Impact of COVID-19 on Patients’ Attitudes and Perceptions of Dental Health Services: A Questionnaire Based Study in an Australian University Dental Clinic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Participants and Data Collection
2.2. Instrument
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Questionnaire Items
| Demographics | |
| 1 | What is your current age? |
| 2 | What gender do you identify as? |
| 3 | Do you identify as Aboriginal and/or Torres Strait Islander? |
| 4 | Do you have a health care card/concession card? |
| 5 | What is your highest level of education attained? |
| 6 | What is your annual income before tax? |
| 7 | What is your current employment status? |
| 8 | How long have you been attending JCU Dental Clinic? |
| Perceptions | |
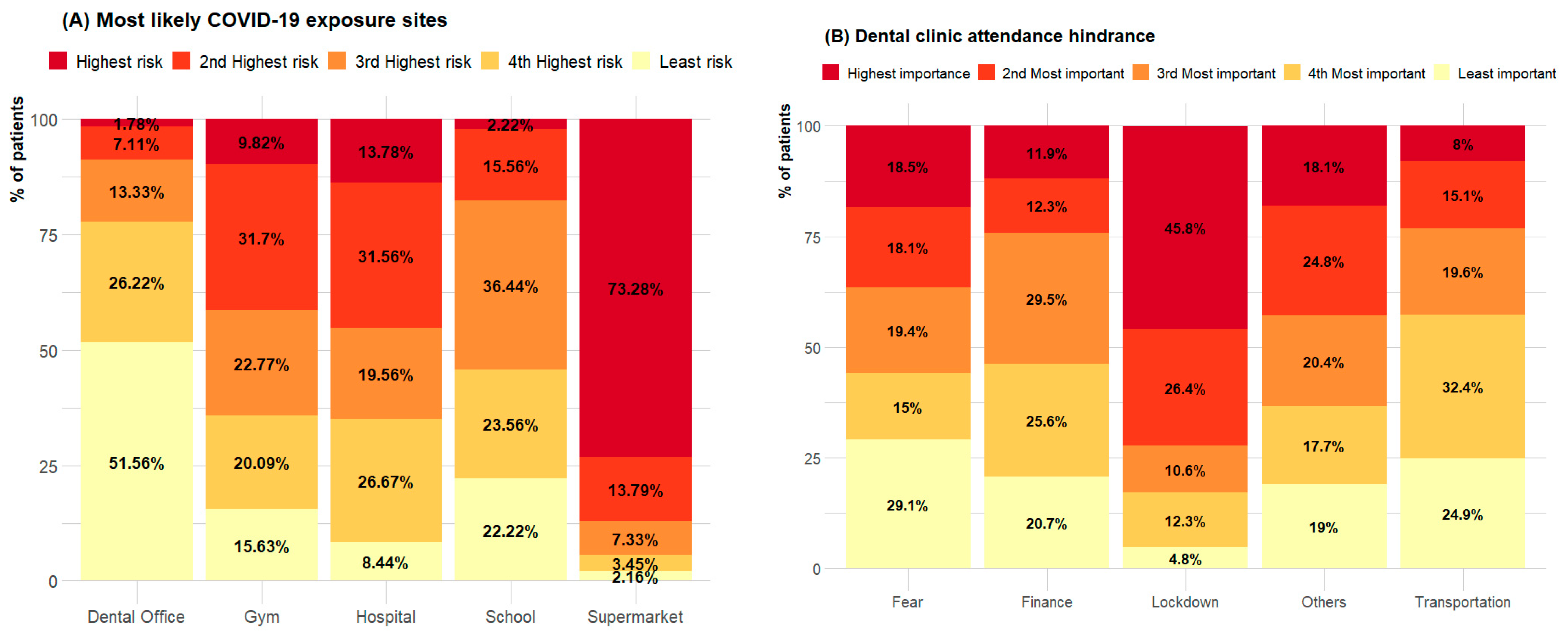
| 9 | Which of the following locations do you feel you are most likely to be exposed to COVID-19? (please number from 1 to 5, 1 being the highest risk of exposure and 5 being the lowest risk). |
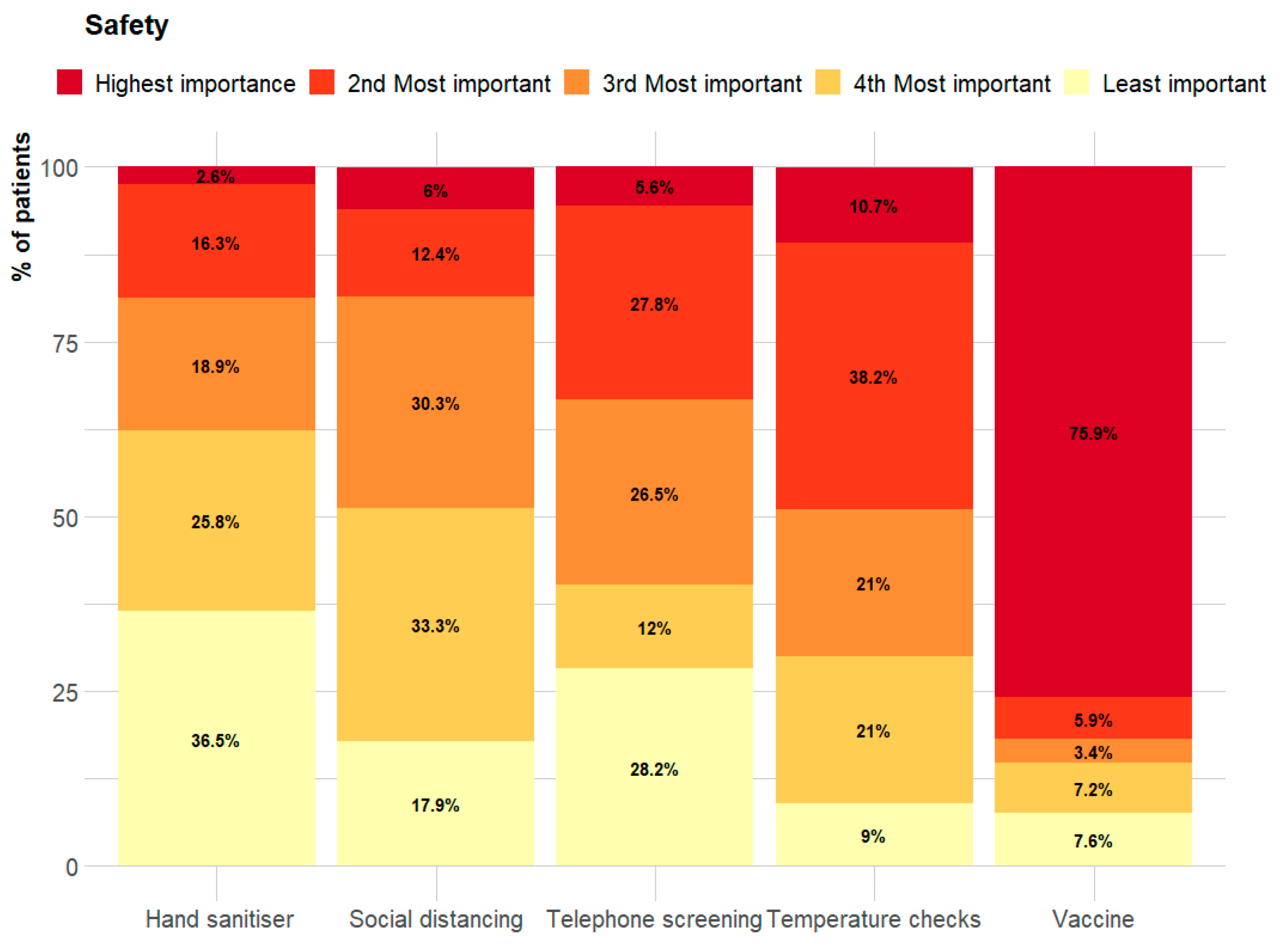
| 10 | What would increase your feeling of safety when coming to the dental clinic? Please number from 1 to 5 in order of importance, with 1 being the most important and 5 being the least important. |
| 11 | How do you think the COVID-19 pandemic has impacted your dental health. |
