Racial/Ethnic Patterns in Opioid Dispensing among Medicaid-Funded Young Children
Abstract
1. Introduction
- Whether the rates of opioid dispensing are different across race/ethnicity groups at any point in time, for each of the two diagnoses studied;
- Whether the gaps in opioid prescribing changed over time among race/ethnicity groups, again for each of the two diagnoses studied.
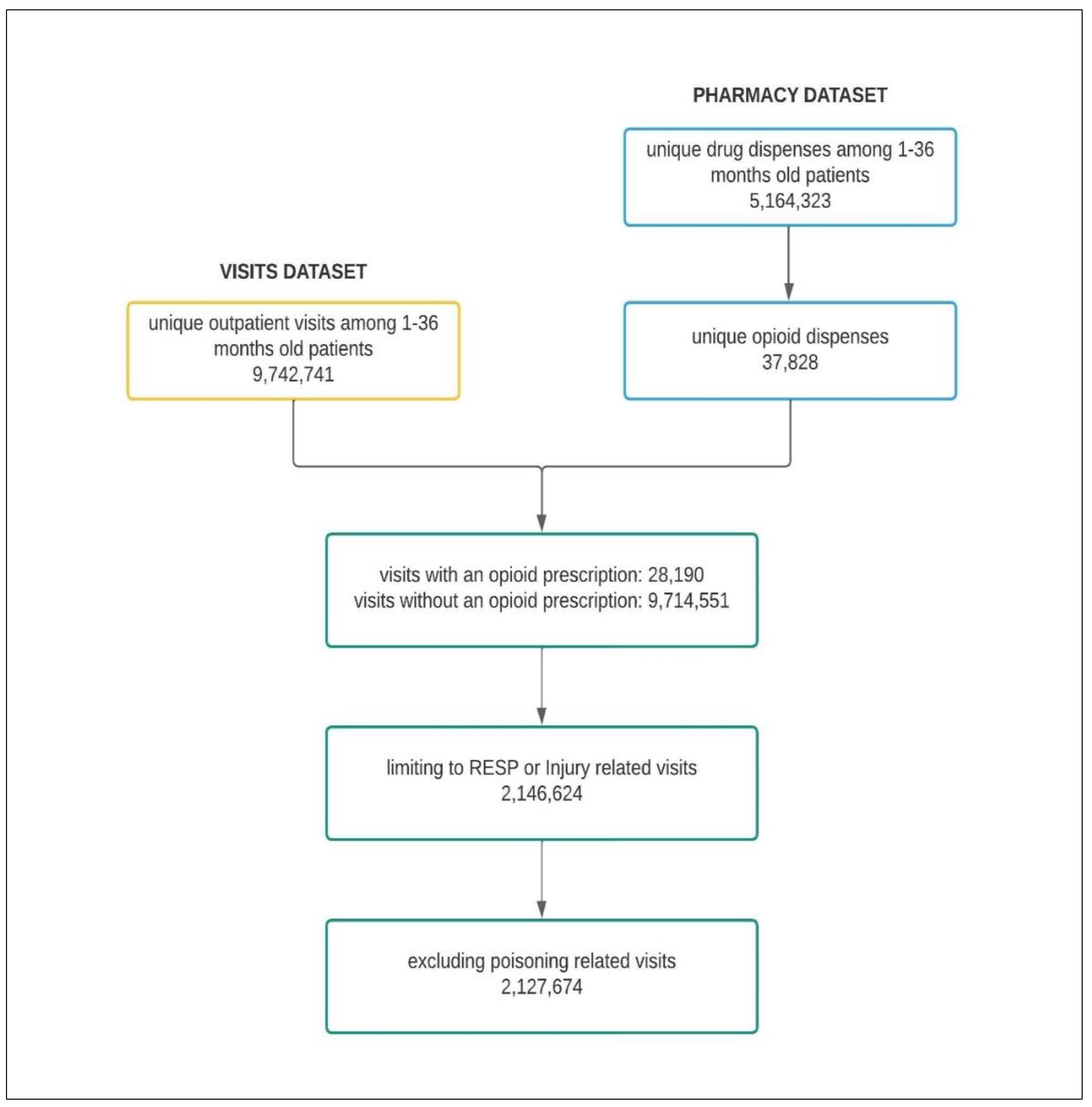
2. Materials and Methods
2.1. Study Population
2.2. Case Identification
2.3. Statistical Analysis
(Number of opioid prescriptions linked to the race/ethnic group for a diagnostic category per 3-year period) × 1000/
(Number of visits related to the race/ethnic group for a diagnostic category per 3-year period)
3. Results
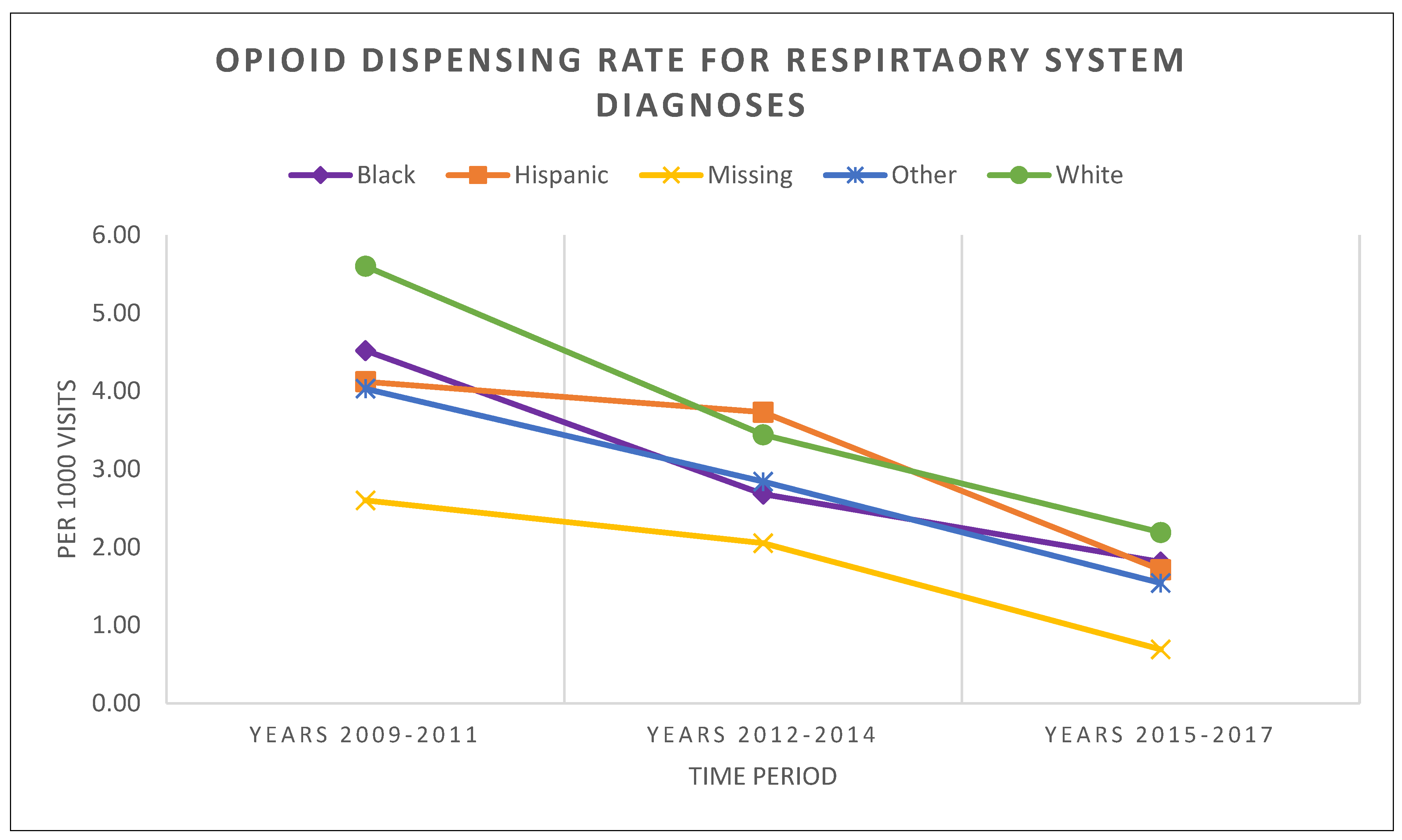
3.1. Opioid Dispensing Patterns in the Diseases of the Respiratory System
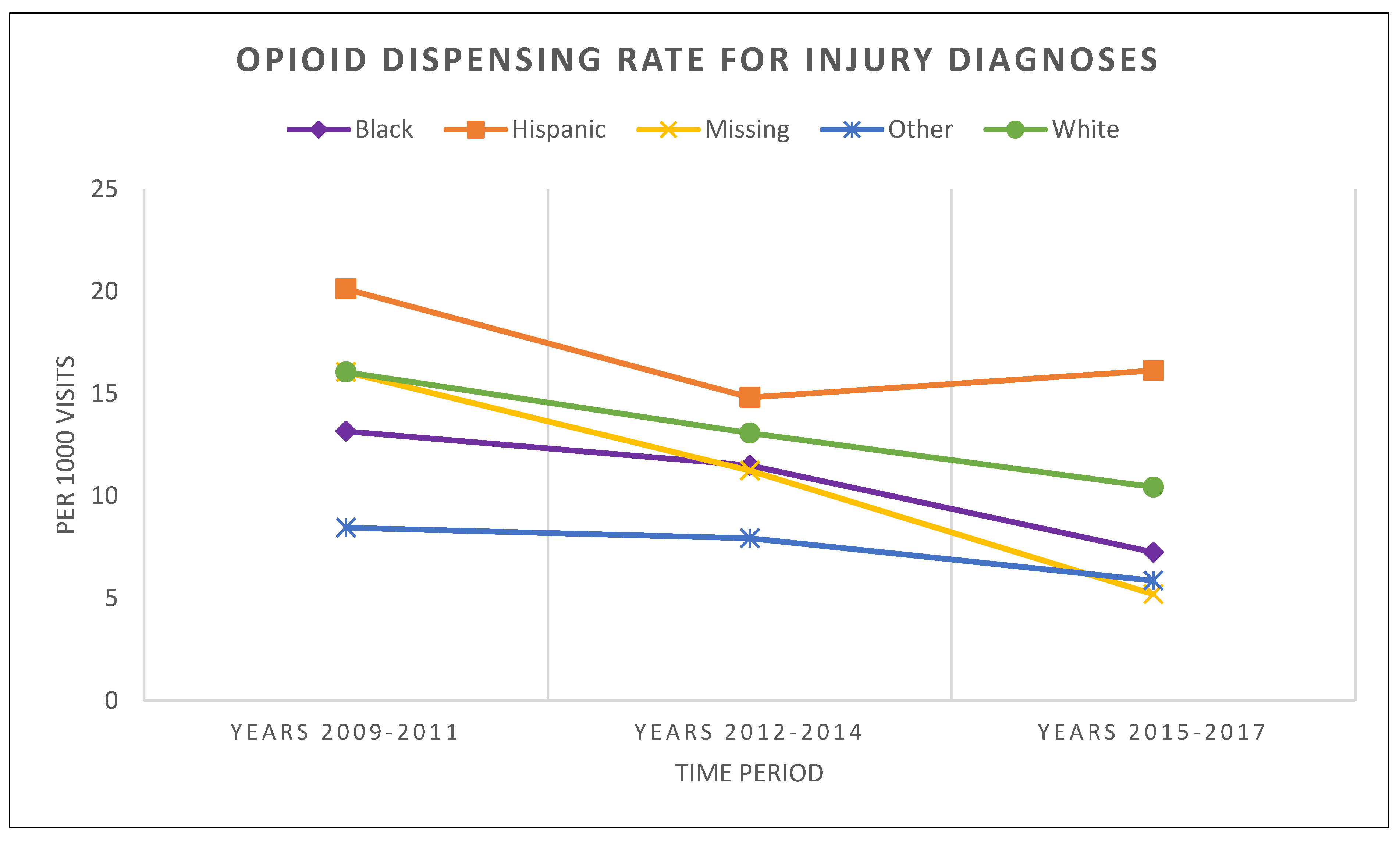
3.2. Opioid Dispensing Patterns in Injury Conditions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Race/Ethnic Group | RESP | INJURY | ||
|---|---|---|---|---|
| Second Period vs. First | Third Period vs. Second | Second Period vs. First | Third Period vs. Second | |
| White | <0.001 | <0.001 | <0.001 | 0.004 |
| Black | <0.001 | <0.001 | 0.040 | <0.001 |
| Hispanic | 0.270 | <0.001 | 0.017 | 0.640 |
| Other | <0.001 | <0.001 | 0.626 | 0.102 |
| Missing | 0.649 | <0.001 | 0.499 | <0.001 |
| Time Period | Compared to White | Compared to Black | Compared to Hispanic | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Black | Hispanic | Other | Missing * | Hispanic | Other | Missing | Other | Missing | |
| First period: 2012–2014 | <0.001 | <0.001 | <0.001 | 0.161 | 0.156 | 0.058 | 0.263 | 0.779 | 0.356 |
