Effects of a Post-Traumatic Growth Program on Young Korean Breast Cancer Survivors
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
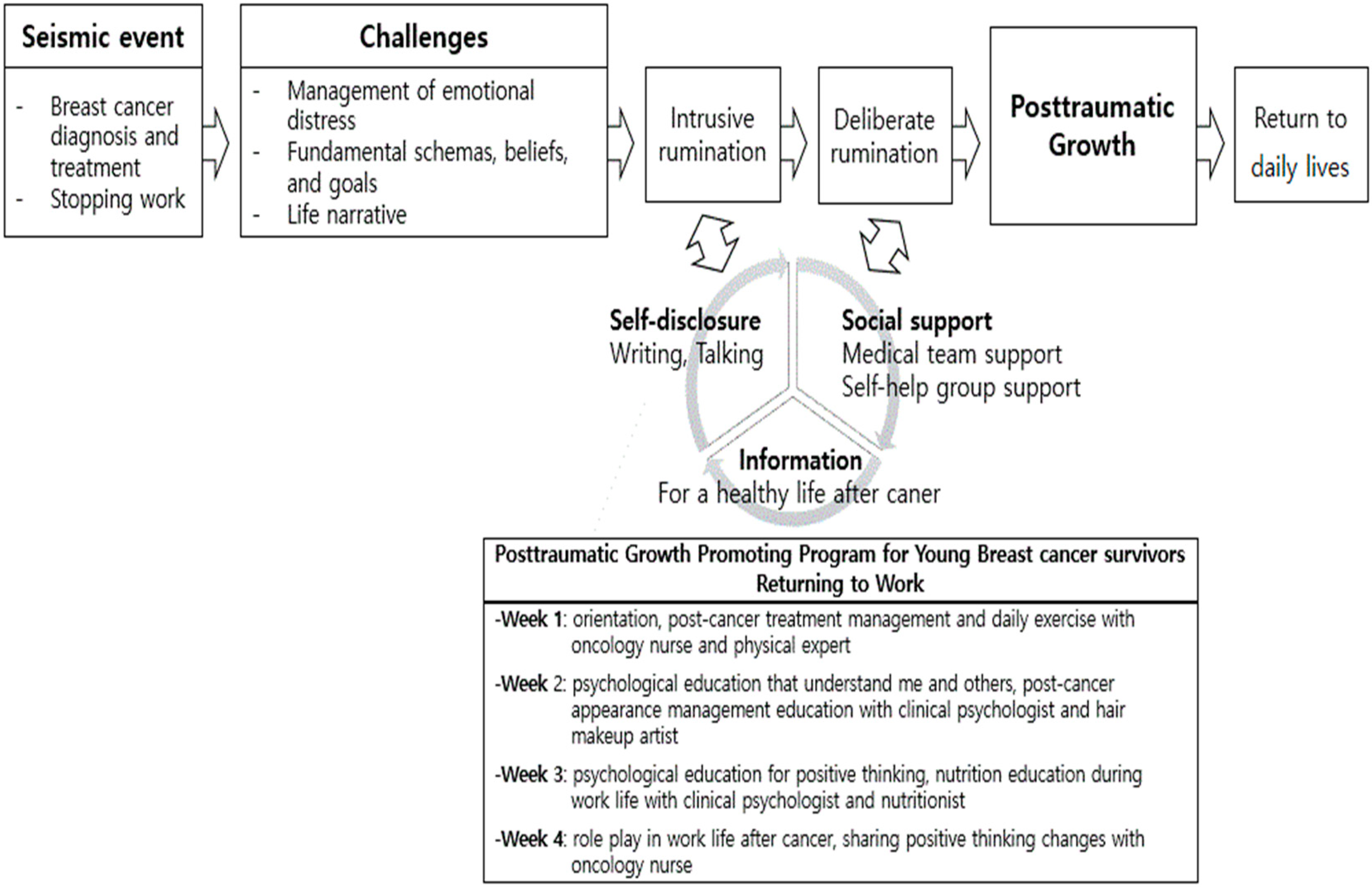
2.2. PTG Promoting Program (JUMP Program)
2.3. Measurements
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kang, M.J.; Won, Y.J.; Lee, J.J.; Jung, K.W.; Kim, H.J.; Kong, H.J.; Im, J.S.; Seo, H.G. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2019. Cancer Res. Treat. 2022, 54, 330–344. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.C.; De Azambuja, E. Improving quality of life after breast cancer: Dealing with symptoms. Maturitas 2011, 70, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Mehnert, A.; Koch, U. Prevalence of acute and post-traumatic stress disorder and comorbid mental disorders in breast cancer patients during primary cancer care: A prospective study. Psychooncology 2007, 16, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Tedeschi, R.G.; Calhoun, L.G. Expert companions: Posttraumatic growth in clinical practice. In Handbook of Posttraumatic Growth: Research and Practice; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2006; pp. 291–310. [Google Scholar]
- Fors, E.; Bertheussen, G.F.; Thune, I.; Juvet, L.K.; Elvsaas, I.K.Ø.; Oldervoll, L.; Anker, G.; Falkmer, U.; Lundgren, S.; Leivseth, G. Psychosocial interventions as part of breast cancer rehabilitation programs? Results from a systematic review. Psycho-Oncology 2011, 20, 909–918. [Google Scholar] [CrossRef]
- Cordova, M.J.; Giese-Davis, J.; Golant, M.; Kronenwetter, C.; Chang, V.; Spiegel, D. Breast cancer as trauma: Posttraumatic stress and posttraumatic growth. J. Clin. Psychol. Med. Settings 2007, 14, 308–319. [Google Scholar] [CrossRef]
- Seo, H.; Park, J.; Kweon, S. Cancer Survivorship; National Cancer Center: IlSan, Republic of Korea, 2013. [Google Scholar]
- Jim, S.L.; Jacobsen, P.B. Posttraumatic Stress and Posttraumatic Growth in Cancer Survivorship: A Review. Cancer J. 2008, 14, 414–419. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J. Trauma Stress 1996, 9, 455–471. [Google Scholar] [CrossRef]
- Liu, J.E.; Wang, H.Y.; Wang, M.L.; Su, Y.L.; Wang, P.L. Posttraumatic growth and psychological distress in Chinese early-stage breast cancer survivors: A longitudinal study. Psycho-Oncology 2014, 23, 437–443. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. Posttraumatic Growth: Conceptual Foundations and Empirical Evidence. Psychol. Inq. 2004, 15, 1–18. [Google Scholar] [CrossRef]
- Danhauer, S.C.; Case, L.D.; Tedeschi, R.; Russell, G.; Vishnevsky, T.; Triplett, K.; Ip, E.H.; Avis, N.E. Predictors of posttraumatic growth in women with breast cancer. Psycho-Oncology 2013, 22, 2676–2683. [Google Scholar] [CrossRef]
