oncology Nursing Society Research Agenda. Oncol. Nurs. Forum 2015, 42, 450–465. [Google Scholar] [CrossRef]
- Yamanaka, M.; Suzuki, K. Educational Intervention for Promoting Self-management of Patients with Cancer Pain: A Literature Review. Palliative Care Res. 2018, 13, 7–21. (In Japanese) [Google Scholar] [CrossRef]
- Priebe, S. Social outcomes in schizophrenia. Br. J. Psychiatry 2007, 191, s15–s20. [Google Scholar] [CrossRef] [PubMed]
- Alagizy, H.; Soltan, M.R.; Soliman, S.S.; Nashat, N. Anxiety, depression and perceived stress among breast cancer patients: Single institute experience. Middle East Curr. Psychiatry 2020, 27, 1–10. [Google Scholar] [CrossRef]
| Characteristic | Value |
|---|---|
| Participants [n] | 73 |
| Male | 0 |
| Female | 73 |
| Age [years (range)] | 62.4 ± 8.6 (44–80) |
| Period of education [years (range)] | 14.3 ± 2.1 (10–22) |
| Marital status [n] | |
| Married | 53 (72.6%) |
| Divorced | 5 (6.9%) |
| Not married | 9 (12.3%) |
| Bereaved | 6 (8.2%) |
| Family structure [n] | |
| Living together | 62 (84.9%) |
| Separate | 11 (15.1%) |
| Type of surgery [n] | |
| Mastectomy | 47 (64.4%) |
| Breast-conserving surgery | 16 (21.9%) |
| Lumpectomy | 9 (12.3%) |
| Unknown | 1 (1.4%) |
| Clinical stage [n] | |
| stage 0 | 2 (2.7%) |
| stage I | 26 (35.6%) |
| stage II | 27 (37.1%) |
| stage III | 7 (9.6%) |
| stage IV | 2 (2.7%) |
| Unknown | 9 (12.3%) |
| Duration from first surgery a [years (range)] | 13.1 ± 7.6 (5.0–36.4) |
| Treatment of post-surgery [n] | |
| Chemotherapy | 39 (53.4%) |
| Radiotherapy | 38 (52.1%) |
| Hormone therapy | 55 (75.3%) |
| Others | 16 (21.9%) |
| Current job status [n] | |
| Working | 35 (47.9%) |
| Not working | 38 (52.1%) |
| Assessment (Range of Score) | Score (Range) |
|---|---|
| FACT-B (0–148) | 100.5 ± 19.2 (60–137) |
| Physical Well-Being (0–28) | 23.3 ± 5.2 (8–28) |
| Social/Family Well-Being (0–28) | 15.8 ± 6.6 (2–28) |
| Emotional Well-Being (0–24) | 17.7 ± 4.5 (7–24) |
| Functional Well-Being (0–28) | 19.7 ± 5.5 (5–28) |
| Breast Cancer Subscale (0–40) | 24.1 ± 5.9 (2–33) |
| HADS | |
| HADS-A (0–21) | 6.6 ± 4.8 (0–20) |
| HADS-D (0–21) | 6.4 ± 4.1 (0–19) |
| SOC-13 | |
| Total (13–91) | 62.1 ± 12.9 (27–87) |
| Comprehensibility (5–35) | 23.3 ± 6.2 (7–34) |
| Manageability (4–28) | 18.1 ± 4.8 (7–28) |
| Meaningfulness (4–28) | 20.8 ± 3.8 (10–28) |
| WHODAS 2.0 (0–100) | |
| Total score | 14.1 ± 10.6 (0–40) |
| Cognition | 9.5 ± 14.3 (0–80) |
| Mobility | 9.7 ± 13.3 (0–56.3) |
| Self-care | 1.5 ± 5.2 (0–30) |
| Getting along | 20.7 ± 18.2 (0–75) |
| Life activities | 18.6 ± 20.8 (0–70) |
| Participation in society | 21.7 ± 17.9 (0–58.3) |
| CAOD | |
| Total score (16–112) | 44.1 ± 19.3 (16–95) |
| Occupational imbalance (4–28) | 11.3 ± 6.2 (4–26) |
| Occupational deprivation (3–21) | 9.9 ± 5.2 (3–21) |
| Occupational alienation (3–21) | 8.7 ± 4.5 (3–18) |
| Occupational marginalization (6–42) | 14.2 ± 6.9 (6–35) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watanabe, A.; Kawaguchi, T.; Nobematsu, A.; Sasada, S.; Kanari, N.; Maru, T.; Kobayashi, T. Estimation of a Structural Equation Modeling of Quality of Life Mediated by Difficulty in Daily Life in Survivors of Breast Cancer. Healthcare 2023, 11, 2082. https://doi.org/10.3390/healthcare11142082
Watanabe A, Kawaguchi T, Nobematsu A, Sasada S, Kanari N, Maru T, Kobayashi T. Estimation of a Structural Equation Modeling of Quality of Life Mediated by Difficulty in Daily Life in Survivors of Breast Cancer. Healthcare. 2023; 11(14):2082. https://doi.org/10.3390/healthcare11142082
Chicago/Turabian StyleWatanabe, Aki, Takayuki Kawaguchi, Ayumi Nobematsu, Satoshi Sasada, Nozomi Kanari, Tatsuya Maru, and Takeshi Kobayashi. 2023. "Estimation of a Structural Equation Modeling of Quality of Life Mediated by Difficulty in Daily Life in Survivors of Breast Cancer" Healthcare 11, no. 14: 2082. https://doi.org/10.3390/healthcare11142082
APA StyleWatanabe, A., Kawaguchi, T., Nobematsu, A., Sasada, S., Kanari, N., Maru, T., & Kobayashi, T. (2023). Estimation of a Structural Equation Modeling of Quality of Life Mediated by Difficulty in Daily Life in Survivors of Breast Cancer. Healthcare, 11(14), 2082. https://doi.org/10.3390/healthcare11142082







