Physicians’ Online Writing Language Style and Patient Satisfaction: The Mediator of Depth of Physician–Patient Interactions
Abstract
:1. Introduction
1.1. Background
1.2. Research Questions
2. Theoretical Background and Literature Review
2.1. Online Pediatric Health Counseling
2.2. Physician Language Characteristics and Patient Satisfaction
2.3. Linguistic Expectancy Theory and Psychological Distance
2.4. Depth of Online Interactions and Physician-Patient Relationship
3. Research Model and Hypotheses
3.1. The Effect of Physician Writing Language Style on Patient Satisfaction
3.2. The Mediating Effect of Depth of Interaction
3.3. Research Model
4. Methods
4.1. Data Collection and Preprocessing
4.2. Variable Design and Measurement
4.2.1. Dependent Variable
4.2.2. Independent Variables
4.2.3. Mediating Variable
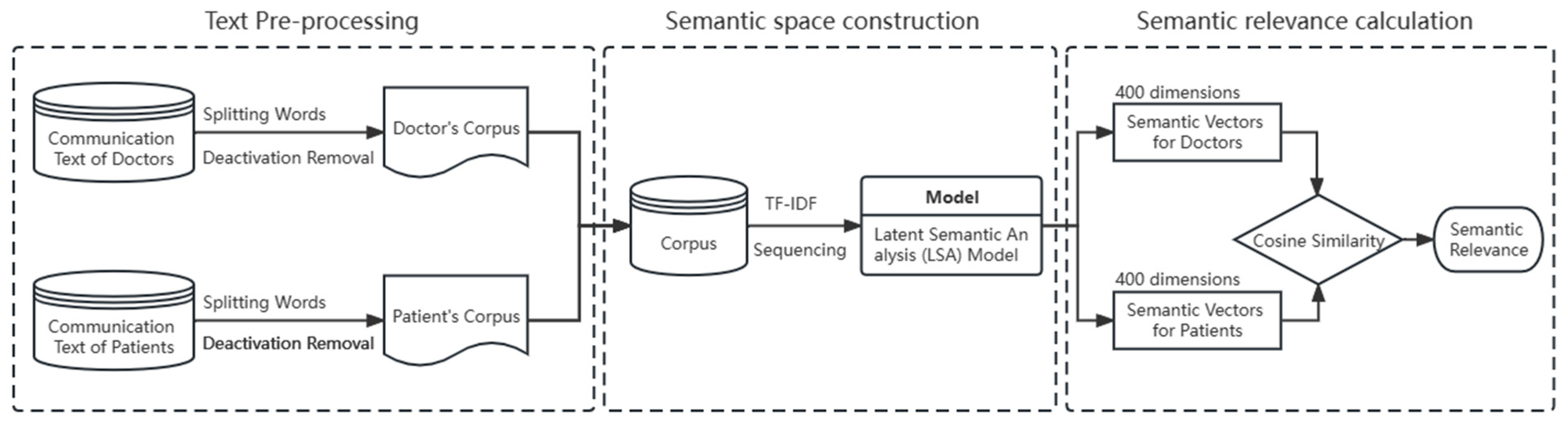
4.2.4. Control Variables
4.3. Descriptive Statistics and Correlation Analysis
5. Results
5.1. Hypothesis Test
5.2. Robustness Checks
5.3. Additional Analysis
6. Discussion
6.1. Key Findings
6.2. Theoretical Contributions
6.3. Practical Implications
6.4. Limitations and Future Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
Appendix C
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Inclusive | 1.357 *** | 1.298 *** | |
| (0.100) | (0.099) | ||
| Emojis | 0.319 *** | ||
| (0.041) | |||
| Control Variables | Yes | Yes | Yes |
| FE Month | Yes | Yes | Yes |
| FE Physician | Yes | Yes | Yes |
| N | 4557 | 4557 | 4557 |
| R2 | 0.33 | 0.36 | 0.37 |
| Variables | Model 1 | Model 2 |
|---|---|---|
| Inclusive | 0.3056 ** | 0.2254 * |
| (0.1282) | (0.1302) | |
| Emojis | 0.6359 *** | 0.6151 *** |
| (0.0875) | (0.0800) | |
| Depth | 0.0516 *** | |
| (0.0153) | ||
| Control Variables | Yes | Yes |
| Sample Size | 4557 | 4557 |
| Pseudo R2 | 0.201 | 0.204 |
Appendix D
| Variables | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Depth | 1.000 | ||||||||||||
| (2) Inclusive | 0.240 | 1.000 | |||||||||||
| (3) Emojis | 0.169 | 0.139 | 1.000 | ||||||||||
| (4) HosLevel | 0.019 | −0.000 | −0.012 | 1.000 | |||||||||
| (5) Ln(Total) | −0.020 | −0.014 | −0.012 | −0.314 | 1.000 | ||||||||
| (6) GoodR | 0.101 | 0.068 | 0.070 | −0.081 | 0.079 | 1.000 | |||||||
| (7) D_Title | −0.012 | 0.024 | 0.023 | −0.198 | 0.286 | −0.092 | 1.000 | ||||||
| (8) Ln(Price) | 0.157 | 0.109 | 0.063 | 0.345 | 0.100 | −0.025 | 0.109 | 1.000 | |||||
| (9) Ln(QLen) | 0.023 | −0.052 | −0.004 | −0.133 | 0.103 | 0.057 | −0.072 | −0.101 | 1.000 | ||||
| (10) D_gender | −0.073 | −0.002 | 0.002 | 0.118 | −0.066 | 0.067 | −0.119 | 0.013 | −0.037 | 1.000 | |||
| (11) RsT | 0.425 | 0.127 | 0.079 | 0.090 | 0.035 | 0.029 | 0.061 | 0.208 | −0.171 | 0.032 | 1.000 | ||
| (12) P_Active | 0.221 | 0.064 | 0.036 | 0.096 | −0.009 | −0.007 | 0.025 | 0.231 | −0.091 | 0.009 | 0.235 | 1.000 | |
| (13) P_Civility | 0.167 | 0.113 | 0.189 | 0.097 | −0.019 | 0.041 | 0.024 | 0.177 | −0.092 | 0.014 | 0.328 | 0.162 | 1.000 |
References
