Trends and Outcomes in Lung Transplantation in Patients with and without Idiopathic Pulmonary Fibrosis in Spain during the Period 2016–2020
Abstract
:1. Introduction
2. Materials and Methods
2.1. Statistical Analysis
2.2. Ethics Statement
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arcasoy, S.M.; Kotloff, R.M. Lung transplantation. N. Engl. J. Med. 1999, 340, 1081–1091. [Google Scholar] [CrossRef] [PubMed]
- Kapnadak, S.G.; Raghu, G. Lung transplantation for interstitial lung disease. Eur. Respir. Rev. 2021, 30, 210017. [Google Scholar] [CrossRef] [PubMed]
- Chambers, D.C.; Cherikh, W.S.; Harhay, M.O.; Hayes, D., Jr.; Hsich, E.; Khush, K.K.; Meiser, B.; Potena, L.; Rossano, J.W.; Toll, A.E.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-sixth adult lung and heart-lung transplantation Report-2019; Focus theme: Donor and recipient size match. J. Heart Lung Transplant. 2019, 38, 1042–1055. [Google Scholar] [CrossRef] [PubMed]
- Chambers, D.C.; Zuckermann, A.; Cherikh, W.S.; Harhay, M.O.; Hayes, D., Jr.; Hsich, E.; Khush, K.K.; Potena, L.; Sadavarte, A.; Singh, T.P.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: 37th adult lung transplantation report-2020; focus on deceased donor characteristics. J. Heart Lung Transplant. 2020, 39, 1016–1027. [Google Scholar] [CrossRef] [PubMed]
- Yusen, R.D.; Edwards, L.B.; Kucheryavaya, A.Y.; Benden, C.; Dipchand, A.I.; Dobbels, F.; Goldfarb, S.B.; Levvey, B.J.; Lund, L.H.; Meiser, B.; et al. The registry of the International Society for Heart and Lung Transplantation: Thirty-first adult lung and heart-lung transplant report-2014; focus theme: Retransplantation. J. Heart Lung Transplant. 2014, 33, 1009–1024. [Google Scholar] [CrossRef]
- Chambers, D.C.; Cherikh, W.S.; Goldfarb, S.B.; Hayes, D., Jr.; Kucheryavaya, A.Y.; Toll, A.E.; Khush, K.K.; Levvey, B.J.; Meiser, B.; Rossano, J.W.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-fifth adult lung and heart-lung transplant report-2018; Focus theme: Multiorgan Transplantation. J. Heart Lung Transplant. 2018, 37, 1169–1183. [Google Scholar] [CrossRef]
- Valapour, M.; Lehr, C.J.; Skeans, M.A.; Smith, J.M.; Uccellini, K.; Goff, R.; Foutz, J.; Israni, A.K.; Snyder, J.J.; Kasiske, B.L. OPTN/SRTR 2018 Annual Data Report: Lung. Am. J. Transplant. 2020, 20 (Suppl. S1), 427–508. [Google Scholar] [CrossRef]
- Glass, D.S.; Grossfeld, D.; Renna, H.A.; Agarwala, P.; Spiegler, P.; DeLeon, J.; Reiss, A.B. Idiopathic pulmonary fibrosis: Current and future treatment. Clin. Respir. J. 2022, 16, 84–96. [Google Scholar] [CrossRef]
- Raghu, G.; Remy-Jardin, M.; Richeldi, L.; Thomson, C.C.; Inoue, Y.; Johkoh, T.; Kreuter, M.; Lynch, D.A.; Maher, T.M.; Martinez, F.J.; et al. Idiopathic Pulmonary Fibrosis (an Update) and Progressive Pulmonary Fibrosis in Adults: An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2022, 205, e18–e47. [Google Scholar] [CrossRef]
- Somogyi, V.; Chaudhuri, N.; Torrisi, S.E.; Kahn, N.; Müller, V.; Kreuter, M. The therapy of idiopathic pulmonary fibrosis: What is next? Eur. Respir. Rev. 2019, 28, 190021. [Google Scholar] [CrossRef]
- Hackman, K.L.; Bailey, M.J.; Snell, G.I.; Bach, L.A. Diabetes is a major risk factor for mortality after lung transplantation. Am. J. Transplant. 2014, 14, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Patti, M.G.; Vela, M.F.; Odell, D.D.; Richter, J.E.; Fisichella, P.M.; Vaezi, M.F. The intersection of GERD, aspiration, and lung transplantation. J. Laparoendosc. Adv. Surg. Tech. A 2016, 26, 501–505. [Google Scholar] [CrossRef] [PubMed]
- George, P.M.; Patterson, C.M.; Reed, A.K.; Thillai, M. Lung transplantation for idiopathic pulmonary fibrosis. Lancet Respir. Med. 2019, 7, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Balestro, E.; Cocconcelli, E.; Tinè, M.; Biondini, D.; Faccioli, E.; Saetta, M.; Rea, F. Idiopathic Pulmonary Fibrosis and Lung Transplantation: When it is Feasible. Medicina 2019, 55, 702. [Google Scholar] [CrossRef] [PubMed]
- Le Pavec, J.; Dauriat, G.; Gazengel, P.; Dolidon, S.; Hanna, A.; Feuillet, S.; Pradere, P.; Crutu, A.; Florea, V.; Boulate, D.; et al. Lung transplantation for idiopathic pulmonary fibrosis. Presse Med. 2020, 49, 104026. [Google Scholar] [CrossRef]
- Force, S.D.; Kilgo, P.; Neujahr, D.C.; Pelaez, A.; Pickens, A.; Fernandez, F.G.; Miller, D.L.; Lawrence, C. Bilateral lung transplantation offers better long-term survival, compared with single-lung transplantation, for younger patients with idiopathic pulmonary fibrosis. Ann. Thorac. Surg. 2011, 91, 244–249. [Google Scholar] [CrossRef]
- Villavicencio, M.A.; Axtell, A.L.; Osho, A.; Astor, T.; Roy, N.; Melnitchouk, S.; D’Alessandro, D.; Tolis, G.; Raz, Y.; Neuringer, I.; et al. Single- versus Double-Lung Transplantation in Pulmonary Fibrosis: Impact of Age and Pulmonary Hypertension. Ann. Thorac. Surg. 2018, 106, 856–863. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Real Decreto 69/2015, de 6 de Febrero, por el que se Regula el Registro de Actividad de Atención Sanitaria Especializada. (Spanish National Hospital Discharge Database). BOE 2015, 35, 10789–10809. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/docs/BOE_RD_69_2015_RAE_CMBD.pdf (accessed on 21 March 2023).
