An Observational Study Using Ultrasound to Assess Allowable Needle Insertion Range of Acupoint CV12
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
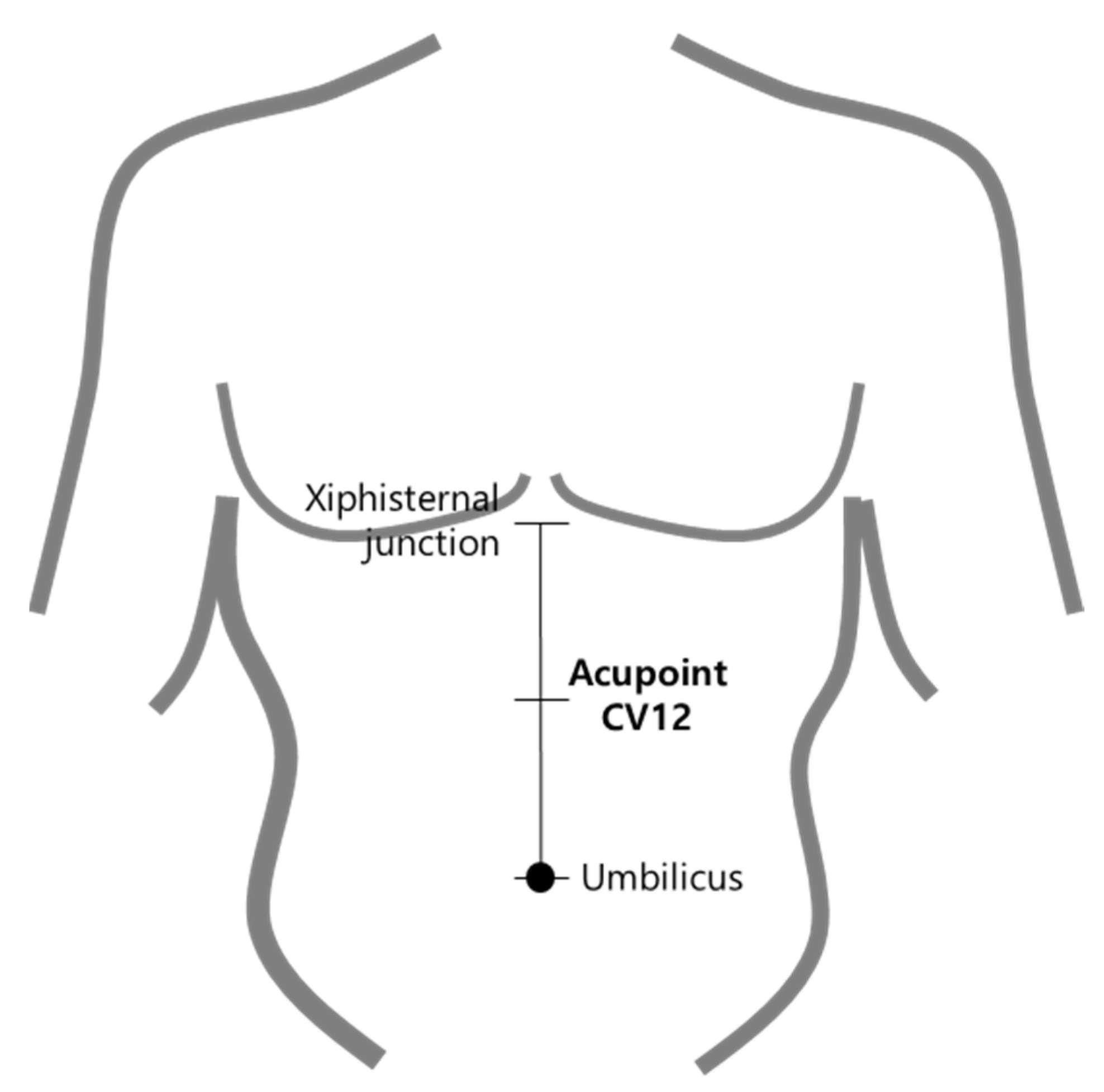
2.2. Location of Acupoint CV12
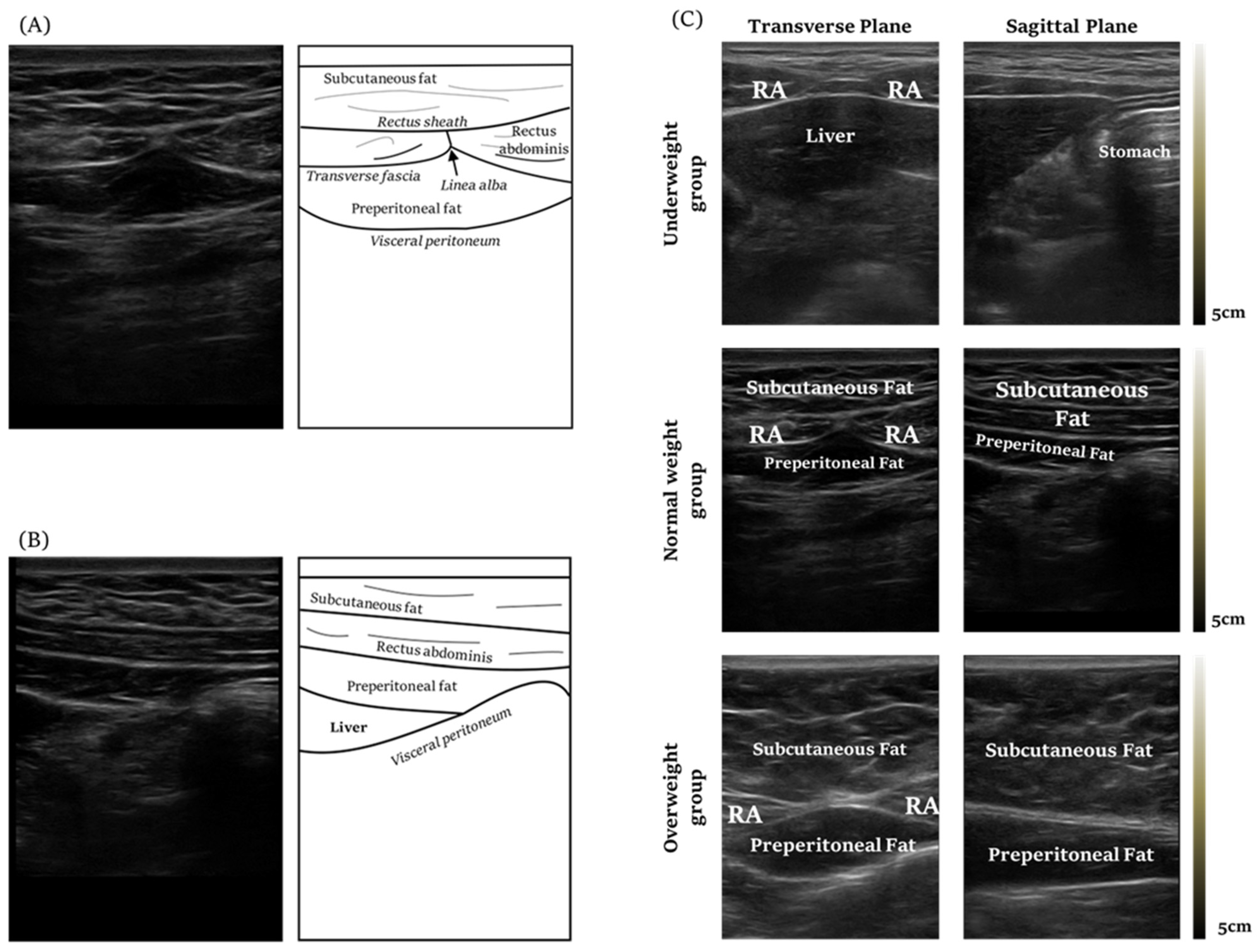
2.3. Acquiring Ultrasound Imaging of Acupoint CV12
2.4. Analysis and Measurement
2.5. Measurement of Anthropometric Parameters
2.6. Satistical Analysis
3. Results
3.1. Subject Characteristics
3.2. Safe Needling Depth of CV12
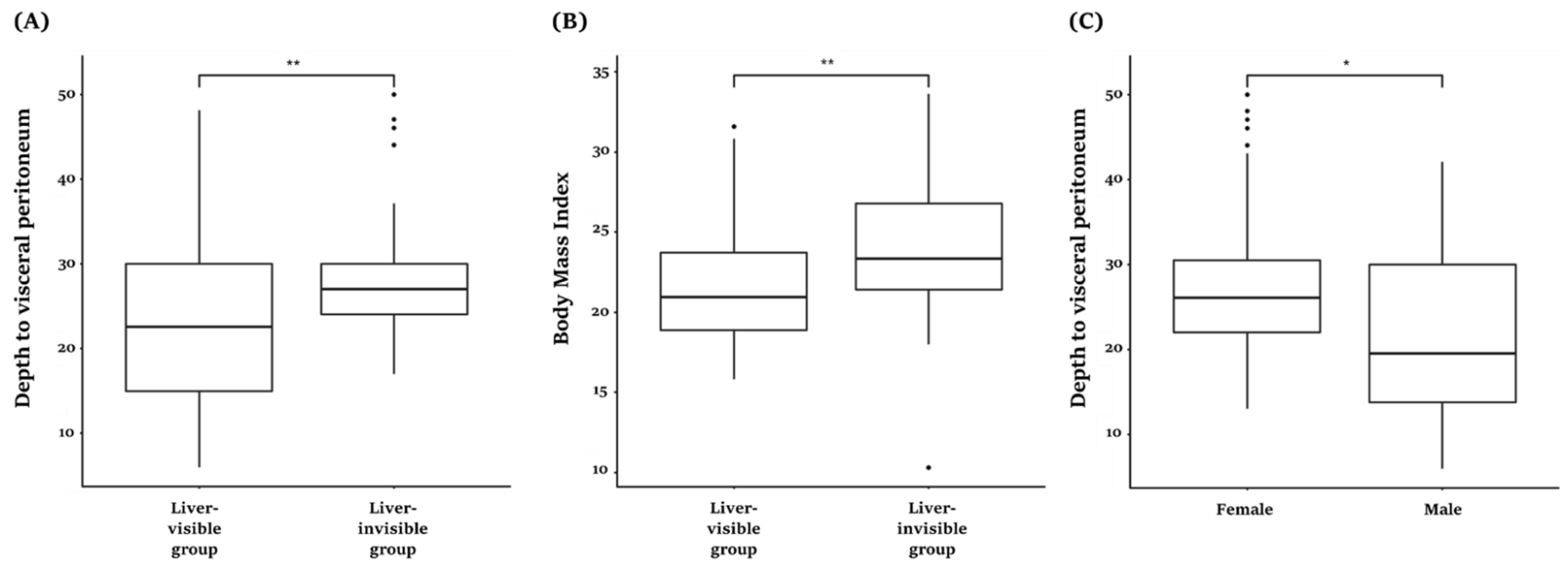
3.3. The Degree of Risk of Liver Damage in CV12 and Physical Characteristics of the Risk Group
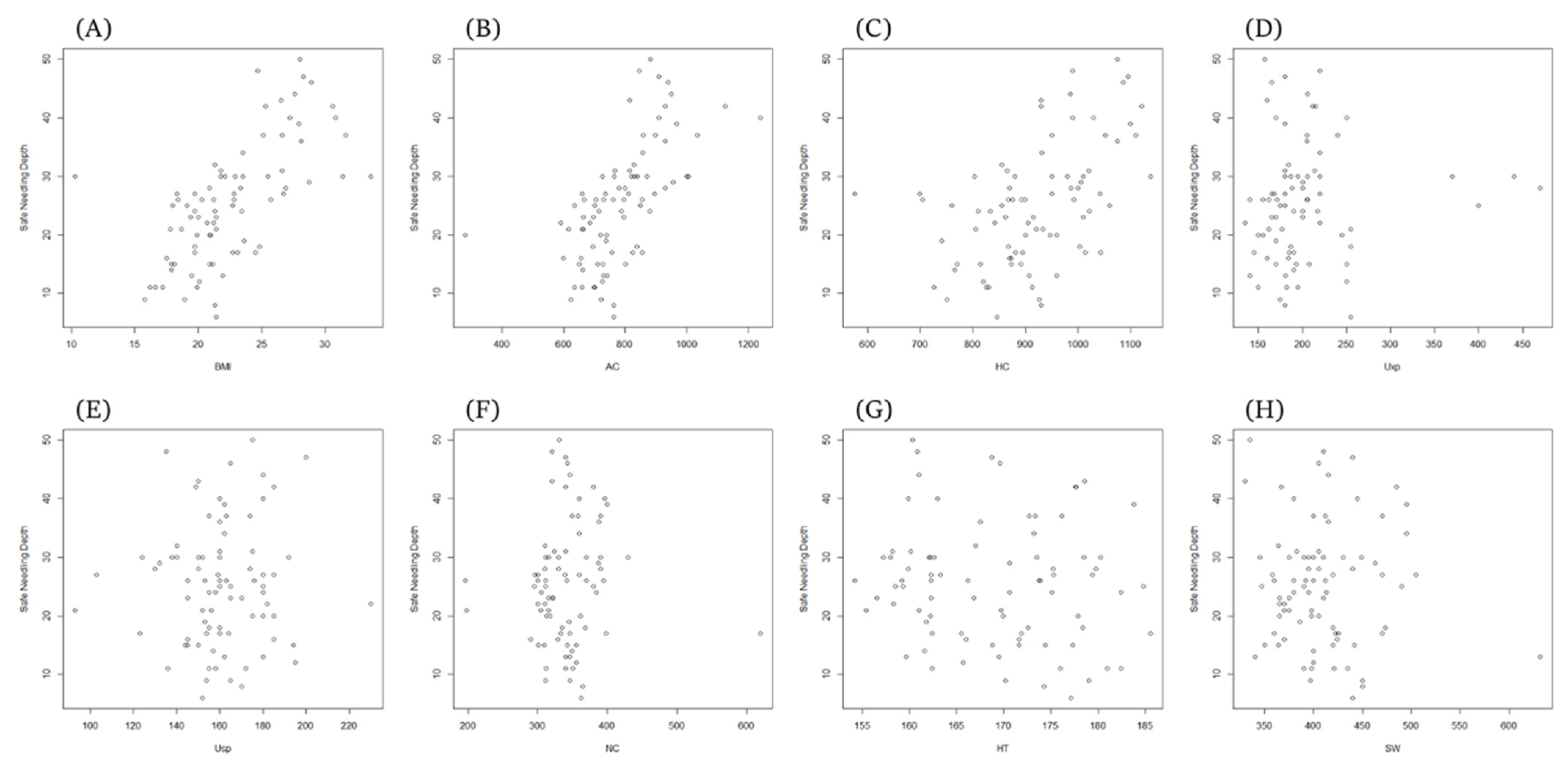
3.4. Correlation between Needling Depth and Anthropometric Parameters in the Study Group
