1. Introduction
At the level of the European Union, the demographic aging process has registered an upward curve in the last two decades due to some contextual factors of increasing the quality of life of the population and, for this reason, the share of elderly people in the total population is quite high. The situation is similar for Romania, the statistical situations provided by [
1] highlighting the fact that 19% of the total population is represented by the over-65 population category [
2,
3].
The aging process involves two essential aspects that are closely related: on the one hand, biological aging and, on the other hand, quality of life [
4]. Some significant elements illustrated by [
5] for the quality of life of the elderly are functional capacity, intergenerational relationships, health status, standard of living, social support, independence status, the environment in which they live, spirituality and state of mental health [
6]. The stated elements present a different degree of importance for the elderly and, depending on their individualized needs and problems, the elements of the quality of life of this category can be perceived differently [
2]. A study highlights the fact that the health status of the elderly population in Romania is weaker compared to other categories of the elderly population in other more developed European states [
2].
Humanity has been subjected to unprecedented challenges, including the recent SARS-CoV-2 pandemic, even though, over time, appropriate treatments or solutions have been identified for many infectious diseases [
7]. The SARS-CoV-2 pandemic has generated several risks and difficulties globally, with the onset of this pandemic reported in China in 2019 and the rapid spread of the pandemic to 118,000 cases globally in 114 countries after only 2 months of its emergence [
2,
8,
9]. The first confirmed case in Romania was registered on 26 February 2020 [
10,
11] and by 1 November 2021, 1,648,031 Romanians had been diagnosed with coronavirus, from which 47,751 died and 1,405,694 recovered [
12,
13].
The most exposed age group to illnesses was the age group between 50 and 59 years old, highlighting the fact that over 85% of the deaths in Romania during the pandemic period were registered in elderly people over 60 years old with comorbidities [
14].
Romania was extremely affected by the COVID-19 pandemic situation in terms of the rate of illness and mortality per 100 thousand inhabitants [
15]. Thus, the COVID-19 pandemic constituted one of the major challenges at the global, European and national levels. A social category extremely affected by the pandemic generated by COVID-19 was the category of elderly people. The present work brings to the fore the elderly, their characteristics and lifestyle during the pandemic and how the mass media had a major influencing role during the pandemic that influenced the lives of these people. Hence, the purpose of our paper was to analyze the ways in which mass media, and very often contradictory information flows, influenced the life and personal communications of the Romanian elderly population during the COVID-19 pandemic.
The complexity of this work is determined, on the one hand, by the theoretical approach to some aspects related to the pandemic situation generated by COVID-19 in Romania and its implications for the elderly in various aspects of life, to the aging process, to the existing multiple stressors and implicitly understanding the resilience capacity and coping mechanisms of the elderly during the pandemic period, to the role of the mass media in influencing the quality of life of the elderly. On the other hand, the applied research carried out at the national level completes the information, bringing added value to this field with a quantitative–qualitative mixed analysis and interpretation part that illustrates how the media communication channels have left their mark on the various aspects of the life of the elderly, the perception of the elderly on their own mental and emotional health or social relationships and how they were affected by the pandemic generated by COVID-19. In addition, another important aspect monitored was the perception regarding the life of the elderly in the pandemic period, in family, social and medical terms and the problems encountered, as well as the methods of support they received. On 2 November 2021, Romania was the second-least vaccinated state of the European Union, even though a record number of daily deaths from the coronavirus were reported and there were no intensive care beds available in Romania [
16].
The emergence of COVID-19 has resulted in an unprecedented disruption of both physical and mental health among the world’s citizens. In [
17,
18], among other effects generated by this, the upward dynamics of social uncertainty and distrust in public institutions are highlighted [
2]. A broader time perspective is needed to perceive the effects of the pandemic on the population [
19]. The pandemic situation caused the emergence of a social and medical crisis with major implications for the vulnerable category of the elderly [
7].
Regarding the measures to prevent the spread of the virus, Romania had to apply a strategic plan to control and prevent the expansion of the pandemic situation either through certain measures to restrict access to air flights, the closure of certain public or private institutions and large stores, the mandatory self-quarantine of affected persons being introduced or other preventive hygiene measures to prevent the spread of the virus [
11].
