Best Practices on Radiology Department Workflow: Tips from the Impact of the COVID-19 Lockdown on an Italian University Hospital
Abstract
:1. Introduction
2. Methods
2.1. University Hospital “Arcispedale Sant’Anna”
2.2. Data Source and Population
- -
- X-rays examinations, including bedside ones, performed respectively by the ERU and GRU;
- -
- Ultrasound investigations, including bedside ones, performed respectively by the ERU and GRU;
- -
- CT scans conducted respectively by the ERU and GRU;
- -
- MRI scans performed by the GRU.
- -
- trauma;
- -
- accidental or syncopal fall;
- -
- road accident;
- -
- wound (incised wound, laceration, abrasion, penetration wound, avulsion, traumatic amputation);
- -
- crush injury;
- -
- hematoma;
- -
- assault or scuffle;
- -
- distractive injuries and strain;
- -
- violent suicide attempt (hanging);
- -
- excessive physical exertion during work or sporting activity.
2.3. Statistical Analysis
3. Results
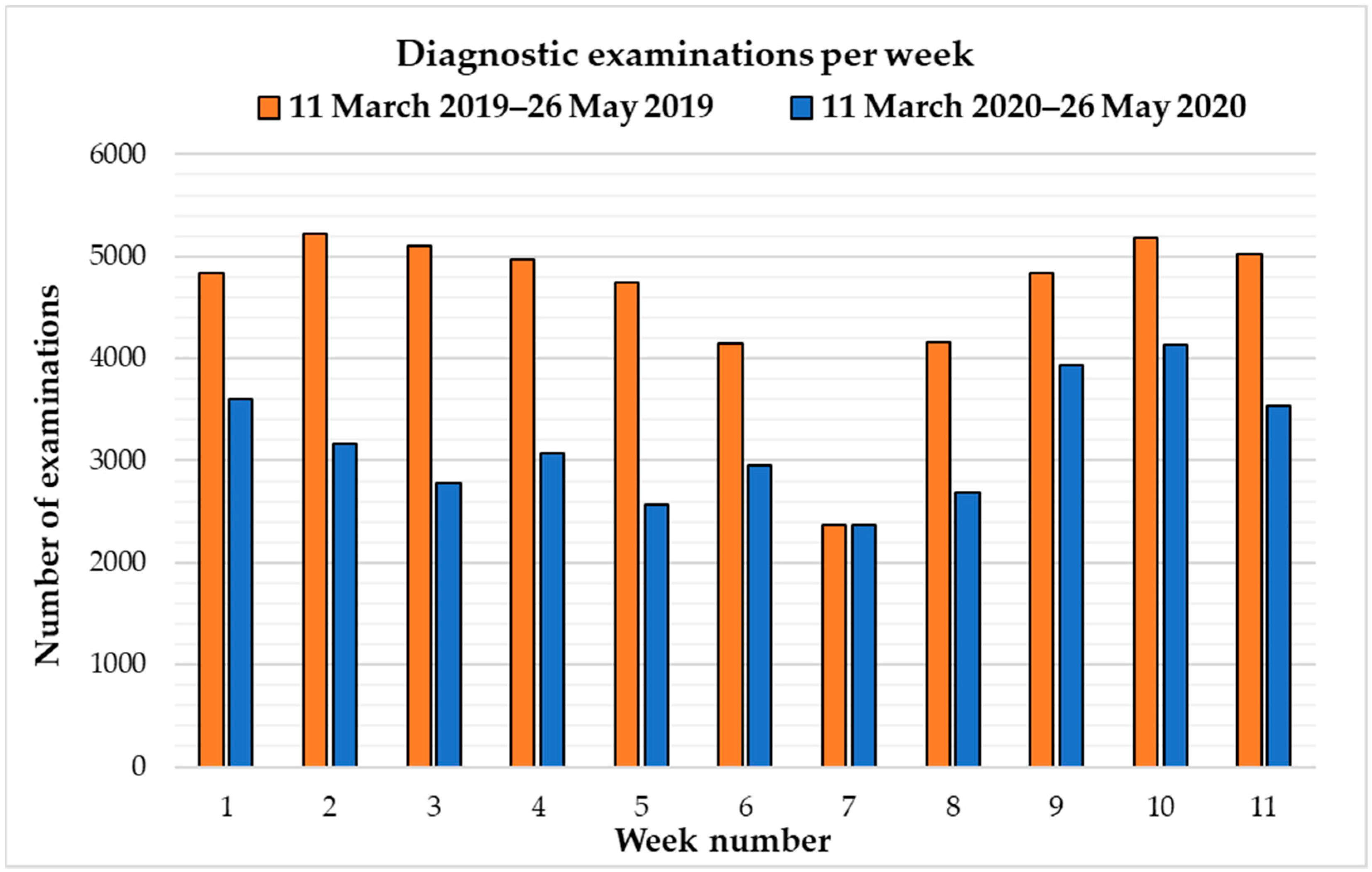
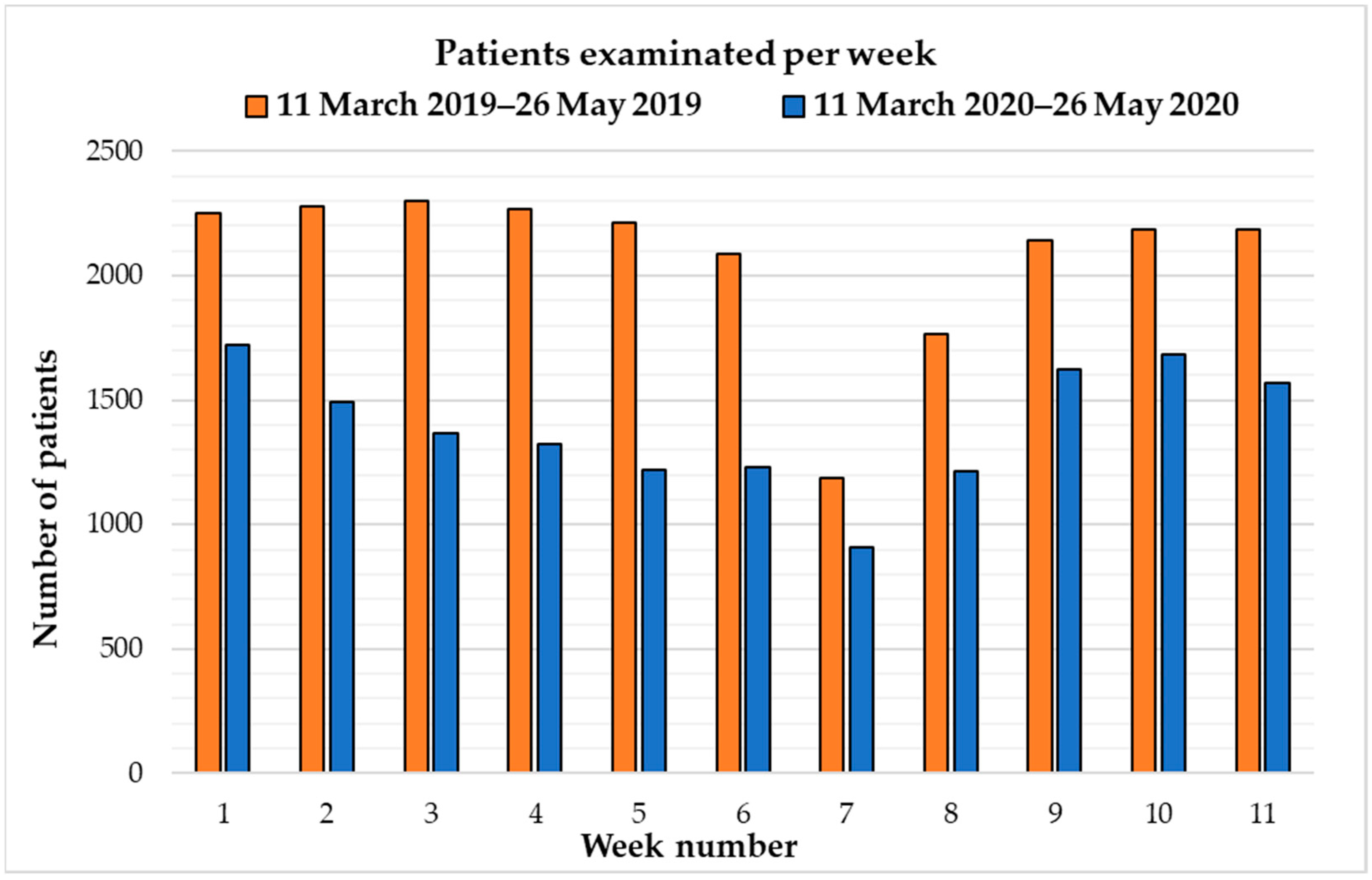
3.1. Variation in the Number of Examinations and Assisted Patients
3.2. Variation in Diagnostic Activity by Patient Type and Method
- -
- 31.2% fewer outpatients (−2264);
- -
- 30.7% fewer inpatients (−1512);
- -
- 38.7% fewer ED patients (−3106).