- Sundararajan, V.; Henderson, T.; Perry, C.; Muggivan, A.; Quan, H.; Ghali, W.A. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J. Clin. Epidemiol. 2004, 57, 1288–1294. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Consumo y Bienestar Social. Solicitud de Extracción de datos–Extraction Request (Spanish National Hospital Discharge Database). Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/2018_Formulario_Peticion_Datos_RAE_CMBD.pdf (accessed on 21 March 2023).
- Hardman, G.; Sutcliffe, R.; Hogg, R.; Mumford, L.; Grocott, L.; Mead-Regan, S.J.; Nuttall, J.; Dunn, S.; Seeley, P.; Clark, S.; et al. The impact of the SARS-CoV-2 pandemic and COVID-19 on lung transplantation in the UK: Lessons learned from the first wave. Clin. Transplant. 2021, 35, e14210. [Google Scholar] [CrossRef]
- Michel, S.; Witt, C.; Gottlieb, J.; Aigner, C. Impact of COVID-19 on Lung Transplant Activity in Germany—A Cross-Sectional Survey. Thorac. Cardiovasc. Surg. 2021, 69, 92–94. [Google Scholar] [CrossRef] [PubMed]
- Picard, C.; Le Pavec, J.; Tissot, A. Impact of the COVID-19 pandemic and lung transplantation program in France. Respir. Med. Res. 2020, 78, 100758. [Google Scholar] [CrossRef]
- King, T.E., Jr.; Bradford, W.Z.; Castro-Bernardini, S.; Fagan, E.A.; Glaspole, I.; Glassberg, M.K.; Gorina, E.; Hopkins, P.M.; Kardatzke, D.; Lancaster, L.; et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N. Engl. J. Med. 2014, 370, 2083–2092. [Google Scholar] [CrossRef] [PubMed]
- Richeldi, L.; du Bois, R.M.; Raghu, G.; Azuma, A.; Brown, K.K.; Costabel, U.; Cottin, V.; Flaherty, K.R.; Hansell, D.M.; Inoue, Y.; et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N. Engl. J. Med. 2014, 370, 2071–2082. [Google Scholar] [CrossRef] [PubMed]
- Laporta Hernandez, R.; Aguilar Perez, M.; Lázaro Carrasco, M.T.; Ussetti Gil, P. Lung Transplantation in IdiopathicPulmonary Fibrosis. Med. Sci. 2018, 6, 68. [Google Scholar] [CrossRef]
- Wei, D.; Gao, F.; Wu, B.; Zhou, M.; Zhang, J.; Yang, H.; Liu, D.; Fan, L.; Chen, J. Single versus bilateral lung transplantation for idiopathic pulmonary fibrosis. Clin. Respir. J. 2019, 13, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Grossman, R.F.; Frost, A.; Zamel, N.; Patterson, G.A.; Cooper, J.D.; Myron, P.R.; Dear, C.L.; Maurer, J. Results of single-lung transplantation for bilateral pulmonary fibrosis. The Toronto Lung Transplant Group. N. Engl. J. Med. 1990, 322, 727–733. [Google Scholar] [CrossRef]
- Thabut, G.; Christie, J.D.; Ravaud, P.; Castier, Y.; Dauriat, G.; Jebrak, G.; Fournier, M.; Lesèche, G.; Porcher, R.; Mal, H. Survival after bilateral versus single-lung transplantation for idiopathic pulmonary fibrosis. Ann. Intern. Med. 2009, 151, 767–774. [Google Scholar] [CrossRef]
- Schaffer, J.M.; Singh, S.K.; Reitz, B.A.; Zamanian, R.T.; Mallidi, H.R. Single- vs double-lung transplantation in patients with chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis since the implementation of lung allocation based on medical need. JAMA 2015, 313, 936–948. [Google Scholar] [CrossRef]