In order to prevent the spread of the virus, and at the level of elderly beneficiaries of social services, various legislative measures were applied to restrict access to these services [
7]. Another challenge for Romania was generated by the numerous demands of the elderly for care in social services caused by social, medical and economic factors: low incomes and pensions, high costs for medicines and food and increased costs of maintenance expenses [
20]. Other categories of social services affected by the pandemic situation were day, residential and home social services intended for the elderly, who had to readjust their intervention plans, procedures, methodologies or activities concerning the new crisis conditions generated by the pandemic [
21,
22]. The consequences of COVID-19 in residential social services have been devastating. Countries such as the United States, Spain and Italy had a high mortality rate among institutionalized elderly. The proximity between residents led to a higher risk of infection and, consequently, adverse outcomes and mortality associated with difficulties in preventing the spread of the virus in institutions [
23,
24,
25]. Clinicians and caregivers were prompted to estimate the availability of resources and consider how the absence of resources can be mitigated for a given individual and family. Of particular importance was the role of technology, which emerged as an important factor in maintaining social connectedness as well as accessing mental health services [
24].
Several studies [
26,
27] demonstrated that the older generation [
28] was affected to the highest degree compared to other vulnerable groups due to the higher risk of isolation, self-isolation and social exclusion associated with the high risk of contracting the disease and losing life [
22,
29,
30,
31,
32,
33] or with the risk of discrimination and manifestation of “ageist” attitudes [
34,
35,
36]. The factor of aging correlated with the factor of COVID-19 is worrisome, considering where studies present the risk of minimizing the value of an older adult’s life, both among healthcare providers and among the public [
37]. These findings are troubling, but also form the basis for understanding elder abuse. Rates of elder abuse have increased since the onset of the pandemic, and this type of abuse has been and is often unreported [
38].
The impact of the severe acute respiratory syndrome (SARS) on mental health [
39] among the public has been previously reported [
40], and recent systematic reviews are beginning to highlight the detrimental impact of COVID-19 on mental health among different populations [
41,
42,
43]. Social isolation measures are a “perfect storm” for mental illness [
44,
45,
46], in the elderly [
47]. Their daily social activities, such as walking and socializing, meeting friends, volunteering and religious gatherings, were restricted due to quarantine orders and transport controls. This exacerbated the challenges of the pandemic and had a severe impact on their mental health [
48,
49].
The COVID-19 pandemic induced worry [
50], fear [
51], anxiety and depressive symptoms [
52] as well as insomnia [
53]. While social distancing has shown positive effects in terms of the number of infections [
54], the sociopsychological consequences are quite discouraging. Social isolation increases the risk of mental health problems [
55,
56]. Policy measures calling for social distancing could therefore directly affect feelings of loneliness and depression [
45,
57]. In particular, the elderly and people living alone, who appear to be even more vulnerable to mental health problems, could be affected by these developments [
58,
59,
60]. Mental health problems themselves are known to be associated with an increased risk of long-term morbidity and mortality, particularly for older people [
61]. Moreover, social isolation in the elderly has been shown to lead to increased risks of cardiovascular [
62], autoimmune and neurocognitive [
63] disease. Fear of contracting the disease [
64] and losing loved ones constituted mental stress and generated anxiety in the elderly population [
65]. The negative impact of COVID-19 on mental health in the general population has been identified as a research priority [
42,
45,
46,
66,
67]. A study by [
68] reported a high prevalence of generalized anxiety disorder and poor sleep quality in Chinese individuals during the COVID-19 outbreak. Another study [
69] observed a higher prevalence of anxiety and depression in people affected by quarantine compared to those not affected by China’s quarantine measures in early February 2020. Krendl and Perry focus on older adults in the US [
70] and find that their mental health has been negatively affected by the COVID-19 pandemic. Respondents experienced higher levels of depression and loneliness than they had before the pandemic. Van Tilburg et al. found that the level of loneliness among elderly people in the Netherlands increased, while overall mental health remained roughly stable [
71]. The study shows that social distancing measures were not the main determinant for the increase in the prevalence of loneliness [
72].
In general, the socio-economic conditions that were imposed on the people en masse, the forced lockdown without provision of basic human needs, poor governance, communication, infrastructure and healthcare facilities, created public anxiety [
55] and disturbed human life [
73]. Given the immense burden of COVID-19 on older populations, it is critical to understand what have been effective coping strategies [
74]. Older adults use various coping strategies to deal with this crisis that draw our attention to the dynamic, changing and temporal dimensions of the coping process, especially regarding expectations about the duration of stressors as a way to enable the population to adapt to stressors [
75].
The deeper the interpersonal connection and interpersonal involvement, the more it favorably influences human resilience, and at the opposite pole, the state of fear and lack of certainty as well as loneliness represent impediments to reaching a reasonable level of resilience or in reaching individual well-being and health [
76].
