Do Out-of-Pocket Payments for Care for Children under 5 Persist Even in a Context of Free Healthcare in Burkina Faso? Evidence from a Cross-Sectional Population-Based Survey
Abstract
1. Background
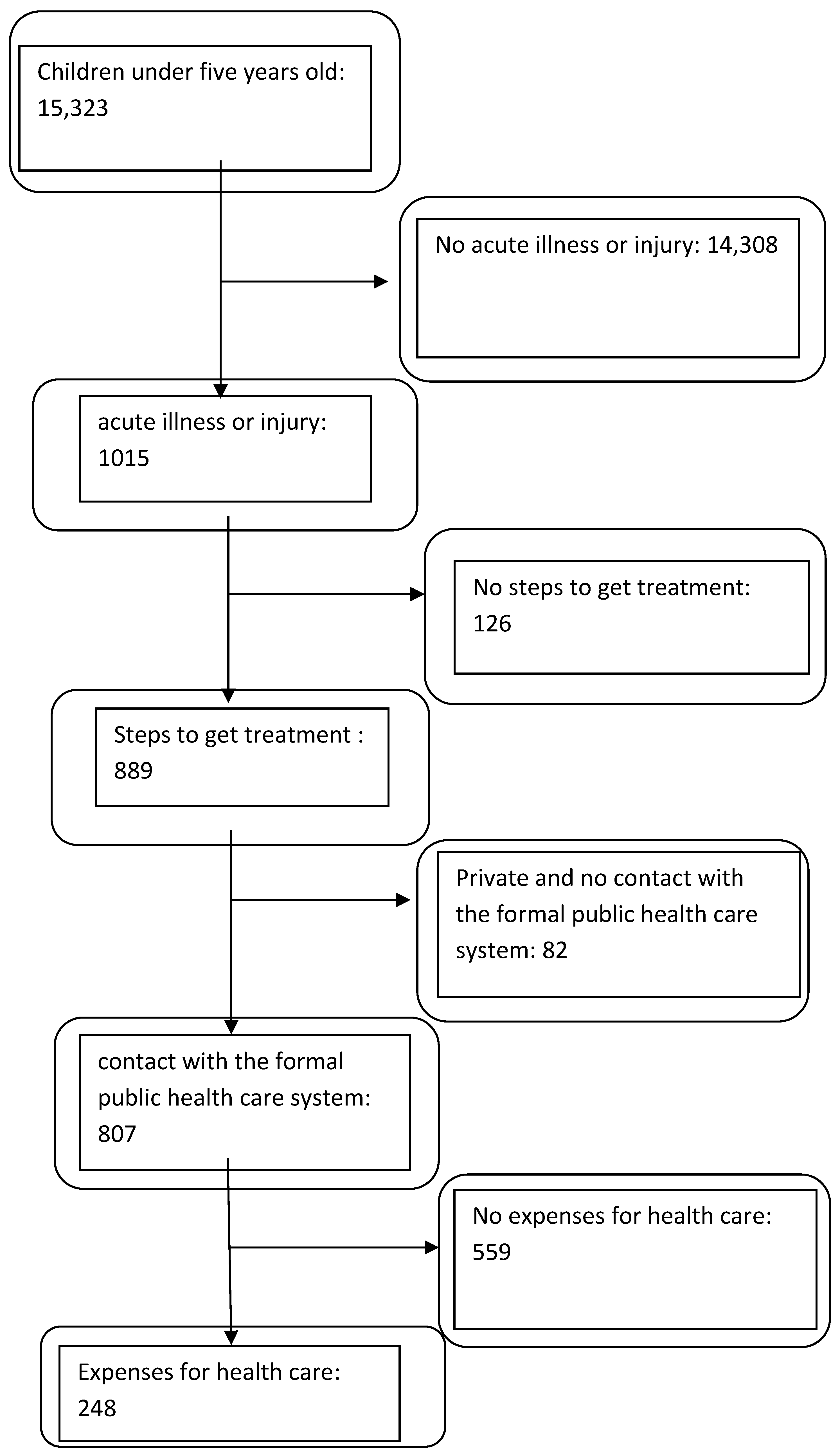
2. Methodology
2.1. Framework of the Study
2.2. The Free Care Policy for Children from 0 to 5 Years
2.3. Data and Data Sources
2.4. Description of the Sample
2.5. Description of the Variables and Their Measures
2.5.1. Variable of Interest
2.5.2. Explanatory (Control) Variables
2.6. Analytical Approach
2.7. Ethical Considerations
3. Results
3.1. Characteristics of Sample
3.2. Direct Childcare Services Payments
3.3. Factors Associated with OOP Payments
4. Discussion
Methodological Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Richard, F.; Witter, S.; de Brouwere, V. Innovative Approaches to Reducing Financial Barriers to Obstetric Care in Low-Income Countries. Am. J. Public Health 2010, 100, 1845–1852. [Google Scholar] [CrossRef] [PubMed]
- Shahrawat, R.; Rao, K.D. Insured yet vulnerable: Out-of-pocket payments and India’s poor. Health Policy Plan. 2012, 27, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Saksena, P.; Hsu, J.; Evans, D.B. Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges. PLoS Med. 2014, 11, e1001701. [Google Scholar] [CrossRef] [PubMed]
- Hercot, D.; Meessen, B.; Ridde, V.; Gilson, L. Removing user fees for health services in low-income countries: A multi-country review framework for assessing the process of policy change. Health Policy Plan. 2011, 26, ii5–ii15. [Google Scholar] [CrossRef] [PubMed]
- Ridde, V.; Morestin, F. A scoping review of the literature on the abolition of user fees in health care services in Africa. Health Policy Plan. 2011, 26, 1–11. [Google Scholar] [CrossRef]
- Lagarde, M.; Palmer, N. The impact of user fees on access to health services in low- and middle-income countries. Cochrane Database Syst. Rev. 2011, CD009094. [Google Scholar] [CrossRef]
