Healthcare Supply Chain Management under COVID-19 Settings: The Existing Practices in Hong Kong and the United States
Abstract
:1. Introduction
2. Literature Review
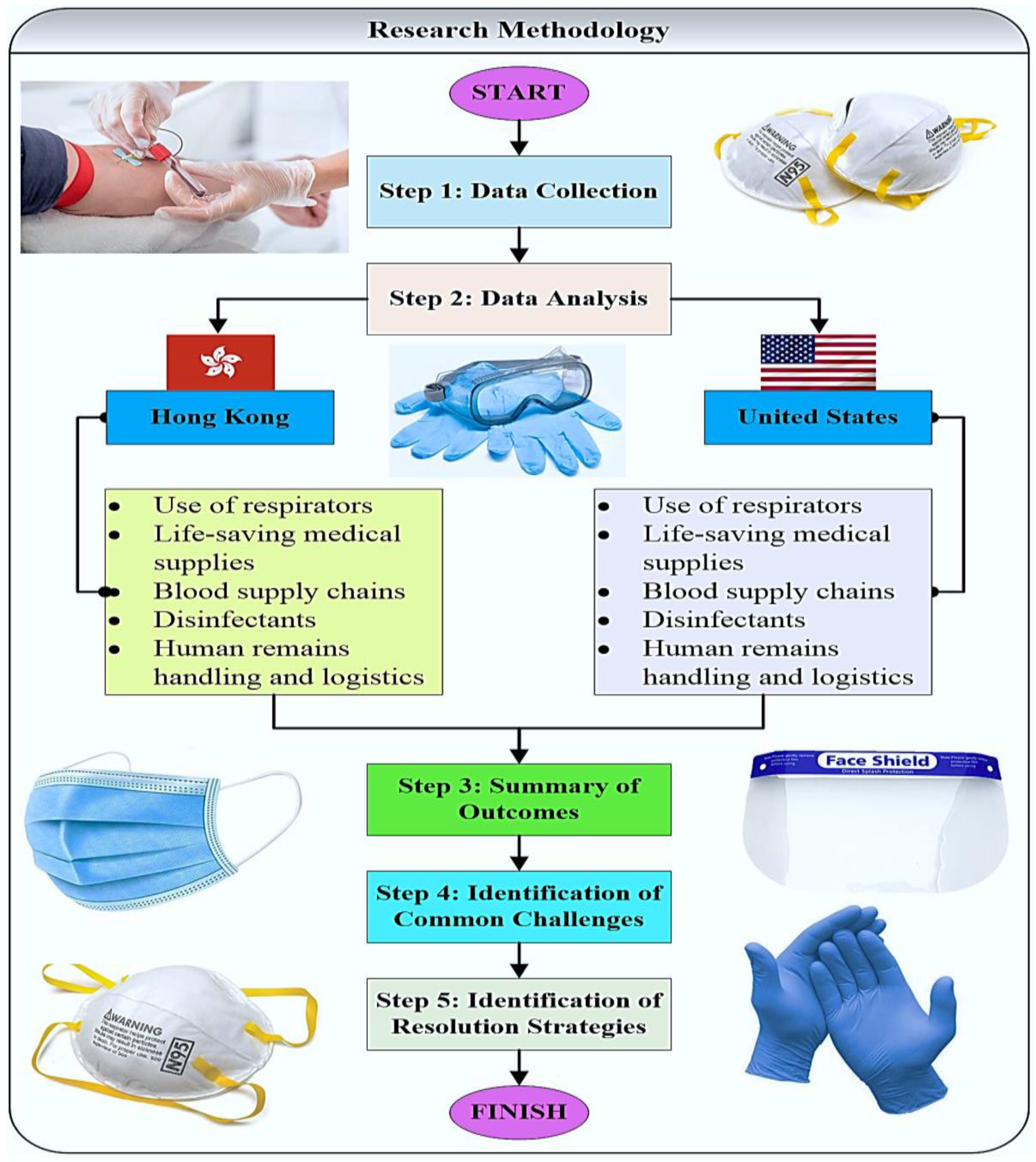
3. Methodology
Case Study
4. Results
4.1. Review of Healthcare Supply Chain Management in Hong Kong
4.1.1. Use of Respirators
4.1.2. Life-Saving Medical Supplies
4.1.3. Blood Supply Chains
- Members of the public who have recently visited a particular place that was later found to have active community transmission of COVID-19 should be deferred from blood donation for at least 28 days from the date of departure.