Social engagement, which includes meaningful interactions and connection with others, is an essential stimulus needed for older people to improve their physical and mental health as individuals [
77,
78]. Positive social connections and relationships are considered to be an integral factor in the well-being of older people as social beings [
79].
Therefore, in the presence of this social imbalance, older adults are challenged to develop strategies to cope with such a situation [
77,
80]. These coping strategies are natural coping capacities known as internal resilience [
81] developed by an older person in response to the aging process and stressful life experiences such as the COVID-19 crisis [
77].
Coping strategies associated with managing the stress and anxiety of social isolation related to COVID-19 have not yet been widely studied [
82], especially among older adults [
83].
In reconfiguring a path of personal balance in the risk conditions generated by the stressors during the COVID pandemic period, it was necessary to draw up a coping strategy [
84]. Depending on individual adaptive resources, negative stressors can be counteracted and, implicitly, the activation of adaptive mechanisms to adverse events or illness [
85] or to the lack of self-efficacy [
86].
Each individual has a unique coping strategy in relation to their ability to psychologically adapt to the disease situation that leads to the management of the stressful situation [
87,
88,
89,
90,
91].
The stressor or risk factor in the present situation is the fear of infection with the COVID-19 virus. Coping ability is the central process in building resilience. The identified stressor is dangerous, so coping responses are activated. Resilience is the result of the interaction of elderly people with their environment and the processes that promote well-being or protect them against the overwhelming influence of the pandemic [
92]. These processes can be individual adaptation strategies or coping mechanisms or they can be stimulated and facilitate the emergence of resilience.
The notion of coping, currently used extremely frequently by specialists, signifies the association between an individual and the contextual life situation, an association that can lead to stress reduction but also signifies the mechanism that generates adaptation to the stressor [
93]. This coping mechanism aims at the transformation and adaptation of systemic segments to be able to respond adaptively to dynamic stimuli generated by external environmental factors [
94].
Lazarus and Folkman define the notion of coping as the behavioral or cognitive ability of the individual to manage external or internal demands in relation to the availability of individual resources [
85]. It is an adaptive reaction in response to actual or imagined stress to maintain psychological integrity [
95]. Within this concept, people are perceived as responding to stress through attack, fight or compromise reactions. These reactions become complicated due to the numerous coping mechanisms whenever the stressor involves the Ego.
Normally, defense mechanisms are used constructively in the coping process. Available coping mechanisms are what people usually use when they have a problem. The Great Pandemic of 2020 was a unique stressor that affected communities around the world [
39]. The nature of this contagion virus has led to mass fear and hysteria and many misconceptions, with widespread stigmatization and discrimination against those infected. Altogether, these perceptions have created immense stress among the population, but still, they are trying to cope with this situation. They try to learn coping strategies to adapt to these traumatic crises. To cope with a situation, a person tries to manage their external and internal demands that are perceived as demanding or exceeding adaptive resources [
96].
Coping acts as a stabilizing factor that can help the individual maintain psychological adaptation during a stressful period [
97]. Coping mechanisms can be divided into two categories: adaptive coping and maladaptive coping. The adaptive coping strategy usually benefits or positively affects the lives of those who use it. Ref. [
98] and some examples of this approach include religious/spiritual coping, such as prayer and scripture reading [
99]; exercise [
100]; meditation; music auditions and socializing with friends and family [
101].
The other form of coping, maladaptive coping, refers to methods that often lead to adverse consequences, including some mental health challenges. Previous research has divided maladaptive coping into two different categories: emotional, where individuals respond to a situation confrontationally or with an excessive emotional response, and avoidance-based, where individuals actively delay responding to a stressful situation or escape a situation altogether through isolation or other maladaptive behaviors [
98,
102,
103]. Maladaptive behaviors may include alcohol consumption [
104], tobacco [
105], drug use and overeating [
101] and other risk behaviors [
106]. Historically, these coping strategies can lead to negative effects on one’s life, including greater depression, greater pain and functional impairment, and lower self-efficacy [
107]. Thus, coping mechanisms can focus on the meaning, practical aspects, emotional aspects and avoidance aspects of a crisis. People differ greatly in their ability to successfully cope with stressful life events, and some coping strategies are much more effective than others when faced with a selected life-changing event [
108]. How one deals with a crisis has important implications for well-being. Effective coping leads a person to achieve better life satisfaction.