- Silva, B.M.; Rodrigues, J.J.; Díez, I.d.l.T.; López-Coronado, M.; Saleem, K. Mobile-health: A review of current state in 2015. J. Biomed. Informatics 2015, 56, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Yu, K.; Bao, X.; Liu, X.; Yao, J. Patterns of eHealth Website User Engagement Based on Cross-site Clickstream Data: Correlational Study. J. Med. Internet Res. 2021, 23, e29299. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, F.; Lindenmeyer, A.; Powell, J.; Lowe, P.; Thorogood, M. Why are health care interventions delivered over the internet? A systematic review of the published literature. J. Med. Internet Res. 2006, 8, e10. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Guo, X.; Wu, T.; Ju, X. Exploring the online physician-patient interaction on patient satisfaction based on text mining and empirical analysis. Inf. Process. Manag. 2020, 57, 102253. [Google Scholar] [CrossRef]
- Yang, H.; Guo, X.; Wu, T. Exploring the influence of the online physician service delivery process on patient satisfaction. Decis. Support Syst. 2015, 78, 113–121. [Google Scholar] [CrossRef]
- Wu, H.; Lu, N. Service provision, pricing, and patient satisfaction in online health communities. Int. J. Med. Inform. 2018, 110, 77–89. [Google Scholar] [CrossRef]
- Liu, X.; Zhou, S.; Chi, X. How Do Team-Level and Individual-Level Linguistic Styles Affect Patients’ Emotional Well-Being—Evidence from Online Physician Teams. Int. J. Environ. Res. Public Health 2023, 20, 1915. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, X.; Lee, P.K. Improving the effectiveness of online healthcare platforms: An empirical study with multi-period patient-physician counseling data. Int. J. Prod. Econ. 2018, 207, 70–80. [Google Scholar] [CrossRef]
- Tan, H.; Yan, M. Physician-user interaction and users’ perceived service quality: Evidence from Chinese mobile healthcare counseling. Inf. Technol. People 2020, 33, 1403–1426. [Google Scholar] [CrossRef]
- Burgoon, J.K. Cross-cultural and intercultural applications of expectancy violations theory. In Intercultural Communication Theory; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1995; pp. 194–214. [Google Scholar]
- Lee, C.H.; Yu, H. The impact of language on retweeting during acute natural disasters: Uncertainty reduction and language expectancy perspectives. Ind. Manag. Data Syst. 2020, 120, 1501–1519. [Google Scholar] [CrossRef]
- Zhu, X. Proximal language predicts crowdfunding success: Behavioral and experimental evidence. Comput. Hum. Behav. 2022, 131, 107213. [Google Scholar] [CrossRef]
- Parhankangas, A.; Renko, M. Linguistic style and crowdfunding success among social and commercial entrepreneurs. J. Bus. Ventur. 2017, 32, 215–236. [Google Scholar] [CrossRef]
- Jin, X.; Li, J.; Gao, J. Joint effect of linguistic style and ethnicity on entrepreneurial fundraising: Evidence from equity crowdfunding. J. Int. Financ. Mark. Inst. Money 2022, 81, 101660. [Google Scholar] [CrossRef]
- Lee, C.H.; Bian, Y.; Karaouzene, R.; Suleiman, N. Examining the role of narratives in civic crowdfunding: Linguistic style and message substance. Ind. Manag. Data Syst. 2019, 119, 1492–1514. [Google Scholar] [CrossRef]
- Wang, X.; Mu, C.; Li, H.; Noble, A.; Wang, Q. Product-Centered Language Style in Chinese Women Online Reviews. Front. Psychol. 2022, 13, 839064. Available online: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.839064 (accessed on 20 January 2023). [CrossRef]
- Dolan, V.L.B. The isolation of online adjunct faculty and its impact on their performance. Int. Rev. Res. Open Distrib. Learn. 2011, 12, 62–77. [Google Scholar] [CrossRef]
- Yoon, S.A.; Miller, K.; Richman, T.; Wendel, D.; Schoenfeld, I.; Anderson, E.; Shim, J. Encouraging collaboration and building Community in Online Asynchronous Professional Development: Designing for social capital. Int. J. Comput. Collab. Learn. 2020, 15, 351–371. [Google Scholar] [CrossRef]
