Advancing Dermatological Care: A Comprehensive Narrative Review of Tele-Dermatology and mHealth for Bridging Gaps and Expanding Opportunities beyond the COVID-19 Pandemic
Abstract
1. Introduction
1.1. Key Pieces of Evidence before the COVID-19 Pandemic
1.2. The Unprecedented Impact of the COVID-19 Pandemic: The Idea of the Overview
1.3. The Purpose of the Overview
- To assess the trends and the evolution of the studies in this field;
- To assess the current state of the art in TD and mHealth, including their strengths and limitations;
- To identify the potential benefits of integrating TD with mHealth, such as increased accuracy and efficiency in diagnosing skin conditions, improved patient outcomes, and cost savings;
- To explore the challenges and barriers to integrating TD with mHealth, such as data privacy concerns, regulatory issues, and the need for specialized expertise;
- To provide guidance on the best practices for implementing and using TD and mHealth in dermatology, including recommendations for data collection and management, model development and validation, and clinical decision-making.
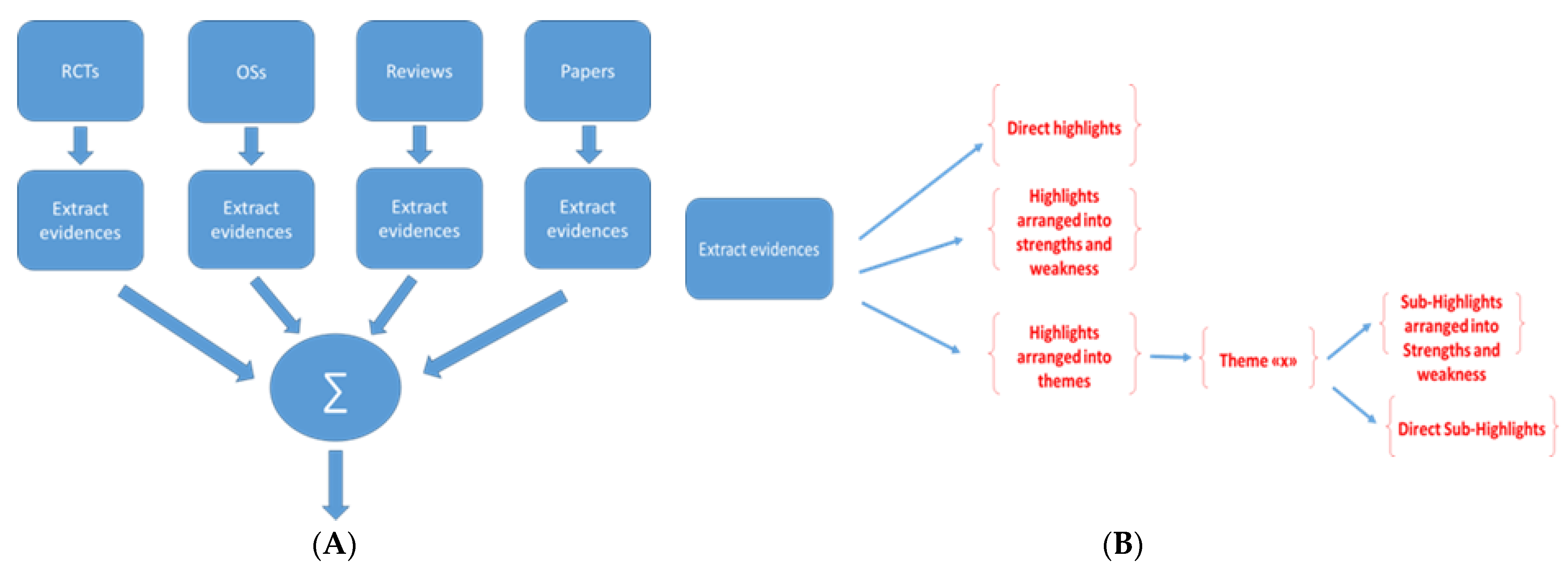
2. Methods
| Algorithm 1 Algorithm applied in the overview |
|
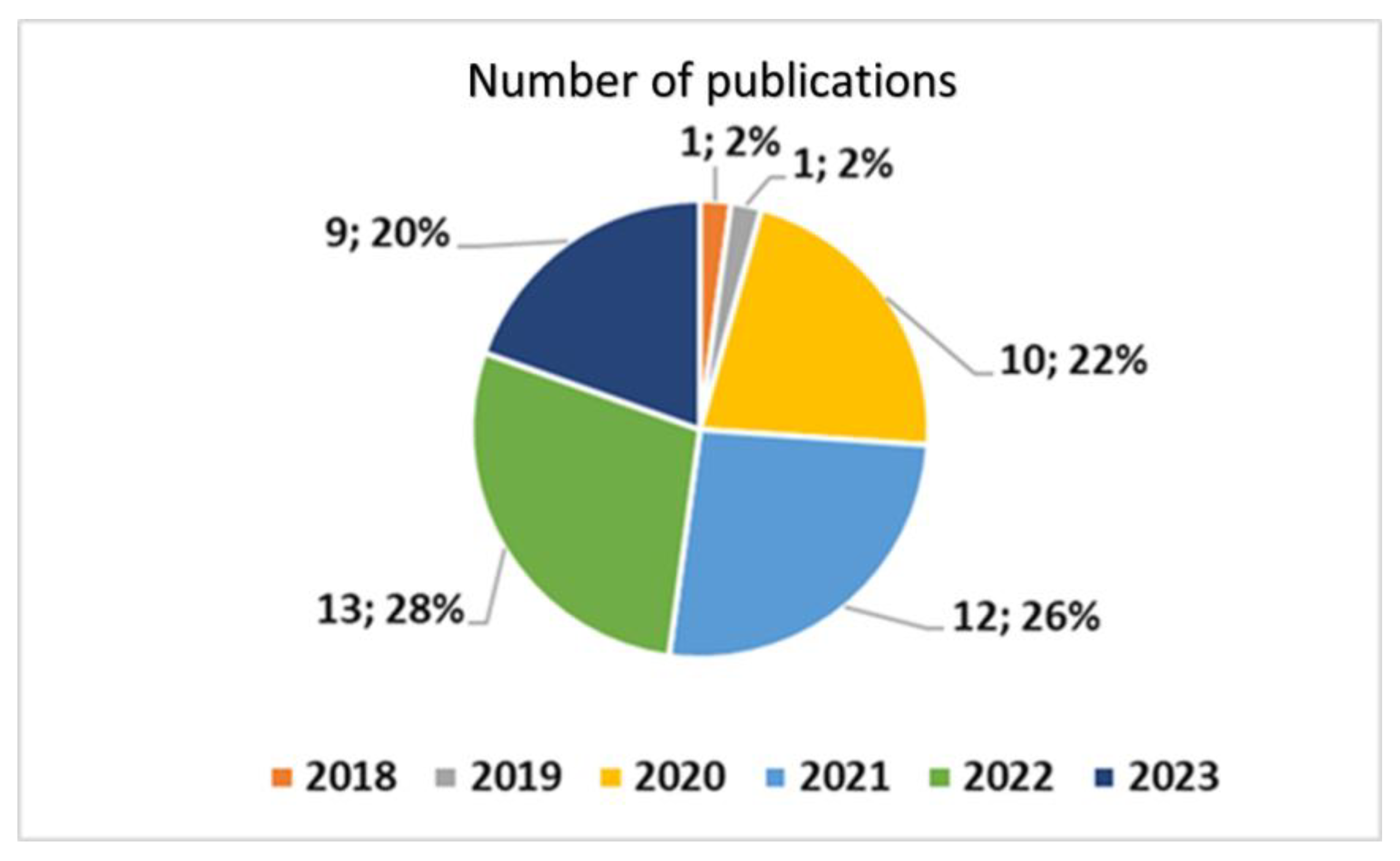
3. Results
3.1. Data Synthesis Plan
3.2. Data Synthesis of the Overview of Scientific Papers
- Opportunities of TD and mHealth. These studies have mostly focused on the horizons of application of TD and mHealth.
- Development, implementation, testing, and shared methodologies. The studies that have addressed these topics have focused on the process of development, testing, and sharing of methodologies.
- Integration models of TD and mHealth. These studies have addressed the issues of integration of TD and mHealth into specific models of the health domain.
- The problems and bottlenecks. These studies have mainly addressed problems and bottlenecks of the integration of TD and mHealth into the health domain.
3.2.1. Opportunities of TD and mHealth
- Improving the accuracy of skin condition diagnoses, especially for challenging conditions like vitiligo, using TD apps;