3.3. Change in Diagnostic Activity Related to Trauma
3.4. Poisson Regression Analysis
4. Discussion
4.1. Immediate Impact of the COVID-19 Lockdown on the Radiology Department Workflow
4.2. Lean Tools for Improving the Radiology Department Workflow
- The significant decrease in the volume of emergency examinations during the global outbreak of coronavirus suggests a temporary downsizing of emergency radiological staff by relocating them to other tasks and to counter the financial strain deriving from COVID-19 patients on other radiology services, particularly those dedicated to the hospitalized patients.
- The increased volume of chest imaging in emergency settings may suggest using radiologists with expertise in thoracic imaging due to their increased sensitivity in detecting subtle pneumonia findings. In addition, specific training programs should be established for generalist radiologists who could also benefit from the support of artificial intelligence to improve the interpretation and efficiency of images, especially during night shifts [42].
- The excessive use of chest CT examinations and the concomitant decrease in conventional chest X-rays found in our data in the first wave of an unknown severe acute respiratory infection is not justified by guidelines regulating the use of imaging in COVID-19 in the subsequent pandemic phases. All major thoracic radiology societies advise against the indiscriminate use of imaging as a screening test for COVID-19 in patients with mild or no symptoms, while recommending its use based on symptom severity, pre-test probability, and COVID-19 testing [29,43,44].
- It is essential to separate the diagnostic pathways between suspected and non-suspected COVID-19 patients to prevent viral transmission between patients and healthcare workers [45]. One CT device should be closest to the COVID-19 emergency room only for infected patients and not too far away from the inpatient unit where patients with suspected or confirmed COVID-19 pneumonia are hospitalized.
- Mobile X-ray units and bedside ultrasounds should be encouraged to avoid the transportation of patients from the ward to the CT unit and to reduce the risk of contamination of staff and other patients. Although chest X-rays had low detection rates in the early stages of COVID-19 infection [27], these methods may be helpful in patient follow-up during treatment and also for detecting complications, such as pleural effusions or pneumothorax in mechanically ventilated subjects [46].
- For overcrowded RDs based on the local prevalence of COVID-19, non-urgent imaging exam appointments should be decreased or scheduled with a longer time gap, and accompanying visitors should be limited to avoid crowding the waiting zones.
- Since radiology is one of the medical specialties with a greater degree of digitalization, teleradiology and teleworking solutions should be strengthened in a similar dramatic scenario. The structured model of outsourced teleradiology has, in fact, been demonstrated to meet the requirements of emergency medicine during the pandemic with high diagnostic accuracy of chest CTs in the diagnosis of COVID-19 and a remarkable inter-observer agreement between teleradiologists with various degrees of experience and in contexts with different levels of disease prevalence [47]. By holding a small group of radiologists on-site and the rest of the group working safely from home to minimize the risk of cross-infection, teleradiology allows for the preservation of workload in the RD, increasing the productivity in other areas, such as administrative, operations, education, and research units, or updating strategies for optimizing workflow and safety protocols [48].
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 11 July 2020).
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Protezione Civile COVID-19 ITALIA—Desktop. Available online: https://opendatadpc.maps.arcgis.com/apps/dashboards/b0c68bce2cce478eaac82fe38d4138b1 (accessed on 11 July 2020).
- Il Sole 24 Ore Coronavirus in Italia, i Dati e la Mappa. Available online: https://lab24.ilsole24ore.com/coronavirus/?refresh_ce=1 (accessed on 13 July 2020).