- Amor, M.; Rosengarten, D.; Shintenberg, D.; Pertzov, B.; Shostak, Y.; Kramer, M. Lung Transplantation in Idiopathic Pulmonary Fibrosis: Risk Factors and Outcome. Isr. Med. Assoc. J. 2020, 22, 741–746. [Google Scholar]
- Li, D.; Liu, Y.; Wang, B. Single versus bilateral lung transplantation in idiopathic pulmonary fibrosis: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0233732. [Google Scholar] [CrossRef] [PubMed]
- Spratt, J.R.; Tomic, R.; Brown, R.Z.; Rudser, K.; Loor, G.; Hertz, M.; Shumway, S.; Kelly, R.F. Single versus Bilateral Lung Transplantation for Idiopathic Pulmonary Fibrosis in the Lung Allocation Score Era. J. Surg. Res. 2019, 234, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Adegunsoye, A.; Strek, M.; Garrity, E.; Guzy, R.; Bag, R. Comprehensive Care of the Lung Transplant Patient. CHEST 2017, 152, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Balestro, E.; Calabrese, F.; Turato, G.; Lunardi, F.; Bazzan, E.; Marulli, G.; Biondini, D.; Rossi, E.; Sanduzzi, A.; Rea, F.; et al. Immune Inflammation and Disease Progression in Idiopathic Pulmonary Fibrosis. PLoS ONE 2016, 11, e0154516. [Google Scholar] [CrossRef] [PubMed]
- Bosa, S.; Vosa, R.; Van Raemdonck, D.; Verledena, G. Survival in adult lung transplantation: Where are we in 2020? Curr. Opin. Organ. Transplant. 2020, 25, 268–273. [Google Scholar] [CrossRef]
- Brouckaert, J.; Verleden, S.E.; Verbelen, T.; Coosemans, W.; Decaluwé, H.; De Leyn, P.; Depypere, L.; Nafteux, P.; Van Veer, H.; Meyns, B.; et al. Double-lung versus heart-lung transplantation for precapillary pulmonary arterial hypertension: A 24-year single-center retrospective study. Transpl. Int. 2019, 32, 717–729. [Google Scholar] [CrossRef]
- Diamond, J.M.; Lee, J.C.; Kawut, S.M.; Shah, R.J.; Localio, A.R.; Bellamy, S.L.; Lederer, D.J.; Cantu, E.; Kohl, B.A.; Lama, V.N.; et al. Clinical risk factors for primary graft dysfunction after lung transplantation. Am. J. Respir. Crit. Care Med. 2013, 187, 527–534. [Google Scholar] [CrossRef]
- Hoetzenecker, K.; Benazzo, A.; Stork, T.; Sinn, K.; Schwarz, S.; Schweiger, T.; Klepetko, W.; Vienna Lung Transplant Group. Bilateral lung transplantation on intraoperative extracorporeal membrane oxygenator: An observational study. J. Thorac. Cardiovasc. Surg. 2020, 160, 320–327.e1. [Google Scholar] [CrossRef]
- Snell, G.I.; Yusen, R.D.; Weill, D.; Strueber, M.; Garrity, E.; Reed, A.; Pelaez, A.; Whelan, T.P.; Perch, M.; Bag, R.; et al. Report of the ISHLT Working Group on Primary Lung Graft Dysfunction, part I: Definition and grading—A 2016 Consensus Group statement of the International Society for Heart and Lung Transplantation. J. Heart Lung Transplant. 2017, 36, 1097–1103. [Google Scholar] [CrossRef]
- Loor, G.; Mattar, A.; Schaheen, L.; Bremner, R. Surgical Complications of Lung Transplantation. Thorac. Surg. Clin. 2022, 32, 197–209. [Google Scholar] [CrossRef]