| Second period: 2012–2014 | <0.001 | 0.300 | 0.012 | 0.003 | <0.001 | 0.455 | 0.124 | 0.005 | 0.001 |
| Third period: 2015–2017 | 0.059 | 0.198 | 0.015 | <0.001 | 0.778 | 0.288 | <0.001 | 0.636 | <0.001 |
| Time Period | Compared to White | Compared to Black | Compared to Hispanic | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Black | Hispanic | Other | Missing * | Hispanic | Other | Missing | Other | Missing | |
| First period: 2012–2014 | <0.001 | 0.012 | <0.001 | 0.999 | <0.001 | <0.001 | 0.689 | <0.001 | 0.653 |
| Second period: 2012–2014 | 0.045 | 0.246 | <0.001 | 0.430 | 0.021 | <0.001 | 0.909 | <0.001 | 0.191 |
| Third period: 2015–2017 | 0.001 | 0.008 | <0.001 | <0.001 | <0.001 | 0.246 | 0.003 | <0.001 | <0.001 |
References
- Groenewald, C.B.; Rabbitts, J.A.; Gebert, J.T.; Palermo, T.M. Trends in opioid prescriptions among children and adolescents in the United States. Pain 2016, 157, 1021–1027. [Google Scholar] [CrossRef]
- Winkelman, T.N.A.; Villapiano, N.; Kozhimannil, K.B.; Davis, M.M.; Patrick, S.W. Incidence and costs of neonatal abstinence syndrome among infants with Medicaid: 2004–2014. Pediatrics 2018, 141, e20173520. [Google Scholar] [CrossRef] [PubMed]
- Conradt, E.; Flannery, T.; Aschner, J.L.; Annett, R.D.; Croen, L.A.; Duarte, C.S.; Friedman, A.M.; Guille, C.; Hedderson, M.M.; Hofheimer, J.A.; et al. Prenatal opioid exposure: Neurodevelopmental Consequences and Future Research Priorities. Pediatrics 2019, 144, e20190128. [Google Scholar] [CrossRef] [PubMed]
- Tobias, J.D.; Green, T.P.; Coté, C.J. Codeine: Time to say no. Pediatrics 2016, 138, e20162396. [Google Scholar] [CrossRef]