- The potential for TD and mHealth to be a valid alternative to in-person visits during the COVID-19 pandemic; even greater acceptability will likely be reached with further refinement of the process;
- The use of mobile phone applications to assess photos taken by patients to improve the value, reliability, and availability of patients’ photos to guide their skin care;
- The potential for apps like eSkinHealth to increase the initial recognition and management of skin diseases, including neglected tropical diseases, in sub-Saharan Africa;
- The potential of AI-based TD services like MoleMe App for melanoma screening to achieve widespread usage;
- The feasibility of using mobile devices in TD settings to achieve adequate diagnostic accuracy;
- The development of smartphone-based dermoscopy applications in large national projects, like the TELESPOT project in Belgium, to improve the diagnosis and treatment of skin cancer;
- The successful reduction in spatial and temporal barriers to dermatological care through TD and mHealth, with remote diagnosis and treatment being possible in many cases.
3.2.2. Development, Implementation, Testing, and Shared Methodologies
- A smartphone app was developed in Norway that allowed referring physicians to send information related to skin lesions to dermatologists for diagnosis and therapeutic advice, which helped patients to avoid referrals with specialists for regular consultations in 70% of cases, and could help them to avoid many ordinary consultations in specialized centers.
- Guidelines were developed based on a shared methodology called CLOSE-UP to guide clinicians in capturing and delivering high-quality clinical dermatological images through mHealth during the COVID-19 pandemic.
- An mHealth tool was developed for the remote self-assessment of digital ulcers in patients with systemic sclerosis, which included an app, a custom color reference sticker, and a smartphone holder, and showed that the feedback mechanism improved the overall image quality.
- The investigation of the potential of an inexpensive device called NurugoTM Derma for remotely diagnosing skin tumors or dermatological diseases through TD, which could be used as a triage tool to detect the cases requiring direct interaction with specialists.