- Dalinjong, P.A.; Wang, A.Y.; Homer, C.S.E. Has the free maternal health policy eliminated out of pocket payments for maternal health services? Views of women, health providers and insurance managers in Northern Ghana. PLoS ONE 2018, 13, e0184830. [Google Scholar] [CrossRef] [PubMed]
- Kaonga, O.; Banda, C.; Masiye, F. Hardship financing of out-of-pocket payments in the context of free healthcare in Zambia. PLoS ONE 2019, 14, e0214750. [Google Scholar] [CrossRef]
- Masiye, F.; Kaonga, O.; Kirigia, J.M. Does User Fee Removal Policy Provide Financial Protection from Catastrophic Health Care Payments? Evidence from Zambia. PLoS ONE 2016, 11, e0146508. [Google Scholar] [CrossRef]
- Mathonnat, J.; Audibert, M.; Belem, S. Analyzing the Financial Sustainability of User Fee Removal Policies: A Rapid First Assessment Methodology with a Practical Application for Burkina Faso. Appl. Health Econ. Health Policy 2020, 18, 767–780. Available online: http://link.springer.com/10.1007/s40258-019-00506-2 (accessed on 13 January 2020). [CrossRef]
- Nakovics, M.I.; Brenner, S.; Robyn, P.J.; Tapsoba, L.D.G.; De Allegri, M. Determinants of individual healthcare expenditure: A cross-sectional analysis in rural Burkina Faso. Int. J. Health Plan. Manag. 2019, 34, e1478–e1494. Available online: http://doi.wiley.com/10.1002/hpm.2812 (accessed on 26 July 2019). [CrossRef] [PubMed]
- Ridde, V.; Diarra, A.; Moha, M. User fees abolition policy in Niger: Comparing the under five years exemption implementation in two districts. Health Policy 2011, 99, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Zombré, D.; De Allegri, M.; Ridde, V. Immediate and sustained effects of user fee exemption on healthcare utilization among children under five in Burkina Faso: A controlled interrupted time-series analysis. Soc. Sci. Med. 2017, 179, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Ministère de la Santé et de la Prévention. Burkina Faso Stratégie Nationale de Mise en Oeuvre de la Politique Nationale de Gratuité des Soins (2018–2022); Ministère de la Santé et de la Prévention: Paris, France, 2017.