3.5. Regression Analysis Results for ANIR Related to Anthropometric Parameters
3.6. Sub-Group Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vincent, C. The safety of acupuncture: Acupuncture is safe in the hands of competent practitioners. BMJ 2011, 323, 467–468. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, H.; Thomas, K.; Walters, S.; Fitter, M. A prospective survey of adverse events and treatment reactions following 34,000 consultations with professional acupuncturists. Acupunct. Med. 2001, 19, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Ernst, E.; White, A.R. Prospective studies of the safety of acupuncture: A systematic review. Am. J. Med. 2001, 110, 481–485. [Google Scholar] [CrossRef]
- Lan, L.; Zeng, F.; Liu, G.J.; Yin, L.; Wu, X.; Liu, M.; Liang, F.R. Acupuncture for functional dyspepsia. Cochrane Database Syst. Rev. 2014, 10, CD008487. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Lee, M.; Choi, T.; Kim, T. Acupuncture for symptomatic gastroparesis. Cochrane Database Syst. Rev. 2018, 12, CD009676. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Shang, H.; Gao, X.; Ernst, E. Acupuncture-related adverse events: A systematic review of the Chinese literature. Bull. World Health Organ. 2010, 88, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, Y.; Kim, W. Safety Concerns with Thoracoabdominal Acupuncture: Experience at a Tertiary-Care Emergency Department. Pain Med. 2017, 18, 2504–2508. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Ahn, J.; Choi, W.; Kim, E.; Bae, S.; Choi, Y.; Jung, H.; Kim, J. A needle penetrating the stomach cavity after acupuncture. Clin. Endosc. 2014, 47, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.; Ahn, S. The study on Needling insertion method at CV12 in Cim-gu-kyung-heom-bang. Korean J. Acupunct. 2010, 27, 35–47. [Google Scholar]
- Lee, D.; Kim, J.; Kang, Y.; Ko, H. A study on historical and cultural viewpoints of traditional measuring units conversion. J. Korean Med. Hist. 2010, 23, 15–22. [Google Scholar]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. 1), S31–S34. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Standard Acupuncture Point Locations in the Western Pacific Region; World Health Organization: Geneva, Switzerland, 2011.