3.2.3. TD, mHealth, and the Integration Models
- TD and mHealth are generally suitable for providing remote dermatological care to patients;
- Organizational readiness for change is important for identifying favorable areas in TD and mHealth;
- Models of dermatological care for elderly patients in senior living communities based on TD and mHealth are available;
- Different business models have been explored, and important partnerships, clinician involvement, management of medico-legal risks, and liabilities have been considered very important for the future of this field;
- Patient satisfaction with smartphone-based hybrid TD models of care during the COVID-19 pandemic was assessed, and while most patients were content, some concerns were raised about the quality of care compared to direct consultations;
- Barriers and facilitators to using mHealth models for monitoring low-risk skin lesions in the elderly were identified, and a conceptual framework involving various themes was proposed;
- TD and mHealth have been found to increase the capacity for follow-up care for dermatology patients after discharge, but may not significantly improve the timeliness of care transitions.
3.2.4. Problems and Bottlenecks
- Quality of publicly available apps: The outcome suggests that involving patients in the development and evaluation of health-related apps is crucial, as the factors that make an app appealing to users may differ between healthcare professionals and patients;
- Diagnostic accuracy: The outcome highlighted that, while TD and mHealth have potential for the initial detection of skin cancer, the accuracy in diagnostic applications was not at the level of face-to-face evaluations, and should, thus, be used in conjunction with face-to-face consultations for accurate diagnosis and management planning;
- Variability in photographed skin appearance: The camera distance and angle can affect color accuracy in medical photography, which is important for consistent diagnosis and treatment. This could increase the variability in the appearance of photographed skin over time;
- Lack of cybersecurity (also including consent and data privacy) and data use policies.
3.3. Data Synthesis from the Observational Studies
- The potential of TD and mHealth as an integrated solution for maintaining dermatological services during the COVID-19 pandemic, with an overall satisfaction and future use score of 91%, a usefulness score of 93.7%, and high interface and interaction quality scores;
- The importance of introducing legislation to implement physician compensation for tele-dermatology where this did not previously exist;
- The significant variation in the likelihood of a follow-up dermatology office visit, depending on the technology and workflow used in the field of TD and mHealth;
- The prevalence of acute inflammatory conditions in WhatsApp consultations, which accounted for 74.1% of the messages, and the negative emotional impact on dermatologists; nearly a third reported negative emotions and 82.3% would prefer not to receive these messages.
3.4. Data Synthesis from Randomized Clinical Trials
- Improved access to healthcare: TD and mHealth can improve access to healthcare services for patients who may face geographic, financial, or other barriers to in-person appointments;
- Increased efficiency: TD and mHealth can help to reduce wait times and streamline the triage and treatment processes;
- Better patient outcomes: TD and mHealth can lead to better patient outcomes, such as more accurate diagnoses and improved management of chronic skin conditions;
- Enhanced patient engagement: TD and mHealth can empower patients to take a more active role in their healthcare by providing them with tools and resources to better manage their skin health;
- Improved mental health: The use of disease management smartphone apps may improve the mental health of people with psoriasis.
3.5. Data Synthesis from the Reviews
- TD and mHealth can provide access to specialized care and improve patient outcomes;
- TD and mHealth can increase access to healthcare resources, improving access to specialized centers for people living in remote areas;
- TD and mHealth can enable the early identification of patients through diagnoses of cutaneous signs;
- mHealth and AI can be useful in dermatology, particularly in African countries with limited medical care and long distances between patients and physicians;
- TD and mHealth can be useful for disease-specific information, screening, disease surveillance, medication compliance, and communication during pandemics;
- Incorporating digital dermatology into clinical practice can improve diagnostic accuracy and provide access to dermatological evaluations for underserved communities and those in rural settings.
- The adoption and implementation of TD and mHealth technologies, including those integrated with AI, face technical issues, legal frameworks, and regulatory barriers;
- Incorporating digital dermatology into clinical practice requires legal frameworks to be addressed and reimbursement policies to be updated to benefit patient care;
- Technical issues can negatively affect the adoption of TD and mHealth technologies;
- The challenge of ethnic variation needs to be addressed in order to improve the accuracy of automated algorithms;
- TD and mHealth technologies face infrastructural and technological barriers, organization and financial barriers, policy and regulatory barriers, as well as cultural barriers.
4. Discussion
4.1. Added Value
4.2. Interpretation of Results
4.2.1. Opportunities
4.2.2. Challenges and Barriers
4.2.3. Future Directions
4.3. Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Kaliyadan, F.; Ramsey, M.L. Teledermatology. 2022 Oct 3. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Pubmed Search. Available online: https://pubmed.ncbi.nlm.nih.gov/?term=%28teledermatology+%5BTitle%2FAbstract%5D%29+OR+%28digital+dermatology+%5BTitle%2FAbstract%5D%29&sort=date&size=50 (accessed on 23 June 2023).
- Santiago, S.; Lu, J. Patient Satisfaction in Teledermatology: An Updated Review. Curr. Dermatol. Rep. 2023, 12, 23–26. [Google Scholar] [CrossRef]
- Kriwy, P.; Nötzold, A.; Seitz, A.-T.; Berger, R. Akzeptanz der Teledermatologie Ergebnisseeiner Befragung sächsischer Haus- und HautärztInnen [Acceptance of Teledermatology: Results of a Survey of General Practitioners and Dermatologists in Saxony (Germany)]. Available online: https://www.thieme-connect.com/products/ejournals/abstract/10.1055/a-1999-7523 (accessed on 20 June 2023).