- Guaitoli, G.; Pancrazi, R. Covid-19: Regional policies and local infection risk: Evidence from Italy with a modelling study. Lancet Reg. Health Eur. 2021, 8, 100169. [Google Scholar] [CrossRef] [PubMed]
- Presidenza Consiglio dei Ministri Coronavirus, Conte Firma il Dpcm 11 Marzo 2020. Available online: www.governo.it (accessed on 13 July 2020).
- Horowitz, J. Italy’s Health Care System Groans Under Coronavirus—A Warning to the World. The New York Times, 12 March 2020. Available online: https://www.nytimes.com/2020/03/12/world/europe/12italy-coronavirus-health-care.html(accessed on 13 July 2020).
- Franchini, S.; Spessot, M.; Landoni, G.; Piani, C.; Cappelletti, C.; Mariani, F.; Mauri, S.; Taglietti, M.V.; Fortunato, M.; Furlan, F.; et al. Stranger months: How SARS-CoV-2, fear of contagion, and lockdown measures impacted attendance and clinical activity during February and March 2020 at an urban Emergency Department in Milan. Disaster Med. Public Health Prep. 2020, 15, e33–e42. [Google Scholar] [CrossRef] [PubMed]
- Bersano, A.; Kraemer, M.; Touzé, E.; Weber, R.; Alamowitch, S.; Sibon, I.; Pantoni, L. Stroke care during the COVID-19 pandemic: Experience from three large European countries. Eur. J. Neurol. 2020, 27, 1794–1800. [Google Scholar] [CrossRef]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Morelli, N.; Rota, E.; Terracciano, C.; Immovilli, P.; Spallazzi, M.; Colombi, D.; Zaino, D.; Michieletti, E.; Guidetti, D. The Baffling Case of Ischemic Stroke Disappearance from the Casualty Department in the COVID-19 Era. Eur. Neurol. 2020, 83, 213–215. [Google Scholar] [CrossRef]
- Hirschfeld, C.B.; Shaw, L.J.; Williams, M.C.; Lahey, R.; Villines, T.C.; Dorbala, S.; Choi, A.D.; Shah, N.R.; Bluemke, D.; Berman, D.S.; et al. Impact of COVID-19 on Cardiovascular Testing in the United States Versus the Rest of the World. Cardiovasc. Imaging 2021, 14, 1787–1799. [Google Scholar] [CrossRef]
- Denys, A.; Guiu, B.; Chevallier, P.; Digklia, A.; de Kerviler, E.; de Baere, T. Interventional oncology at the time of COVID-19 pandemic: Problems and solutions. Diagn. Interv. Imaging 2020, 101, 347–353. [Google Scholar] [CrossRef]
- Bellan, M.; Gavelli, F.; Hayden, E.; Patrucco, F.; Soddu, D.; Pedrinelli, A.R.; Cittone, M.G.; Rizzi, E.; Casciaro, G.F.; Vassia, V.; et al. Pattern of Emergency Department referral during the COVID-19 outbreak in Italy. Panminerva Med. 2021, 63, 478–481. [Google Scholar] [CrossRef]
- Ierardi, A.M.; Carnevale, A.; Giganti, M.; Carrafiello, G. The Interventional Radiology Service During the COVID-19 Pandemic: Steps to Managing the Risk of Infection. J. Endovasc. Resusc. Trauma Manag. 2020, 4, 69–73. [Google Scholar] [CrossRef]
- Lapolla, P.; Mingoli, A.; Lee, R. Deaths from COVID-19 in healthcare workers in Italy-What can we learn? Infect. Control Hosp. Epidemiol. 2020, 42, 364–365. [Google Scholar] [CrossRef]
- Bollettino Sorveglianza Integrata COVID-19—18 Agosto 2020. Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_18-agosto-2020.pdf (accessed on 15 July 2020).
