Early Class III Treatment Using a Hybrid Rapid Palatal Expander and Facemask in a Patient with Partially Edentulous Maxilla Post MNTI Removal: A Case Report
Abstract
1. Introduction
- -
- Vestibular inclination of the anchorage teeth with eruption of the palatal cusps of the posterior teeth;
- -
- Rotation of the lower jaw clockwise;
- -
- Unstable and relapsing expansion;
- -
- Decrease of the dental-periodontal integrity of anchorage teeth and teeth subjected to expansive forces.
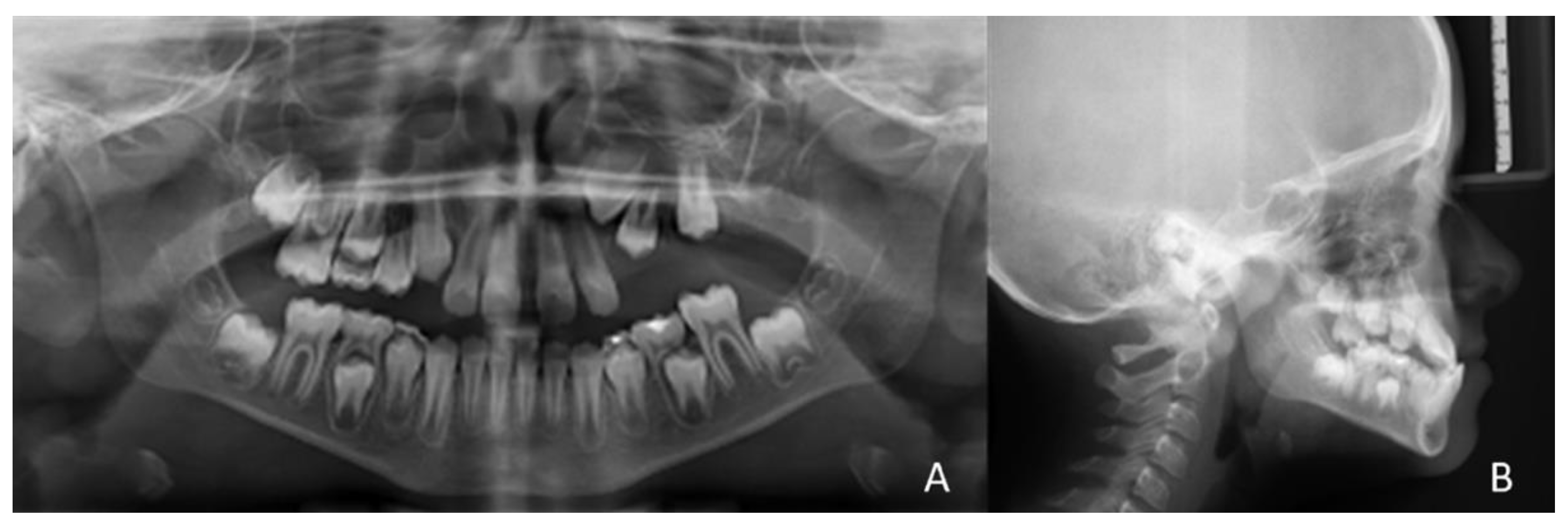
2. Patient Information and Clinical Findings
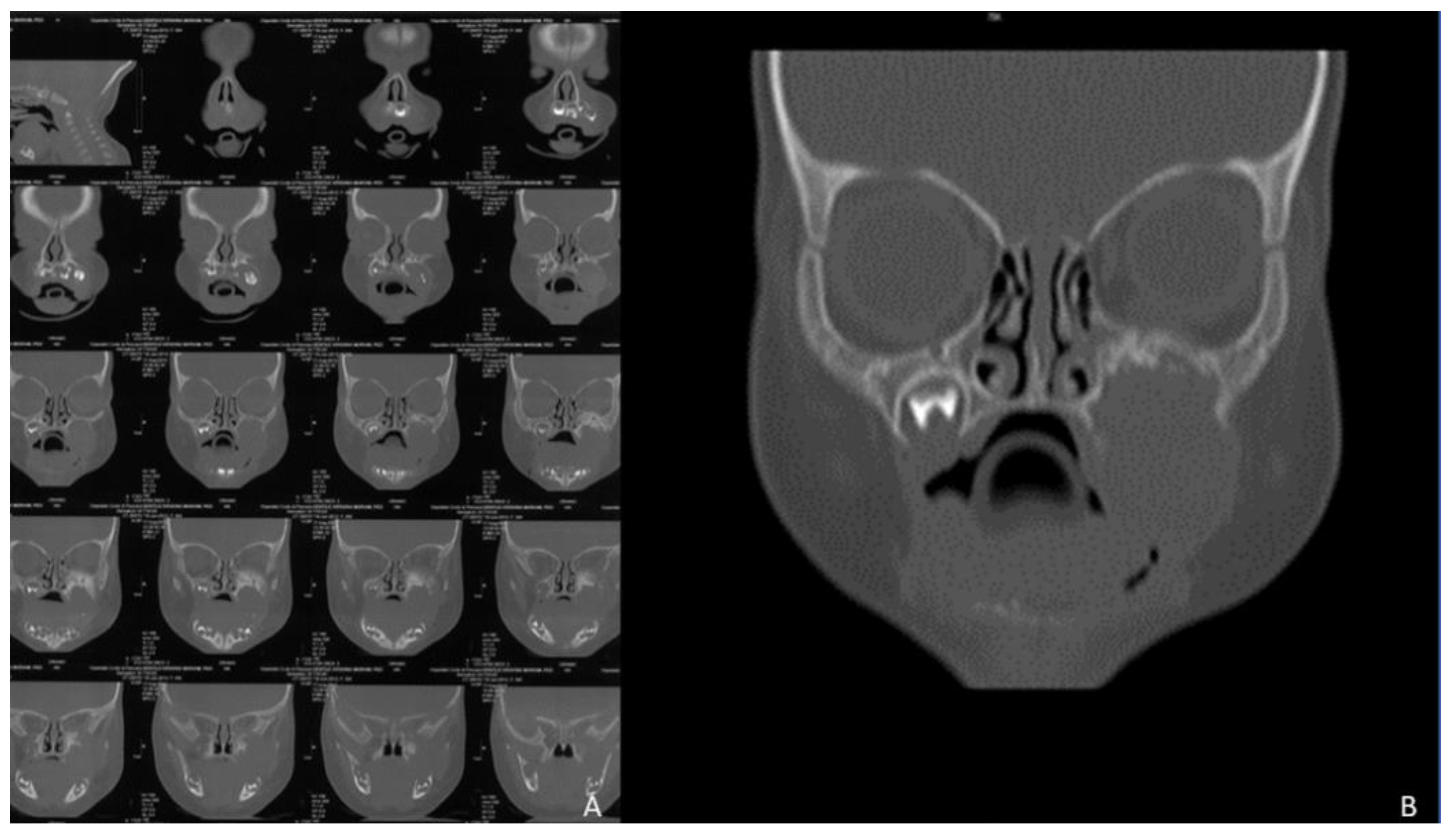
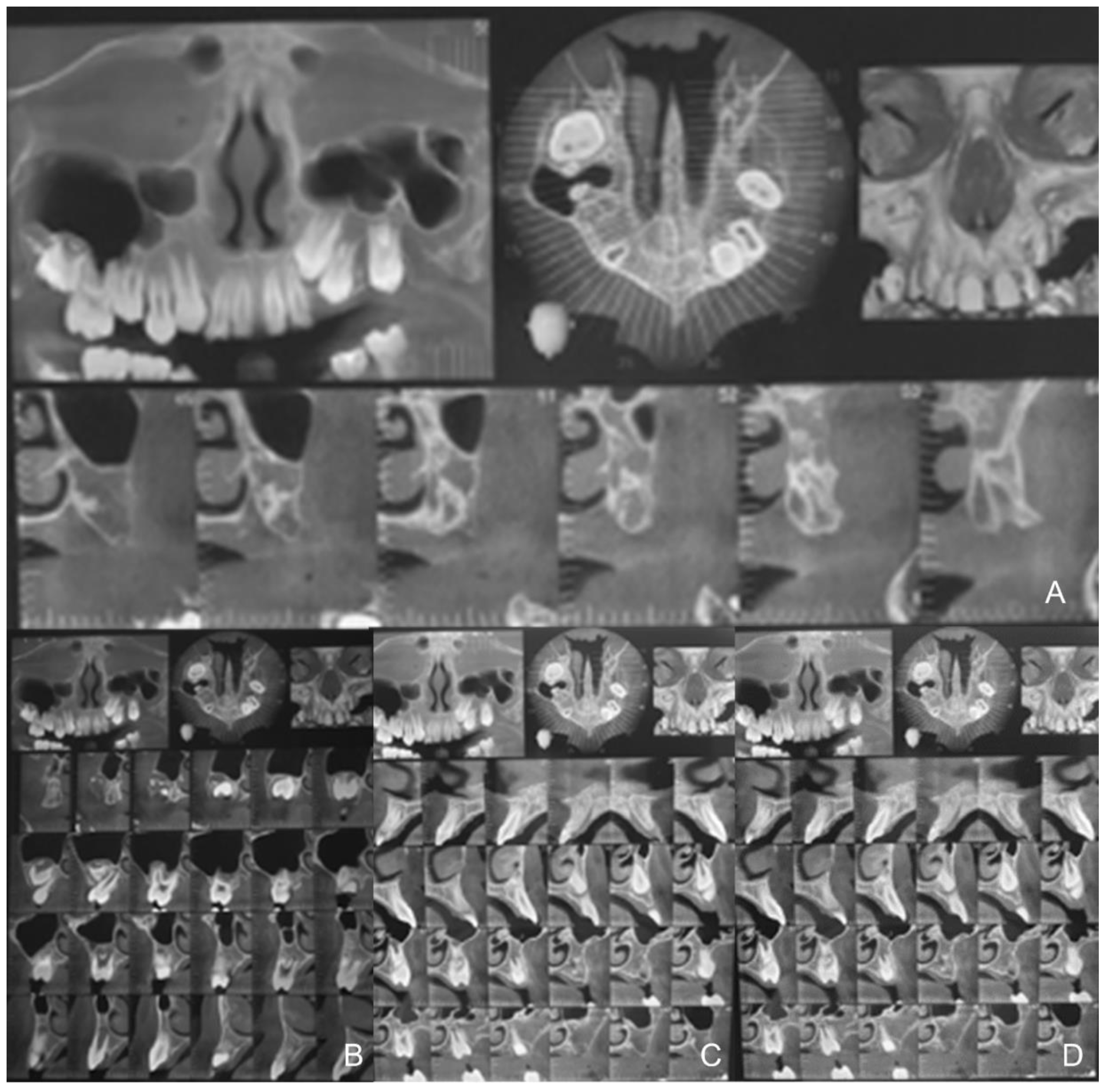
3. Diagnostic Assessment
Treatment Objectives
- -
- Correction of bilateral posterior crossbite through orthopaedic expansion procedures avoiding dental compensation.
- -
- Achieving Class I canines and molars relationship.
- -
- Correction of the frontal cross bite.
- -
- Improvement of facial aesthetics.
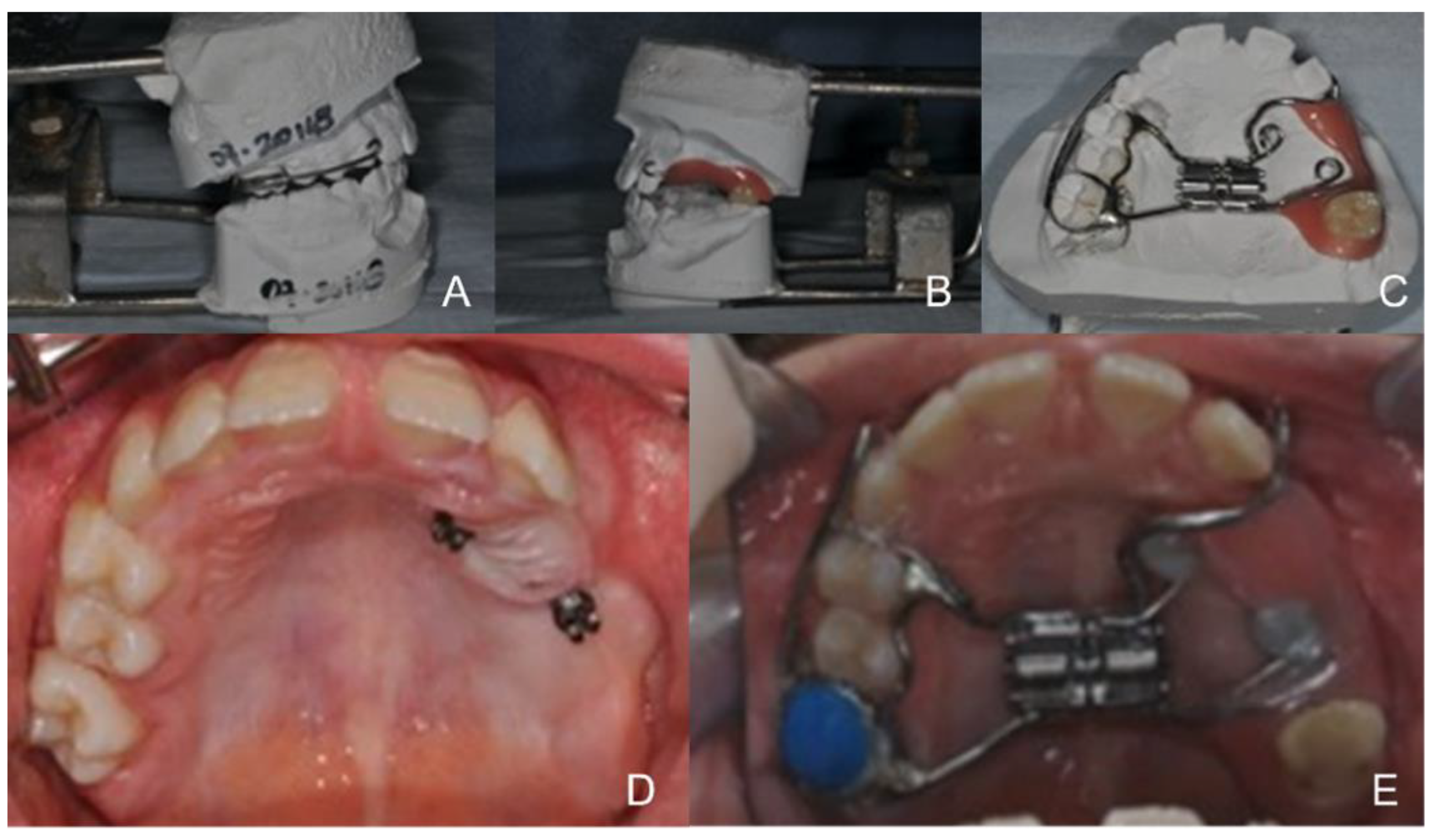
4. Therapeutic Intervention
5. Outcomes and Follow-Up
6. Discussion
7. Conclusions
8. Patient Perspective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zere, E.; Chaudhari, P.K.; Sharan, J.; Dhingra, K.; Tiwari, N. Developing Class III malocclusions: Challenges and solutions. Clin. Cosmet. Investig. Dent. 2018, 10, 99–116. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Park, Y.C.; Park, J.Y.; Hwang, W.S. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 830–839. [Google Scholar] [CrossRef]