As for coping, it involves a process and several anticipatory, confrontational and analytical stages that lead to the reduction of the stressful situation. Therefore, coping can represent a stable personal predisposition [
109], but it is also seen as an evolutionary process, including genetically [
110,
111]. Theoretical perspectives on coping suggest that older age may be advantageous for coping due to the accumulation of life experiences that encourage the refinement of coping skills [
112,
113]. The process of coping with stress can build resilience, and for older adults, there is an increased likelihood that they have increased coping resources and strategies to draw upon from their experiences [
112,
114].
The COVID-19 pandemic presents a variety of stressors, including social distancing, but it is conceivable that older adults will apply their accumulated coping skills to cope. Coping strategies are essential factors that determine one’s well-being in old age [
115]. Coping strategies compensate for or mitigate stressful circumstances by reformulating and adapting to a new and positively evaluated environment [
81,
115].
Internal resilience theory proposes that in times of crisis, health needs to compel older people to develop internal resilience to preserve their integrity, well-being and quality of life as individuals [
81]. Internal resilience refers to the ability to adapt well in the face of adversity, danger, trauma or significant sources of stress, collectively known as a crisis, to sustain a sense of purpose and vigor and to emerge stronger from such stressful situations [
77,
81].
Regarding the forms of coping, a classic classification is delimited into problem-centered coping and emotion-centered coping [
85].
Emotion-focused coping is generally used by older people to adapt to stress [
116].
Coping is illustrated by Stone and Neale as being characterized by several factors such as acceptance, social support, direct action, relaxation and religious feelings [
117], and Folkman and Lazarus also complete the palette of specific factors with aspects related to self-control, distancing, confrontation, planning to remedy the problem or positive re-evaluation [
118].
Another study [
84] proposed a coping framework that describes the interconnections between characteristics of how individuals cope. Personal resources include characteristics of the individual such as dispositional coping style and characteristics such as cognitive and intellectual ability and general personality traits. These systems influence a cascade of processes that affect the psychosocial functioning and well-being of the individual. Thus, the authors of [
84] describe coping in two domains: coping styles and coping responses. Coping styles are relatively stable and describe how individuals typically interact with their environment, while coping responses are used by the individual to manage particularly stressful encounters [
80,
84].
Another study recorded the notion of locus of control, which he associated with those traits by which individuals express their success or failure through controllable or uncontrollable causes [
119]. The belief that the responsibility for success or failure is determined by the qualities or defects of the individual was named LCI-internal locus of control; in the same context, LCE was also identified, which signifies the belief that fate has a significant role in generating favorable or unfavorable events of life [
120]. The meaning of self-efficacy (AE) is also illustrated, as well as the belief in the mobilization of motivational and cognitive resources in the successful performance of certain tasks [
110]. The sense of coherence is structured from childhood and adolescence and is consolidated around the age of 30 and has three components: comprehension, control and purpose, and self-esteem. Thus, self-esteem correlates positively with adaptive coping strategies such as refocusing towards planning, refocusing positively and positive reappraisal and correlates negatively with maladaptive coping strategies such as self-blame, catastrophizing, rumination and blaming others [
121]. Optimism is a personal resource defined as a general expectation or belief that good things will happen frequently in the future, while bad things will happen only rarely [
122]. Perceived social support is defined as the perceived availability of support if needed. Studies indicate that optimism and perceived social support are effective resources for coping with adversity and challenges and may serve as a primary source of self-care and subjective well-being, especially in old age [
123,
124]. These latter variables are known to decrease well-being and increase the risk of depression and cognitive dysfunction. Another study pointed out that a decrease in activity and mobility in older adults during isolation can also lead to more frailty and lower well-being in older adults. Moreover, in response to stress, sleep quality may decrease and increase the risk of depression [
106].
Depression may be negatively associated with health-related quality of life. Studies have found that COVID-19 patients with depression reported lower health-related quality of life compared to those without depression [
125]. Similar findings have been found for other diseases such as diabetes [
126] and gastrointestinal diseases [
127]. The COVID-19 pandemic period has accelerated the risk and manifestations of depression, with depression influencing the ways to remedy or counteract individual problems or generating difficulties in achieving personal or professional goals, making recovery from the crisis even more difficult. Even if it manifests itself in different ways, at the base of depression there is always an attitude of giving up [
128].
Based on the above analysis, understanding the implications of COVID-19 restrictions on the health and well-being of older adults is of major importance [
129].