- Giansanti, D.; Di Basilio, F. The Artificial Intelligence in Digital Radiology: Part 1: The Challenges, Acceptance and Consensus. Healthcare 2022, 10, 509. [Google Scholar] [CrossRef] [PubMed]
- Giovagnoli, M.R.; Giansanti, D. Artificial Intelligence in Digital Pathology: What Is the Future? Part 1: From the Digital Slide Onwards. Healthcare 2021, 9, 858. [Google Scholar] [CrossRef] [PubMed]
- Chao, E.; Meenan, C.K.; Ferris, L.K. Smartphone-Based Applications for Skin Monitoring and Melanoma Detection. Dermatol. Clin. 2017, 35, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Damanpour, S.; Srivastava, D.; Nijhawan, R. Self-acquired patient images: The promises and the pitfalls. Semin. Cutan. Med. Surg. 2016, 35, 13–17. [Google Scholar] [CrossRef]
- Pubmed Search. Available online: https://pubmed.ncbi.nlm.nih.gov/?term=%28%28App%5BTitle%2FAbstract%5D%29+OR+%28smartphone%5BTitle%2FAbstract%5D%29+OR+%28mobile+health%5BTitle%2FAbstract%5D%29%29+AND+%28%28Digital+dermatology%5BTitle%2FAbstract%5D%29+OR+%28teledermatology%5BTitle%2FAbstract%5D%29%29 (accessed on 23 June 2023).
- Liopyris, K.; Gregoriou, S.; Dias, J.; Stratigos, A.J. Artificial Intelligence in Dermatology: Challenges and Perspectives. Dermatol. Ther. 2022, 12, 2637–2651. [Google Scholar] [CrossRef]
- Tongdee, E.; Markowitz, O. Mobile app rankings in dermatology. Cutis 2018, 102, 252–256. [Google Scholar]
- Damsin, T.; Jacquemin, P.; Canivet, G.; Giet, D.; Gillet, P.; Nikkels, A.F. Le projet TeleSPOT: Détection précoce du mélanome par télédermoscopie en Médecine générale [TeleSPOT Project: Early detection of melanoma by teledermoscopy in general practice]. Rev. Med. Liege 2019, 74, 650–654. (In French) [Google Scholar]
- Marwaha, S.S.; Fevrier, H.; Alexeeff, S.; Crowley, E.; Haiman, M.; Pham, N.; Tuerk, M.J.; Wukda, D.; Hartmann, M.; Herrinton, L.J. Comparative effectiveness study of face-to-face and teledermatology workflows for diagnosing skin cancer. J. Am. Acad. Dermatol. 2019, 81, 1099–1106. [Google Scholar] [CrossRef]
- Sambhi, R.-D.; Kalaichandran, R.; Tan, J. Critical analysis of features and quality of applications for clinical management of acne. Dermatol. Online J. 2019, 25, 13030/qt1668h2kt. [Google Scholar] [CrossRef]
- Akdeniz, M.; Hahnel, E.; Ulrich, C.; Blume-Peytavi, U.; Kottner, J. Prevalence and associated factors of skin cancer in aged nursing home residents: A multicenter prevalence study. PLoS ONE 2019, 14, e0215379, Erratum in PLoS ONE 2019, 14, e0220488. [Google Scholar] [CrossRef]
- Silveira, C.E.G.; Carcano, C.; Mauad, E.; Faleiros, H.; Longatto-Filho, A. Cell phone usefulness to improve the skin cancer screening: Preliminary results and critical analysis of mobile app development. Rural Remote Health 2019, 19, 4895. [Google Scholar] [CrossRef] [PubMed]
- Koh, U.; Horsham, C.; Soyer, H.P.; Loescher, L.J.; Gillespie, N.; Vagenas, D.; Janda, M. Consumer Acceptance and Expectations of a Mobile Health Application to Photograph Skin Lesions for Early Detection of Melanoma. Dermatology 2019, 235, 4–10. [Google Scholar] [CrossRef]
- Done, N.; Oh, D.H.; Weinstock, M.A.; Whited, J.D.; Jackson, G.L.; King, H.A.; Peracca, S.B.; Elwy, A.R.; Prentice, J.C. VA Telederm study: Protocol for a stepped-wedge cluster randomised trial to compare access to care for a mobile app versus a workstation-based store-and-forward teledermatology process. BMJ Open 2018, 8, e022218. [Google Scholar] [CrossRef]
- Clark, A.K.; Bosanac, S.; Ho, B.; Sivamani, R.K. Systematic review of mobile phone-based teledermatology. Arch. Dermatol. Res. 2018, 310, 675–689. [Google Scholar] [CrossRef]
- Morone, G.; Pirrera, A.; Iannone, A.; Giansanti, D. Development and Use of Assistive Technologies in Spinal Cord Injury: A Narrative Review of Reviews on the Evolution, Opportunities, and Bottlenecks of Their Integration in the Health Domain. Healthcare 2023, 11, 1646. [Google Scholar] [CrossRef]
- Gandhi, K.; Ezzedine, K.; Anastassopoulos, K.P.; Patel, R.; Sikirica, V.; Daniel, S.R.; Napatalung, L.; Yamaguchi, Y.; Baik, R.; Pandya, A.G. Prevalence of Vitiligo Among Adults in the United States. JAMA Dermatol. 2022, 158, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Glines, K.R.; Haidari, W.; Ramani, L.; Akkurt, Z.M.; Feldman, S.R. Digital future of dermatology. Dermatol. Online J. 2020, 26, 13030/qt75p7q57j. [Google Scholar] [CrossRef]