- Seong, E.H.; Choi, S.H.; Kim, H.J.; Yu, H.S.; Park, Y.C.; Lee, K.J. Evaluation of the effects of miniscrew incorporation in palatal expanders for young adults using finite element analysis. Korean J. Orthod. 2018, 48, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, P.H.A.; Moura, L.B.; Trento, G.S.; Holzinger, D.; Gabrielli, M.A.C.; Gabrielli, M.F.R.; Filho, V.A.P. Surgically assisted rapid maxillary expansion: A systematic review of complications. Int. J. Oral Maxillofac. Surg. 2020, 49, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Seiryu, M.; Ida, H.; Mayama, A.; Sasaki, S.; Sasaki, S.; Deguchi, T.; Takano-Yamamoto, T. A comparative assessment of orthodontic treatment outcomes of mild skeletal Class III malocclusion between facemask and facemask in combination with a miniscrew for anchorage in growing patients: A single-center, prospective randomized controlled trial. Angle Orthod. 2020, 90, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Rachidi, S.; Sood, A.J.; Patel, K.G.; Nguyen, S.A.; Hamilton, H.; Neville, B.W.; Day, T.A. Melanotic Neuroectodermal Tumor of Infancy: A Systematic Review. J. Oral Maxillofac. Surg. 2015, 73, 1946–1956. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Gomez, R.S. Melanotic neuroectodermal tumour of infancy of the jaws: An analysis of diagnostic features and treatment. Int. J. Oral Maxillofac. Surg. 2019, 48, 1–8. [Google Scholar] [CrossRef]
- Borello, E.D.; Gorlin, R.J. Melanotic neuroectodermal tumor of infancy—A neoplasm of neural crese origin. Report of a case associated with high urinary excretion of vanilmandelic acid. Cancer 1966, 19, 196–206. [Google Scholar]
- Angelieri, F.; Cevidanes, L.H.; Franchi, L.; Gonçalves, J.R.; Benavides, E.; McNamara, J.A., Jr. Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 759–769. [Google Scholar] [CrossRef]