| 12 | JCU Dentals response to COVID-19 included closure of the dental clinic in March 2020. |
| 13 | COVID-19 protocols implemented by JCU Dental included social distancing, mandatory patient handwashing and patient mouthwash performed prior to treatment. |
| 14 | Closing down the JCU Dental in the March 2020 COVID-19 outbreak was appropriate. |
| 15 | If you have attended a dental clinic in the past 12 months, have the clinic’s COVID-19 protocols impacted fears around safety? |
| Access | |
| 16 | Are you attending JCU Dental because you couldn’t attend your regular dentist? |
| 17 | COVID-19 pandemic has impacted my ability to travel when attending JCU Dental. |
| 18 | Since JCU Dental has re-opened after the COVID-19 pandemic, booking an appointment has been ______. |
| 19 | Did you have an appointment cancelled due to the COVID-19 closure? |
| 20 | What was the purpose of the cancelled appointment? |
| 21 | Did you have to attend another dental clinic because JCU Dental was closed due to COVID-19? |
| 22 | Were you notified of JCU Dental Clinic’s closure due to COVID-19? |
| 23 | Were you notified when JCU Dental Clinic planned to re-open? |
| 24 | Has COVID-19 caused you any financial hardship? |
| 25 | If you answered “yes” to the above, has this financial hardship impacted your ability to afford dental treatment? |