- Richard, F.; Antony, M.; Witter, S.; Kelley, A.; Kafando, Y.; Meessen, B. Fee Exemption for Maternal Care in Sub-Saharan Africa: A Review of 11 Countries and Lessons for the Region. Glob. Health Gov. 2013, 6, 52–72. [Google Scholar]
- Meda, I.B.; Baguiya, A.; Ridde, V.; Ouédraogo, H.G.; Dumont, A.; Kouanda, S. Out-of-pocket payments in the context of a free maternal health care policy in Burkina Faso: A national cross-sectional survey. Health Econ. Rev. 2019, 9, 1–14. Available online: https://healtheconomicsreview.springeropen.com/articles/10.1186/s13561-019-0228-8 (accessed on 5 May 2019). [CrossRef]
- Ridde, V.; Agier, I.; Jahn, A.; Mueller, O.; Tiendrebéogo, J.; Yé, M.; De Allegri, M. The impact of user fee removal policies on household out-of-pocket spending: Evidence against the inverse equity hypothesis from a population based study in Burkina Faso. Eur. J. Health Econ. 2015, 16, 55–64. [Google Scholar] [CrossRef]
- Nguyen, H.T. Economic Evaluation of User-Fee Exemption Policies for Maternal Healthcare in Burkina Faso: Evidence From a Cost-Effectiveness Analysis. VALUE Health 2020, 23, 300–308. [Google Scholar] [CrossRef]
- KI, E. Le Taux de Pauvreté Passe de 47% à 40.1% au Burkina Faso. Available online: http://www.ecodufaso.com/le-taux-de-pauvrete-passe-de-47-a-401-au-burkina-faso/ (accessed on 11 May 2018).
- Ecofin, A. Le Classement des Pays Africains Dans L’édition 2016 de L’indice de Développement Humain du PNUD. Available online: https://www.agenceecofin.com/economie/2403-45994-le-classement-des-pays-africains-dans-l-edition-2016-de-l-indice-de-developpement-humain-du-pnud (accessed on 28 March 2018).
- Ministère de la Santé du Burkina Faso. Annuaire Statistique Ministère de la Santé. Available online: https://www.sante.gov.bf/fileadmin/annuaire_2020_mshp.pdf (accessed on 28 March 2022).
- Ketsela, T.; Habimana, P.; Martines, J.; Mbewe, A.; Williams, A.; Sabiiti, J.N.; Thiam, A.; Narayanan, I.; Bahl, R. Prise en charge intégrée des maladies de l’enfance (PCIME). In Donnons Sa Chance à chaque Nouveau-né de L’Afrique; 2010; Volume 10, Available online: https://www.who.int/pmnch/media/publications/oanfr_III_5.pdf (accessed on 28 March 2023).
- Kolenikov, S.; Angeles, G. Socioeconomic Status Measurement with Discrete Proxy Variables: Is Principal Component Analysis a Reliable Answer? Rev. Income Wealth 2009, 55, 128–165. [Google Scholar] [CrossRef]
- Vyas, S.; Kumaranayake, L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006, 21, 459–468. [Google Scholar] [CrossRef]
- Shete, S.; Beasley, T.M.; Etzel, C.J.; Fernández, J.R.; Chen, J.; Allison, D.B.; Amos, C.I. Effect of Winsorization on Power and Type 1 Error of Variance Components and Related Methods of QTL Detection. Behav. Genet. 2004, 34, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Mihaylova, B.; Briggs, A.; O’Hagan, A.; Thompson, S.G. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2010, 21, 897–916. [Google Scholar] [CrossRef] [PubMed]
- Belotti, F.; Deb, P.; Manning, W.G.; Norton, E.C. Twopm: Two-Part Models. Stata J. Promot. Commun. Stat. Stata 2015, 15, 3–20. [Google Scholar] [CrossRef]
- Deb, P.; Norton, E.C.; Manning, W.G. Health Econometrics Using Stata. Available online: https://www.routledge.com/Health-Econometrics-Using-Stata-1st-Edition/Deb-Norton-Manning/p/book/9781597182287 (accessed on 11 July 2020).
- World Bank. Poverty & Equity Data Portal. Poverty & Equity Data Portal—Burkina Faso. Available online: http://povertydata.worldbank.org/poverty/country/BFA (accessed on 9 November 2018).