- Nienkemper, M.; Wilmes, B.; Pauls, A.; Drescher, D. Maxillary protraction using a hybrid hyrax- facemask combination. Prog. Orthod. 2013, 14, 5. [Google Scholar] [CrossRef]
- Jager, A.; Braumann, B.; Kim, C.; Wahner, S. Skeletaland dental effects of maxillary pro- traction in patients with Angle Class III malocclusion: A meta-analysis. J. Orofac. Orthop. 2001, 62, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.Y.; Yang, H.; Lai, E.H.; Lin, S.Y.; Chang, J.Z. Three-phase treatment concept for skeletal Class III growing patients with severe space deficiency: A report of three cases with skeletally anchored maxillary protraction. J. Med. Assoc. 2020, 119, 869–878. [Google Scholar] [CrossRef] [PubMed]
- Kruse-Lösler, B.; Gaertner, C.; Bürger, H.; Seper, L.; Joos, U.; Kleinheinz, J. Melanotic neuroectodermal tumor of infancy: Systematic review of the literature and presentation of a case. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, 204–216. [Google Scholar] [CrossRef]
- Hichijo, N.; Noguchi, T.; Sasaguri, K.; Mori, Y. Orthodontic Treatment for a Child with Melanotic Neuroectodermal Tumor during Infancy: A Case Report. Appl. Sci. 2021, 11, 11541. [Google Scholar] [CrossRef]
- Elpis Kolokitha, O.; Kotsiomiti, E.; Lazaridis, K.; Lazaridis, N. Mandibular Melanotic Neuroectodermal Tumor of Infancy: Interdisciplinary Treatment from 2 Months to 19 Years of Age. J. Maxillofac. Oral Surg. 2022, 21, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.H.; Chen, T.W.; Chang, H.S. Melanotic neuroectodermal tumour of infancy in the maxilla: A case report. Int. J. Paediatr. Dent. 2004, 14, 371–375. [Google Scholar] [CrossRef]