- Members of the public who had close contact with a person positively tested for COVID-19 while that person was symptomatic should be deferred from blood donation for at least 28 days.
- Members of the public who tested positive for COVID-19 will be deferred from blood donation for at least 180 days after complete recovery.
4.1.4. Disinfectants
4.1.5. Human Remains Handling and Logistics
4.2. Review of Healthcare Supply Chain Management in the United States
4.2.1. Use of Respirators
4.2.2. Life-saving Medical Supplies
4.2.3. Blood Supply Chains
4.2.4. Disinfectants
4.2.5. Human Remains Handling and Logistics
5. Discussion
- Some of the strategies that are used in Hong Kong and the U.S. for optimizing the supply of N95 respirators and conducting other healthcare activities may seem harsh to a certain extent (e.g., the use of respirators beyond the design shelf life for healthcare delivery). Some additional alternatives should be considered in order to improve the existing strategies. In particular, countries that experience a sharp increase in COVID-19 cases should collaborate with countries that have surpassed the COVID-19 peak, so the countries that have a surplus of N95 respirators can share them with the countries that experience a shortage. Furthermore, there are some alternatives to extending the life of N95 respirators. It is possible to extend the use of N95 respirators for up to 8 h or reuse N95 respirators by following certain methods, such as mask rotation, decontamination/reprocessing, hydrogen peroxide vaporization, UV treatment, moist heat, and dry heat. Furthermore, the healthcare industry may collaborate with logistics firms and manufacturers to create a storage system for the extended use and reuse of N95 filtering facepiece respirators so as to stabilize the supply of N95 respirators in the long term [55]. In the near future, a new product (i.e., Aeri mask) is expected to be introduced to the healthcare market. This product can perform various functions (e.g., self-cleaning, facial recognition, antifogging, removable air filters, and incorporated fan for breathable relaxation) and overcome the shortage problem along with the shortcomings of N95 respirators [56].
- As the HA and the U.S. Strategic National Stockpile are expected to have a shortage of life-saving medical supplies and pharmaceuticals due to the COVID-19 pandemic, new policies should be developed to prioritize deliveries of life-saving medical supplies and pharmaceuticals among key locations (i.e., nursing homes, hospitals, healthcare facilities, and the regions that experience severe COVID-19 consequences should receive priority). In other words, healthcare supply chain stakeholders need to be responsive to the evidence instead of allocating the available resources on a first-come, first-served principle. As suggested by Lau et al. (2020) [4], an extensive distribution network can ensure the reliability of the inventory level for life-saving medical supplies and pharmaceuticals and the effectiveness of emergency material transportation. In order to solve the issue of deficiency of life-saving medical supplies and pharmaceuticals, expanding the resources to a minimum of two different countries and producing life-saving medical and pharmaceuticals in the home countries or cities rather than depending on imports would be viable alternatives [57].
- The U.S. American Association of Blood Banks (AABB) does provide some strategies for hospitals to tackle the issues that are associated with the blood supply shortage. However, these strategies have to be further tested and evaluated to determine their effectiveness for blood supply chains. On the other hand, the Hong Kong Red Cross is mainly concerned with the minimization of COVID-19 transmission via blood donation. This leads to shortages in the donated blood inventory level. The HA closely collaborates with the Hong Kong Red Cross to oversee emergency blood supplies and manage the donated blood inventory level. As expected, the COVID-19 pandemic and the termination of mobile blood drives further discourage donors from blood donations. As such, one viable alternative to address this issue would be the allocation of mobile blood drives traveling directly to donors’ homes following necessary COVID-19 precautions, especially in the case of lockdown and social distancing policies. Furthermore, blood conservation approaches, such as improved patient blood management, could also be adopted. Under patient blood management, the overall blood utilization could be enhanced. Additionally, better management of the demand for blood transfusions will help to protect blood stocks during the pandemic situation [58].
