Blood Service in a Region of China’s Qinghai–Tibetan Plateau
Abstract
:1. Introduction
2. Methods
2.1. Study Setting and Design
2.2. Patient and Public Involvement
3. Results
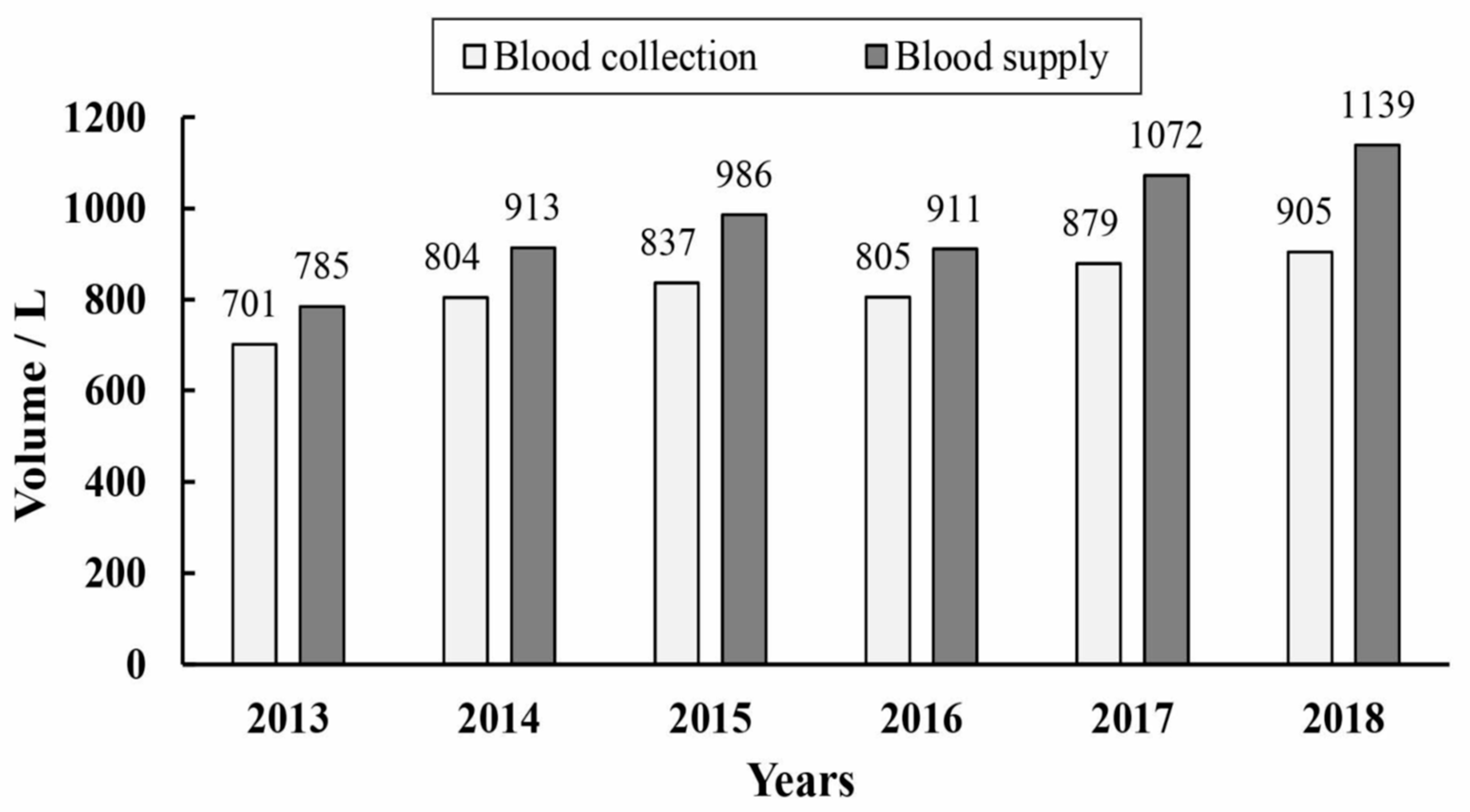
3.1. Blood Donation
3.2. Blood Donors
3.3. Blood Screening
3.4. Blood Supply
4. Discussion
Strengths and Limitations of This Study
- We conducted a systematic and comprehensive study on the status of blood service in the Aba Tibetan and Qiang Regions (Aba Prefecture) from 2013 to 2018 that included geography, population, voluntary non-remunerated blood donation, donors, screening and supply.
- The special characteristics of Aba Prefecture make the blood donation service there different from that in other part of China.
- The results may only reflect blood donation in Aba Tibetan and Qiang Regions, not be generalizable over other minority groups at high-altitude regions.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- People’s Government of Aba Prefecture. Aba Prefecture Yearbook 2018; Sichuan Science and Technology Press: Chengdu, China, 2018.