- Aguilar-Guisado, M.; Givaldá, J.; Ussetti, P.; Ramos, A.; Morales, P.; Blanes, M.; Bou, G.; de la Torre-Cisneros, J.; Román, A.; Borro, J.M.; et al. Pneumonia after lung transplantation in the RESITRA Cohort: A multicenter prospective study. Am. J. Transplant. 2007, 7, 1989–1996. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Huang, H.; Liu, S.; Yu, P.; Wan, Q. Staphylococcus aureus bacteremias following liver transplantation: A clinical analysis of 20 cases. Ther. Clin. Risk Manag. 2015, 11, 933–937. [Google Scholar] [CrossRef] [PubMed]
- Yun, J.H.; Lee, S.O.; Jo, K.W.; Choi, S.H.; Lee, J.; Chae, E.J.; Do, K.H.; Choi, D.K.; Choi, I.C.; Hong, S.B.; et al. Infections after lung transplantation: Time of occurrence, sites, and microbiologic etiologies. Korean J. Intern. Med. 2015, 30, 506–514. [Google Scholar] [CrossRef]
- Joean, O.; Welte, T.; Gottlieb, J. Chest Infections after Lung Transplantation. Chest 2022, 161, 937–948. [Google Scholar] [CrossRef] [PubMed]
- Bunsow, E.; Los-Arcos, I.; Martin-Gómez, M.T.; Bello, I.; Pont, T.; Berastegui, C.; Ferrer, R.; Nuvials, X.; Deu, M.; Peghin, M.; et al. Donor-derived bacterial infections in lung transplant recipients in the era of multidrug resistance. J. Infect. 2020, 80, 190–196. [Google Scholar] [CrossRef]
- Chang, A.; Musk, M.; Lavender, M.; Wrobel, J.; Yaw, M.C.; Lawrence, S.; Chirayath, S.; Boan, P. Cytomegalovirus viremia in lung transplantation during and after prophylaxis. Transpl. Infect. Dis. 2019, 21, e13069. [Google Scholar] [CrossRef]
- Prudencio-Ribera, V.C.; Corral-Blanco, M.; Jarrín-Estupiñán, M.E.; Alonso-Moralejo, R.; Pérez-González, V.; Martínez-Serna, I.; González-Serrano, M.; De Pablo-Gafas, A. Analysis of Intrahospital Mortality in Patients with Lung Transplant Due to Diffuse Parenchymal Lung Disease. Transplant. Proc. 2019, 51, 372–375. [Google Scholar] [CrossRef]
- Arango Tomás, E.A.; Algar Algar, F.J.; Cerezo Madueno, F.; Salvatierra Valazquez, A. Evolution and risk factors for early mortality after lung transplantation for idiopathic pulmonary fibrosis: An experience of 20 years. Transplant. Proc. 2015, 47, 2656.e8. [Google Scholar] [CrossRef]
- Chambers, D.C.; Perch, M.; Zuckermann, A.; Cherikh, W.S.; Harhay, M.O.; Hayes, D., Jr.; Hsich, E.; Khush, K.K.; Potena, L.; Sadavarte, A.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-eighth adult lung transplantation report-2021; Focus on recipient characteristics. J. Heart Lung Transplant. 2021, 40, 1060–1072. [Google Scholar] [CrossRef]
- Urlik, M.; Stącel, T.; Latos, M.; Antończyk, R.; Ferens, M.; Zawadzki, F.; Król, B.; Pasek, P.; Przybyłowski, P.; Zembala, M.; et al. Donor-related Risk Factors Associated with Increased Mortality after Lung Transplant. Transplant. Proc. 2020, 52, 2133–2137. [Google Scholar] [CrossRef]
- Mosher, C.; Weber, J.; Frankel, C.; Neely, M.; Palmer, S. Risk factors for mortality in lung transplant recipients aged ≥65 years: A retrospective cohort study of 5,815 patients in the scientific registry of transplant recipients. J. Heart Lung Transplant. 2021, 40, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Lund, L.H.; Edwards, L.B.; Kucheryavaya, A.Y.; Benden, C.; Dipchand, A.I.; Goldfarb, S.; Levvey, B.J.; Meiser, B.; Rossano, J.W.; Yusen, R.D.; et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-second Official Adult Heart Transplantation Report—2015; Focus Theme: Early Graft Failure. J. Heart Lung Transplant. 2015, 34, 1244–1254. [Google Scholar] [CrossRef] [PubMed]