- The U.S. Environmental Protection Agency (EPA) provides a database for the recommended disinfectants against COVID-19. However, some regions of the country experienced a shortage of certain disinfectants (especially, during the COVID-19 peak period). A set of additional guidelines are needed for individuals and healthcare institutions on the use of alternative disinfectants in case of primary disinfectants being temporarily unavailable (due to the shortage issue). Similar to the United States, there is a wide range of disinfectants against COVID-19 in Hong Kong for the general public. To this end, the Hong Kong Consumer Council conducted a comprehensive investigation into the quality of disinfectants. Hong Kong residents are required to follow the Hong Kong Consumer Council recommendations on purchasing disinfectant products from reputable brands or renowned retailers. Interestingly, business firms, educational institutions, hospitals, and governments outsource disinfection services to professional service providers. Outsourcing the non-core business could help the firm minimize the investment risk, keep operational control, and concentrate on core tasks during the COVID-19 pandemic. Importantly, the firms may need to form a cross-disciplinary team to search for the best possible service providers and develop strategic partners. Both parties may jointly invest and produce local disinfectants so as to avoid relying on imported products.
- Both the United States (i.e., The U.S. Center for Disease Control and Prevention (CDC) and state Departments of Health) and Hong Kong (i.e., Food and Environmental Hygiene Department and Center for Health Protection (CHP)) have detailed guidelines for handling the remains of COVID-19 decedents. Additional tips based on the lessons learned throughout handling remains of the COVID-19 decedents (i.e., typical difficulties that were encountered in the past and how they can be effectively addressed) would be helpful for the stakeholders who are directly involved in human remains handling and logistics. Due to COVID-19, there is a remarkably increasing amount of human remains. However, flight schedules continuously change or are cancelled at a short notice due to the COVID-19 disruptions, which caused uncertainties in the delivery of human remains from one country to another. Human remains handling and logistics have seriously suffered. In order to address this issue, human remains logistics firms may form a partnership or sign an agreement with airlines to provide a charter flight or a specific flight in case of original flight changes. This will facilitate human remains logistics throughout the COVID-19 pandemic and post-pandemic periods.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Govindan, K.; Mina, H.; Alavi, B. A decision support system for demand management in healthcare supply chains considering the epidemic outbreaks: A case study of coronavirus disease 2019 (COVID-19). Transp. Res. Part E Logist. Transp. Rev. 2020, 138, 101967. [Google Scholar] [CrossRef]
- Yuki, K.; Fujiogi, M.; Koutsogiannaki, S. COVID-19 pathophysiology: A review. Clin. Immun. 2020, 215, 108427. [Google Scholar] [CrossRef]
- Spinelli, A.; Pellino, G. COVID-19 pandemic: Perspectives on an unfolding crisis. Brit. J. Surg. 2020, 107, 785–787. [Google Scholar] [CrossRef]
- Lau, Y.Y.; Zhang, J.; Ng, A.K.Y.; Panahi, R. Implications of a pandemic outbreak risk: A discussion on China’s emergency logistics in the era of coronavirus disease 2019 (COVID-19). J. Int. Logist. Trade 2020, 18, 127–135. [Google Scholar] [CrossRef]
- Van Bavel, J.J.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 4 June 2021).
- Xie, K.; Liang, B.; Dulebenets, M.A.; Mei, Y. The impact of risk perception on social distancing during the COVID-19 pandemic in China. Int. J. Environ. Res. Public Health 2020, 17, 6256. [Google Scholar] [CrossRef]
- Khorram-Manesh, A.; Dulebenets, M.; Goniewicz, K. Implementing Public Health Strategies—The Need for Educational Initiatives: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 5888. [Google Scholar] [CrossRef]
- Moosavi, J.; Fathollahi-Fard, A.M.; Dulebenets, M.A. Supply chain disruption during the COVID-19 pandemic: Recognizing potential disruption management strategies. Int. J. Disaster Risk Reduct. 2022, 75, 102983. [Google Scholar] [CrossRef]
- Tang, Y.M.; Ng, G.W.Y.; Chia, N.H.; So, E.H.K.; Wu, C.H.; Ip, W.H. Application of virtual reality (VR) technology for medical practitioners in type and screen (T&S) training. J. Comput. Assist. Learn. 2021, 37, 359–369. [Google Scholar]
- Osorio-Saez, E.M.; Eryilmaz, N.; Sandoval-Hernandez, A.; Lau, Y.Y.; Barahona, E.; Bhatti, A.A.; Ofoe, G.C.; Ordóñez, L.A.; Ochoa, A.A.; Pizarro, R.Á. Survey data on the impact of COVID-19 on parental engagement across 23 countries. Data Brief 2021, 35, 106813. [Google Scholar] [CrossRef]
- United Nations. What Is the Coronavirus Disease (COVID-19)? Available online: https://www.un.org/en/civil-society/page/coronavirus-disease-covid-19 (accessed on 5 June 2021).