- Tadros, A.; Layman, S.M.; Davis, S.M.; Bozeman, R.; Davidov, D.M. Emergency department visits by pediatric patients for poisoning by prescription opioids. AJDAA 2016, 42, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Gaither, J.R.; Shabanova, V.; Leventhal, J.M. US National Trends in Pediatric Deaths From Prescription and Illicit Opioids, 1999–2016. JAMA Netw. Open 2018, 1, e186558. [Google Scholar] [CrossRef] [PubMed]
- Sachdeva, D.K.; Stadnyk, J.M. Are one or two dangerous? Opioid exposure in toddlers. J. Emerg. Med. 2005, 29, 77–84. [Google Scholar] [CrossRef]
- Chung, C.P.; Callahan, S.T.; Cooper, W.O.; Dupont, W.D.; Murray, K.T.; Franklin, A.D.; Hall, K.; Dudley, J.A.; Stein, C.M.; Ray, W.A. Outpatient opioid prescriptions for children and opioid-Related adverse events. Pediatrics 2017, 142, e20172156. [Google Scholar] [CrossRef]
- FDA Drug Safety Communication: FDA Requires Labeling Changes for Prescription Opioid Cough and Cold Medicines to Limit Their Use to Adults 18 Years and Older|FDA. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-requires-labeling-changes-prescription-opioid-cough-and-cold (accessed on 2 April 2023).
- Kuehn, B.M. FDA Committee: More Restrictions Needed on Hydrocodone Combination Products. JAMA 2013, 309, 862. [Google Scholar] [CrossRef]
- Kids and Pain: FDA Considers Rules for Pediatric Opioid Trials|MedPage Today. Available online: https://www.medpagetoday.com/painmanagement/painmanagement/60261 (accessed on 9 March 2023).
- Sivaraj, L.B.M.; Basco, W.T.; Heavner, S.F.; Lopes, S.S.; Rolke, L.; Shi, L.; Truong, K. Outpatient Opioid Dispensing Patterns for SC Medicaid Children 1–36 Months Old. Matern. Child Health J. 2023, 27, 1043–1050. [Google Scholar] [CrossRef]