| Attitude | |
| 26 | When attending JCU Dental, which of the following impacts your likeliness to attend the clinic? Rank in order from 1 to 5, with 1 being the most important reason to not attend and 5 being the least important reason. |
| 27 | Has COVID-19 impacted your likeliness to attend the dental clinic |
| 28 | Would you have scheduled an appointment if you had a dental emergency after the COVID-19 restrictions were put in place? |
| 29 | Are you likely to attend JCU Dental if we had a new outbreak of Cairns? |
| 30 | Does the large number of patients attending the JCU Dental Clinic influence your attendance? |
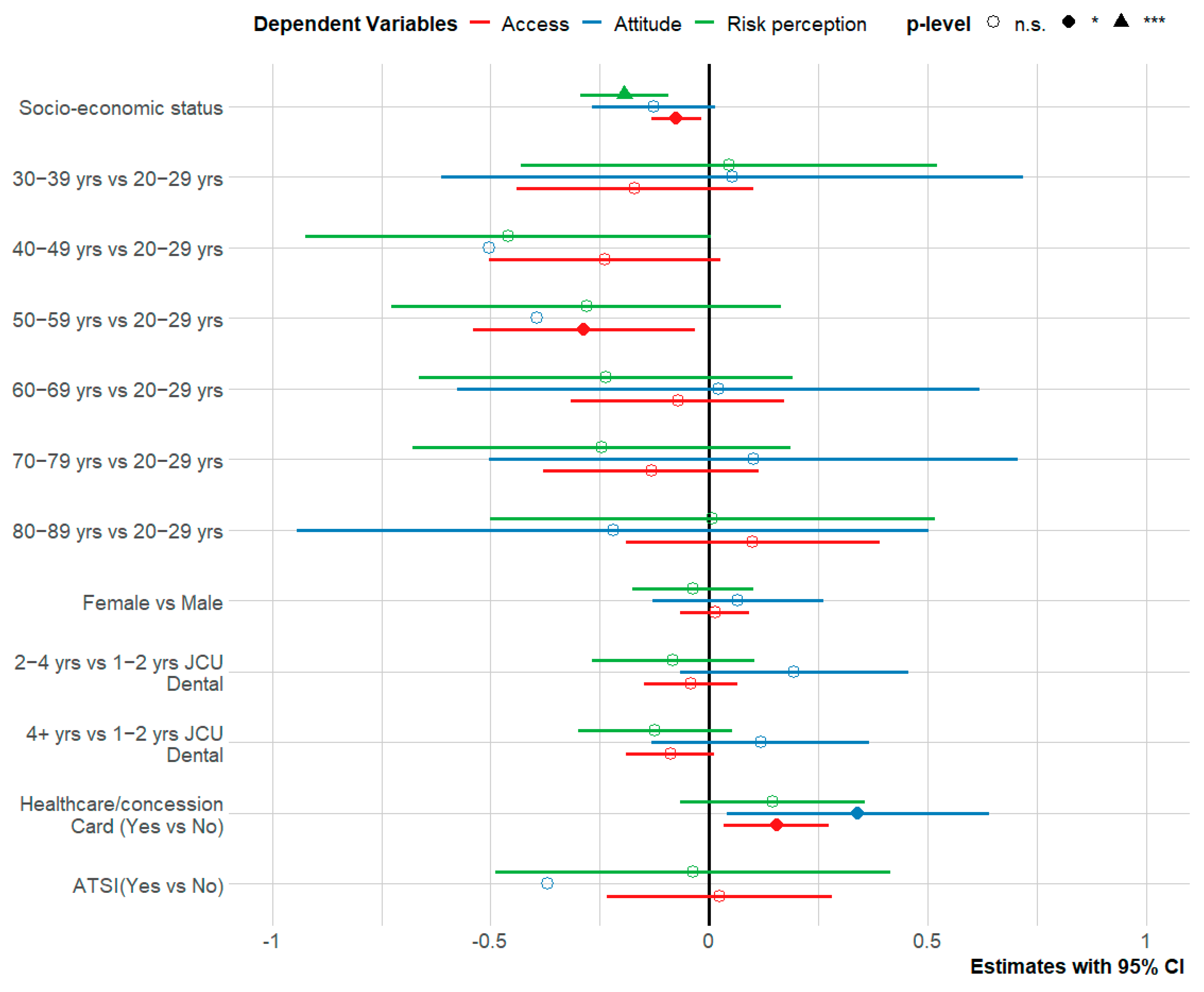
Appendix B. Differences in Risk Perception, Attitude and Access Based on Demographic Levels
| Variables | Risk Perception | Attitude | Access | ||||||
| Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Gender | 0.75 | 0.48 | 0.96 | ||||||
| Male | 2.20 | 0.57 | 2.70 | 0.85 | 1.81 | 0.35 | |||
| Female | 2.18 | 0.59 | 2.62 | 0.84 | 1.81 | 0.34 | |||
| Age | 0.11 | 0.13 | 0.14 | ||||||
| 20–29 | 2.34 | 0.18 | 2.77 | 0.66 | 1.89 | 0.28 | |||
| 30–39 | 2.35 | 0.54 | 2.64 | 0.96 | 1.74 | 0.29 | |||
| 40–49 | 1.80 | 0.52 | 3.29 | 1.06 | 1.63 | 0.4 | |||
| 50–59 | 1.96 | 0.56 | 3.24 | 0.92 | 1.56 | 0.34 | |||
| 60–69 | 2.20 | 0.6 | 2.53 | 0.69 | 1.99 | 0.29 | |||