Depression is a common condition in older adults, being the second cause of global morbidity after cardiovascular diseases, and also having multifactorial origin. Depression has diverse clinical manifestations and is difficult to identify, which causes a decrease in the quality of life and an increase in suffering, often leading to fatal outcomes [
130,
131,
132].
Coping involves cognitive and behavioral strategies that individuals use to cope with or control stressful circumstances and can be influenced by several biological and psychosocial factors, including physical health, personality, spirituality and social support. Active coping involves behaviors to proactively address, modify or overcome a stressor or situation. Regulatory coping refers to reflecting on the stressor to reduce its effects, such as reframing a stressor or adapting through a change in attitude, expectation or perception. An individual may consciously or subconsciously use both types of strategies simultaneously [
71,
133]. Not all coping strategies are successful or helpful. Denial, for example, may not be the most appropriate response to a problem, but it is a cognitive coping strategy frequently used as people age [
134]. Aldwin’s five main categories [
135] are problem-focused coping (behaviors and cognitions oriented toward solving or managing a problem, such as implementing a plan), emotion-focused coping (managing the emotional reaction to the problem), social support coping (eliciting helping others or offering support to others), religious coping (seeking help from a higher power, such as through prayer) and cognitive reframing (trying to understand the problem and/or focusing on the positive aspects of the situation). Resilience is a multifaceted and important concept: high resilience in later life has been associated with reduced risk of depression and mortality, better self-perception of successful aging, increased quality of life and improved lifestyle [
136,
137,
138].
The mass media has an important role because it must provide correct information about the coping resources available to the elderly. The mass media can prepare the public to face the disaster, it can give warnings and information about coping strategies, it can provide a forum for public reactions and it can provide a report of the events. The substantial stress of “information overload” can lead to paranoia and mistrust of health care, which could lead one to avoid quarantine, with serious consequences for public health [
139].
Thus, the 2019 coronavirus (COVID-19) pandemic was a public health crisis that required interventions to reduce the spread of the disease, including social distancing and isolation [
140], generating stressful situations that challenged individuals’ coping skills. As older adults have been particularly encouraged to practice social distancing and self-quarantine, given their higher risk of hospitalization and mortality from COVID-19 [
141], it is important to understand how they adapted and coped with this social isolation [
83]. It is possible that, given their wealth of life experiences, older adults are uniquely able to adapt well during this unprecedented crisis [
142].
Moreover, recently published studies have also suggested that COVID-19 had a particularly significant impact on psychological well-being, including suffering from social deprivation due to isolation or quarantine, feeling stressed, experiencing anxiety [
143] or depression, or suicide in more serious cases [
144].
However, the consequences of self-isolation, such as separation from loved ones and friends, loss of usual routine, participation in fewer social activities and limited access to regular medical care can be distressing for individuals [
78].
Overcoming this situation requires the identification of effective factors in controlling and combating this epidemic in order to increase resistance to the virus and contribute to the social, economic and social development of the community [
145].
Variables Taken into Consideration in the Research
Considering the purpose of our paper, in our research we examined variables that referred to the sources of information of the elderly and their way of living during the pandemic. In this regard, the variables we examined refer to: type of media channels followed, type of information they have seen about the virus, people with whom the elderly talked most often about the virus, their trust in media channels, ways through which they verified information regarding the virus, ways of fighting/coping with the pandemic period, perception about their mental and emotional health, the means of communication that the elderly used in order to talk with friends and family members, the topics they discussed most, the main problems they have faced during the pandemic and the medical and social support they have received in the pandemic period.
6. Discussion and Conclusions
In the context of the pandemic, one of the categories that was most affected by the virus and by the measures implemented in order to stop the spread of the virus was represented by the elderly. In this regard, similarly to previous studies [
26,
27,
28], we argue that the older generation was affected by the virus to the highest degree compared to other vulnerable groups due to their risk of being isolated in order to protect their health.
The purpose of our paper was to analyze the ways in which mass media and very often contradictory information flows influenced the life and personal communications of the Romanian elderly during the COVID-19 pandemic. In this regard, in our paper, we were interested in identifying the media channels used by the Romanian elderly to get information about the pandemic, identifying the main types of information followed by the elderly on the media communications channels, assessing the trust of the elderly in certain media channels, identifying the measures the elderly took in order to protect themselves during the pandemic, identifying the perception of the elderly about the way the pandemic affected their health and emotional state and identifying the ways in which the social relations of the elderly were affected during the pandemic.