- Wu, R.; Chen, J.; Wang, C.L.; Zhou, L. The influence of emoji meaning multipleness on perceived online review helpfulness: The mediating role of processing fluency. J. Bus. Res. 2022, 141, 299–307. [Google Scholar] [CrossRef]
- Newman, M.L.; Pennebaker, J.; Berry, D.S.; Richards, J.M. Lying Words: Predicting Deception from Linguistic Styles. Pers. Soc. Psychol. Bull. 2003, 29, 665–675. [Google Scholar] [CrossRef]
- Heeschen, C.; Schegloff, E.A. Agrammatism, adaptation theory, conversation analysis: On the role of so-called telegraphic style in talk-in-interaction. Aphasiology 1999, 13, 365–405. [Google Scholar] [CrossRef]
- Slatcher, R.B.; Vazire, S.; Pennebaker, J. Am “I” more important than “we”? Couples’ word use in instant messages. Pers. Relatsh. 2008, 15, 407–424. [Google Scholar] [CrossRef]
- Saponara, M.; Pantaleo, M.A.; Nannini, M.; Biasco, G. Chronic therapy in gastrointestinal stromal tumours (GISTs): The big gap between theory and practice. Target. Oncol. 2012, 7, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.-J. Does the relationship between brand attitude, brand attachment and purchase intention vary based on the type of prosocial expression-based brand emoji? J. Prod. Brand Manag. 2022, 31, 1180–1195. [Google Scholar] [CrossRef]
- Persky, S.; Ferrer, R.A.; Klein, W.M.P. Nonverbal and paraverbal behavior in (simulated) medical visits related to genomics and weight: A role for emotion and race. J. Behav. Med. 2016, 39, 804–814. [Google Scholar] [CrossRef] [PubMed]
- Troiano, G.; Nante, N. Emoji: What does the scientific literature say about them?—A new way to communicate in the 21th century. J. Hum. Behav. Soc. Environ. 2018, 28, 528–533. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, M.; Gao, B.; Jiang, G. Physician voice characteristics and patient satisfaction in online health consultation. Inf. Manag. 2020, 57, 103233. [Google Scholar] [CrossRef]
- Yan, M.; Tan, H.; Jia, L.; Akram, U. The antecedents of poor physician-patient relationship in mobile counseling: A perspective from computer-mediated communication. Int. J. Environ. Res. Public Health 2020, 17, 2579. [Google Scholar] [CrossRef]
- Igler, E.; Lang, A.; Balistreri, K.; Sejkora, E.; Drendel, A.; Davies, W.H. Parents Reliably Identify Pain Dismissal by Pediatric Providers. Clin. J. Pain 2019, 36, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Lorié, E.S.; Wreesmann, W.-J.W.; van Veenendaal, N.R.; van Kempen, A.A.; Labrie, N.H. Parents’ needs and perceived gaps in communication with healthcare professionals in the neonatal (intensive) care unit: A qualitative interview study. Patient Educ. Couns. 2021, 104, 1518–1525. [Google Scholar] [CrossRef]
- Venegas, V.; Manterola, C.; De Pablo, J.; Garcia, M.; de León, S.P.; Cavada, G. How the characteristics of pediatric neurologists in Latin America influence the communication of sudden unexpected death in epilepsy to patients and caregivers. Epilepsia Open 2022, 7, 442–451. [Google Scholar] [CrossRef]
- Liu, S.; Si, G.; Gao, B. Which voice are you satisfied with? Understanding the physician–patient voice interactions on online health platforms. Decis. Support Syst. 2022, 157, 113754. [Google Scholar] [CrossRef]
- Suman, C.; Saha, S.; Bhattacharyya, P.; Chaudhari, R.S. Emoji Helps! A Multi-modal Siamese Architecture for Tweet User Verification. Cogn. Comput. 2020, 13, 261–276. [Google Scholar] [CrossRef]