- Scala, B.; Lindsay, C.F. Supply chain resilience during pandemic distruption: Evidence from healthcare. Supply Chain Manag. Int. J. 2021, 26, 672–688. [Google Scholar] [CrossRef]
- Sibevei, A.; Azar, A.; Zandieh, M.; Khalili, S.M.; Yazdani, M. Developing a Risk Reduction Support System for Health System in Iran: A Case Study in Blood Supply Chain Management. Int. J. Environ. Res. Public Health 2022, 19, 2139. [Google Scholar] [CrossRef]
- Abdolazimi, O.; Shishebori, D.; Shakhsi-Niaei, M. Development of sustainable and resilient healthcare and non-cold pharmaceutical distribution supply chain for COVID-19 pandemic: A case study. Int. J. Logist. Manag. 2022. [CrossRef]
- Marroquín, B.; Vine, V.; Morgan, R. Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Res. 2020, 293, 113419. [Google Scholar] [CrossRef]
- Mathur, B.; Gupta, S.; Meena, M.L.; Dangayach, G. Healthcare supply chain management: Literature review and some issues. J. Adv. Manag. Res. 2018, 15, 265–287. [Google Scholar] [CrossRef]
- Goodarzian, F.; Ghasemi, P.; Gunasekaren, A.; Taleizadeh, A.A.; Abraham, A. A sustainable-resilience healthcare network for handling COVID-19 pandemic. Ann. Oper. Res. 2021, 312, 761–825. [Google Scholar] [CrossRef] [PubMed]
- Jahangiri, S.; Chobar, A.P.; Ghasemi, P.; Abolghasemian, M. Simulation-based Optimization: Analysis of the Emergency Department Resources under COVID-19 Conditions. Int. J. Ind. Syst. Eng. 2021, 1. [Google Scholar] [CrossRef]
- Gagliano, A.; Villani, P.G.; Co’, F.M.; Manelli, A.; Paglia, S.; Bisagni, P.A.G.; Perotti, G.; Storti, E.; Lombardo, M. COVID-19 Epidemic in the Middle Province of Northern Italy: Impact, Logistics, and Strategy in the First Line Hospital. Disaster Med. Public Health Prep. 2020, 14, 372–376. [Google Scholar] [CrossRef]
- Golec, A.; Karadeniz, G. Performance analysis of healthcare supply chain management with competency-based operation evaluation. Comput. Indust. Eng. 2020, 146, 106546. [Google Scholar] [CrossRef]
- Bartlett, L.; Vavrus, F. Comparative case studies: An innovative approach. Nord. J. Comp. Int. Educ. 2017, 1, 5–17. [Google Scholar] [CrossRef]
- Di Vaio, A.; Varriale, L.; Alvino, F. Key performance indicators for developing environmentally sustainable and energy efficient ports: Evidence from Italy. Energy Policy 2018, 122, 229–240. [Google Scholar] [CrossRef]
- Alam, M.K. Qualitative research in organizations and management. Qual. Res. Organ. Manag. 2021, 16, 1–31. [Google Scholar]
- Hong Kong—the Facts. Available online: https://www.gov.hk/en/about/abouthk/facts.htm (accessed on 10 August 2022).