| 70–79 | 2.27 | 0.55 | 2.34 | 0.65 | 1.87 | 0.29 | |||
| 80–89 | 2.52 | 0.69 | 2.69 | 0.75 | 2.09 | 0.49 | |||
| Years at JCU Dental | 0.939 | 0.02 | 0.686 | ||||||
| 1–2 Years | 2.17 | 0.84 | 2.96 | 1.07 | 1.79 | 0.49 | |||
| 2–4 Years | 2.19 | 0.44 | 2.52 | 0.70 | 1.83 | 0.25 | |||
| 4+ Years | 2.19 | 0.47 | 2.56 | 0.71 | 1.82 | 0.29 | |||
| Health Care or Concession Card | <0.001 | <0.001 | <0.001 | ||||||
| Yes | 2.29 | 0.57 | 2.48 | 0.69 | 1.89 | 0.29 | |||
| No | 1.88 | 0.55 | 3.26 | 1.04 | 1.57 | 0.39 | |||
| Aboriginal or Torres Strait Islander | 0.141 | 0.448 | 0.77 | ||||||
| Yes | 2.27 | 0.76 | 3.03 | 0.77 | 1.85 | 0.33 | |||
| No | 2.17 | 0.58 | 2.65 | 0.85 | 1.81 | 0.35 | |||
References
- Meng, L.; Hua, F.; Bian, Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J. Dent. Res. 2020, 99, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Shang, Y.; Yao, S.; Liu, R.; Liu, H. Perioperative care provider’s considerations in managing patients with the COVID-19 infections. Transl. Perioper. Pain Med. 2020, 7, 216–224. [Google Scholar]
- Thomas, M. Dental Board of Australia—COVID-19 Update: Now Moving to Level 1 Restrictions Dental Board Ahpra: Ahpra. Available online: https://www.dentalboard.gov.au/News/2020-05-08-COVID19-update-to-dental-practitioners-8-May.aspx (accessed on 23 July 2022).