- Kim, S.; Lee, S.; Ha, W.; Lee, J.; Jung, H.; Chu, H.; Yang, S.; Choi, S.; Son, M.; Kim, J.; et al. Development of an ultrasound-imaging procedure and acquisition of ultrasound images of acupuncture points for safety and accuracy of needle insertion. Integr. Med. Res. 2017, 6, 427–433. [Google Scholar] [CrossRef] [PubMed]
- CDC (Centers for Disease Control and Prevention). National Health and Nutrition Examination Survey (NHANES): Anthropometry Procedures Manual; Centers for Disease Control and Prevention: Cincinnati, OH, USA, 2016.
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- WHO (World Health Organization). BMI Classification; World Health Organization: Geneva, Switzerland, 2014.
- Chen, H.; Lin, J.; Yang, A.; Chang, S. Safe depth of abdominal acupoints in pediatric patients. Complement. Med. 2008, 16, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Lin, J.; Ying, L.; Huang, C.; Lin, C. The therapeutic depth of abdominal acupuncture points approaches the safe depth in overweight and in older children. J. Altern. Complement. Med. 2009, 15, 1033–1037. [Google Scholar] [CrossRef]
- Xu, T.; Mao, Z.; Yu, W. Cardiac tamponade following acupuncture: How can we do more to avoid this happening? Acupunct. Med. 2020, 38, 207–208. [Google Scholar] [CrossRef]
- Leow, M.; Cao, T.; Lee, S.; Cui, S.; Tay, S.; Ooi, C. Ultrasonography in acupuncture: Potential uses for education and research. Acupunct. Med. 2016, 34, 320–322. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, B.; Kim, S.; Shin, J.; Choi, Y.; Song, B.; Yook, T.; Jeon, Y.; Lee, S. A Pilot Clinical Study on the Accuracy and Safety of Ultrasound-guided Gyeontonghyeol (BP-LE6) Acupuncture: A Prospective Randomized, Single Blinded Crossover Study. J. Acupunct. Res. 2019, 36, 272–276. [Google Scholar] [CrossRef]
- Cho, E.; Han, Y.; Kang, Y.; Kim, J.; Shin, M.; Oh, M.; Cho, N.; Jung, H.; Leem, J. Implementation of Objective Structured Clinical Examination on Diagnostic Musculoskeletal Ultrasonography Training in Undergraduate Traditional Korean Medicine Education: An Action Research. Diagnostics 2022, 12, 1707. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.; Han, Y.; Kang, Y.; Kim, J.; Shin, M.; Oh, M.; Jung, H.; Jeon, H.; Cho, N.; Leem, J. Development of an Objective Structured Clinical Examination Checklist and a Post-Education Questionnaire for Musculoskeletal Ultrasound Training Focusing on Volar Wrist and Carpal Tunnel Syndrome. J. Acupunct. Res. 2022, 39, 105–114. [Google Scholar] [CrossRef]


| Male | Female | Total | |
|---|---|---|---|
| Sample | 40 | 43 | 83 |
| BMI (kg/m2) | 23.0 ± 4.6 | 21.9 ± 3.7 | 22.4 ± 4.2 |
| Underweight (<18.5 kg/m2) | 7 | 7 | 14 |
| Normal Weight (≥18.5 & <25 kg/m2) | 21 | 26 | 47 |
| Overweight (≥25 kg/m2) | 12 | 10 | 22 |
| Neck circumference (mm) | 369.4 ± 47.3 | 313.8 ± 31.0 | 340.6 ± 48.4 |
| Shoulder width (mm) | 438.1 ± 45.6 | 381.7 ± 26.2 | 408.9 ± 46.4 |
| Abdomen circumference (mm) | 825.4 ± 134.6 | 748.8 ± 118.8 | 785.7 ± 132.3 |
| Hip circumference (mm) | 928.2 ± 125.6 | 912.1 ± 88.6 | 919.8 ± 108.3 |