- He, Y.; Guo, X.; Wu, T.; Vogel, D. The effect of interactive factors on online health counseling review deviation: An empirical investigation. Int. J. Med. Inform. 2022, 163, 104781. [Google Scholar] [CrossRef] [PubMed]
- Huff, E.S.; Leahy, J.E.; Kittredge, D.B.; Noblet, C.L.; Weiskittel, A.R. Psychological distance of timber harvesting for private woodland owners. For. Policy Econ. 2017, 81, 48–56. [Google Scholar] [CrossRef]
- Sungur, H.; Van Koningsbruggen, G.M.; Hartmann, T.; Information, R. Psychological Distance Cues in Online Messages. J. Media Psychol. 2019, 31, 65–80. [Google Scholar] [CrossRef]
- Kwon, K.H.; Pellizzaro, K.; Shao, C.; Chadha, M. “I Heard That COVID-19 Was...”: Rumors, Pandemic, and Psychological Distance. Am. Behav. Sci. 2022, 7, 00027642211066026. [Google Scholar] [CrossRef]
- MacEntee, M.I.; Mathu-Muju, K.R. Confronting dental uncertainty in old age. Gerodontology 2014, 31, 37–43. [Google Scholar] [CrossRef]
- Matusitz, J.; Spear, J. Effective physician–patient communication: An updated examination. Soc. Work. Public Health 2014, 29, 252–266. [Google Scholar] [CrossRef]
- Dearman, S.P.; Joiner, A.; Gordon, M.; Vince, G. Experiences of patients with mental illness’ interactions with medical students: A systematic review. Can. J. Psychiatry 2017, 63, 4–11. [Google Scholar] [CrossRef]
- Yilmaz, R.M.; Baydas, O.; Karakus, T.; Goktas, Y. An examination of interactions in a three-dimensional virtual world. Comput. Educ. 2015, 88, 256–267. [Google Scholar] [CrossRef]
- Dong, X.; Wang, T. Social tie formation in Chinese online social commerce: The role of IT affordances. Int. J. Inf. Manag. 2018, 42, 49–64. [Google Scholar] [CrossRef]
- Levin, D.Z.; Cross, R. The Strength of Weak Ties You Can Trust: The Mediating Role of Trust in Effective Knowledge Transfer. Manag. Sci. 2004, 50, 1477–1490. [Google Scholar] [CrossRef]
- Guo, S.; Guo, X.; Zhang, X.; Vogel, D. Doctor–patient relationship strength’s impact in an online healthcare community. Inf. Technol. Dev. 2017, 24, 279–300. [Google Scholar] [CrossRef]
- Kang, K.; Lu, J.; Guo, L.; Li, W. The dynamic effect of interactivity on customer engagement behavior through tie strength: Evidence from live streaming commerce platforms. Int. J. Inf. Manag. 2020, 56, 102251. [Google Scholar] [CrossRef]
- Mascaro, J.S.; Palmer, P.K.; Willson, M.; Ash, M.J.; Florian, M.P.; Srivastava, M.; Sharma, A.; Jarrell, B.; Walker, E.R.; Kaplan, D.M.; et al. The Language of Compassion: Hospital Chaplains’ Compassion Capacity Reduces Patient Depression via Other-Oriented, Inclusive Language. Mindfulness 2022, 13, 1–4. [Google Scholar] [CrossRef]
- Huynh, H.P.; Dicke-Bohmann, A.; Nelson, C. What do humble physicians do? A conceptualization of clinician humility from the patient’s perspective. Patient Educ. Couns. 2021, 104, 3066–3071. [Google Scholar] [CrossRef] [PubMed]
- Ge, J.; Gretzel, U. Emoji rhetoric: A social media influencer perspective. J. Mark. Manag. 2018, 34, 1272–1295. [Google Scholar] [CrossRef]
- Skiba, D.J. Face with tears of joy is word of the year: Are emoji a sign of things to come in health care? Nurs. Educ. Perspect. 2016, 37, 56–57. [Google Scholar] [CrossRef]
- Rains, S.A.; Brunner, S.R.; Akers, C.; Pavlich, C.A.; Tsetsi, E. The Implications of Computer-Mediated Communication (CMC) for Social Support Message Processing and Outcomes: When and Why Are the Effects of Support Messages Strengthened During CMC? Hum. Commun. Res. 2016, 42, 553–576. [Google Scholar] [CrossRef]