- Basco, W.T.; McCauley, J.L.; Zhang, J.; Mauldin, P.D.; Simpson, K.N.; Heidari, K.; Marsden, J.E.; Ball, S.J. Trends in dispensed opioid analgesic prescriptions to children in South Carolina: 2010–2017. Pediatrics 2021, 147, e20200649. [Google Scholar] [CrossRef]
- Basco, W.T.; Roberts, J.R.; Ebeling, M.; Garner, S.S.; Hulsey, T.C.; Simpson, K. Indications for Use of Combination Acetaminophen/Opioid Drugs in Infants < 6 months old. Clin. Pediatr. 2018, 57, 741–744. [Google Scholar] [CrossRef]
- Berlin, J.; McCarver-May, D.G.; Notterman, D.A.; Ward, R.M.; Weismann, D.N.; Wilson, G.S.; Wilson, J.T.; March, J.; Bennett, D.R.; Hoskins, I.A.; et al. Use of Codeine- and dextromethorphan-containing cough remedies in children. Pediatrics 1997, 99, 918–920. [Google Scholar] [CrossRef]
- Schechter, N.L.; Walco, G.A. The potential impact on children of the CDC guideline for prescribing opioids for chronic pain: Above all, do no harm. JAMA Pediatr. 2016, 170, 425–426. [Google Scholar] [CrossRef] [PubMed]
- Califf, R.M.; Woodcock, J.; Ostroff, S. A Proactive Response to Prescription Opioid Abuse. N. Engl. J. Med. 2016, 374, 1480–1485. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Drendel, A.L.; Kircher, J.; Beno, S. Pain management of musculoskeletal injuries in children: Current state and future directions. Pediatr. Emerg. Care 2010, 26, 518–528. [Google Scholar] [CrossRef]
- Singhal, A.; Tien, Y.; Hsia, R.Y. Racial-Ethnic Disparities in Opioid Prescriptions at Emergency Department Visits for Conditions Commonly Associated with Prescription Drug Abuse. PLoS ONE 2016, 11, e0159224. [Google Scholar] [CrossRef]
- Rambachan, A.; Fang, M.C.; Prasad, P.; Iverson, N. Racial and Ethnic Disparities in Discharge Opioid Prescribing From a Hospital Medicine Service. J. Hosp. Med. 2021, 16, 589–595. [Google Scholar] [CrossRef]