- Fielding-Singh, V.; Grogan, T.R.; Neelankavil, J.P. Accuracy of administrative database estimates of national surgical volume: Solid organ transplantation in the National Inpatient Sample. Clin. Transplant. 2021, 35, e14441. [Google Scholar] [CrossRef] [PubMed]
- Registro Español de Trasplante Pulmonar. Resultados 2001–2020. Available online: http://www.ont.es/infesp/Documents/MEMORIA%20ANUAL%20RETP%202001-2020.pdf (accessed on 19 May 2023).
- Merlo, C.A.; Weiss, E.S.; Orens, J.B.; Borja, M.C.; Diener-West, M.; Conte, J.V.; Shah, A.S. Impact of U.S. Lung Allocation Score on survival after lung transplantation. J. Heart Lung Transplant. 2009, 28, 769–775. [Google Scholar] [CrossRef]
| 2016 | 2017 | 2018 | 2019 | 2020 | TOTAL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No IPF | IPF | No IPF | IPF | No IPF | IPF | No IPF | IPF | No IPF | IPF | No IPF | IPF | ||
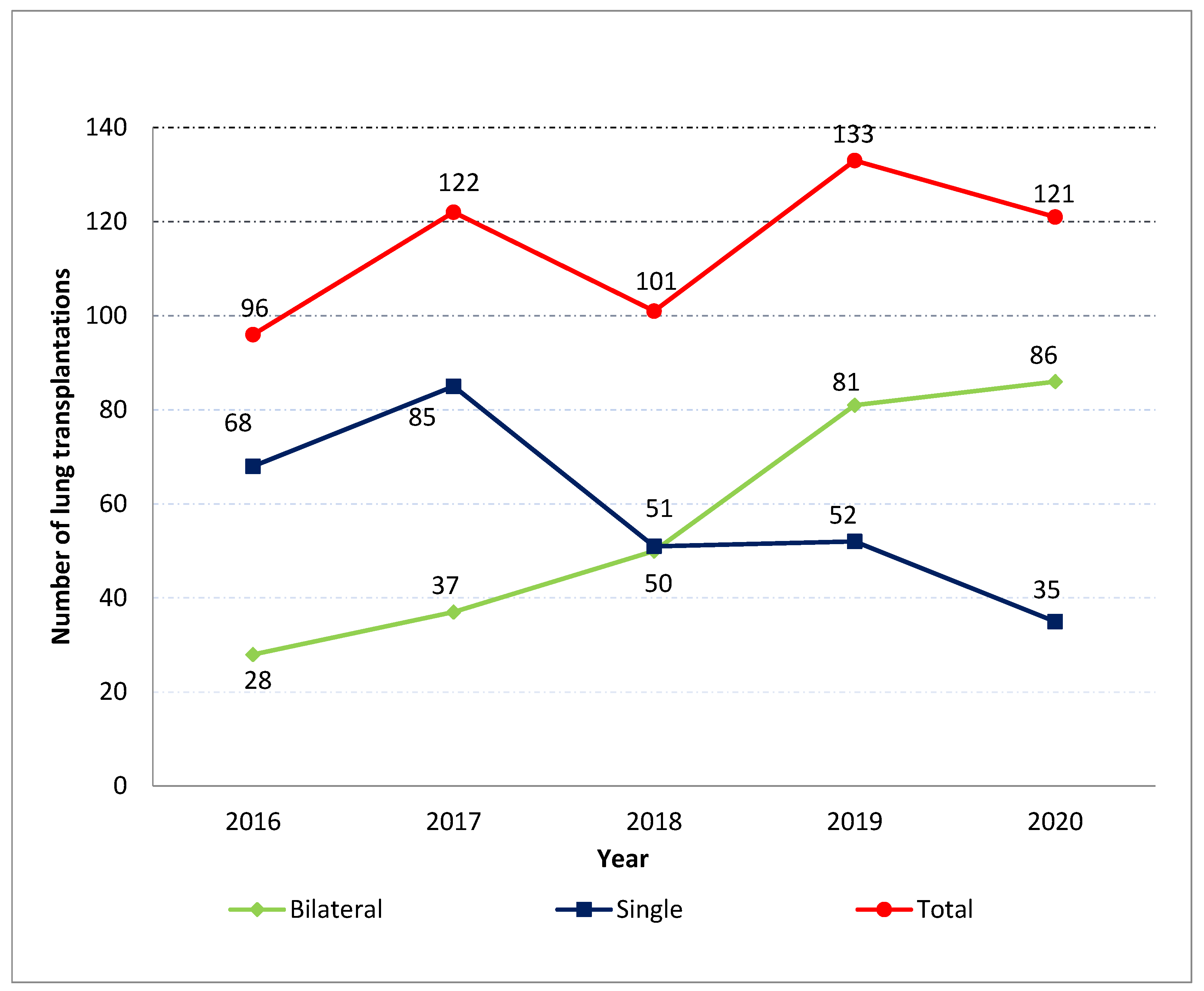
| N. of transplantations | 215 | 96 | 228 | 122 | 260 | 101 | 282 | 133 | 219 | 121 | 1204 | 573 | |
| Type, n (%) | Single abc | 98 (45.6) | 68 (70.8) | 104 (45.6) | 85 (69. 7) | 53 (20.4) | 51 (50.5) | 50 (17.7) | 52 (39.1) | 43 (19.6) | 35 (28.9) | 348 (28.9) | 291 (50.8) |
| Bilateral abc | 117 (54.4) | 28 (29.2) | 124 (54.4) | 37 (30.3) | 207 (79.6) | 50 (49.5) | 232 (82.3) | 81 (60.9) | 176 (80.4) | 86 (71.1) | 856 (71.1) | 282 (49.2) | |
| Female sex, n (%) c | 83 (38.6) | 25 (26.0) | 88 (38.6) | 32 (26.2) | 114 (43.9) | 26 (25.7) | 116 (41.1) | 37 (27.8) | 91 (41.6) | 21 (17.4) | 492 (40.9) | 141 (24.6) | |
| Age, mean (SD) bc | 49.0 (15.9) | 56.4 (9.5) | 50.5 (13.4) | 58.1 (8.9) | 51.6 (13.6) | 58.4 (8.5) | 52.7 (13.7) | 58.2 (9.2) | 52.6 (14.3) | 59.1 (9.0) | 51.4 (14.2) | 58.1 (9.0) | |
| <45 years, n (%) c | 63 (29.3) | 11 (11.5) | 63 (27.6) | 11 (9.0) | 61 (23.5) | 6 (6.0) | 63 (22.3) | 12 (9.0) | 49 (22.4) | 5 (4.1) | 299 (24.8) | 45 (7.9) | |
| 45–54 years, n (%) c | 42 (19.5) | 14 (14.6) | 45 (19.7) | 20 (16.4) | 48 (18.5) | 16 (15.8) | 50 (17.7) | 21 (15.8) | 36 (16.4) | 17 (14.0) | 221 (18.4) | 88 (15.4) | |
| 55–64 years, n (%) c | 91 (42.3) | 52 (54.2) | 105 (46.1) | 63 (51.6) | 130 (50.0) | 60 (59.4) | 130 (46.1) | 72 (54.1) | 110 (50.2) | 72 (59.5) | 566 (47.0) | 319 (55.7) | |
| ≥65 years, n (%) c | 19 (8.8) | 19 (19.8) | 15 (6.6) | 28 (23.0) | 21 (8.1) | 19 (18.8) | 39 (13.8) | 28 (21.1) | 24 (11.0) | 27 (22.3) | 118 (9.8) | 121 (21.1) | |
| CCI, n (%) | 0 c | 38 (17.7) | 53 (55.2) | 28 (12.3) | 55 (45.1) | 56 (21.5) | 48 (47.5) | 49 (17.4) | 61 (45.9) | 36 (16.4) | 57 (47.1) | 207 (17.2) | 274 (47.8) |
| ≥1 c | 177 (82.3) | 43 (44.8) | 200 (87.7) | 67 (54.9) | 204 (78.5) | 53 (52.5) | 233 (82.6) | 72 (54.1) | 183 (83.6) | 64 (52.9) | 997 (82.8) | 299(52.2) | |