- Meessen, B.; Zhenzhong, Z.; Damme, W.V.; Devadasan, N.; Criel, B.; Bloom, G. Iatrogenic poverty. Trop. Med. Int. Health 2003, 8, 581–584. [Google Scholar] [CrossRef] [PubMed]
- Sauerborn, R.; Adams, A.; Hien, M. Household strategies to cope with the economic costs of illness. Soc. Sci. Med. 1982 1996, 43, 291–301. [Google Scholar] [CrossRef]
- Asante, F.; Chikwama, C.; Daniels, A.; Armar-Klemesu, M. Evaluating the Economic Outcomes of the Policy of Fee Exemption for Maternal Delivery Care in Ghana. Ghana Med. J. 2007, 41, 110–117. [Google Scholar] [CrossRef]
- Kruk, M.E.; Mbaruku, G.; Rockers, P.C.; Galea, S. User fee exemptions are not enough: Out-of-pocket payments for “free” delivery services in rural Tanzania. Trop. Med. Int. Health 2008, 13, 1442–1451. [Google Scholar] [CrossRef]
- Carasso, B.S.; Lagarde, M.; Cheelo, C.; Chansa, C.; Palmer, N. Health worker perspectives on user fee removal in Zambia. Hum. Resour. Health 2012, 10, 40. [Google Scholar] [CrossRef]
- Ridde, V.; Leppert, G.; Hien, H.; Robyn, P.J.; De Allegri, M. Street-level workers’ inadequate knowledge and application of exemption policies in Burkina Faso jeopardize the achievement of universal health coverage: Evidence from a cross-sectional survey. Int. J. Equity Health 2018, 17, 5. [Google Scholar] [CrossRef]
- Sato, M.; Gilson, L. Exploring health facilities’ experiences in implementing the free health-care policy (FHCP) in Nepal: How did organizational factors influence the implementation of the user-fee abolition policy? Health Policy Plan. 2015, 30, 1272–1288. [Google Scholar] [CrossRef]
- Opwora, A.; Waweru, E.; Toda, M.; Noor, A.; Edwards, T.; Fegan, G.; Molyneux, S.; Goodman, C. Implementation of patient charges at primary care facilities in Kenya: Implications of low adherence to user fee policy for users and facility revenue. Health Policy Plan. 2015, 30, 508–517. [Google Scholar] [CrossRef] [PubMed]
- Castellani, J.; Mihaylova, B. Out-of-Pocket Costs and Other Determinants of Access to Healthcare for Children with Febrile Illnesses: A Case-Control Study in Rural Tanzania. PLoS ONE 2015, 10, e0122386. [Google Scholar] [CrossRef]
- Hendrix, N.; Bar-Zeev, N.; Atherly, D.; Chikafa, J.; Mvula, H.; Wachepa, R.; Crampin, A.C.; Mhango, T.; Mwansambo, C.; Heyderman, R.S.; et al. The economic impact of childhood acute gastroenteritis on Malawian families and the healthcare system. Open Access 2017, 7, e017347. [Google Scholar] [CrossRef] [PubMed]
- Laokri, S. Assessing out-of-pocket expenditures for primary health care: How responsive is the Democratic Republic of Congo health system to providing financial risk protection? BMC Health Serv. Res. 2018, 18, 451. [Google Scholar] [CrossRef] [PubMed]
- Taffa, N.; Chepngeno, G. Determinants of health care seeking for childhood illnesses in Nairobi slums. Trop. Med. Int. Health 2005, 10, 6. [Google Scholar] [CrossRef] [PubMed]
- Riner, B.; Bussy, A.; Hélène-Pelage, J.; Moueza, N.; Lamy, S.; Carrère, P. “No generics, Doctor!” The perspective of general practitioners in two French regions. BMC Health Serv. Res. 2017, 17, 707. [Google Scholar] [CrossRef]
- Dunne, S.S.; Dunne, C.P. What do people really think of generic medicines? A systematic review and critical appraisal of literature on stakeholder perceptions of generic drugs. BMC Med. 2015, 13, 173. [Google Scholar] [CrossRef]
- Sauerborn, R.; Berman, P.; Nougtara, A. Age bias, but no gender bias, in the intra-household resource allocation for health care in rural Burkina Faso. Health Transit. Rev. 1996, 23, 131–145. [Google Scholar]
- Mugisha, F.; Kouyate, B.; Gbangou, A.; Sauerborn, R. Examining out-of-pocket expenditure on health care in Nouna, Burkina Faso: Implications for health policy. Trop. Med. Int. Health 2002, 7, 10. [Google Scholar] [CrossRef]
- Hjortsberg, C. Why do the sick not utilise health care? The case of Zambia. Health Econ. 2003, 12, 755–770. [Google Scholar] [CrossRef]
- Tey, N.; Lai, S. Correlates of and Barriers to the Utilization of Health Services for Delivery in South Asia and Sub-Saharan Africa. Sci. World J. 2013, 2013, 423403. [Google Scholar] [CrossRef] [PubMed]
- Heijink, R.; Xu, K.; Saksena, P.; Evans, D.; WHO. Validity and Comparability of Out of Pocket Health Expenditure from Household Surveys a Review of the Literature and Current Survey Instruments. 2011. Available online: http://www.who.int/health_financing/documents/covdp_e_11_01oop_errors/en/ (accessed on 10 September 2018).