- Pletcher, M.J.; Kertesz, S.G.; Kohn, M.A.; Gonzales, R. Trends in Opioid Prescribing by Race/Ethnicity for Patients Seeking Care in US Emergency Departments. JAMA 2008, 299, 70–78. [Google Scholar] [CrossRef]
- Joynt, M.; Train, M.K.; Robbins, B.W.; Halterman, J.S.; Caiola, E.; Fortuna, R. The impact of neighborhood socioeconomic status and race on the prescribing of opioids in emergency departments throughout the United States. J. Gen. Intern. Med. 2013, 28, 1604–1610. [Google Scholar] [CrossRef]
- Ly, D.P. Racial and ethnic disparities in the evaluation and management of pain in the outpatient setting, 2006–2015. Pain Med. 2019, 20, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Mossey, J.M. Defining racial and ethnic disparities in pain management. Clin. Orthop. Relat. Res. 2011, 469, 1859–1870. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.O.; Green, C.R.; Payne, R. Racial and ethnic disparities in pain: Causes and consequences of unequal care. J. Pain 2009, 10, 1187–1204. [Google Scholar] [CrossRef] [PubMed]
- Lopes, S.S.; Shi, L.; Sivaraj, L.B.; Truong, K.; Rolke, L.; Heavner, S.F.; Basco, W.T. Dispensed Opioid Prescription Patterns, by Racial/Ethnic Groups, Among South Carolina Medicaid-Funded Children Experiencing Limb Fracture Injuries. Acad. Pediatr. 2022, 22, 631–639. [Google Scholar] [CrossRef]
- Liao, L.; Reyes, L. Evaluating for racial differences in pain management of long-bone fractures in a pediatric rural population. Pediatr. Emerg. Care 2021, 37, 348–351. [Google Scholar] [CrossRef]
- Groenewald, C.B.; Rabbitts, J.A.; Hansen, E.E.; Palermo, T.M. Racial differences in opioid prescribing for children in the United States. Pain 2018, 159, 2050–2057. [Google Scholar] [CrossRef] [PubMed]