- Peracca, S.B.; Fonseca, A.; Hines, A.; King, H.A.; Grenga, A.M.; Jackson, G.L.; Whited, J.D.; Chapman, J.G.; Lamkin, R.; Mohr, D.C.; et al. Implementation of Mobile Teledermatology: Challenges and Opportunities. Telemed. e-Health 2021, 27, 1416–1422. [Google Scholar] [CrossRef]
- Marasca, C.; Annunziata, M.C.; Camela, E.; Di Guida, A.; Fornaro, L.; Megna, M.; Napolitano, M.; Patruno, C.; Potestio, L.; Fabbrocini, G. Teledermatology and Inflammatory Skin Conditions during COVID-19 Era: New Perspectives and Applications. J. Clin. Med. 2022, 11, 1511. [Google Scholar] [CrossRef]
- Kvedarienė, V.; Burzdikaitė, P.; Česnavičiūtė, I. mHealth and telemedicine utility in the monitoring of allergic diseases. Front. Allergy 2022, 3, 919746. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.; Shukla, N.; Halley, M.; Nava, V.; Budaraju, J.; Zhang, L.; Linos, E. Barriers and facilitators to mobile health and active surveillance use among older adults with skin disease. Health Expect. 2021, 24, 1582–1592. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, S.M.H.; Schopf, T.; Sangha, A.; Ulvin, K.; Gjersvik, P. Teledermatology in Norway using a mobile phone app. PLoS ONE 2020, 15, e0232131. [Google Scholar] [CrossRef] [PubMed]
- Havelin, A.; Hampton, P. Telemedicine and e-Health in the Management of Psoriasis: Improving Patient Outcomes—A Narrative Review. Psoriasis 2022, 12, 15–24. [Google Scholar] [CrossRef]
- Lee, C.; Witkowski, A.; Żychowska, M.; Ludzik, J. The role of mobile teledermoscopy in skin cancer triage and management during the COVID-19 pandemic. Indian J. Dermatol. Venereol. Leprol. 2022, 89, 347–352. [Google Scholar] [CrossRef]
- Perrone, G.; Bilotta, C.; Tullio, V.; Pirrone, R.; Argo, A.; Zerbo, S. Telehealth modulation and new proposals during the COVID-19 pandemic: A literature review. Clin. Ther. 2022, 173, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Lull, C.; von Ahnen, J.A.; Gross, G.; Olsavszky, V.; Knitza, J.; Leipe, J.; Schmieder, A. German Mobile Apps for Patients with Psoriasis: Systematic Search and Evaluation. JMIR mHealth uHealth 2022, 10, e34017. [Google Scholar] [CrossRef]
- Mbunge, E.; Batani, J.; Gaobotse, G.; Muchemwa, B. Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: A systematic review. Glob. Health J. 2022, 6, 102–113. [Google Scholar] [CrossRef]
- Sun, M.D.; Kentley, J.; Wilson, B.W.; Soyer, H.P.; Curiel-Lewandrowski, C.N.; Rotemberg, V.; Halpern, A.C.; The ISIC Technique Working Group. Digital skin imaging applications, part I: Assessment of image acquisition technique features. Ski. Res. Technol. 2022, 28, 623–632. [Google Scholar] [CrossRef]
- Kling, S.M.R.; A Saliba-Gustafsson, E.; Winget, M.; Aleshin, M.A.; Garvert, D.W.; Amano, A.; Brown-Johnson, C.G.; Kwong, B.Y.; Calugar, A.; El-Banna, G.; et al. Teledermatology to Facilitate Patient Care Transitions from Inpatient to Outpatient Dermatology: Mixed Methods Evaluation. J. Med. Internet Res. 2022, 24, e38792. [Google Scholar] [CrossRef]
- Yadav, D.; Bhatia, S.; Ramam, M.; Singh, V.; Khanna, N.; Khandpur, S.; Gupta, V. Patient perception and satisfaction with a smartphone-based teledermatology service initiated during the COVID-19 pandemic at a tertiary care hospital in North India. Indian J. Dermatol. Venereol. Leprol. 2022, 88, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Greis, C.; Maul, L.V.; Hsu, C.; Djamei, V.; Schmid-Grendelmeier, P.; Navarini, A.A. Künstliche Intelligenz zur Unterstützung der Telemedizin am Beispiel Afrikas [Artificial intelligence to support telemedicine in Africa]. Hautarzt 2020, 71, 686–690. (In German) [Google Scholar] [CrossRef] [PubMed]
- Domogalla, L.; Beck, A.; Schulze-Hagen, T.; Herr, R.; Benecke, J.; Schmieder, A. Impact of an eHealth Smartphone App on the Mental Health of Patients with Psoriasis: Prospective Randomized Controlled Intervention Study. JMIR mHealth uHealth 2021, 9, e28149. [Google Scholar] [CrossRef]