| Umbilicus to xiphoid process (mm) | 216.4 ± 69.6 | 188.4 ± 37.8 | 201.9 ± 57.2 |
| Umbilicus to symphysis pubis (mm) | 158.1 ± 13.6 | 162.7 ± 24.9 | 160.5 ± 20.4 |
| Subcutaneous Fat Thickness at CV12 (mm) | Depth to Peritoneum at CV12 (mm) | ||
|---|---|---|---|
| Total | Total | 16.0 ± 7.7 | 25.3 ± 10.2 |
| Underweight | 8.1 ± 4.5 | 15.4 ± 5.9 | |
| Normal Weight | 14.0 ± 5.2 | 22.2 ± 7.5 | |
| Overweight | 24.3 ± 6.8 | 36.9 ± 6.9 | |
| Male | Total | 13.4 ± 7.5 | 22.3 ± 10.2 |
| Underweight | 5.9 ± 2.6 | 12.4 ± 2.4 | |
| Normal Weight | 11.4 ± 5.6 | 18.8 ± 7.5 | |
| Overweight | 20.5 ± 5.5 | 33.9 ± 5.2 | |
| Female | Total | 18.5 ± 7.1 | 28.1 ± 9.4 |
| Underweight | 13.3 ± 3.7 | 23.3 ± 5.8 | |
| Normal Weight | 15.8 ± 4.1 | 24.7 ± 6.4 | |
| Overweight | 28.0 ± 6.3 | 40.1 ± 7.4 | |
| ANIR | BMI | AC | NC | SW | HC | Uxp | Usp | HT | |
|---|---|---|---|---|---|---|---|---|---|
| ANIR | |||||||||
| BMI | 0.662 ** | ||||||||
| AC | 0.620 ** | 0.788 ** | |||||||
| NC | 0.053 | 0.409 ** | 0.478 ** | ||||||
| SW | −0.050 | 0.210 | 0.299 | 0.385 ** | |||||
| HC | 0.507 ** | 0.656 ** | 0.601 | 0.309 ** | 0.271 | ||||
| Uxp | 0.093 | 0.065 | 0.273 | 0.178 | 0.164 | 0.157 | |||
| Usp | 0.042 | 0.029 | −0.073 | 0.076 | 0.015 | 0.091 | −0.124 | ||
| HT | −0.114 | 0.101 | 0.249 | 0.325 ** | 0.469 | 0.181 | 0.265 | −0.001 |
| Stepwise Linear Regression | Variable | B | SE | β | t | F | R2 |
|---|---|---|---|---|---|---|---|
| −10.960 | 4.638 | −2.363 * | 63.204 *** | 0.431 *** | |||
| Independent variable | BMI (kg/m2) | 1.616 | 0.203 | 0.662 | 7.950 *** | ||
| Multiple Regression | Variable | B | SE | β | t | F | R2 |
| −12.271 | 5.354 | −2.292 * | 50.613 *** | 0.377 *** | |||
| Independent variable | Abdomen (mm) | 0.048 | 0.007 | 0.620 | 7.114 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chu, H.; Kim, J.; Park, S.; Kim, J.; Lee, J.-H.; Ha, W.-B.; Jung, H.-J.; Yang, S.-b.; Kim, C.-h.; Park, J.Y.; et al. An Observational Study Using Ultrasound to Assess Allowable Needle Insertion Range of Acupoint CV12. Healthcare 2022, 10, 1707. https://doi.org/10.3390/healthcare10091707
Chu H, Kim J, Park S, Kim J, Lee J-H, Ha W-B, Jung H-J, Yang S-b, Kim C-h, Park JY, et al. An Observational Study Using Ultrasound to Assess Allowable Needle Insertion Range of Acupoint CV12. Healthcare. 2022; 10(9):1707. https://doi.org/10.3390/healthcare10091707
Chicago/Turabian StyleChu, Hongmin, Jaehyo Kim, Seongjun Park, Jaehyun Kim, Jung-Han Lee, Won-Bae Ha, Hyun-Jong Jung, Seung-bum Yang, Cheol-hyun Kim, Jun Yong Park, and et al. 2022. "An Observational Study Using Ultrasound to Assess Allowable Needle Insertion Range of Acupoint CV12" Healthcare 10, no. 9: 1707. https://doi.org/10.3390/healthcare10091707
APA StyleChu, H., Kim, J., Park, S., Kim, J., Lee, J.-H., Ha, W.-B., Jung, H.-J., Yang, S.-b., Kim, C.-h., Park, J. Y., Kang, K.-h., Lee, S., & Lee, S. (2022). An Observational Study Using Ultrasound to Assess Allowable Needle Insertion Range of Acupoint CV12. Healthcare, 10(9), 1707. https://doi.org/10.3390/healthcare10091707