| Mesurements and Categorization | |
|---|---|
| Variables of Interest | |
| Probability of out-of-pocket expenditure | 0 = No; 1 = Yes |
| Out-of-pocket expenditure [FRS CFA] | Continuous |
| Explanatory variables | |
| Age (months) | 1= (0–6); 2= (7–23); 3 =(24–59) |
| Sex | 0 = Boy; 1 = Girl |
| Perceived illness severity | 0 = No effect on activities; 1 = Any effect on activities |
| Hospitalization | 0 = No; 1 = Yes |
| Distance from household to nearest health facility (km) | 0= ≤ 5 km; 1= > 5 km |
| Place of residence | 0 = Rural; 1 = Urban |
| Poverty status (SES) | 0 = Other; 1 = Poor (Socio-economic status/quintile 1) |
| Mother’s level of education in the household | 0= Uneducated; 1= Educated |
| District Fbr | 0 = No; 1 = Yes |
| Region | 1 = Boucle du Mouhoun; 2 = Center est; 3 = Center nord; 4 = Center ouest; 5= Nord; 6 = Sud ouest |
| N | % | Average (Frs CFA) | SD (Frs CFA) | Median (Frs CFA) | Min (Frs CFA) | Max (Frs CFA) | |
|---|---|---|---|---|---|---|---|
| Probability of OOPE among those who used formal services (n = 807) | |||||||
| OOP = 0 | 559 | 69 | NA | NA | NA | NA | NA |
| OOP > 0 | 248 | 31 | 3407.77 | 2839.53 | 3200 | 100 | 10,000 |
| Components of OOPE (n = 248) | |||||||
| Consultation fees | 59 | 24 | 3269.06 | 3459.1 | 1500 | 100 | 10,100 |
| Laboratory/radiography and surgery costs (examinations) | 5 | 2 | 4100 | 1341.64 | 5000 | 2000 | 5000 |
| Drugs | 237 | 96 | 2895.33 | 2388.14 | 2000 | 100 | 8000 |
| Hospitalization costs | 11 | 4 | 12,209.09 | 16,358.74 | 5050 | 750 | 50,000 |
| Total direct health payments | 248 | 100 | 3407.77 | 2839.53 | 3200 | 100 | 10,000 |
| Transports | 109 | 44 | 728.73 | 210.70 | 700 | 300 | 1000 |
| Characteristics | Children Who Paid (n = 248) | Children Who Did not Pay (n = 559) | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age groups (months) | 0.012 | ||||
| (0–6) | 58 | 40.28 | 86 | 59.72 | |
| (7–23) | 119 | 27.17 | 319 | 72.83 | |
| (24–59) | 71 | 31.56 | 154 | 68.44 | |
| Perceived illness severity | 0.099 | ||||
| No effect | 92 | 27.54 | 242 | 72.46 | |
| Effect | 156 | 32.98 | 317 | 67.02 | |
| Poverty indices | 0.009 | ||||
| Not poor | 216 | 32.73 | 444 | 67.27 | |
| Poor (the poorest) | 32 | 21.77 | 115 | 78.23 | |
| Mother’s level of education in the household | 0.708 | ||||
| Uneducated | 195 | 30.42 | 446 | 69.58 | |
| Educated | 53 | 31.93 | 113 | 68.07 | |
| Place of residence | 0.000 | ||||
| Rural | 206 | 28.22 | 524 | 71.78 | |
| Urban | 42 | 54.55 | 35 | 45.45 | |
| Proximity to a health center (distance in km) | 0.472 | ||||
| ≤5 km | 187 | 31.43 | 408 | 68.57 | |
| >5 km | 61 | 28.77 | 151 | 71.23 | |
| District Fbr | 0.621 | ||||
| No | 49 | 29.17 | 119 | 70.83 | |
| Yes | 199 | 31.14 | 440 | 68.86 | |
| Region | 0.000 | ||||
| Boucle du Mouhoun | 30 | 26.79 | 82 | 73.21 | |
| Center Est | 67 | 48.2 | 72 | 51.8 | |
| Center Nord | 44 | 32.35 | 92 | 67.65 | |
| Center Ouest | 38 | 27.74 | 99 | 72.26 | |
| Nord | 56 | 26.17 | 158 | 73.83 | |