- Haberko, P.; Lewandowski, B.; Brodowski, R.; Chrzanowska-Kler, E.; Osluchowski, M.; Zych, B.; Migut, M. Melanotic neuroectodermal tumor of infancy. J. Pre-Clin. Clin. 2021, 15, 26–29. [Google Scholar] [CrossRef]
- Kyoko, K.; Katsuhiko, A.; Kazuma, H.; Masaya, O.; Mikihiko, K.; Susumu, T. The secondary case of melanotic neuroectodermal tumor in the infant maxilla: Long-term observation after the enucleation. J. Oral Maxillofac Surg. Med. Pathol. 2022, 34, 599–604. [Google Scholar]
- Rustemeyer, J.; Günther, L.; Junker, K.; Thieme, V.; Busch, A.; Okcu, Y.; Siegmund, B.J. Melanotic Neuroectodermal Tumour of Infancy: Clinical Courses and Therapeutic Options—A Review of Three Cases. J. Maxillofac Oral Surg. 2021, 20, 219–226. [Google Scholar] [CrossRef]
- Jedliński, M.; Mazur, M.; Grocholewicz, K.; Janiszewska-Olszowska, J. 3D Scanners in Orthodontics-Current Knowledge and Future Perspectives-A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 1121. [Google Scholar] [CrossRef]
- Trybek, G.; Jedliński, M.; Jaroń, A.; Preuss, O.; Mazur, M.; Grzywacz, A. Impact of lactoferrin on bone regenerative processes and its possible implementation in oral surgery—A systematic review of novel studies with metanalysis and metaregression. BMC Oral Health 2020, 20, 232. [Google Scholar] [CrossRef] [PubMed]
- Janes, L.E.; Bazina, M.; Morcos, S.S.; Ukaigwe, A.; Valiathan, M.; Jacobson, R.; Gosain, A.K. The Relationship Between Dental Agenesis and Maxillary Hypoplasia in Patients With Cleft Lip and Palate. J. Craniofac. Surg. 2021, 32, 2012–2015. [Google Scholar] [CrossRef] [PubMed]