- Department of Health. Health Facts of Hong Kong; Department of Health: Hong Kong, China, 2019. [Google Scholar]
- Phua, J.; Mohammad, F.; Atul, K.; Ike, R.; Khamsay, D.; Naranpurev, M.; Kyi, S.; Babu, S.; Madiha, H.; Emmanuel, P.J.; et al. Critical Care Bed Capacity in Asian Countries and Regions. Crit. Car Med. 2020, 48, 654–662. [Google Scholar] [CrossRef] [PubMed]
- Hospital Authority. HA Annual Report 2018–2019; Hospital Authority: Hong Kong, China, 2019. [Google Scholar]
- Hospital Authority. Hospital Authority Activates Emergency Response Level; Hospital Authority: Hong Kong, China, 2020. [Google Scholar]
- The Standard, Respirators Not Available to All Hospital Staff. Available online: https://www.thestandard.com.hk/breaking-news/section/4/143485/Respirators-not-available-to-all-hospital-staff (accessed on 10 March 2020).
- Ng, K.C. Coronavirus: New Mask Guidelines Rankle Union as Hospital Authority Urges Longer Use Amid Citywide Shortage. Available online: https://www.scmp.com/news/hong-kong/health-environment/article/3050543/coronavirus-new-mask-guidelines-rankle-union (accessed on 2 March 2021).
- Hospital Authority. Hospital Authority Communication Kit—Coronavirus Disease 2019 (COVID-19) Version 7.2; Hospital Authority: Hong Kong, China, 2021. [Google Scholar]
- Cathay Pacific Cargo. Available online: http://cargoclan.cathaypacificcargo.com/cathay-pacific-delivers-essential-protective-gear-to-hong-kongs-frontline-healthcare-workers/ (accessed on 6 June 2021).
- World Integrated Trade Solution (WITS). Available online: https://wits.worldbank.org/trade/comtrade/en/country/HKG/year/2019/tradeflow/Imports/partner/ALL/nomen/h5/product/280440 (accessed on 7 June 2021).
- Shirazi, H.; Kia, R.; Ghasemi, P. A stochastic bi-objective simulation-optimization model for plasma supply chain in case of COVID-19 outbreak. Appl. Soft Comp. 2021, 112, 107725. [Google Scholar] [CrossRef] [PubMed]
- The Government of Hong Kong Special Administrative Region, Press Releases (2020), Blood Donation Precautionary Measures in Response to COVID-19. Available online: https://www.info.gov.hk/gia/general/202002/29/P2020022900486.htm (accessed on 8 September 2020).
- The University of Hong Kong. What Disinfectants Can We Use to Fight Against the Coronavirus? 2021. Available online: https://www.med.hku.hk/en/covid-19/articles/suitable-disinfectants (accessed on 13 June 2021).
- HKSAR. Hong Kong Customs Urges Public to Stop Using One Type of Disinfectant Alcohol with Suspected False Description on Composition and Toxic Methanol. Available online: https://www.info.gov.hk/gia/general/202010/12/P2020101200681.htm (accessed on 13 June 2021).
- Centre for Health Protection. Guidelines on Prevention of Coronavirus Disease 2019 (COVID-19) for the General Public; Centre for Health Protection: Hong Kong, China, 2021. [Google Scholar]
- EPD. Available online: https://www.epd.gov.hk/epd/tc_chi/top.html (accessed on 9 January 2021).
- SCMP. Coronavirus: Sports Institute Sprays Hong Kong—Invented Disinfectant Across Entire Facility to Protect Against COVID-19. Available online: https://www.scmp.com/sport/hong-kong/article/3081610/coronavirus-sports-institute-sprays-hong-kong-invented-disinfectant (accessed on 13 June 2021).
- Center for Health Protection. Precautions for Handling and Disposal of Dead Bodies, 10th ed.; Food and Environmental Hygiene Department: Hong Kong, China, 2022. [Google Scholar]
- Hospital Authority. Precautions for Handling and Disposal of Dead Bodies; Hospital Authority: Hong Kong, China, 2020. [Google Scholar]
- AHA. Fast Facts on U.S. Hospitals. 2021. Available online: https://www.aha.org/statistics/fast-facts-us-hospitals (accessed on 27 June 2021).