Considering the results of the quantitative research, most respondents described the pandemic period using negative words such as fear, disease, quarantine, disaster and virus. In the context of the channels they most used during the pandemic, the elderly declared that they watched television and some of them also accessed the Internet or listened to the radio. Thus, our results show that there were differences in the preferences of the elderly for different types of media channels, but we highlight that the effect size of the statistical analysis conducted is rather small. In this regard, while looking for the factors that influence the use of media channels among the elderly, the results revealed that gender and residential environment (urban/rural) do not influence the way the elderly use mass media channels. However, the research shows different results according to the last school graduated and to the age of the elderly. Thus, the elderly who had graduated from high school and who were between 65 and 70 years old were the ones who had the highest level of media consumption compared to the other categories. Furthermore, it should be noted that at the beginning of the pandemic, the Romanian Government issued an Emergency Ordinance (no. 63 of 7 May 2020) “for organizing and conducting public information campaigns in the context of the epidemiological situation caused by the spread of COVID-19”. Further analysis of the distribution of the important funds (over EUR 40 million) was made by the Expert Forum [
154]. In this report, it is specified that some political inferences were possible because “the period in which all the funds were promised overlapped with the electoral period”. Other observations refer to the “allocation criteria, the presence on the list of some beneficiaries with significant amounts of highly politicized providers” and the observation that “the beneficiary, who received significant funds from the Government, becomes vulnerable to the perspective of journalistic independence”. In the same report, it is specified that “the first 10 suppliers collected 50% of the money promised by the Government. Most of the money went to national television, but also to several online portals”. All TV channels mentioned received a great proportion of money even if some of these channels “promoted at the same time the messages sent by the government and conspiratorial themes or in conflict with the official data”.
Taking into account the type of information that the elderly mostly saw on the media channels they followed and the frequency of that information, the respondents declared they mostly saw information about the rules they had to follow, about prevention methods, about the number of the victims and about ways to cure the disease. What was interesting was the number of respondents who declared they saw the news about the negative effect of the vaccine on the channels they watched. These results could thus be an indicator of the amount of fake news that was spread on media channels regarding the virus and the vaccine.
Given the trust in media channels, the results showed that the respondents declared that they had the most trust in TV channels compared to any other media channel. Then, trust in radio registered higher numbers compared to trust in newspapers, websites and social networks. Furthermore, trust in newspapers registered higher numbers compared to social networks or websites. Thus, we observed that the respondents had little trust in Internet sources and this could happen either because the elderly do not frequently access Internet sources or because they were advised by their friends or relatives not to trust the information they see on social networks or websites. In this context, we highlight that when we compared the trust in media channels, the effect sizes were: small in the context of comparing: TV channels and radio, TV channels and newspapers; small to medium in the context of comparing TV channels and social networks; and medium in the context of comparing TV channels and news websites. Furthermore, the effect sizes were small in the case in which we compared trust in radio and newspapers, when we compared trust in radio and social networks and when we compared trust in radio and news websites. Even though trust in newspapers was higher than trust in social networks and news websites, the effect size of the statistical analyses was small.
Moreover, in terms of factors influencing trust in media channels, the results showed no difference in the opinions of the elderly depending on their living environment (rural, urban) or their educational level. However, the research showed that the trust in media channels of people aged between 65 and 70 years old was significantly different compared to those aged between 70 and 75 years old, meaning that the first category tended to trust media channels to a higher extent than the second category.
Given the social relations of the elderly in the context of the pandemic, the results showed that the people with whom they talked the most in this period were their children, followed by their spouses. Moreover, when discussing the pandemic and the virus, most respondents declared they chose to discuss it with their family members, but a large amount of them mentioned they would rather talk with their family doctors. In this regard, we observed that the elderly mostly preferred to receive advice from their family members and their doctors.
In terms of the coping mechanism to which the elderly resorted in order to protect themselves from the virus and survive during the pandemic, most respondents decided to get vaccinated or to take additional drugs in order to boost their immune system. However, some of them decided not to leave their house or not to meet their family members. Hence, we observed that most respondents had positive attitudes towards the vaccine and they resorted to appropriate measures in order to protect themselves. A possible explanation for this result would be that, since the TV was the channel that the elderly trusted the most, they may have been influenced by the information spread by TV channels regarding the benefits of the vaccine or the benefits of certain additional drugs.