- Blum, A.; Bosch, S.; Haenssle, H.A.; Fink, C.; Hofmann-Wellenhof, R.; Zalaudek, I.; Kittler, H.; Tschandl, P. Künstliche Intelligenz und Smartphone-Programm-Applikationen (Apps): Bedeutung für die dermatologische Praxis [Artificial intelligence and smartphone program applications (Apps): Relevance for dermatological practice]. Hautarzt 2020, 71, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, P.I.N.; Hegazy, A.A. Dermatological consultations in the COVID-19 era: Is teledermatology the key to social distancing? An Egyptian experience. J. Dermatol. Treat. 2022, 33, 910–915. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.D.; Kentley, J.; Wilson, B.W.; Soyer, H.P.; Curiel-Lewandrowski, C.N.; Rotemberg, V.M.; Halpern, A.C.; The ISIC Technique Working Group. Digital skin imaging applications, part II: A comprehensive survey of post-acquisition image utilization features and technology standards. Ski. Res. Technol. 2022, 28, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Kho, J.; Gillespie, N.; Horsham, C.; Snoswell, C.; Vagenas, D.; Soyer, H.P.; Janda, M. Skin Doctor Consultations Using Mobile Teledermoscopy: Exploring Virtual Care Business Models. Telemed. e-Health 2020, 26, 1406–1413. [Google Scholar] [CrossRef]
- Handa, S.; Mehta, H.; Bishnoi, A.; Vinay, K.; Mahajan, R.; Narang, T.; Kumaran, M.S.; De, D.; Dogra, S.; Parsad, D. Teledermatology during the COVID-19 pandemic: Experience at atertiary care centre in North India. Dermatol. Ther. 2021, 34, e15022. [Google Scholar] [CrossRef]
- Abbott, L.M.; Soyer, H.P. A CLOSE-UP guide to capturing clinical images. Australas. J. Dermatol. 2020, 61, 353–354. [Google Scholar] [CrossRef]
- Hampton, P.; Richardson, D.; Brown, S.; Goodhead, C.; Montague, K.; Olivier, P. Usability testing of MySkinSelfie: A mobile phone application for skin self-monitoring. Clin. Exp. Dermatol. 2020, 45, 73–78. [Google Scholar] [CrossRef]
- Yotsu, R.R.; Itoh, S.; Yao, K.A.; Kouadio, K.; Ugai, K.; Koffi, Y.D.; Almamy, D.; Vagamon, B.; Blanton, R.E. The Early Detection and Case Management of Skin Diseases With an mHealth App (eSkinHealth): Protocol for a Mixed Methods Pilot Study in Côte d’Ivoire. JMIR Res. Protoc. 2022, 11, e39867. [Google Scholar] [CrossRef] [PubMed]
- Dusendang, J.R.; Marwaha, S.; Alexeeff, S.E.; Crowley, E.; Haiman, M.; Pham, N.; Tuerk, M.J.; Wudka, D.; Hartmann, M.; Herrinton, L.J. Association of teledermatology workflows with standardising co-management of rashes by primary care physicians and dermatologists. J. Telemed. Telecare 2022, 28, 182–187. [Google Scholar] [CrossRef]
- Gimeno-Vicente, M.; Alfaro-Rubio, A.; Gimeno-Carpio, E. Teledermatology by WhatsApp in Valencia: Characteristics of Remote Consultation and Its Emotional Impact on the Dermatologist. Actas Dermosifiliogr. 2020, 111, 364–380, (In English and In Spanish). [Google Scholar] [CrossRef] [PubMed]
- Han, B.; Jhaveri, R.H.; Wang, H.; Qiao, D.; Du, J. Application of Robust Zero-Watermarking Scheme Based on Federated Learning for Securing the Healthcare Data. IEEE J. Biomed. Health Inform. 2021, 27, 804–813. [Google Scholar] [CrossRef]
- Zhang, J.; Mihai, C.; Tüshaus, L.; Scebba, G.; Distler, O.; Karlen, W. Wound Image Quality from a Mobile Health Tool for Home-Based Chronic Wound Management with Real-Time Quality Feedback: Randomized Feasibility Study. JMIR mHealth uHealth 2021, 9, e26149. [Google Scholar] [CrossRef] [PubMed]
- Chin, Y.P.H.; Huang, I.H.; Hou, Z.Y.; Chen, P.Y.; Bassir, F.; Wang, H.H.; Lin, Y.T.; Li, Y.C.J. User satisfaction with a smartphone-compatible, artificial intelligence-based cutaneous pigmented lesion evaluator. Comput. Methods Programs Biomed. 2020, 195, 105649. [Google Scholar] [CrossRef]
- Tognetti, L.; Cartocci, A.; Balistreri, A.; Cataldo, G.; Cinotti, E.; Moscarella, E.; Farnetani, F.; Lallas, A.; Tiodorovic, D.; Carrera, C.; et al. The Comparative Use of Multiple Electronic Devices in the Teledermoscopic Diagnosis of Early Melanoma. Telemed. J. e-Health 2021, 27, 495–502. [Google Scholar] [CrossRef]
- Peracca, S.B.; Fonseca, A.S.; Lachica, O.; Jackson, G.L.; Morris, I.J.; King, H.A.; Misitzis, A.; Whited, J.D.; Mohr, D.C.; Lamkin, R.P.; et al. Organizational Readiness for Patient-Facing Mobile Teledermatology to Care for Established Veteran Patients in the United States. Telemed. J. e-Health 2023, 29, 72–80. [Google Scholar] [CrossRef]
- Trinh, P.; Yekrang, K.; Phung, M.; Pugliese, S.; Chang, A.L.S.; Bailey, E.E.; Ko, J.M.; Sarin, K.Y. Partnering with a senior living community to optimise teledermatology via full body skin screening during the COVID-19 pandemic: A pilot programme. Ski. Health Dis. 2022, 2, e141. [Google Scholar] [CrossRef]