- CDC. Recommended Guidance for Extended Use and Limited Reuse of N95 Filtering Facepiece Respirators in Healthcare Settings. Available online: https://www.cdc.gov/niosh/topics/hcwcontrols/recommendedguidanceextuse.html (accessed on 21 April 2020).
- FDA. Emergency Use Authorizations. Available online: https://www.fda.gov/medical-devices/emergency-situations-medical-devices/emergency-use-authorizations (accessed on 21 April 2020).
- CDC. Strategies for Optimizing the Supply of N95 Respirators. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html#conventional (accessed on 21 April 2020).
- U.S. Department of Health and Human Services. About the Strategic National Stockpile. Available online: https://www.phe.gov/about/sns/Pages/about.aspx (accessed on 21 April 2020).
- AHRMM. AHRMM Recommendations on COVID-19 for Health Care Supply Chain. Available online: https://www.ahrmm.org/ahrmm-covid-19 (accessed on 21 April 2020).
- AABB. AABB’s Coronavirus Resources. Available online: http://www.aabb.org/advocacy/regulatorygovernment/Pages/AABB-Coronavirus-Resources.aspx (accessed on 22 April 2020).
- EPA. List N: Disinfectants for Use against SARS-CoV-2. Available online: https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2, (accessed on 21 April 2020).
- CDC. Cleaning and Disinfecting Your Home. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/disinfecting-your-home.html (accessed on 21 April 2020).
- CDC. Collection and Submission of Postmortem Specimens from Deceased Persons with Known or Suspected COVID-19 (Interim Guidance). Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-postmortem-specimens.html (accessed on 22 April 2020).
- LDH. COVID-19: Funerals and Handling of Bodies. Available online: http://ldh.la.gov/assets/oph/Coronavirus/resources/COVID-19_FuneralGuidance.pdf (accessed on 21 April 2020).
- Sages. N95 Mask Re-use Strategies. Available online: https://www.sages.org/n-95-re-use-instructions/ (accessed on 14 June 2021).
- Chua, M.H.; Cheng, W.; Goh, S.S.; Kong, J.; Li, B.; Lim, J.Y.C.; Mao, L.; Wang, S.; Xue, K.; Yang, L.; et al. Face Masks in the New COVID-19 Normal: Materials, Testing, and Perspectives. Research 2020, 2020, 7286735. [Google Scholar] [CrossRef]
- Lucero-Prisno, D.E.; Essar, M.Y.; Ahmadi, A.; Lin, X.; Adebisi, Y.A. Conflict and COVID-19: A double burden for Afghanistan’s healthcare system. Confl. Health 2020, 14, 65–67. [Google Scholar] [CrossRef] [PubMed]
- Yahya, B.M.; Yahya, F.S.; Thannoun, R.G. COVID-19 prediction analysis using artificial intelligence procedures and GIS spatial analyst: A case study for Iraq. Appl. Geomat. 2021, 13, 481–491. [Google Scholar] [CrossRef]
- Pasha, J.; Dulebenets, M.A.; Fathollahi-Fard, A.M.; Tian, G.; Lau, Y.-Y.; Singh, P.; Liang, B. An integrated optimization method for tactical-level planning in liner shipping with heterogeneous ship fleet and environmental considerations. Adv. Eng. Inform. 2021, 48, 101299. [Google Scholar] [CrossRef]
- Theophilus, O.; Dulebenets, M.A.; Pasha, J.; Lau, Y.Y.; Fathollahi-Fard, A.M.; Mazaheri, A. Truck scheduling optimization at a cold-chain cross-docking terminal with product perishability considerations. Comput. Ind. Eng. 2021, 156, 107240. [Google Scholar] [CrossRef]
- Riahi, Y.; Saikouk, T.; Gunasekaran, A.; Badraoui, I. Artifical intelligence applications in supply chain: A descriptive bibliometic analysis and future research directions. Exp. Syst. Appl. 2021, 173, 114702. [Google Scholar] [CrossRef]