| CCI, mean (SD) c | 1.2 (0.9) | 0.78 (1.2) | 1.25 (0.9) | 0.78 (0.9) | 1.09 (0.9) | 0.76 (0.9) | 1.29 (1.1) | 0.81 (1.0) | 1.26 (1.0) | 0.86 (1.2) | 1.22 (1.0) | 0.8 (1.0) | |
| LOHS, mean (SD) c | 54.2 (53.8) | 48.5 (42.4) | 46.8 (37.5) | 42.1 (32.3) | 47.6 (42.3) | 44.8 (39.4) | 49.0 (37.4) | 49.6 (40.9) | 46.3 (41.9) | 39.1 (26.1) | 48.7 (42.6) | 44.7 (36.5) | |
| IHM, n (%) | 21 (9.8) | 13 (13.5) | 22 (9.7) | 15 (12.3) | 32 (12.3) | 7 (6.9) | 34 (12.1) | 16 (12.0) | 29 (13.2) | 17 (14.1) | 138 (11.5) | 68 (11.9) | |
| IPF | 2016 | 2017 | 2018 | 2019 | 2020 | TOTAL | |
|---|---|---|---|---|---|---|---|
| Myocardial infarction, n (%) | Yes | 0 (0) | 2 (1.6) | 2 (2.0) | 1 (1.0) | 1 (0.8) | 6 (1.1) |
| No | 2 (0.9) | 2 (0.9) | 2 (0.8) | 9 (3.2) | 3 (1.4) | 18 (1.5) | |
| Congestive heart failure, n (%) | Yes | 5 (5.2) | 11 (9.0) | 9 (9.0) | 7 (5.3) | 7 (5.8) | 39 (6.8) |
| No | 11 (5.1) | 13 (5.7) | 9 (3.5) | 21 (7.5) | 7 (3.2) | 61 (5.1) | |
| Peripheral vascular disease, n (%) | Yes | 0 (0) | 1 (0.8) | 2 (2.0) | 1 (0.8) | 5 (4.1) | 9 (1.6) |
| No | 4 (1.9) | 3 (1.3) | 5 (1.9) | 6 (2.1) | 6 (2.7) | 24 (2.0) | |
| Cerebrovascular disease, n (%) | Yes | 3 (3.1) | 3 (2.5) | 2 (2.0) | 4 (3.0) | 6 (5.0) | 18 (3.1) |
| No | 7 (3.3) | 7 (3.1) | 10 (3.9) | 4 (1.4) | 14 (6.4) | 42 (3.5) | |
| Dementia, n (%) | Yes | 0 (0) | 0 (0) | 0 (0) | 1 (0.8) | 0 (0) | 1 (0.2) |
| No | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Rheumatoid disease, n (%) b | Yes | 9 (9.4) | 12 (9.8) | 7 (6.9) | 10 (7.5) | 7 (5.8) | 45 (7.9) |
| No | 6 (2.8) | 11 (4.8) | 11 (4.2) | 8 (2.8) | 6 (2.7) | 42 (3.5) | |
| Peptic ulcer disease, n (%) | Yes | 1 (1.0) | 0 (0) | 0 (0) | 0 (0) | 2 (1.7) | 3 (0.5) |
| No | 1 (0.5) | 2 (0.9) | 3 (1.2) | 2 (0.7) | 2 (0.9) | 10 (0.8) | |
| Moderate or severe liver disease, n (%) | Yes | 3 (3.1) | 5 (4.1) | 8 (7.9) | 12 (9.0) | 8 (6.6) | 36 (6.3) |
| No a | 9 (4.2) | 13 (5.7) | 14 (5.4) | 32 (11.4) | 22 (10.1) | 90 (7.5) | |
| Diabetes and diabetes with complications, n (%) | Yes | 10 (10.4) | 19 (15.6) | 15 (14.9) | 19 (14.3) | 10 (8.3) | 73 (12.7) |
| No | 29 (13.5) | 25 (11.0) | 28 (10.8) | 23 (8.2) | 17 (7.8) | 122 (10.1) | |
| Hemiplegia or paraplegia, n (%) | Yes | 0 (0) | 2 (1.6) | 0 (0) | 0 (0) | 0 (0) | 2 (0.4) |
| No a | 3 (1.4) | 0 (0) | 0 (0) | 2 (0.7) | 5 (2.3) | 10 (0.8) | |
| Renal disease, n (%) | Yes | 1 (1.0) | 1 (0.8) | 1 (1.0) | 3 (2.3) | 3 (2.5) | 9 (1.6) |
| No a | 6 (2.8) | 12 (5.3) | 4 (1.5) | 3 (1.1) | 5 (2.3) | 30 (2.5) | |
| Cancer and metastatic solid tumour, n (%) | Yes | 2 (2.1) | 1 (0.8) | 1 (1.0) | 2 (1.5) | 7 (5.8) | 13 (2.3) |
| No a | 6 (2.8) | 3 (1.3) | 5 (1.9) | 15 (5.3) | 4 (1.8) | 33 (2.7) | |
| AIDS/HIV, n (%) | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| No | 0 (0) | 0 (0) | 1 (0.38) | 0 (0) | 1 (0.5) | 2 (0.2) | |
| Pulmonary hypertension, n (%) | Yes a | 21 (21.9) | 29 (23.8) | 25 (24.8) | 19 (14.3) | 40 (33.1) | 134 (23.4) |
| No | 47 (21.9) | 49 (21.5) | 57 (21.9) | 53 (18.8) | 50 (22.8) | 256 (21.3) | |
| Chronic Obstructive Pulmonary Disease, n (%) b | Yes | 12 (12.5) | 12 (9.8) | 16 (15.8) | 20 (15.0) | 15 (12.4) | 75 (13.1) |