- Silva, S.M.; Crespo, C.; Canavarro, M.C. Pathways for psychological adjustment in breast cancer: A longitudinal study on coping strategies and posttraumatic growth. Psychol. Health 2012, 27, 1323–1341. [Google Scholar] [CrossRef]
- Rajandram, R.K.; Jenewein, J.; McGrath, C.P.J.; Zwahlen, R.A. Posttraumatic growth: A novel concept in oral cavity cancer care? Oral Oncol. 2010, 46, 791–794. [Google Scholar] [CrossRef]
- Li, J.; Peng, X.; Su, Y.; He, Y.; Zhang, S.; Hu, X. Effectiveness of psychosocial interventions for posttraumatic growth in patients with cancer: A meta-analysis of randomized controlled trials. Eur. J. Oncol. Nurs. 2020, 48, 101798. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.J. A phenomenological approach to the job-seeking experience of Cancer survivors in low-income. Health Soc. Welf. Rev. 2019, 39, 468–505. [Google Scholar]
- Roepke, A.M. Psychosocial interventions and posttraumatic growth: A meta-analysis. J. Consult. Clin. Psychol. 2015, 83, 129. [Google Scholar] [CrossRef]
- Song, S.; Lee, H.; Park, J.; Kim, K.H. Validity and reliability of the Korean version of the posttraumatic growth inventory. Korean J. Health Psychol. 2009, 14, 193–214. [Google Scholar] [CrossRef]
- Cann, A.; Calhoun, L.G.; Tedeschi, R.G.; Triplett, K.N.; Vishnevsky, T.; Lindstrom, C.M. Assessing posttraumatic cognitive processes: The event related rumination inventory. Anxiety Stress Coping 2011, 24, 137–156. [Google Scholar] [CrossRef]
- Ahn, H.; Joo, H.; Min, J.; Sim, K. Validation of the event related rumination inventory in a Korean population. Cogn. Behavi. Ther. Korea 2013, 13, 149–172. [Google Scholar]
- Oh, S.M.; Min, K.J.; Park, D. A study on the standardization of the hospital anxiety and depression scale for Koreans: A comparison of normal, depressed and anxious groups. Physics 1999, 38, 289–296. [Google Scholar]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Horowitz, M.; Wilner, N.; Alvarez, W. Impact of Event Scale: A measure of subjective stress. Psychosom. Med. 1979, 41, 209–218. [Google Scholar] [CrossRef]
- Eun, H.-J.; Kwon, T.-W.; Lee, S.-M.; Kim, T.-H.; Choi, M.-R.; Cho, S.-J. A study on reliability and validity of the Korean version of impact of event scale-revised. J. Korean Neuropsychiatr. Assoc. 2005, 44, 303–310. [Google Scholar]
- Lo, C.; Hales, S.; Rydall, A.; Panday, T.; Chiu, A.; Malfitano, C.; Jung, J.; Li, M.; Nissim, R.; Zimmermann, C.J.T. Managing Cancer And Living Meaningfully: Study protocol for a randomized controlled trial. Trials 2015, 16, 391. [Google Scholar] [CrossRef] [PubMed]