- Imai, H.; Furukawa, T.A. The risk perception against COVID-19 and outpatients’ anxiety of visiting the clinic during COVID-19 pandemic. Psychiatry Clin. Neurosci. 2021, 75, 208. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.L.; Jensen, J.D.; Scherr, C.L.; Brown, N.R.; Christy, K.; Weaver, J. The Health Belief Model as an explanatory framework in communication research: Exploring parallel, serial, and moderated mediation. Health Commun. 2015, 30, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Moffat, R.; Yentes, C.; Crookston, B.; West, J. Patient perceptions about professional dental services during the COVID-19 pandemic. JDR Clin. Trans. Res. 2021, 6, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Bairwa, M.; Rajput, M.; Sachdeva, S. Modified kuppuswamy’s socioeconomic scale: Social researcher should include updated income criteria, 2012. Indian J. Community Med. 2013, 38, 185. [Google Scholar] [CrossRef] [PubMed]
- Ursachi, G.; Horodnic, I.A.; Zait, A. How reliable are measurement scales? External factors with indirect influence on reliability estimators. Procedia Econ. Financ. 2015, 20, 679–686. [Google Scholar] [CrossRef]
- Personal Income in Australia. Available online: https://www.abs.gov.au/statistics/labour/earnings-and-work-hours/personal-income-australia/latest-release (accessed on 23 July 2022).
- McCaffery, K.J.; Dodd, R.H.; Cvejic, E.; Ayre, J.; Batcup, C.; Isautier, J.M.; Copp, T.; Bonner, C.; Pickles, K.; Nickel, B. Health literacy and disparities in COVID-19 related knowledge, attitudes, beliefs and behaviours by health literacy. Public Health Res. Pract. 2020, 30, 30342012. [Google Scholar] [CrossRef] [PubMed]
- de Almeida-Pititto, B.; Dualib, P.M.; Zajdenverg, L.; Dantas, J.R.; De Souza, F.D.; Rodacki, M.; Bertoluci, M.C. Severity and mortality of COVID 19 in patients with diabetes, hypertension and cardiovascular disease: A meta-analysis. Diabetol. Metab. Syndr. 2020, 12, 75. [Google Scholar] [CrossRef] [PubMed]
- Calder, R. Low Socio-Economic Status Increases Levels of Chronic Disease. Available online: https://www.ceda.com.au/NewsAndResources/Opinion/Health-Ageing/Low-socioeconomic-status-increases-levels-of-chron. (accessed on 23 July 2022).
- Australia Bureau of Statistics. Cairns. Available online: https://www.abs.gov.au/census/find-census-data/quickstats/2016/306 (accessed on 14 August 2022).
- Alam, M.M.; Wei, H.; Wahid, A.N.M. COVID-19 outbreak and sectoral performance of the Australian stock market: An event study analysis. Aust. Econ. Pap. 2021, 60, 482–495. [Google Scholar] [CrossRef] [PubMed]
- Advice for Groups at Greater Risk. Available online: https://www.health.gov.au/health-alerts/covid-19/advice-for-groups-at-risk (accessed on 23 July 2022).
- Cairns. Available online: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/306 (accessed on 23 July 2022).
- Australia Bureau of Statistics. Estimates of Aboriginal and Torres Strait Islander Australians. Available online: https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/estimates-aboriginal-and-torres-strait-islander-australians/latest-release (accessed on 23 July 2022).