- Statistics Bureau of Aba Prefecture. Economic and Social Development Statistical Bulletin of Aba Prefecture. Available online: http://www.abazhou.gov.cn/abazhou/c101963/201904/831c01ea7c0a45868f815731d6189492.shtml (accessed on 20 April 2023).
- Lin, Y.W.; Wu, D.R.; Ma, L.; Liu, B.; Zhuo, M.; Xue, L.L.; Guo, F.; Ye, S.L.; Li, C.Q. Analysis on the current voluntary blood donation status in Aba Prefecture. Chin. J. Blood Transfus. 2019, 8, 805–807. [Google Scholar]
- World Health Organization. Blood Safety and Availability. Available online: https://www.who.int/en/news-room/fact-sheets/detail/blood-safety-and-availability (accessed on 20 April 2023).
- Zhu, Y.; Xie, D.; Wang, X.; Qian, K. Challenges and Research in Managing Blood Supply in China. Transfus. Med. Rev. 2017, 31, 84–88. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of the People’s Republic of China. China’s Report on Blood Safety 2018; People’s Medical Publishing House: Beijing, China, 2020.
- Liu, H.; Li, W.H.; Huang, X.Q.; Wang, Y.; Liu, X.X.; Liu, B.; Liu, Z.; Liu, Y. Analysis and comments on the current voluntary blood donation status in Sichuan province. Chin. J. Blood Transfus. 2018, 31, 517–519. [Google Scholar]
- National Health Commission of the People’s Republic of China. Bulletin on the China’s blood safety technology verifacation 2017. Chin. Pract. J. Rural Dr. 2018, 25, 3–4. [Google Scholar]
- World Health Organization. WHO Global Database of Blood Safety Summary Report 2008; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- World Health Organization. Global Status Report on Blood Safety and Availability 2021; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Statistics Bureau of Aba Prefecture. Economic and Social Development Statistical Bulletin of Sichuan Province. Available online: http://www.sc.gov.cn/10462/10778/10876/2019/3/7/61bb956f4e064bbab10b009d0ed2f935.shtml (accessed on 23 April 2023).
- Deng, Z. Causes and countermeasures of difficulties in recruiting blood donors in Plateau. World Latest Med. Inf. 2018, 18, 2. [Google Scholar]
- Shang, L.; Li, Y.J.; Tu, D.J. Investigation and analysis blood donation population in Nyingchi, Tibet, 2012–2015. Chongqing Med. Sci. 2016, 45, 245–246. [Google Scholar]
- Mao, R.; Sun, J. Analysis of the blood donation, supply and characteristics of the blood donors in Lhasa, Tibet. J. Pract. Med. Tech. 2016, 23, 148–150. [Google Scholar]
- Wang, Y.; Wu, Z.; Yin, Y.H.; Rao, S.Q.; Liu, B.; Huang, X.Q.; Liu, X.X.; Li, W.H.; Ye, S.L.; Li, S.Y.; et al. Blood service in the Tibetan regions of Garzê and Aba, China: A longitudinal survey. Transfus. Med. 2017, 27, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Wang, Z.; Shen, Y.; Liu, Z.; Wang, H.; Zhang, S.; Gan, J.; Xue, F.; Han, W.; Shi, X.; et al. Population-based projections of blood supply and demand, China, 2017–2036. Bull. World Health Organ. 2020, 98, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Chen, W.; Liu, Z.; Huang, Y. Safety and current status of blood transfusion in China: An update. Lancet Haematol. 2016, 3, e60–e62. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.H.; Li, C.Q.; Liu, Z. Blood donation in China: Sustaining efforts and challenges in achieving safety and availability. Transfusion 2015, 55, 2523–2530. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y. Characteristics and causes of pre-donation deferrals at a Chinese blood center. Transfus. Apher. Sci. 2021, 60, 103153. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.R.; Flamm, S.L.; Di Bisceglie, A.M.; Bodenheimer, H.C. Serum activity of alanine aminotransferase (ALT) as an indicator of health and disease. Hepatology 2008, 47, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- Li, F.Q.; Liu, J. Investigation on prevalence of HBV, HCV, TP and HIV infection among blood donors in Aba. Sichuan Province. Pract. Prev. Med. 2008, 15, 3. [Google Scholar]
- National Health Commission of the People’s Republic of China. China’s Report on Blood Safety 2016; People’s Medical Publishing House: Beijing, China, 2017.