- Willershausen, I.; Krautkremer, F.; Hilbert, T.; Seidel, C.L.; Geppert, C.I.; Ghanaati, S.; Necker, F.; Paulsen, F.; Gölz, L.; Scholz, M. The comparison of the morphology of the mid-palatal suture between edentulous individuals and dentate jaws shows morphological differences. Ann. Anat. 2022, 243, 151948. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Ahn, H.-W.; Kim, S.-J.; Moon, S.-C.; Kim, S.H.; Nelson, G. Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015, 85, 253–262. [Google Scholar] [CrossRef]
- Choi, S.-H.; Shi, K.-K.; Cha, J.-Y.; Park, Y.-C.; Lee, K.J. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 2016, 86, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Park, J.J.; Park, Y.-C.; Lee, K.-J.; Cha, J.Y.; Tahk, J.H.; Choi, Y.J. Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study. Korean J. Orthod. 2017, 47, 77–86. [Google Scholar] [CrossRef]
- Chuang, Y.-H.; Chen, J.-H.; Ho, K.-H.; Kang, K.-L.; Hsieh, S.-C.; Chang, H.-M. The role of micro-implant-assisted rapid palatal expansion (MARPE) in clinical orthodontics-a literature review. Aust. Orthod. J. 2021, 37, 206–216. [Google Scholar]
- Ierardo, G.; Luzzi, V.; Sfasciotti, G.L.; Nardacci, G.; Polimeni, A.; Vozza, I. Using of modified rapid palate expander with miniscrews in a patient affected by ectodermic dysplasia. Clin. Ter. 2019, 170, e168–e173. [Google Scholar]
- Suzuki, H.; Moon, W.; Previdente, L.H.; Suzuki, S.S.; Garcez, A.S.; Consolaro, A. Miniscrew-assisted rapid palatal expander (MARPE): The quest for pure orthopedic movement. Dent. Press J. Orthod. 2016, 4, 17–23. [Google Scholar] [CrossRef]