- Rasooly, I.R.; Mullins, P.M.; Mazer-Amirshahi, M.; van den Anker, J.; Pines, J.M. The impact of race on analgesia use among pediatric emergency department patients. J. Pediatr. 2014, 165, 618–621. [Google Scholar] [CrossRef]
- Goyal, M.K.; Kuppermann, N.; Cleary, S.D.; Teach, S.J.; Chamberlain, J.M. Racial disparities in pain management of children with appendicitis in Emergency Departments. JAMA Pediatr. 2015, 169, 996–1002. [Google Scholar] [CrossRef]
- Johnson, T.J.; Weaver, M.D.; Borrero, S.; Davis, E.M.; Myaskovsky, L.; Zuckerbraun, N.S.; Kraemer, K.L. Association of race and ethnicity with management of abdominal pain in the emergency department. Pediatrics 2013, 132, e851–e858. [Google Scholar] [CrossRef]
- Ortega, H.W.; Velden, H.V.; Lin, C.W.; Reid, S. Race, ethnicity, and analgesia provision at discharge among children with long-bone fractures requiring emergency care. Pediatr. Emerg. Care 2013, 29, 492–497. [Google Scholar] [CrossRef]
- Goyal, M.K.; Johnson, T.J.; Chamberlain, J.M.; Cook, L.; Webb, M.; Drendel, A.L.; Alessandrini, E.; Bajaj, L.; Lorch, S.; Grundmeier, R.W.; et al. Racial and ethnic differences in emergency department pain management of children with fractures. Pediatrics 2020, 145, e20193370. [Google Scholar] [CrossRef] [PubMed]
- Al Shamsi, H.; Almutairi, A.G.; Al Mashrafi, S.; Kalbani, T.A. Implications of language barriers for healthcare: A systematic review. Oman. Med. J. 2020, 35, e122. [Google Scholar] [CrossRef] [PubMed]
- CDC’s Opioid Overdose Indicator Support Toolkit: Guidance for Building and Reporting on Opioid-Related Mortality, Morbidity, and PDMP Indicators; Version 2.0; CDC: Atlanta, GA, USA, 2018.