- Scheffold, K.; Philipp, R.; Engelmann, D.; Schulz-Kindermann, F.; Rosenberger, C.; Oechsle, K.; Härter, M.; Wegscheider, K.; Lordick, F.; Lo, C. Efficacy of a brief manualized intervention Managing Cancer and Living Meaningfully (CALM) adapted to German cancer care settings: Study protocol for a randomized controlled trial. BMC Cancer 2015, 15, 592. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, A.L.; Pakenham, K.I.; Chambers, S.K.; Patrao, T.A.; Courneya, K.S. Effects of a multiple health behavior change intervention for colorectal cancer survivors on psychosocial outcomes and quality of life: A randomized controlled trial. Ann. Behav. Med. 2014, 48, 359–370. [Google Scholar] [CrossRef]
- Köhle, N.; Drossaert, C.H.; Schreurs, K.M.; Hagedoorn, M.; Verdonck-de Leeuw, I.M.; Bohlmeijer, E.T. A web-based self-help intervention for partners of cancer patients based on Acceptance and Commitment Therapy: A protocol of a randomized controlled trial. BMC Public Health 2015, 15, 303. [Google Scholar] [CrossRef]
- Labelle, L.E.; Lawlor-Savage, L.; Campbell, T.S.; Faris, P.; Carlson, L.E. Does self-report mindfulness mediate the effect of Mindfulness-Based Stress Reduction (MBSR) on spirituality and posttraumatic growth in cancer patients? J. Posit. Psychol. 2015, 10, 153–166. [Google Scholar] [CrossRef]
- Zernicke, K.A.; Campbell, T.S.; Speca, M.; McCabe-Ruff, K.; Flowers, S.; Carlson, L.E. A randomized wait-list controlled trial of feasibility and efficacy of an online mindfulness–based cancer recovery program: The etherapy for cancer applying mindfulness trial. Psychosom. Med. 2014, 76, 257–267. [Google Scholar] [CrossRef]
- Wagner, B.; Knaevelsrud, C.; Maercker, A. Post-traumatic growth and optimism as outcomes of an internet-based intervention for complicated grief. Cogn. Behav. Ther. 2007, 36, 156–161. [Google Scholar] [CrossRef]
- Beyer, J. The Effects of Web-Based Interactive Emotional Disclosure on Stress and Health: A Randomized, Controlled Study. Ph.D. Dissertation, Wayne State University, Detroit, MI, USA, 2010. [Google Scholar]
- Bae, K.R.; Kwon, S.Y. The workplace experiences of breast cancer survivors: A survey of an online community. Asian Oncol. Nurs. 2016, 16, 208–216. [Google Scholar] [CrossRef][Green Version]
- Zoellner, T.; Maercker, A. Posttraumatic growth in clinical psychology—A critical review and introduction of a two component model. Clin. Psychol. Rev. 2006, 26, 626–653. [Google Scholar] [CrossRef] [PubMed]
- Hobfoll, S.E.; Palmieri, P.A.; Johnson, R.J.; Canetti-Nisim, D.; Hall, B.J.; Galea, S. Trajectories of resilience, resistance, and distress during ongoing terrorism: The case of Jews and Arabs in Israel. J. Consult. Clin. Psychol. 2009, 77, 138. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n (%) | Mean ± Standard Deviation |
|---|---|---|
| Age (years) | 42.21 ± 4.84 | |
| 30s | 12 (31.6) | |
| 40s | 26 (68.4) | |
| Spouse presence, yes | 30 (78.9) | |
| Religion, yes | 26 (68.4) | |
| Education, ≥university | 36 (94.8) | |
| Monthly household income | ||
| <USD 3000 | 5 (13.2) | |
| ≥USD 3000 | 33 (86.8) | |