| Counties | Area/km2 | Altitude /m a | Population /1000 b | Number of Blood Donors per Year | Volume of Blood Donation per Year /L | Volume of Blood Use per Year/L |
|---|---|---|---|---|---|---|
| Barkam | 6639 | 2600 | 59.9 | 618 ± 90 | 159.6 ± 21.0 | 423.6 ± 50.8 |
| Jinchuan | 5524 | 2165 | 75.0 | 186 ± 41 | 49.1 ± 10.3 | 28.9 ± 4.7 |
| Xiaojin | 5571 | 2367 | 80.0 | 166 ± 51 | 43.1 ± 13.0 | 29.8 ± 4.0 |
| Aba | 10,435 | 3290 | 77.0 | 139 ± 29 | 36.4 ± 7.9 | 50.9 ± 15.0 |
| Ruoergai | 10,437 | 3406 | 78.1 | 137 ± 63 | 35.3 ± 14.8 | 27.5 ± 10.7 |
| Hongyuan | 8398 | 3504 | 49.3 | 110 ± 17 | 27.1 ± 4.5 | 14.5 ± 3.0 |
| Rangtang | 6836 | 3285 | 41.9 | 96 ± 14 | 24.4 ± 2.7 | 29.3 ± 10.5 |
| Wenchuan | 4083 | 1326 | 102.3 | 585 ± 70 | 140.4 ± 14.6 | 64.7 ± 16.7 |
| Li | 4318 | 1888 | 48.7 | 181 ± 68 | 49.8 ± 20.1 | 9.7 ± 4.9 |
| Mao | 4075 | 1580 | 110.8 | 372 ± 34 | 101.3 ± 10.7 | 89.8 ± 29.2 |
| Songpan | 8486 | 2851 | 75.2 | 232 ± 46 | 59.6 ± 14.2 | 96.5 ± 24.0 |
| Jiuzhaigou | 5286 | 1406 | 81.3 | 237 ± 36 | 66.3 ± 11.3 | 85.0 ± 15.1 |
| Heishui | 4154 | 2350 | 60.6 | 115 ± 61 | 29.3 ± 14.3 | 17.5 ± 6.3 |
| Total | 84,242 | — | 940.1 | 3175 ± 305 | 821.8 ± 71.4 | 967.6 ± 126.5 |
| Counties | Rejection Rates in Laboratory Testing (%) a | |||||
|---|---|---|---|---|---|---|
| ALT | HBV | HCV | TP | HIV | Total | |
| Barkam | 3.45 | 0.43 | 0.08 | 0.78 | 0.08 | 4.83 |
| Jinchuan | 4.11 | 0.45 | 0.27 | 1.07 | 0.27 | 6.17 |
| Xiaojin | 4.11 | 0.50 | 0.10 | 0.50 | 0 | 5.21 |
| Aba | 4.80 | 0.24 | 0.36 | 1.08 | 0 | 6.48 |
| Ruoergai | 4.88 | 0.73 | 0.24 | 1.10 | 0.12 | 7.07 |
| Hongyuan | 4.55 | 0.91 | 0.30 | 1.06 | 0.61 | 7.42 |
| Rangtang | 3.81 | 0.35 | 0.17 | 1.04 | 0.17 | 5.55 |
| Wenchuan | 2.28 | 0.77 | 0.17 | 0.40 | 0.03 | 3.65 |
| Li | 3.50 | 0.18 | 0.09 | 0.55 | 0 | 4.33 |
| Mao | 2.56 | 0.40 | 0.13 | 0.54 | 0.04 | 3.68 |
| Songpan | 2.58 | 0.79 | 0.14 | 0.43 | 0 | 3.95 |
| Jiuzhaigou | 2.95 | 0.63 | 0 | 0.56 | 0.49 | 4.64 |
| Heishui | 3.47 | 0.14 | 0.14 | 0.58 | 0.43 | 4.77 |
| Total | 3.28 | 0.53 | 0.15 | 0.67 | 0.13 | 4.75 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, P.; Zhu, L.; Ma, L.; Li, C.; Wang, Z.; Zhang, R.; Ye, S.; Wang, Y. Blood Service in a Region of China’s Qinghai–Tibetan Plateau. Healthcare 2023, 11, 1944. https://doi.org/10.3390/healthcare11131944
Sun P, Zhu L, Ma L, Li C, Wang Z, Zhang R, Ye S, Wang Y. Blood Service in a Region of China’s Qinghai–Tibetan Plateau. Healthcare. 2023; 11(13):1944. https://doi.org/10.3390/healthcare11131944
Chicago/Turabian StyleSun, Pan, Liyuan Zhu, Li Ma, Changqing Li, Zongkui Wang, Rong Zhang, Shengliang Ye, and Ya Wang. 2023. "Blood Service in a Region of China’s Qinghai–Tibetan Plateau" Healthcare 11, no. 13: 1944. https://doi.org/10.3390/healthcare11131944
APA StyleSun, P., Zhu, L., Ma, L., Li, C., Wang, Z., Zhang, R., Ye, S., & Wang, Y. (2023). Blood Service in a Region of China’s Qinghai–Tibetan Plateau. Healthcare, 11(13), 1944. https://doi.org/10.3390/healthcare11131944