- IBM® Micromedex® RED BOOK® Data Sheet Comprehensive Drug Pricing and Product Information. Available online: https://www.ibm.com/products/micromedex-red-book/resources (accessed on 2 April 2023).
- Defalco, F.J.; Ryan, P.B.; Soledad Cepeda, M. Applying standardized drug terminologies to observational healthcare databases: A case study on opioid exposure. Health Serv. Outcomes Res. Methodol. 2013, 13, 58–67. [Google Scholar] [CrossRef]
- Phang, K.G.; Roberts, J.R.; Ebeling, M.; Garner, S.S.; Basco, W.T. Opioids or steroids for pneumonia or sinusitis. Pediatrics 2020, 146, e20193690. [Google Scholar] [CrossRef]
- Chua, K.P.; Shrime, M.G.; Conti, R.M. Effect of FDA investigation on opioid prescribing to children after tonsillectomy/adenoidectomy. Pediatrics 2017, 140, e20171765. [Google Scholar] [CrossRef] [PubMed]
- Clinical Classifications Software (CCS) for ICD-9-CM. Available online: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp (accessed on 2 April 2023).
- Kang, A.M.; Brooks, D.E. US poison control center calls for infants 6 months of age and younger. Pediatrics 2016, 137, e20151865. [Google Scholar] [CrossRef]
- Basco, W.T.; McCauley, J.L.; Zhang, J.; Marsden, J.E.; Simpson, K.N.; Heidari, K.; Mauldin, P.D.; Ball, S.J. High-risk opioid analgesic dispensing to adolescents 12–18 years old in South Carolina: 2010–2017. Pharmacoepidemiol. Drug Saf. 2022, 31, 353–360. [Google Scholar] [CrossRef]
- Groenewald, C.B. Opioid prescribing patterns for pediatric patients in the USA. Clin. J. Pain 2019, 35, 515–520. [Google Scholar] [CrossRef]
- Hudgins, J.D.; Porter, J.J.; Monuteaux, M.C.; Bourgeois, F.T. Trends in opioid prescribing for adolescents and young adults in ambulatory care settings. Pediatrics 2019, 143, e20181578. [Google Scholar] [CrossRef]
- Tomaszewski, D.M.; Arbuckle, C.; Yang, S.; Linstead, E. Trends in Opioid Use in Pediatric Patients in US Emergency Departments from 2006 to 2015. JAMA Netw Open 2018, 1, e186161. [Google Scholar] [CrossRef]
- McDonald, D.C.; Carlson, K.; Izrael, D. Geographic variation in opioid prescribing in the U.S. J. Pain 2012, 13, 988–996. [Google Scholar] [CrossRef] [PubMed]
- Ukert, B.; Huang, Y.; Sennett, B.; Delgado, K. State-level variation in opioid prescribing after knee arthroscopy among the opioid-naïve in the USA: 2015–2019. BMJ Open 2020, 10, e035126. [Google Scholar] [CrossRef] [PubMed]
- Schieber, L.Z.; Guy, G.P.; Seth, P. Trends and Patterns of Geographic Variation in Opioid Prescribing Practices by State, United States, 2006–2017. JAMA Netw. Open 2019, 2, e190665. [Google Scholar] [CrossRef] [PubMed]
| Race/Ethnicity Groups a | Number of Outpatient Visits (%) |
|---|---|
| White and Caucasian | 695,750 (32.70) |