- Park, A.; Hartzler, A.; Huh, J.; Hsieh, G.; McDonald, D.; Pratt, W. “How Did We Get Here?”: Topic Drift in Online Health Discussions. J. Med. Internet Res. 2016, 18, e284. Available online: https://www.jmir.org/2016/11/e284 (accessed on 10 January 2023). [CrossRef]
- Nook, E.C.; Schleider, J.L.; Somerville, L.H. A linguistic signature of psychological distancing in emotion regulation. J. Exp. Psychol. Gen. 2017, 146, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Scarpi, D. The Importance of Consumer Engagement in Brand Heritage Advertising How Feeling Close to a Brand Can Increase Willingness to Pay More. J. Advert. Res. 2021, 61, 334–345. [Google Scholar] [CrossRef]
- Nishimura, Y. Impoliteness in Japanese BBS interactions: Observations from message exchanges in two online communities. J. Polite. Res. 2010, 6, 35–55. [Google Scholar] [CrossRef]
- Koh, Y.; Lee, M.; Kim, J.; Yang, Y. Successful restaurant crowdfunding: The role of linguistic style. Int. J. Contemp. Hosp. Manag. 2020, 32, 3051–3066. [Google Scholar] [CrossRef]
- Lin, W.-F.; Lin, Y.-C.; Huang, C.-L.; Chen, L.H. We Can Make It Better: “We” Moderates the Relationship Between a Compromising Style in Interpersonal Conflict and Well-Being. J. Happiness Stud. 2014, 17, 41–57. [Google Scholar] [CrossRef]
- Lin, X.; Sarker, S.; Featherman, M. Users’ Psychological Perceptions of Information Sharing in the Context of Social Media: A Comprehensive Model. Int. J. Electron. Commer. 2019, 23, 453–491. [Google Scholar] [CrossRef]
- Li, Z.; Song, M.; Duan, S.; Wang, Z. Are users attracted by playlist titles and covers? Understanding playlist selection behavior on a music streaming platform. J. Innov. Knowl. 2022, 7, 100212. [Google Scholar] [CrossRef]
- Huang, L.; Joshi, P.; Wakslak, C.; Wu, A. Sizing Up Entrepreneurial Potential: Gender Differences in Communication and Investor Perceptions of Long-Term Growth and Scalability. Acad. Manag. J. 2021, 64, 716–740. [Google Scholar] [CrossRef]
- Vrana, S.R.; Vrana, D.T.; Penner, L.A.; Eggly, S.; Slatcher, R.B.; Hagiwara, N. Latent Semantic Analysis: A new measure of patient-physician communication. Soc. Sci. Med. 2017, 198, 22–26. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, H.; Xia, C.; Lu, N. Impact of the Price of Gifts from Patients on Physicians’ Service Quality in Online Consultations: Empirical Study Based on Social Exchange Theory. J. Med. Internet Res. 2020, 22, e15685. Available online: https://www.jmir.org/2020/5/e15685 (accessed on 11 January 2023). [CrossRef]
- Stock, J.H.; Yogo, M. Testing for Weak Instruments in Linear IV Regression; Cambridge University Press: New York, NY, USA, 2002. [Google Scholar]
- Baggia, A.; Žnidaršič, A.; Tratnik, A. Emoticons in student-professor email communication. [Emoticonos en la comunicación por correo electrónico entre estudiantes y profesores]. Comunicar 2022, 73, 119–133. [Google Scholar] [CrossRef]
- Lind, J.T.; Mehlum, H. With or without u? the appropriate test for a U-shaped relationship. Oxf. Bull. Econ. Stat. 2010, 72, 109–118. [Google Scholar] [CrossRef]
- Chinese Industry News. 2021 China Internet Medical Content Platform Physician and User Insights: Q&A Content Is the Most Frequent form of User Access. Available online: http://www.chyxx.com/industry/202109/973048.html (accessed on 20 January 2022). (In Chinese).