- Veronese, F.; Tarantino, V.; Zavattaro, E.; Biacchi, F.; Airoldi, C.; Salvi, M.; Seoni, S.; Branciforti, F.; Meiburger, K.M.; Savoia, P. Teledermoscopy in the Diagnosis of Melanocytic and Non-Melanocytic Skin Lesions: NurugoTM Derma Smartphone Microscope as a Possible New Tool in Daily Clinical Practice. Diagnostics 2022, 12, 1371. [Google Scholar] [CrossRef]
- Huang, K.; Wu, X.; Li, Y.; Lv, C.; Yan, Y.; Wu, Z.; Zhang, M.; Huang, W.; Jiang, Z.; Hu, K.; et al. Artificial Intelligence–Based Psoriasis Severity Assessment: Real-world Study and Application. J. Med. Internet Res. 2023, 25, e44932. [Google Scholar] [CrossRef]
- Veronese, F.; Branciforti, F.; Zavattaro, E.; Tarantino, V.; Romano, V.; Meiburger, K.M.; Salvi, M.; Seoni, S.; Savoia, P. The Role in Teledermoscopy of an Inexpensive and Easy-to-Use Smartphone Device for the Classification of Three Types of Skin Lesions Using Convolutional Neural Networks. Diagnostics 2021, 11, 451. [Google Scholar] [CrossRef] [PubMed]
- Damsin, T.; Canivet, G.; Jacquemin, P.; Seidel, L.; Gillet, P.; Giet, D.; Nikkels, A.F. Value of Teledermoscopy in Primary Healthcare Centers: Preliminary Results of the TELESPOT Project in Belgium. Dermatol. Ther. 2020, 10, 1405–1413. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, T.; Prasad, S.; Schuster, A.; Laurinaviciene, R.; Andersen, M.; Bygum, A. Diagnostic accuracy and interobserver concordance: Teledermoscopy of 600 suspicious skin lesions in Southern Denmark. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1601–1608. [Google Scholar] [CrossRef] [PubMed]
- Sondermann, W.; Von Kalle, C.; Utikal, J.S.; Schadendorf, D.; Esser, S.; Durani, B.; Durani, H.; Jansen, M.; Brinker, T.J. Externe wissenschaftliche Evaluation der ersten Teledermatologie-App ohne direkten Patientenkontakt in Deutschland (“Online Hautarzt–AppDoc”) [External scientific evaluation of the first teledermatology app without direct patient contact in Germany (Online Dermatologist-AppDoc)]. Hautarzt 2020, 71, 887–897. [Google Scholar] [CrossRef]
- Cronin, A.; Tkaczyk, E.R.; Hussain, I.; Bowden, A.; Saknite, I. Effect of camera distance and angle on color of diverse skin tone-based standards in smartphone photos. J. Biophotonics 2023, 16, e202200381. [Google Scholar] [CrossRef]
- Alipour, J.; Hayavi-Haghighi, M.H. Opportunities and Challenges of Telehealth in Disease Management during COVID-19 Pandemic: A Scoping Review. Appl. Clin. Inform. 2021, 12, 864–876. [Google Scholar] [CrossRef]
- Giansanti, D.; Morone, G.; Loreti, A.; Germanotta, M.; Aprile, I. A Narrative Review of the Launch and the Deployment of Telemedicine in Italy during the COVID-19 Pandemic. Healthcare 2022, 10, 415. [Google Scholar] [CrossRef]
- Vazquez, T.; Forouzandeh, M.; Sisk, M.; Florez-White, M.; Nouri, K. The modern-day moulage: Incorporating three-dimensional scanning and printing to enhance dermatology education and teledermatology. J. Eur. Acad. Dermatol. Venereol. 2019, 33, e383–e384. [Google Scholar] [CrossRef]
- Ladd, R.; Becevic, M.; Misterovich, H.; Edison, K. Dermatology ECHO: A case presentation demonstrating benefits of specialty telementoring in primary care. J. Telemed. Telecare 2019, 25, 506–509. [Google Scholar] [CrossRef]
- Benedetto, A.V. Travel as a teaching and learning tool. Clin. Dermatol. 2019, 37, 29–37. [Google Scholar] [CrossRef]
- Zheng, Y.; Lin, Y.; Cui, Y. Teledermatology in China: History, Current Status, and the Next Step. J. Investig. Dermatol. Symp. Proc. 2018, 19, S71–S73. [Google Scholar] [CrossRef]
- van Deursen, A.J.; van Dijk, J.A. The first-level digital divide shifts from inequalities in physical access to inequalities in material access. New Media Soc. 2019, 21, 354–375. [Google Scholar] [CrossRef] [PubMed]
- Neter, E.; Brainin, E.; Baron-Epel, O. Group differences in health literacy are ameliorated in ehealth literacy. Health Psychol. Behav. Med. 2021, 9, 480–497. [Google Scholar] [CrossRef] [PubMed]
- Giansanti, D.; Veltro, G. The Digital Divide in the Era of COVID-19: An Investigation into an Important Obstacle to the Access to the mHealth by the Citizen. Healthcare 2021, 9, 371. [Google Scholar] [CrossRef] [PubMed]
- Giansanti, D. The Artificial Intelligence in Digital Pathology and Digital Radiology: Where Are We? Healthcare 2020, 9, 30. [Google Scholar] [CrossRef]