When communicating with their family members, the elderly mostly resorted to phone calls and they used very little communication through video calls or online platforms. In this regard, it is possible that the elderly had little access to Internet sources or mobile phones that could have allowed them to communicate with their families through certain apps. In this regard, our paper is in line with a previous study [
24], which highlighted the role of technology in maintaining social interaction and communication in crisis periods.
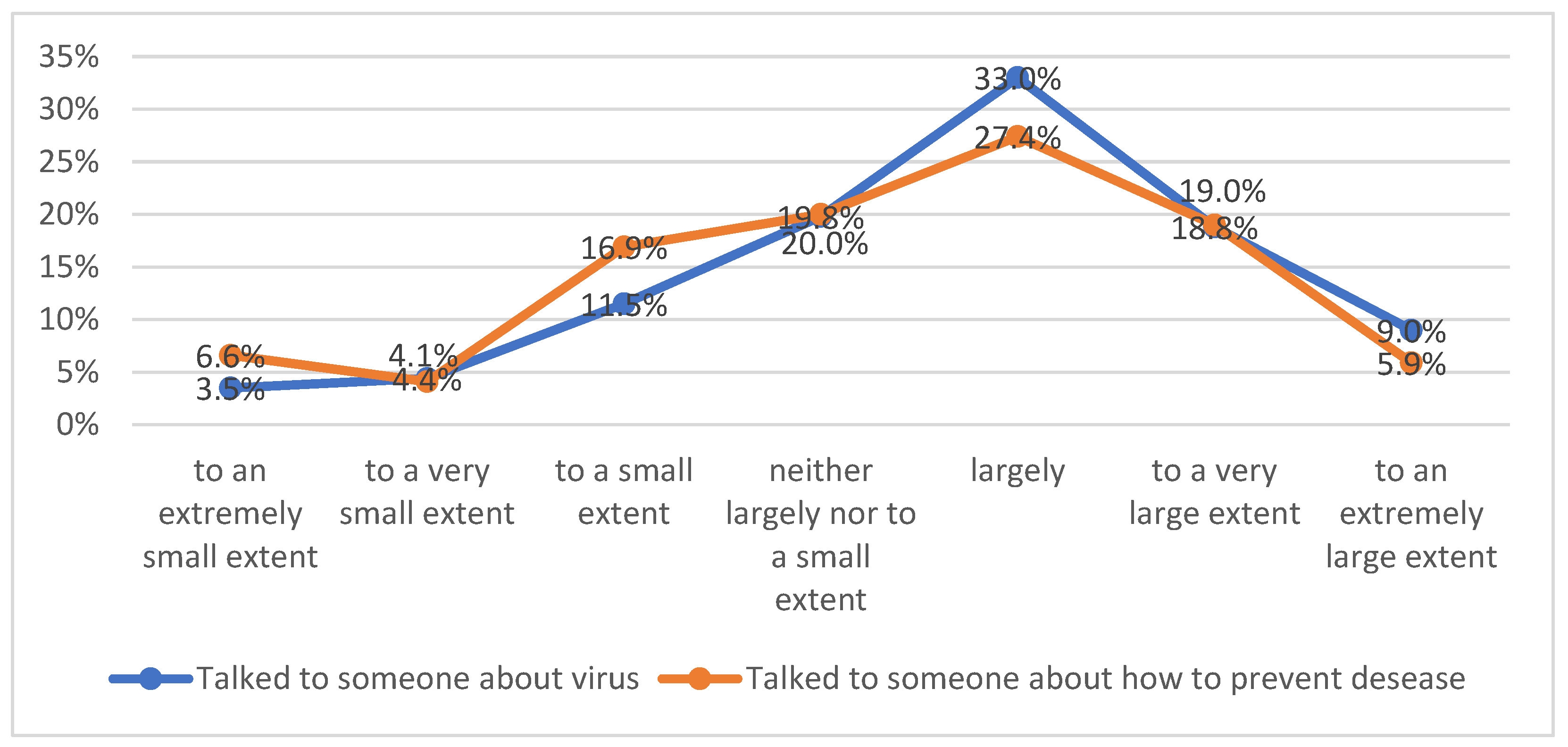
The topics that the elderly mostly discussed with their families referred to ways of preventing infection with the virus, the severity of the disease, the difficulties they encountered and their physical and mental health.
Considering the qualitative research, the results are in line with the results of the quantitative research in the sense that the elderly described the pandemic with negative words, highlighting that during this period, they felt isolated and lonely because they could no longer meet their family, and respondents also stated that the main channel they used in order to obtain information about the virus was the TV.