- Ford, S.; Fallowfield, L.; Lewis, S. Physician-patient interactions in oncology. Soc. Sci. Med. 1996, 42, 1511–1519. [Google Scholar] [CrossRef] [PubMed]
- Deerwester, S.; Dumais, S.; Furnas, G.; Landauer, T.; Harshman, R. Indexing by Latent Semantic Analysis. J. Am. Soc. Inf. Sci. 1990, 41, 391–407. [Google Scholar] [CrossRef]
- Landauer, T.K.; Dumais, S.T. A solution to Plato’s problem: The latent semantic analysis theory of acquisition, induction, and representation of knowledge. Psychol. Rev. 1997, 104, 211–240. [Google Scholar] [CrossRef]
- Louwerse, M.M. Symbol Interdependency in Symbolic and Embodied Cognition. Top. Cogn. Sci. 2011, 3, 273–302. [Google Scholar] [CrossRef]
- Tofighi, D.; MacKinnon, D.P. RMediation: An R package for mediation analysis confidence intervals. Behav. Res. 2011, 43, 692–700. [Google Scholar] [CrossRef]
- MacKinnon, D.P.; Cox, M.C. Commentary on “Mediation analysis and categorical variables: The final frontier” by Dawn Iacobucci. J. Consum. Psychol. 2012, 22, 600–602. [Google Scholar] [CrossRef]




| Information Form | Literature | Language Form | Key Variables | Key Findings |
|---|---|---|---|---|
| Information expression | This study | Language and paralanguage | Depth of interaction (content relevance was considered), emoticons, and inclusive language. | Findings: Emojis and inclusive language have a positive impact on patient satisfaction. The depth of doctor–patient interaction mediates this impact. |
| 2022; [32] | paralanguage | Pitch and Intensity. | Findings: The pitch of the physician’s voice has a positive effect on patient-perceived satisfaction, and the intensity has a negative effect on patient-perceived satisfaction, respectively, and the physician’s popularity moderates this effect. In addition, patient-perceived satisfaction affects subsequent economic returns for physicians. | |
| 2020; [27] | paralanguage | Speech rate and average spectral centroid. | Findings: physician speech rate had a positive effect on patient satisfaction, and average spectral centroid had a negative effect on patient satisfaction. Physicians’ professional capital moderated this effect. | |
| 2023; [7] | Language | Vocabulary richness, health-related terms, and emotional expressions. | Findings: Physician-level and individual-level language styles (vocabulary richness, health-related terminology, and emotional expressions) affect patient mood. | |
| Information content | 2019; [8] | Language and paralanguage | Depth of interaction (only the frequency of interaction was considered), response time, and service content. | Findings: Depth of interaction, physician service content, and response time significantly impacted patients’ decisions to continue consulting. Their impact on patient satisfaction varied over time. |
| 2020; [9] | Language | Information support, emotional support, physician responsiveness, and use of voice services or not. | Findings: The user’s perceived quality of service is influenced by the physician’s information support, emotional support, responsiveness, and use of voice service, in addition to the interaction effects between them. | |
| 2015; [5] | paralanguage | Response speed, interaction frequency, and patient’s risk of disease. | Findings: Interaction frequency and response speed are important aspects related to patient satisfaction. In addition, patients’ risk of illness moderated their relationship. | |
| 2022; [34] | Language and paralanguage | Frequency of interaction, message delivery method, and medical information. | Findings: Frequency of interaction, medical information, and message delivery method are three important aspects of online physician reviews bias. In addition, physician specialization varies to affect the effectiveness of voice messages. | |