| Sud Ouest | 13 | 18.84 | 56 | 81.16 | |
| Part 1: Likelihood of Having a Direct Payment (n = 807) | Part 2: Determinants of the Amount of OOPE (n = 248) | |||||
|---|---|---|---|---|---|---|
| Explanatory Variables | OR | 95% CI | p-Value | Coeff | 95% CI | p-Value |
| Age group (months) | ||||||
| (0–6 months) | 1 | 0 | ||||
| (7–23 months) | 0.52 | 0.35–0.83 | 0.003 *** | −0.09 | −0.39–0.19 | 0.51 |
| (24–59 months) | 0.62 | 0.39–1.01 | 0.052 * | −0.015 | −0.33–0.30 | 0.92 |
| Hospitalization | ||||||
| No | 1 | 0 | ||||
| Yes | 4.53 | 1.92–8.88 | <0.001 *** | 0.78 | 0.38–1.17 | <0.001 *** |
| Perceived illness severity | ||||||
| No effect | 1 | 0 | ||||
| Effect | 1.53 | 1.07–2.09 | 0.018 ** | 0.24 | −0.003–0.49 | 0.047 ** |
| Place of residence | ||||||
| Rural | 1 | 0 | ||||
| Urban | 3.47 | 1.88–5.34 | <0.001 *** | 0.34 | −0.032–0.66 | 0.031 ** |
| Poverty Indices | ||||||
| Not poor | 1 | 0 | ||||
| Poor | 0.67 | 0.44–1.07 | 0.098 * | 0.09 | −0.25–0.45 | 0.61 |
| Regions | ||||||
| South-West | 1 | 0 | ||||
| Boucle du Mouhoun | 1.51 | 0.70–3.28 | 0.288 | −0.02 | −0.63–0.58 | 0.945 |
| Central-East | 4.50 | 2.18–9.29 | <0.001 *** | 0.60 | 0.06–1.14 | 0.029 ** |
| Central-North | 2.43 | 1.16–5.08 | 0.018 ** | 0.59 | 0.02–1.16 | 0.040 ** |
| Centre-West | 1.60 | 0.75–3.37 | 0.216 | 0.76 | 0.18–1.34 | 0.01 ** |
| North | 1.71 | 0.84–3.48 | 0.137 | 0.23 | −32–0.78 | 0.409 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tapsoba, L.D.G.; Yara, M.; Nakovics, M.I.; Somda, S.M.A.; Lohmann, J.; Robyn, P.J.; Hamadou, S.; Hien, H.; De Allegri, M. Do Out-of-Pocket Payments for Care for Children under 5 Persist Even in a Context of Free Healthcare in Burkina Faso? Evidence from a Cross-Sectional Population-Based Survey. Healthcare 2023, 11, 1379. https://doi.org/10.3390/healthcare11101379
Tapsoba LDG, Yara M, Nakovics MI, Somda SMA, Lohmann J, Robyn PJ, Hamadou S, Hien H, De Allegri M. Do Out-of-Pocket Payments for Care for Children under 5 Persist Even in a Context of Free Healthcare in Burkina Faso? Evidence from a Cross-Sectional Population-Based Survey. Healthcare. 2023; 11(10):1379. https://doi.org/10.3390/healthcare11101379
Chicago/Turabian StyleTapsoba, Ludovic D. G., Mimbouré Yara, Meike I. Nakovics, Serge M. A. Somda, Julia Lohmann, Paul J. Robyn, Saidou Hamadou, Hervé Hien, and Manuela De Allegri. 2023. "Do Out-of-Pocket Payments for Care for Children under 5 Persist Even in a Context of Free Healthcare in Burkina Faso? Evidence from a Cross-Sectional Population-Based Survey" Healthcare 11, no. 10: 1379. https://doi.org/10.3390/healthcare11101379
APA StyleTapsoba, L. D. G., Yara, M., Nakovics, M. I., Somda, S. M. A., Lohmann, J., Robyn, P. J., Hamadou, S., Hien, H., & De Allegri, M. (2023). Do Out-of-Pocket Payments for Care for Children under 5 Persist Even in a Context of Free Healthcare in Burkina Faso? Evidence from a Cross-Sectional Population-Based Survey. Healthcare, 11(10), 1379. https://doi.org/10.3390/healthcare11101379