- Iacobellis, F.; Abu-Omar, A.; Crivelli, P.; Galluzzo, M.; Danzi, R.; Trinci, M.; Orabona, G.D.; Conti, M.; Romano, L.; Scaglione, M. Current Standards for and Clinical Impact of Emergency Radiology in Major Trauma. Int. J. Environ. Res. Public Health 2022, 19, 539. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; Goretti, G.; Giordano, M.; Voza, A. Lean-ing Method in an Emergency Department of the Italian Epicenter of the COVID-19 Outbreak: When the Algorithm Makes Difference. Appl. Syst. Innov. 2021, 4, 55. [Google Scholar] [CrossRef]
- JASP Team. JASP; Version 0.16.3; JASP Team: Amsterdam, The Netherlands, 2022. [Google Scholar]
- Alquézar-Arbé, A.; Piñera, P.; Jacob, J.; Martín, A.; Jiménez, S.; Llorens, P.; Martín-Sánchez, F.J.; Burillo-Putze, G.; García-Lamberechts, E.J.; González Del Castillo, J.; et al. Impact of the COVID-19 pandemic on hospital emergency departments: Results of a survey of departments in 2020—The Spanish ENCOVUR study. Emergencias 2020, 32, 320–331. [Google Scholar]
- Nuñez, J.H.; Sallent, A.; Lakhani, K.; Guerra-Farfan, E.; Vidal, N.; Ekhtiari, S.; Minguell, J. Impact of the COVID-19 Pandemic on an Emergency Traumatology Service: Experience at a Tertiary Trauma Centre in Spain. Injury 2020, 51, 1414. [Google Scholar] [CrossRef] [PubMed]
- Houshyar, R.; Tran-Harding, K.; Glavis-Bloom, J.; Nguyentat, M.; Mongan, J.; Chahine, C.; Loehfelm, T.W.; Kohli, M.D.; Zaragoza, E.J.; Murphy, P.M.; et al. Effect of shelter-in-place on emergency department radiology volumes during the COVID-19 pandemic. Emerg. Radiol. 2020, 27, 781. [Google Scholar] [CrossRef]
- Cavallo, J.J.; Forman, H.P. The Economic Impact of the COVID-19 Pandemic on Radiology Practices. Radiology 2020, 296, E141–E144. [Google Scholar] [CrossRef]
- Link, E.; Baumann, E.; Czerwinski, F.; Rosset, M.; Suhr, R. Of seekers and nonseekers: Characteristics of Covid-19-related information-seeking behaviors. World Med. Health Policy 2022, 14, 276–294. [Google Scholar] [CrossRef]
- Li, J.; Long, X.; Wang, X.; Fang, F.; Lv, X.; Zhang, D.; Sun, Y.; Hu, S.; Lin, Z.; Xiong, N. Radiology indispensable for tracking COVID-19. Diagn. Interv. Imaging 2021, 102, 69. [Google Scholar] [CrossRef]
- Fang, Y.; Zhang, H.; Xie, J.; Lin, M.; Ying, L.; Pang, P.; Ji, W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology 2020, 296, E115–E117. [Google Scholar] [CrossRef]
- Rubin, G.D.; Ryerson, C.J.; Haramati, L.B.; Sverzellati, N.; Kanne, J.P.; Raoof, S.; Schluger, N.W.; Volpi, A.; Yim, J.J.; Martin, I.B.K.; et al. The role of chest imaging in patient management during the covid-19 pandemic: A multinational consensus statement from the fleischner society. Radiology 2020, 296, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Gil-Rodrigo, A.; Miró, Ò.; Piñera, P.; Burillo-Putze, G.; Jiménez, S.; Martín, A.; Martín-Sánchez, F.J.; Jacob, J.; Guardiola, J.M.; García-Lamberechts, E.J.; et al. En representación de la red de investigación S. Analysis of clinical characteristics and outcomes in patients with COVID-19 based on a series of 1000 patients treated in Spanish emergency departments. Emergencias 2020, 32, 233–241. [Google Scholar] [PubMed]
- Coppola, F.; Faggioni, L.; Neri, E.; Grassi, R.; Miele, V. Impact of the COVID-19 outbreak on the profession and psychological wellbeing of radiologists: A nationwide online survey. Insights Imaging 2021, 12, 23. [Google Scholar] [CrossRef]