| No | 113 (52.6) | 120 (52.6) | 140 (53.9) | 167 (59.2) | 135 (61.6) | 675 (56.1) | |
| Asthma, n (%) b | Yes | 2 (2.1) | 1 (0.8) | 0 (0) | 2 (1.5) | 0 (0) | 5 (0.9) |
| No | 3 (1.4) | 4 (1.8) | 8 (3.1) | 9 (3.2) | 4 (1.8) | 28 (2.3) | |
| Current tobacco use, n (%) | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| No | 1 (0.5) | 0 (0) | 2 (0.8) | 0 (0) | 0 (0) | 3 (0.3) | |
| Haemodialysis, n (%) | Yes | 3 (3.1) | 5 (4.1) | 4 (4.0) | 11 (8.3) | 12 (9.9) | 35 (6.1) |
| No | 18 (8.4) | 22 (9.7) | 18 (6.9) | 18 (6.4) | 19 (8.7) | 95 (7.9) | |
| Extracorporeal membrane oxygenation, n (%) | Yes a | 14 (14.6) | 14 (11.5) | 22 (21.8) | 31 (23.3) | 30 (24.8) | 111 (19.4) |
| No a | 31 (14.4) | 39 (17.1) | 45 (17.3) | 76 (27.0) | 59 (26.9) | 250 (20.8) | |
| Tracheostomy, n (%) | Yes | 23 (24.0) | 24 (19.7) | 24 (23.8) | 39 (29.3) | 27 (22.3) | 137 (23.9) |
| No | 45 (20.9) | 49 (21.5) | 68 (26.2) | 63 (22.3) | 45 (20.6) | 270 (22.4) |
| IPF | 2016 | 2017 | 2018 | 2019 | 2020 | TOTAL | |
|---|---|---|---|---|---|---|---|
| Lung transplant rejection, n (%) | Yes a | 15 (15.6) | 20 (16.4) | 32 (31.7) | 39 (29.3) | 36 (29.8) | 142 (24.8) |
| No a | 35 (16.3) | 29 (12.7) | 84 (32.3) | 102 (36.2) | 56 (25.6) | 306 (25.4) | |
| Lung transplant failure, n (%) | Yes a | 1 (1.1) | 7 (5.7) | 12 (11.9) | 17 (12.8) | 16 (13.2) | 53 (9.3) |
| No a | 8 (3.7) | 10 (4.4) | 28 (10.8) | 22 (7.8) | 16 (7.3) | 84 (7.0) | |
| Lung transplant infection, n (%) | Yes a | 3 (3.1) | 10 (8.2) | 15 (14.9) | 25 (18.8) | 15 (12.4) | 68 (11.9) |
| No | 18 (8.4) | 22 (9.7) | 39 (15.0) | 35 (12.4) | 29 (13.2) | 143 (11.9) | |
| Other or unspecified complications of lung transplant, n (%) | Yes a | 19 (19.8) | 32 (26.2) | 21 (20.8) | 15 (11.3) | 17 (14.1) | 104 (18.2) |
| No a | 49 (22.8) | 61 (26.8) | 43 (16.5) | 43 (15.3) | 23 (10.5) | 219 (18.2) | |
| Any complication of lung transplant, n (%) | Yes a | 36 (37.5) | 58 (47.5) | 64 (63.4) | 71 (53.4) | 63 (52.1) | 292 (51.0) |
| No a | 89 (41.4) | 104 (45.6) | 151 (58.1) | 158 (56.1) | 98 (44.8) | 600 (49.8) | |
| Pneumonia, n (%) | Yes | 6 (6.3) | 5 (4.1) | 4 (4.0) | 10 (7.5) | 10 (8.3) | 35 (6.1) |
| No | 18 (8.4) | 18 (7.9) | 26 (10.0) | 18 (6.4) | 18 (8.2) | 98 (8.1) | |
| Ventilator-associated Pneumonia, n (%) | Yes | 1 (1.1) | 2 (1.6) | 1 (1.0) | 3 (2.3) | 1 (0.8) | 8 (1.4) |
| No | 2 (0.9) | 2 (0.9) | 2 (0.8) | 3 (1.1) | 7 (3.2) | 16 (1.3) | |
| Staphylococcus bacteraemia, n (%) | Yes | 9 (9.4) | 12 (9.8) | 11 (10.9) | 20 (15.1) | 15 (12.4) | 67 (11.7) |
| No | 23 (10.7) | 26 (11.4) | 33 (12.7) | 27 (9.6) | 26 (11.9) | 135 (11.2) | |
| Gram-negative bacteraemia, n (%) | Yes | 7 (7.3) | 9 (7.4) | 6 (5.9) | 8 (6.1) | 8 (6.6) | 38 (6.6) |
| No | 15 (7.0) | 12 (5.3) | 17 (6.5) | 23 (8.2) | 15 (6.9) | 82 (6.8) | |
| Pseudomonas aeruginosa, n (%) | Yes | 5 (5.2) | 11 (9.1) | 13 (12.9) | 11 (8.3) | 9 (7.4) | 49 (8.5) |
| No | 20 (9.3) | 16 (7.1) | 32 (12.3) | 19 (6.7) | 23 (10.5) | 110 (9.1) | |
| Aspergillus, n (%) | Yes | 6 (6.3) | 2 (1.6) | 6 (5.9) | 6 (4.5) | 3 (2.5) | 23 (4.1) |