- Giansanti, D. The Artificial Intelligence in Teledermatology: A Narrative Review on Opportunities, Perspectives, and Bottlenecks. Int. J. Environ. Res. Public Health 2023, 20, 5810. [Google Scholar] [CrossRef]
- Baashar, Y.; Alkawsi, G.; Ahmad, W.N.W.; Alomari, M.A.; Alhussian, H.; Tiong, S.K. Towards Wearable Augmented Reality in Healthcare: A Comparative Survey and Analysis of Head-Mounted Displays. Int. J. Environ. Res. Public Health 2023, 20, 3940. [Google Scholar] [CrossRef]
- Seo, Y.J.; Kwon, K.H. An application of AR in cosmetological industry after coronavirus disease-19 pandemic. J. Cosmet. Dermatol. 2022, 21, 5314–5320. [Google Scholar] [CrossRef]
- Ryan, G.V.; Callaghan, S.; Rafferty, A.; Higgins, M.F.; Mangina, E.; McAuliffe, F. Learning Outcomes of Immersive Technologies in Health Care Student Education: Systematic Review of the Literature. J. Med. Internet Res. 2022, 24, e30082. [Google Scholar] [CrossRef]
- Miller, A.C.; Blalock, T.W. Augmented reality: A novel means of measurement in dermatology. J. Med. Eng. Technol. 2021, 45, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Elder, A.; Ring, C.; Heitmiller, K.; Gabriel, Z.; Saedi, N. The role of artificial intelligence in cosmetic dermatology—Current, upcoming, and future trends. J. Cosmet. Dermatol. 2021, 20, 48–52. [Google Scholar] [CrossRef]
- Obagi, Z.A.; Rundle, C.W.; Dellavalle, R.P. Widening the scope of virtual reality and augmented reality in dermatology. Dermatol. Online J. 2020, 26, 13030/qt6mz1s20x. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Vleugels, R.A.; Nambudiri, V.E. Augmented reality in dermatology: Are we ready for AR? J. Am. Acad. Dermatol. 2019, 81, 1216–1222. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, B.; Badawy, S.M. Using Google Glass in Nonsurgical Medical Settings: Systematic Review. JMIR mHealth uHealth 2017, 5, e159. [Google Scholar] [CrossRef]
- Liu, Y.; Pharr, M.; Salvatore, G.A. Lab-on-Skin: A Review of Flexible and Stretchable Electronics for Wearable Health Monitoring. ACS Nano 2017, 11, 9614–9635. [Google Scholar] [CrossRef]
- Shin, J.; Wang, H.; Kwon, K.; Ostojich, D.; Christiansen, Z.; Berkovich, J.; Park, Y.; Li, Z.; Lee, G.; Nasif, R.; et al. Wireless, Soft Sensors of Skin Hydration with Designs Optimized for Rapid, Accurate Diagnostics of Dermatological Health. Adv. Health Mater. 2023, 12, e2202021. [Google Scholar] [CrossRef]
- Disclaime Spinazze, P.; Bottle, A.; Car, J. Digital Health Sensing for Personalized Dermatology. Sensors 2019, 19, 3426. [Google Scholar] [CrossRef]
- Griffies, J.D.; Zutty, J.; Sarzen, M.; Soorholtz, S. Wearable sensor shown to specifically quantify pruritic behaviors in dogs. BMC Veter-Res. 2018, 14, 124. [Google Scholar] [CrossRef]
- Giansanti, D.; Maccioni, G. Development and testing of a wearable Integrated Thermometer sensor for skin contact thermography. Med. Eng. Phys. 2007, 29, 556–565. [Google Scholar] [CrossRef]
- Giansanti, D. Improving spatial resolution in skin-contact thermography: Comparison between a spline based and linear interpolation. Med. Eng. Phys. 2008, 30, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Giansanti, D.; Maccioni, G.; Bernhardt, P. Toward the Design of a Wearable System for Contact Thermography in Telemedicine. Telemed. J. e-Health 2009, 15, 290–295. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giansanti, D. Advancing Dermatological Care: A Comprehensive Narrative Review of Tele-Dermatology and mHealth for Bridging Gaps and Expanding Opportunities beyond the COVID-19 Pandemic. Healthcare 2023, 11, 1911. https://doi.org/10.3390/healthcare11131911
Giansanti D. Advancing Dermatological Care: A Comprehensive Narrative Review of Tele-Dermatology and mHealth for Bridging Gaps and Expanding Opportunities beyond the COVID-19 Pandemic. Healthcare. 2023; 11(13):1911. https://doi.org/10.3390/healthcare11131911
Chicago/Turabian StyleGiansanti, Daniele. 2023. "Advancing Dermatological Care: A Comprehensive Narrative Review of Tele-Dermatology and mHealth for Bridging Gaps and Expanding Opportunities beyond the COVID-19 Pandemic" Healthcare 11, no. 13: 1911. https://doi.org/10.3390/healthcare11131911
APA StyleGiansanti, D. (2023). Advancing Dermatological Care: A Comprehensive Narrative Review of Tele-Dermatology and mHealth for Bridging Gaps and Expanding Opportunities beyond the COVID-19 Pandemic. Healthcare, 11(13), 1911. https://doi.org/10.3390/healthcare11131911