- Shahid, S.; Finn, L.D.; Thompson, S.C. Barriers to participation of Aboriginal people in cancer care: Communication in the hospital setting. Med. J. Aust. 2009, 190, 574–579. [Google Scholar] [CrossRef] [PubMed]
| Variables | n | % |
|---|---|---|
| Overall | 247 | |
| Gender | ||
| Male | 122 | 49.4 |
| Female | 125 | 50.6 |
| Age | ||
| 20–29 | 7 | 2.8 |
| 30–39 | 19 | 7.7 |
| 40–49 | 22 | 8.9 |
| 50–59 | 33 | 13.4 |
| 60–69 | 75 | 30.4 |
| 70–79 | 78 | 31.6 |
| 80–89 | 13 | 5.3 |
| Years Attending JCU Dental | ||
| 1–2 Years | 68 | 27.5 |
| 2–4 Years | 74 | 30.0 |
| 4+ Years | 105 | 42.5 |
| Highest Level of Education | ||
| Year 10 | 88 | 35.6 |
| Year 12 | 54 | 21.9 |
| Tafe/Certificate 3 or 4 | 45 | 18.2 |
| Bachelor’s Degree | 34 | 13.8 |
| Post Graduate Degree | 16 | 6.5 |
| Annual Income Before Tax | ||
| AUD <30,000 | 127 | 51.4 |
| AUD 30,001–50,000 | 28 | 11.36 |
| AUD 50,001–70,000 | 18 | 7.3 |
| AUD 70,001–90,000 | 22 | 8.9 |
| AUD 90,001–120,000 | 6 | 2.4 |
| AUD >120,000 | 5 | 2.0 |
| Employment Status | ||
| Working Full Time | 30 | 12.1 |
| Working Part Time | 41 | 16.6 |
| Unemployed | 29 | 11.7 |
| Retired | 136 | 55.1 |
| Health Care or Concession Card | ||
| Yes | 184 | 74.5 |
| No | 55 | 22.3 |
| Aboriginal or Torres Strait Islander | ||
| Yes | 6 | 2.4 |
| No | 234 | 94.7 |
| Significantly Better n (%) | Slightly Better n (%) | Much the Same n (%) | Slightly Worse n (%) | Significantly Worse n (%) | Mean | SD | |
|---|---|---|---|---|---|---|---|
| How do you think the COVID-19 pandemic has impacted your dental health. | 11 (4.5) | 20 (8.1) | 153 (61.9) | 38 (15.4) | 24 (9.7) | 3.18 | 0.88 |
| JCU Dental’s response to COVID-19 was appropriate; this included closure of the dental clinic in March 2020. | 105 (42.5) | 103 (41.7) | 15 (6.1) | 15 (6.1) | 9 (3.6) | 1.87 | 1.02 |
| COVID-19 protocols implemented by JCU Dental included social distancing, mandatory patient handwashing and patient mouthwash performed prior to treatment. | 21 (8.5) | 26 (10.5) | 176 (71.3) | 14 (5.7) | 10 (4) | 2.86 | 0.81 |
| Closing the JCU Dental in the March 2020 COVID-19 outbreak was appropriate. | 154 (62.3) | 38 (15.4) | 21 (8.5) | 21 (8.5) | 13 (5.3) | 1.79 | 1.22 |
| If you have attended a dental clinic in the past 12 months, have the clinic’s COVID-19 protocols impacted fears around safety? | 70 (28.3) | 37 (15) | 121 (49) | 10 (4) | 9 (3.6) | 2.4 | 1.05 |
| Access Score | Yes n (%) | No n (%) |
|---|---|---|
| Are you attending JCU Dental because you couldn’t attend your regular dentist? | 200 (51) | 40 (16.6) |
| COVID-19 pandemic has impacted my ability to travel when attending JCU Dental. | 93 (37.6) | 154 (62.3) |
| Since JCU Dental has re-opened after the COVID-19 pandemic, has the process changed to book an appointment? | 101 (42.1) | 139 (57.9) |
| Did you have an appointment cancelled due to the COVID-19 closure? | 101 (42.1) | 139 (57.9) |
| Did you have to attend another dental clinic because JCU Dental was closed due to COVID-19? | 43 (17.4) | 195 (78.9) |