| No | 11 (5.1) | 7 (3.1) | 15 (5.8) | 23 (8.2) | 10 (4.6) | 66 (5.5) | |
| Cytomegalovirus, n (%) | Yes | 2 (2.1) | 3 (2.5) | 5 (5.0) | 10 (7.5) | 2 (1.7) | 22 (3.8) |
| No | 3 (1.4) | 10 (4.4) | 19 (7.3) | 13 (4.6) | 17 (7.8) | 62 (5.2) |
| IPF | NO IPF | BOTH | ||
|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | ||
| Sex | Men | 1 | 1 | 1 |
| Women | 1.34 (0.75–2.39) | 1.14 (0.79–1.65) | 1.2 (0.88–1.63) | |
| Age groups | <45 years | 1 | 1 | 1 |
| 45–54 years | 1.15 (0.41–3.23) | 0.9 (0.52–1.55) | 0.92 (0.58–1.48) | |
| 55–64 years | 0.94 (0.37–2.36) | 0.9 (0.57–1.43) | 0.88 (0.59–1.31) | |
| ≥65 years | 0.55 (0.18–1.65) | 0.83 (0.41–1.7) | 0.64 (0.36–1.13) | |
| CCI index | 0 | 1 | 1 | 1 |
| ≥1 | 1.33 (0.78–2.28) | 0.83 (0.51–1.34) | 1.07 (0.75–1.53) | |
| Any complication of lung transplant | Yes | 1.47 (1.01–2.55) | 1.49 (1.03–2.15) | 1.48 (1.09–1.98) |
| Pulmonary hypertension | Yes | 2.48 (1.43–4.31) | 1.35 (0.89–2.05) | 1.7 (1.23–2.35) |
| Year | 2016 | 1 | 1 | 1 |
| 2017 | 0.82 (0.36–1.86) | 0.98 (0.52–1.85) | 0.93 (0.57–1.53) | |
| 2018 | 0.4 (0.15–1.1) | 1.21 (0.67–2.18) | 0.92 (0.56–1.5) | |
| 2019 | 0.88 (0.39–1.99) | 1.22 (0.68–2.19) | 1.1 (0.69–1.76) | |
| 2020 | 0.92 (0.41–2.08) | 1.4 (0.77–2.56) | 1.24 (0.77–1.99) | |
| IPF | Yes | NA | NA | 1.13 (0.8–1.59) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Muñiz Ballesteros, B.; Lopez-de-Andres, A.; Jimenez-Garcia, R.; Zamorano-Leon, J.J.; Carabantes-Alarcon, D.; Cuadrado-Corrales, N.; Del-Barrio, J.L.; Perez-Farinos, N.; De Miguel-Díez, J. Trends and Outcomes in Lung Transplantation in Patients with and without Idiopathic Pulmonary Fibrosis in Spain during the Period 2016–2020. Healthcare 2023, 11, 1534. https://doi.org/10.3390/healthcare11111534
López-Muñiz Ballesteros B, Lopez-de-Andres A, Jimenez-Garcia R, Zamorano-Leon JJ, Carabantes-Alarcon D, Cuadrado-Corrales N, Del-Barrio JL, Perez-Farinos N, De Miguel-Díez J. Trends and Outcomes in Lung Transplantation in Patients with and without Idiopathic Pulmonary Fibrosis in Spain during the Period 2016–2020. Healthcare. 2023; 11(11):1534. https://doi.org/10.3390/healthcare11111534
Chicago/Turabian StyleLópez-Muñiz Ballesteros, Belén, Ana Lopez-de-Andres, Rodrigo Jimenez-Garcia, Jose J. Zamorano-Leon, David Carabantes-Alarcon, Natividad Cuadrado-Corrales, Jose L. Del-Barrio, Napoleon Perez-Farinos, and Javier De Miguel-Díez. 2023. "Trends and Outcomes in Lung Transplantation in Patients with and without Idiopathic Pulmonary Fibrosis in Spain during the Period 2016–2020" Healthcare 11, no. 11: 1534. https://doi.org/10.3390/healthcare11111534
APA StyleLópez-Muñiz Ballesteros, B., Lopez-de-Andres, A., Jimenez-Garcia, R., Zamorano-Leon, J. J., Carabantes-Alarcon, D., Cuadrado-Corrales, N., Del-Barrio, J. L., Perez-Farinos, N., & De Miguel-Díez, J. (2023). Trends and Outcomes in Lung Transplantation in Patients with and without Idiopathic Pulmonary Fibrosis in Spain during the Period 2016–2020. Healthcare, 11(11), 1534. https://doi.org/10.3390/healthcare11111534