| 2020; [4] | Language | Patient’s activity; Physician’s informational support; Physician’s emotional support; Severity of patient’s disease. | Findings: Informational and emotional support significantly affected patient satisfaction, and the effect of emotional support was greater. The severity of the patient’s illness moderated the association between them. |
| Literature | Dimension | Research Field | Definition |
|---|---|---|---|
| 2015; [41] | Frequency | Online learning | Frequency of participants interacting with the 3D virtual world. |
| 2019; [8] | Frequency | Online healthcare | Number of interactions between physician and patient. |
| 2020; [18] | Content | Online learning | Interactive content closely related to goals. |
| Variables | Measurement and Description | |
|---|---|---|
| Dependent variable | PatSatis | If the patient leaves a satisfactory evaluation, the code is 1 and the other is 0. |
| Independent and Mediating variables | Depth | Use content-relevant interactions to measure interaction depth. |
| Inclusive | Inclusive language is measured by the number of “first-person plural” that a physician uses during counseling. | |
| Emojis | Frequency of emoji usage is measured by the number of emoticons used by the physician during counseling. | |
| Control variables | RsT | The average response time of a physician is the average time difference between the physician’s response to the patient across all physician–patient interactions. |
| QLen | The complexity of the patient’s question is measured using the total number of words asked by the patient during the counseling. | |
| D_Gender | The physician’s gender is a binary variable (1 for male physicians, 0 for female physicians). | |
| Price | Single counseling price. | |
| Total | Total number of patients received by physician online. | |
| GoodR | Physician’s online recommended value. | |
| D_Title | The physician’s professional title. Chief Physician, Associate Chief Physician, Attending Physician, and Physician are indicated as 4, 3, 2, and 1, respectively. | |
| HosLevel | The rank of the physician’s hospital (1 for tertiary hospitals, 0 otherwise). | |
| P_Active | The total number of examination pictures provided by the patient in the interaction. | |
| P_Civility | Total number of polite words used by patients. |
| Variable | N | Mean | Std | Min | Max |
|---|---|---|---|---|---|
| PatSatis | 5064 | 0.807 | 0.390 | 0 | 1 |
| Depth | 5064 | 4.070 | 3.500 | 0 | 25.24 |
| Inclusive | 5064 | 0.110 | 0.460 | 0 | 7 |
| Emojis | 5064 | 0.520 | 1.350 | 0 | 19 |
| HosLevel | 5064 | 0.500 | 0.500 | 0 | 1 |
| Ln(Total) | 5064 | 8.460 | 1.330 | 4.530 | 11.52 |
| GoodR | 5064 | 5064 | 4.940 | 0.090 | 4.500 |
| D_Title | 5064 | 1.970 | 0.850 | 1 | 4 |
| Ln(Price) | 5064 | 1.540 | 1.210 | 0 | 6.080 |
| Ln(QLen) | 5064 | 4.630 | 0.930 | 0 | 7.670 |
| D_gender | 5064 | 0.480 | 0.500 | 0 | 1 |
| RsT | 5064 | 0.020 | 0.020 | 0 | 0.240 |
| P_Active | 5064 | 2.150 | 2.760 | 0 | 50 |
| P_Civility | 5064 | 1.690 | 1.730 | 0 | 24 |
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| HosLevel | −0.0074 | −0.6410 | −0.5216 |
| (1.9819) | (1.9420) | (1.9302) | |
| Ln(Total) | 0.1368 | −0.1874 | −0.1947 |
| (0.6521) | (0.6393) | (0.6353) | |
| GoodR | 9.1268 | 7.0232 | 6.3844 |
| (10.2176) | (10.0107) | (9.9496) | |
| D_Title | −0.9977 | −1.1112 | −1.0318 |
| (0.8208) | (0.8041) | (0.7992) | |
| Ln(Price) | 0.5347 *** | 0.4706 *** | 0.4310 *** |
| (0.0496) | (0.0488) | (0.0488) | |
| D_Gender | −2.7371 | −1.3965 | −1.2793 |
| (2.0866) | (2.0463) | (2.0338) | |
| RsT | 15.2348 *** | 16.0445 *** | 16.3005 *** |
| (2.5029) | (2.4526) | (2.4378) | |
| Ln(QLen) | 1.4865 *** | 1.4261 *** | 1.4165 *** |
| (0.0500) | (0.0491) | (0.0489) | |
| P_Active | 0.1643 *** | 0.1642 *** | 0.1656 *** |