Moreover, the elderly perceived themselves as the group category that was most affected by the pandemic. In other words, the respondents understood that the virus is more likely to severely damage their health compared to other groups of people. As the results of the quantitative research stated, the results of the qualitative study showed that the elderly mostly talked with their family members about the virus and ways of preventing infection.
When it comes to the problems faced, for most respondents, the restrictions they had to comply with were the main problem. Some of them declared that the biggest problem was loneliness, the inability to be with their families or the lack of access to medical services.
Taking into account the coping mechanisms of the elderly, most of them declared they tried to adapt to the new way of life and that they received help from their friends and families. Others resorted to methods such as mental health education or meditation. In the context of their health issues, the elderly managed to get through the pandemic with the help of their doctors and through hope and trust in divinity. Thus, similar to previous research [
75], our study also shows that the elderly can resort to diverse coping mechanisms in times of crisis.
In the context of the lifestyle during the pandemic, the elderly described the period as full of fear, anxiety and difficulties. The elderly were afraid of the virus, they could not communicate with their family members and they had to change their habits due to the restrictions. Furthermore, they declared that they had issues with access to food, medication and public services. In other words, the elderly had trouble with buying food and medicine and paying their bills due to excessive digitization and the lack of proper devices or digital skills. Taking into account the difficulties the elderly faced during the pandemic, our study is in line with previous studies [
48,
49], which showed how the pandemic and the rules implemented affected social activities and the mental health of people. Moreover, similar to a previous study, our research also emphasizes the fact that the pandemic made people worry more about their life [
50] and that it generated feelings of fear [
51] or anxiety [
52].
However, when asked how the pandemic influenced their family life, most respondents declared that the pandemic did not affect their family life. This might mean that, even if they were no longer able to meet face to face their relatives, the ties the elderly had with them remained the same and they were not negatively influenced by the pandemic.
Considering the medical and social services, the elderly declared that they received medical support from their family doctors but a large amount of them stated that they did not receive any kind of medical or social support.
Therefore, through our study, we managed to obtain a perspective regarding the way information from mass media affected the life of the elderly during the pandemic and regarding the difficulties they faced in this time of crisis. Hence, the mass media did not exercise its surveillance function during the pandemic, the elderly declaring that they saw on TV and other channels both information about prevention methods and negative information about the vaccine. Thus, the information spread by media channels was sometimes contradictory and generated feelings of fear and anxiety among the elderly. Furthermore, based on the results of our research, we argue that the children of the elderly also had a role in influencing the behavior of the elderly and the ways this vulnerable group decided to take measures in order to cope with the pandemic situation.
Hence, we argue that mass media channels have an essential role during periods of crisis and media specialists and professionals from other fields should take into account this matter. In this regard, a previous study highlighted the importance of the media channels by showing that the COVID-19 pandemic has influenced the adoption of telemedicine in the healthcare sector and that the evolution of the pandemic affected the subject discussed on Twitter by the Spanish community and implicitly affected the emotions associated with those subjects [
155]. Furthermore, the importance of studying mass media use in the context of older adults was emphasized by a previous study that focused on the adoption of social networking sites by older adults and that identified several types of elders who use these kinds of sites [
156], as well as by a previous study that showed how older adults accept and use social networking sites after the pandemic period [
157].
From the viewpoint of the theoretical implications, this paper contributes to the literature regarding the coping mechanisms to which the elderly resorted to during the pandemic and regarding the impact that the pandemic had on the lifestyle of the elderly. From the viewpoint of the practical implications, the results obtained through our research show the media consumption of the elderly and the struggles they faced during the pandemic period and such results could be considered a point of reference for the way the lifestyle of the elderly could be improved in general and in times of crises in particular.
Limitations and Future Research Directions
In terms of the limitations of the paper, one limitation is represented by the fact that the study has only been conducted in Romania. In this regard, in a future study, the research instruments should be used in order to also gather information from people who live in other countries. Another limitation is represented by the fact that the data were collected during the pandemic and thus future similar research should be conducted in order to see if and how the responses of the elderly differ. Furthermore, another limitation is represented by the fact that the study was only conducted on one vulnerable group (the elderly) and future research should take into account other vulnerable groups such as people with disabilities in order to make a comparative analysis between these groups. Moreover, future research should take into consideration the development of a comparative analysis of the mass media experiences of the group of older adults and the experiences of other categories of people affected by crises. Another element that should be taken into consideration in a future similar study would be the use of theories, such as the elaboration likelihood model (ELM).