- Antonini, M.; Hinwood, M.; Paolucci, F.; Balogh, Z.J. The Epidemiology of Major Trauma During the First Wave of COVID-19 Movement Restriction Policies: A Systematic Review and Meta-analysis of Observational Studies. World J. Surg. 2022, 46, 2045–2060. [Google Scholar] [CrossRef]
- Lim, M.Q.; Saffari, S.E.; Fu, A.; Ho, W.; Nathaniel, J.; Liew, M.H.; Kiat, B.; Tan, K.; Sim, N.S.; Shen, Y.; et al. A Descriptive Analysis of the Impact of COVID-19 on Emergency Department Attendance and Visit Characteristics in Singapore. COVID 2021, 1, 739–750. [Google Scholar] [CrossRef]
- Thornton, J. Covid-19: A & E visits in England fall by 25% in week after lockdown. BMJ 2020, 369, m1401. [Google Scholar] [CrossRef]
- Jeffery, M.M.; D’Onofrio, G.; Paek, H.; Platts-Mills, T.F.; Soares, W.E.; Hoppe, J.A.; Genes, N.; Nath, B.; Melnick, E.R. Trends in Emergency Department Visits and Hospital Admissions in Health Care Systems in 5 States in the First Months of the COVID-19 Pandemic in the US. JAMA Intern. Med. 2020, 180, 1328–1333. [Google Scholar] [CrossRef]
- Bottari, G.; Stellacci, G.; Ferorelli, D.; Dell’erba, A.; Aricò, M.; Benevento, M.; Palladino, G.; Solarino, B. Imaging Appropriateness in Pediatric Radiology during COVID-19 Pandemic: A Retrospective Comparison with No COVID-19 Period. Children 2021, 8, 463. [Google Scholar] [CrossRef]
- Kuo, L.W.; Fu, C.Y.; Liao, C.A.; Liao, C.H.; Wu, Y.T.; Huang, J.F.; Hsieh, C.H.; Cheng, C.T. How much could a low COVID-19 pandemic change the injury trends? A single-institute, retrospective cohort study. BMJ Open 2021, 11, e046405. [Google Scholar] [CrossRef]
- Christey, G.; Amey, J.; Singh, N.; Denize, B.; Campbell, A. Admission to hospital for injury during COVID-19 alert level restrictions. N. Z. Med. J. 2021, 134, 50–58. [Google Scholar] [PubMed]
- Zsilavecz, A.; Wain, H.; Bruce, J.L.; Smith, M.T.D.; Bekker, W.; Laing, G.L.; Lutge, E.; Clarke, D.L. Trauma patterns during the COVID-19 lockdown in South Africa expose vulnerability of women. S. Afr. Med. J. 2020, 110, 1105–1109. [Google Scholar] [CrossRef] [PubMed]
- Choi, A.; Bae, W.; Kim, K.; Kim, S. Impact of Covid-19 on the Visit of Pediatric Patients with Injuries to the Emergency Department in Korea. Children 2021, 8, 568. [Google Scholar] [CrossRef]
- Kiss, P.; Carcel, C.; Hockham, C.; Peters, S.A.E. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: A systematic review. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 18–27. [Google Scholar] [CrossRef]
- Li, L.; Qin, L.; Xu, Z.; Yin, Y.; Wang, X.; Kong, B.; Bai, J.; Lu, Y.; Fang, Z.; Song, Q.; et al. Using Artificial Intelligence to Detect COVID-19 and Community-acquired Pneumonia Based on Pulmonary CT: Evaluation of the Diagnostic Accuracy. Radiology 2020, 296, E65–E71. [Google Scholar] [CrossRef] [PubMed]
- Revel, M.P.; Parkar, A.P.; Prosch, H.; Silva, M.; Sverzellati, N.; Gleeson, F.; Brady, A. COVID-19 patients and the radiology department—Advice from the European Society of Radiology (ESR) and the European Society of Thoracic Imaging (ESTI). Eur. Radiol. 2020, 30, 4903–4909. [Google Scholar] [CrossRef]