| Were you notified of JCU Dental Clinic’s closure due to COVID-19? | 106 (44.1) | 133 (55.8) |
| Were you notified when JCU Dental Clinic planned to re-open? | 117 (47.4) | 120 (48.6) |
| Has COVID-19 caused you any financial hardship? | 88 (38.3) | 142 (61.7) |
| Has financial hardship impacted your ability to afford dental treatment? | 40 (28.8) | 27 (9.4) |
| Does the large number of patients attending the JCU Dental Clinic influence your attendance? | 87 (35.6) | 157 (63.6) |
| Access Score | Significantly Likely | Slightly Likely n (%) | Neither n (%) | Slightly Less Likely n (%) | Significantly Less Likely n (%) | Mean | SD |
|---|---|---|---|---|---|---|---|
| Has COVID-19 impacted your likeliness to attend the dental clinic? | 30 (12.1) | 29 (11.7) | 138 (55.9) | 19 (7.7) | 28 (11.3) | 2.94 | 1.07 |
| Would you have scheduled an appointment if you had a dental emergency after the COVID-19 restrictions were put in place? | 116 (47) | 30 (12.1) | 49 (19.8) | 20 (8.1) | 29 (11.7) | 2.25 | 1.42 |
| Are you likely to attend JCU Dental if we had a new outbreak of Cairns? | 76 (30.8) | 37 (15) | 56 (22.7) | 43 (17.4) | 31 (12.6) | 2.65 | 1.41 |
| Does the large number of patients attending the JCU Dental Clinic influence your attendance? | 17 (6.9) | 20 (8.1) | 157 (63.6) | 23 (9.3) | 27 (10.9) | 3.09 | 0.94 |
| Indicators | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Perceptions | ||||
| 2. Access | 0.473 *** | |||
| 3. Attitudes | −0.254 *** | −0.331 *** | ||
| 4. Socio-economic | −0.367 *** | −0.391 *** | 0.354 *** | |
| Mean ± SD | 2.42 ± 0.72 | 1.82 ±0.35 | 2.74 ± 0.93 | 1.90 ± 0.91 |
| Cronbach’s α | 0.649 | 0.67 | 0.61 | 0.665 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azam, H.; Agilan, N.; Pitigala, P.; Gupta, A.; Fung, J.; Miller, C.M.; Adegboye, O.; Sharma, D. Impact of COVID-19 on Patients’ Attitudes and Perceptions of Dental Health Services: A Questionnaire Based Study in an Australian University Dental Clinic. Healthcare 2022, 10, 1747. https://doi.org/10.3390/healthcare10091747
Azam H, Agilan N, Pitigala P, Gupta A, Fung J, Miller CM, Adegboye O, Sharma D. Impact of COVID-19 on Patients’ Attitudes and Perceptions of Dental Health Services: A Questionnaire Based Study in an Australian University Dental Clinic. Healthcare. 2022; 10(9):1747. https://doi.org/10.3390/healthcare10091747
Chicago/Turabian StyleAzam, Hashim, Niesha Agilan, Pulina Pitigala, Anjaneya Gupta, Julian Fung, Catherine M. Miller, Oyelola Adegboye, and Dileep Sharma. 2022. "Impact of COVID-19 on Patients’ Attitudes and Perceptions of Dental Health Services: A Questionnaire Based Study in an Australian University Dental Clinic" Healthcare 10, no. 9: 1747. https://doi.org/10.3390/healthcare10091747
APA StyleAzam, H., Agilan, N., Pitigala, P., Gupta, A., Fung, J., Miller, C. M., Adegboye, O., & Sharma, D. (2022). Impact of COVID-19 on Patients’ Attitudes and Perceptions of Dental Health Services: A Questionnaire Based Study in an Australian University Dental Clinic. Healthcare, 10(9), 1747. https://doi.org/10.3390/healthcare10091747