| Child existence, yes | 30 (78.9) | |
| Cancer stage | ||
| I | 13 (34.2) | |
| II | 12 (31.6) | |
| III | 12 (31.6) | |
| IV | 1 (2.6) | |
| Time since diagnosis (months) | 13.84 ± 16.27 | |
| <6 | 7 (18.4) | |
| 6–12 | 21 (55.3) | |
| >12 | 10 (26.3) | |
| Operation, yes | 37 (97.4) | |
| Total mastectomy | 15 (39.5) | |
| Breast conserving surgery | 22 (57.9) | |
| Chemotherapy, yes | 29 (76.3) | |
| Radiation therapy, yes | 28 (73.7) | |
| Anti-hormone therapy, yes | 21 (55.3) | |
| Occupation type | ||
| Managers | 5 (13.2) | |
| Professionals and related workers | 11 (28.9) | |
| Clerks | 21 (55.3) | |
| Sales workers | 1 (2.6) | |
| Work period (months) | 127.29 ± 90.15 | |
| Current occupational status | ||
| Continued working | 8 (21.1) | |
| Leave of absence | 26 (68.4) | |
| Stopped working | 4 (10.5) |
| Variables | Pre | Post | One Month Later | Pre/Post p | Pre/One Month Later p |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |||
| Post-traumatic growth | |||||
| Total | 60.66 ± 19.09 | 72.87 ± 16.00 | 72.23 ± 17.96 | <0.001 | <0.001 |
| Relating to others | 19.61 ± 7.08 | 23.58 ± 6.21 | 23.83 ± 6.57 | <0.001 | <0.001 |
| New possibilities | 14.18 ± 4.87 | 17.11 ± 4.08 | 16.91 ± 4.43 | <0.001 | <0.001 |
| Personal strengths | 11.61 ± 4.05 | 14.26 ± 3.37 | 14.00 ± 3.87 | <0.001 | 0.001 |
| Spiritual changes | 4.74 ± 3.02 | 5.95 ± 2.71 | 5.94 ± 3.03 | 0.001 | 0.003 |
| Appreciation of life | 10.53 ± 3.21 | 11.97 ± 2.38 | 11.54 ± 2.59 | 0.001 | 0.001 |
| Rumination | |||||
| Intrusive rumination | 12.03 ± 5.99 | 10.66 ± 5.10 | 11.46 ± 6.77 | 0.107 | 0.936 |
| Deliberate rumination | 18.53 ± 5.23 | 20.24 ± 3.81 | 19.23 ± 5.12 | 0.038 | 0.373 |
| Distress | |||||
| Anxiety | 7.13 ± 3.06 | 6.34 ± 3.15 | 5.74 ± 3.14 | 0.035 | 0.005 |
| Depression | 7.34 ± 3.19 | 6.63 ± 3.30 | 6.86 ± 3.67 | 0.104 | 0.517 |
| Traumatic experience | |||||
| Trauma perception | 42.74 ± 13.49 | 38.95 ± 13.42 | 39.03 ± 17.72 | 0.081 | 0.059 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bae, K.R.; So, W.-Y.; Jang, S. Effects of a Post-Traumatic Growth Program on Young Korean Breast Cancer Survivors. Healthcare 2023, 11, 140. https://doi.org/10.3390/healthcare11010140
Bae KR, So W-Y, Jang S. Effects of a Post-Traumatic Growth Program on Young Korean Breast Cancer Survivors. Healthcare. 2023; 11(1):140. https://doi.org/10.3390/healthcare11010140
Chicago/Turabian StyleBae, Ka Ryeong, Wi-Young So, and Seyong Jang. 2023. "Effects of a Post-Traumatic Growth Program on Young Korean Breast Cancer Survivors" Healthcare 11, no. 1: 140. https://doi.org/10.3390/healthcare11010140
APA StyleBae, K. R., So, W.-Y., & Jang, S. (2023). Effects of a Post-Traumatic Growth Program on Young Korean Breast Cancer Survivors. Healthcare, 11(1), 140. https://doi.org/10.3390/healthcare11010140