- Neri, E.; Miele, V.; Coppola, F.; Grassi, R. Use of CT and artificial intelligence in suspected or COVID-19 positive patients: Statement of the Italian Society of Medical and Interventional Radiology. Radiol. Med. 2020, 125, 505–508. [Google Scholar] [CrossRef]
- Kato, S.; Ishiwata, Y.; Aoki, R.; Iwasawa, T.; Hagiwara, E.; Ogura, T.; Utsunomiya, D. Imaging of COVID-19: An update of current evidences. Diagn. Interv. Imaging 2021, 102, 493–500. [Google Scholar] [CrossRef]
- Blažić, I.; Brkljačić, B.; Frija, G. The use of imaging in COVID-19-results of a global survey by the International Society of Radiology. Eur. Radiol. 2021, 31, 1185–1193. [Google Scholar] [CrossRef]
- Nivet, H.; Crombé, A.; Schuster, P.; Ayoub, T.; Pourriol, L.; Favard, N.; Chazot, A.; Alonzo-Lacroix, F.; Youssof, E.; Ben Cheikh, A.; et al. The accuracy of teleradiologists in diagnosing COVID-19 based on a French multicentric emergency cohort. Eur. Radiol. 2021, 31, 2833. [Google Scholar] [CrossRef]
- Martín-Noguerol, T.; Lopez-Ortega, R.; Ros, P.R.; Luna, A. Teleworking beyond teleradiology: Managing radiology departments during the COVID-19 outbreak. Eur. Radiol. 2021, 31, 601–604. [Google Scholar] [CrossRef] [PubMed]
| 11 March 2019–26 May 2019 | 11 March 2020–26 May 2020 | Comparison | ||||
|---|---|---|---|---|---|---|
| Unit | Number of Patients | Proportion | Number of Patients | Proportion | Difference | Percentage |
| GRU | 10,866 | 55% | 8070 | 60.6% | −2796 | −25.7% |
| ERU | 8905 | 45% | 5252 | 39.4% | −3653 | −41% |
| Total | 19,771 | - | 13,322 | - | −6449 | −32.6% |
| Unit | Number of Examinations | Proportion | Number of Examinations | Proportion | Difference | Percentage |
| GRU | 31,203 | 61.7% | 23,260 | 66.8% | −7943 | −25.5% |
| ERU | 19,396 | 38.3% | 11,552 | 33.2% | 41 | −40.4% |
| Total | 50,599 | - | 34,812 | - | −15,787 | −31.2% |
| 11 March 2019–26 May 2019 | 11 March 2020–26 May 2020 | Comparison | ||
|---|---|---|---|---|
| Week Number | Number of Examinations | Number of Examinations | Difference | Percentage |
| Week 1 (11/03–17/03) | 4841 | 3601 | −1240 | −25.6% |
| Week 2 (18/03–24/03) | 5221 | 3171 | −2050 | −39.3% |
| Week 3 (25/03–31/03) | 5109 | 2783 | −2326 | −45.5% |
| Week 4 (01/04–07/04) | 4972 | 3070 | −1902 | −38.3% |
| Week 5 (08/04–14/04) | 4750 | 2569 | −2181 | −45.9% |
| Week 6 (15/04–21/04) | 4145 | 2957 | −1188 | −28.7% |
| Week 7 (22/04–28/04) | 2364 | 2364 | 0 | - |
| Week 8 (29/04–05/05) | 4155 | 2687 | −1468 | −35.3% |
| Week 9 (06/05–12/05) | 4840 | 3940 | −900 | −18.6% |
| Week 10 (13/05–19/05) | 5181 | 4137 | −1044 | −20.2% |
| Week 11 (20/05–26/05) | 5021 | 3533 | −1488 | −29.6% |
| Total | 50,599 | 34,812 | −15,787 | −31.2% |
| 11 March 2019–26 May 2019 | 11 March 2020–26 May 2020 | Comparison | ||
|---|---|---|---|---|
| Week Number | Number of Patients | Number of Patients | Difference | Percentage |
| Week 1 (11/03–17/03) | 2250 | 1721 | −529 | −23.5% |
| Week 2 (18/03–24/03) | 2278 | 1492 | −786 | −34.5% |
| Week 3 (25/03–31/03) | 2302 | 1366 | −936 | −40.7% |
| Week 4 (01/04–07/04) | 2267 | 1321 | −946 | −41.7% |
| Week 5 (08/04–14/04) | 2214 | 1221 | −993 | −44.9% |
| Week 6 (15/04–21/04) | 2085 | 1230 | −855 | −41% |
| Week 7 (22/04–28/04) | 1187 | 908 | −279 | −23.5% |
| Week 8 (29/04–05/05) | 1765 | 1213 | −552 | −31.3% |
| Week 9 (06/05–12/05) | 2140 | 1626 | −514 | −24% |
| Week 10 (13/05–19/05) | 2187 | 1683 | −504 | −23% |