| Black and African American | 655,025 (30.79) |
| Hispanic | 159,105 (7.48) |
| Asian | 7471 (0.35) |
| Federally Recognized Native American | 965 (0.05) |
| Native Hawaiian or Pacific | 404 (0.02) |
| Other Native American | 4163 (0.20) |
| Alaska | 21 (0.00) |
| Having more than one race | 14,264 (0.67) |
| Other/unknown | 214,287 (10.07) |
| Missing | 376,219 (17.68) |
| Baseline Characteristic | Total (n = 2,127,674) | RESP (n = 1,832,272) | INJURY (n = 295,402) |
|---|---|---|---|
| Opioid-related | 9059 (0.43) | 5752 (0.31) | 3307 (1.12) |
| Age (months) at outpatient visit: mean (SD) | 16.95 (10.18) | 16.47 (10.18) | 19.94 (9.69) |
| Gender: n (%) | |||
| Male | 1,167,807 (54.89) | 1,006,796 (54.95) | 161,011 (54.51) |
| Female | 959,834 (45.11) | 825,448 (45.05) | 134,386 (45.49) |
| Race/Ethnicity: n (%) | |||
| Non-Hispanic White and Caucasian | 695,750 (32.70) | 591,129 (32.26) | 104,621 (35.42) |
| Non-Hispanic Black and African American | 655,025 (30.79) | 564,227 (30.79) | 90,798 (30.74) |
| Hispanic | 159,105 (7.48) | 142,184 (7.76) | 16,921 (5.73) |
| Other a | 241,575 (11.35) | 204,741 (11.17) | 36,834 (12.47) |
| Missing | 376,219 (17.68) | 329,991 (18.01) | 46,228 (15.65) |
| Diagnostic Category | RESP | INJURY | |||||
|---|---|---|---|---|---|---|---|
| Time Period | 2009–2011 | 2012–2014 | 2015–2017 | 2009–2011 | 2012–2014 | 2015–2017 | |
| Race/ethnic group | White | 5.60 | 3.44 * | 2.19 * | 16.06 | 13.08 * | 10.44 * |
| Black | 4.52 a | 2.68 a,* | 1.81 * | 13.16 a | 11.49 a,* | 7.25 a,* | |
| Hispanic | 4.12 a | 3.73 b | 1.71 * | 20.12 a,b | 14.82 b,* | 16.13 a,b | |
| Other | 4.03 a | 2.84 a,c,* | 1.54 a,* | 8.45 a,b,c | 7.94 a,b,c | 5.86 a,c | |
| Missing | 2.60 | 2.05 a,c | 0.69 a,b,c,* | 16.06 | 11.24 | 5.20 a,b,c,* | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sivaraj, L.B.; Truong, K.; Basco, W.T., Jr. Racial/Ethnic Patterns in Opioid Dispensing among Medicaid-Funded Young Children. Healthcare 2023, 11, 1910. https://doi.org/10.3390/healthcare11131910
Sivaraj LB, Truong K, Basco WT Jr. Racial/Ethnic Patterns in Opioid Dispensing among Medicaid-Funded Young Children. Healthcare. 2023; 11(13):1910. https://doi.org/10.3390/healthcare11131910
Chicago/Turabian StyleSivaraj, Laksika B., Khoa Truong, and William T. Basco, Jr. 2023. "Racial/Ethnic Patterns in Opioid Dispensing among Medicaid-Funded Young Children" Healthcare 11, no. 13: 1910. https://doi.org/10.3390/healthcare11131910
APA StyleSivaraj, L. B., Truong, K., & Basco, W. T., Jr. (2023). Racial/Ethnic Patterns in Opioid Dispensing among Medicaid-Funded Young Children. Healthcare, 11(13), 1910. https://doi.org/10.3390/healthcare11131910