- de Almeida, R.R.; Alessio Junior, L.E.; de Almeida-Pedrin, R.R.; de Almeida, M.R.; Pinzan, A.; Vieira, L.S. Management of the Class III malocclusion treated with maxillary expansion, facemask therapy and corrective orthodontic. A 15-year follow-up. J. Appl. Oral Sci. 2015, 1, 101–109. [Google Scholar] [CrossRef]









Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luzzi, V.; Marasca, B.; Mazur, M.; Ndokaj, A.; Pirro, V.; Guaragna, M.; Altieri, F.; Ierardo, G. Early Class III Treatment Using a Hybrid Rapid Palatal Expander and Facemask in a Patient with Partially Edentulous Maxilla Post MNTI Removal: A Case Report. Healthcare 2022, 10, 1746. https://doi.org/10.3390/healthcare10091746
Luzzi V, Marasca B, Mazur M, Ndokaj A, Pirro V, Guaragna M, Altieri F, Ierardo G. Early Class III Treatment Using a Hybrid Rapid Palatal Expander and Facemask in a Patient with Partially Edentulous Maxilla Post MNTI Removal: A Case Report. Healthcare. 2022; 10(9):1746. https://doi.org/10.3390/healthcare10091746
Chicago/Turabian StyleLuzzi, Valeria, Beatrice Marasca, Marta Mazur, Artnora Ndokaj, Valentina Pirro, Mariana Guaragna, Federica Altieri, and Gaetano Ierardo. 2022. "Early Class III Treatment Using a Hybrid Rapid Palatal Expander and Facemask in a Patient with Partially Edentulous Maxilla Post MNTI Removal: A Case Report" Healthcare 10, no. 9: 1746. https://doi.org/10.3390/healthcare10091746
APA StyleLuzzi, V., Marasca, B., Mazur, M., Ndokaj, A., Pirro, V., Guaragna, M., Altieri, F., & Ierardo, G. (2022). Early Class III Treatment Using a Hybrid Rapid Palatal Expander and Facemask in a Patient with Partially Edentulous Maxilla Post MNTI Removal: A Case Report. Healthcare, 10(9), 1746. https://doi.org/10.3390/healthcare10091746