| Week 11 (20/05–26/05) | 2187 | 1567 | −620 | −28.3% |
| Total | 22,862 | 15,348 | −7514 | −32.9% |
| 11 March 2019–26 May 2019 | 11 March 2020–26 May 2020 | Comparison | |||||
|---|---|---|---|---|---|---|---|
| Examinations by Patient Type | Number of Patients | Proportion | Number of Patients | Proportion | Difference | Percentage | p Value |
| Outpatient | 7249 | 35.9% | 4985 | 37.4% | −2264 | −31.2% | 0.004 |
| Inpatient | 4918 | 24.3% | 3406 | 25.6% | −1512 | −30.7% | 0.012 |
| ED patient | 8035 | 39.8% | 4929 | 37% | −3106 | −38.7% | <0.001 |
| Total | 20,202 | - | 13,320 | - | −6882 | −34.1% | - |
| Examinations by Patient Type | Number of Examinations | Proportion | Number of Examinations | Proportion | Difference | Percentage | p Value |
| Outpatient | 15,179 | 30% | 10,253 | 29.5% | −4926 | −32.5% | >0.05 |
| Inpatient | 19,793 | 39.1% | 14,393 | 41.3% | −5400 | −27.3% | <0.001 |
| ED patient | 15,627 | 30.9% | 10,166 | 29.2% | −5461 | −34.9% | <0.001 |
| Total | 50,599 | - | 34,812 | - | −15,787 | −31.2% | - |
| 11 March 2019–26 May 2019 | 11 March 2020–26 May 2020 | Comparison | ||||
|---|---|---|---|---|---|---|
| Examinations by Clinical Question | Number of Examinations | Proportion | Number of Examinations | Proportion | Difference | Percentage |
| Not trauma | 43,008 | 85.2% | 30,372 | 87.5% | −12,636 | −29.4% |
| Trauma | 7470 | 14.8% | 4348 | 12.5% | −3122 | −41.8% |
| Not determined | 121 | - | 92 | - | - | - |
| Total | 50,478 | - | 34,720 | - | −15,758 | −31.2% |
| 11 March 2019–26 May 2019 | 11 March 2020–26 May 2020 | Comparison | ||||
|---|---|---|---|---|---|---|
| Patients by Clinical Condition | Number of Patients | Proportion | Number of Patients | Proportion | Difference | Percentage |
| Not trauma | 15,316 | 83.4% | 10,486 | 87.5% | −4830 | −31.5% |
| Trauma | 3038 | 16.6% | 1495 | 12.5% | −1543 | −50.8% |
| Not determined | 52 | - | 49 | - | - | |
| Total | 18,354 | - | 11,981 | - | −6373 | −34.7% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pellegrino, F.; Carnevale, A.; Bisi, R.; Cavedagna, D.; Reverberi, R.; Uccelli, L.; Leprotti, S.; Giganti, M. Best Practices on Radiology Department Workflow: Tips from the Impact of the COVID-19 Lockdown on an Italian University Hospital. Healthcare 2022, 10, 1771. https://doi.org/10.3390/healthcare10091771
Pellegrino F, Carnevale A, Bisi R, Cavedagna D, Reverberi R, Uccelli L, Leprotti S, Giganti M. Best Practices on Radiology Department Workflow: Tips from the Impact of the COVID-19 Lockdown on an Italian University Hospital. Healthcare. 2022; 10(9):1771. https://doi.org/10.3390/healthcare10091771
Chicago/Turabian StylePellegrino, Fabio, Aldo Carnevale, Riccardo Bisi, Davide Cavedagna, Roberto Reverberi, Licia Uccelli, Stefano Leprotti, and Melchiore Giganti. 2022. "Best Practices on Radiology Department Workflow: Tips from the Impact of the COVID-19 Lockdown on an Italian University Hospital" Healthcare 10, no. 9: 1771. https://doi.org/10.3390/healthcare10091771
APA StylePellegrino, F., Carnevale, A., Bisi, R., Cavedagna, D., Reverberi, R., Uccelli, L., Leprotti, S., & Giganti, M. (2022). Best Practices on Radiology Department Workflow: Tips from the Impact of the COVID-19 Lockdown on an Italian University Hospital. Healthcare, 10(9), 1771. https://doi.org/10.3390/healthcare10091771