| (0.0160) | (0.0157) | (0.0156) | |
| P_Civility | 0.0501 * | 0.0299 | −0.5216 |
| (0.0263) | (0.0258) | (1.9302) | |
| Inclusive | 1.3604 *** | 1.3004 *** | |
| (0.0965) | (0.0962) | ||
| Emojis | 0.3064 *** | ||
| (0.0398) | |||
| FE Month | Yes | Yes | Yes |
| FE Physician | Yes | Yes | Yes |
| _cons | −48.1987 | −34.9483 | −31.8304 |
| (49.5114) | (48.5124) | (48.2166) | |
| N | 5064 | 5064 | 5064 |
| R2 | 0.33 | 0.36 | 0.37 |
| Variables | Model 1 | Model 2 |
|---|---|---|
| Depth | 0.0575 *** | |
| (0.0145) | ||
| Inclusive | 0.3198 ** | 0.2362 * |
| (0.1273) | (0.1291) | |
| Emojis | 0.6059 *** | 0.5845 *** |
| (0.0824) | (0.0828) | |
| HosLevel | −0.1785 * | −0.1516 |
| (0.0918) | (0.0922) | |
| Ln(Total) | −0.1870 *** | −0.1787 *** |
| (0.0331) | (0.0331) | |
| GoodR | 4.8030 *** | 4.6613 *** |
| (0.4063) | (0.4088) | |
| D_Title | −0.0172 | −0.0128 |
| (0.0501) | (0.0501) | |
| Ln(Price) | −0.1584 *** | −0.1715 *** |
| (0.0377) | (0.0379) | |
| D_Gender | 0.0361 | 0.0631 |
| (0.0810) | (0.0814) | |
| RsT | 8.4656 *** | 6.9138 *** |
| (2.4331) | (2.4577) | |
| Ln(QLen) | 0.0824 * | 0.0021 |
| (0.0450) | (0.0495) | |
| P_Active | 0.0353 ** | 0.0288 * |
| (0.0169) | (0.0171) | |
| P_Civility | 0.8248 *** | 0.8446 *** |
| (0.0444) | (0.0451) | |
| _cons | −21.2444 *** | −22.0378 *** |
| (2.0223) | (2.0074) | |
| Sample Size | 5064 | 5064 |
| Pseudo R2 | 0.200 | 0.204 |
| Research Hypothesis | Result |
|---|---|
| H1: The effect of physicians’ use of inclusive language on patient satisfaction is positive. | Support |
| H2: The effect of physician use of emojis on patient satisfaction is positive. | Support |
| H3: The effect of depth of online interaction on patient satisfaction is positive. | Support |
| H4: The effect of physicians’ use of inclusive language on the depth of online interactions is positive. | Support |
| H5: The effect of physicians’ use of emojis on the depth of online interaction is positive. | Support |
| First | Second | First | Second | |
|---|---|---|---|---|
| Inclusive | Depth | Emojis | Depth | |
| (1) | (2) | (3) | (4) | |
| Inclusive_y | 1.1623 *** | |||
| (0.0245) | ||||
| Inclusive | 1.2651 *** | |||
| (0.1637) | ||||
| Emojis_y | 1.1303 *** | |||
| (0.0216) | ||||
| Emojis | 0.3797 *** | |||
| (0.0642) | ||||
| Contral Variables | Yes | Yes | Yes | Yes |
| FE Month | Yes | Yes | Yes | Yes |
| FE Physician | Yes | Yes | Yes | Yes |
| N | 5064 | 5064 | 5064 | 5064 |
| r2 | 0.4672 | 0.4047 | 0.6611 | 0.3894 |
| Cragg-Donald Wald F statistic | 2248 | 2750 |
| Variables | PatSatis |
|---|---|
| Emojis | 0.7307 *** |
| (0.0962) | |
| Emojis2 | −0.0379 *** |
| (0.0098) | |
| Inclusive | 0.3207 ** |
| (0.1271) | |
| Control Variables | Yes |
| Sample Size | 5064 |
| Pseudo R2 | 0.2012 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Jiang, H.; Wang, S. Physicians’ Online Writing Language Style and Patient Satisfaction: The Mediator of Depth of Physician–Patient Interactions. Healthcare 2023, 11, 1569. https://doi.org/10.3390/healthcare11111569
Liu J, Jiang H, Wang S. Physicians’ Online Writing Language Style and Patient Satisfaction: The Mediator of Depth of Physician–Patient Interactions. Healthcare. 2023; 11(11):1569. https://doi.org/10.3390/healthcare11111569
Chicago/Turabian StyleLiu, Jingfang, Huihong Jiang, and Shiqi Wang. 2023. "Physicians’ Online Writing Language Style and Patient Satisfaction: The Mediator of Depth of Physician–Patient Interactions" Healthcare 11, no. 11: 1569. https://doi.org/10.3390/healthcare11111569
APA StyleLiu, J., Jiang, H., & Wang, S. (2023). Physicians’ Online Writing Language Style and Patient Satisfaction: The Mediator of Depth of Physician–Patient Interactions. Healthcare, 11(11), 1569. https://doi.org/10.3390/healthcare11111569