- Kim, H.; Lee, C. Relationships among Healthcare Digitalization, Social Capital, and Supply Chain Performance in the Healthcare Manufacturing Industry. Int. J. Environ. Res. Public Health 2021, 18, 1417. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; See, K.C. Artifical intelligence for COVID-19: Rapid Review. J. Med. Int. Res. 2020, 22, e21476. [Google Scholar]
- Mashamba-Thompason, T.P.; Crayton, E.D. Blockchain and aritifical intelligence technology for novel coronavirus disease 2019 self-testing. Diagnostics 2020, 10, 198. [Google Scholar] [CrossRef]
- Shamout, F.E.; Shen, Y.; Wu, N.; Geras, K.J. An artificial intelligence system for predicting the deterioration of COVID-19 patients in the emergency department. Digit Med. 2021, 80, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.; Ko, H.; Kang, W.S.; Kim, K.W.; Lee, H.; Park, C.; Song, H.; Choi, T.; Seo, J.H.; Lee, J. Prediction and feature importance analysis for severity of COVID-19 in South Korea using artificial intelligence: Model Development and Validation. J. Med. Int. Res. 2021, 23, e27060. [Google Scholar] [CrossRef]
- Tang, Y.M.; Chau, K.Y.; Li, W.Q.; Wan, T.W. Forecasting economic recession through share price in the logistics industry with Artificial Intelligence (AI). Computation 2020, 8, 70. [Google Scholar] [CrossRef]
- Perpetuini, D.; Filippini, C.; Cardone, D.; Merla, A. An overview of thermal infrared imaging-based screenings during pandemic emergencies. Int. J. Environ. Res. Pub. Health 2021, 18, 3286. [Google Scholar] [CrossRef]
- Anitha Kumari, K.; Purusothaman, P.; Dharani, D.; Padmashani, R. COVID-19: AI-Enabled Social Distancing Detector Using CNN. In Computational Intelligence Techniques for Combating COVID-19; Kautish, S., Peng, S.L., Obaid, A.J., Eds.; Springer: Cham, Switzerland, 2021. [Google Scholar]
- Saponara, S.; Elhanashi, A.; Gagliardi, A. Implementing a real-time, AI-based, people detection and social distancing measuring system for Covid-19. J. Real-Time Image Process. 2021, 18, 1937–1947. [Google Scholar] [CrossRef]
- Yang, Z.; Zeng, Z.; Wang, K.; Wong, S.-S.; Liang, W.; Zanin, M.; Liu, P.; Cao, X.; Gao, Z.; Mai, Z.; et al. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. J. Thorac. Dis. 2020, 12, 165–174. [Google Scholar] [CrossRef]
- Fong, K.N.K.; Tang, Y.M.; Sie, K.; Yu, A.K.H.; Lo, C.C.W.; Ma, Y.W.T. Task-specific virtual reality training on hemiparetic upper extremity in patients with stroke. Virtual Real. 2021, 26, 453–464. [Google Scholar] [CrossRef]
- Wahl, B.; Cossy-Gantner, A.; Germann, S.; Schwalbe, N.R. Artificial intelligence (AI) and global health: How can AI contribute to health in resource-poor settings? BMJ Glob. Health 2018, 3, e000798. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.M.; Chen, P.C.; Law, K.M.; Wu, C.; Lau, Y.-Y.; Guan, J.; He, D.; Ho, G. Comparative analysis of Student’s live online learning readiness during the coronavirus (COVID-19) pandemic in the higher education sector. Comput. Educ. 2021, 168, 104211. [Google Scholar] [CrossRef] [PubMed]
- Lau, Y.-Y.; Tang, Y.M.; Chau, K.Y.; Vyas, L.; Sandoval-Hernandez, A.; Wong, S. COVID-19 Crisis: Exploring Community of Inquiry in Online Learning for Sub-Degree Students. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.; Yeung, J.K.W.; Lau, Y.Y.; So, J. Technical sustainability of cloud-based blockchain integrated with machine learning for supply chain management. Sustainability 2021, 13, 8270. [Google Scholar] [CrossRef]
| Attribute\Country | Hong Kong | United States |
|---|---|---|
| Use of respirators |
|
|
| Life-saving medical supplies |
|
|
| Blood supply chains |
|
|
| Disinfectants |
|
|
| Human remains handling and logistics |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lau, Y.-Y.; Dulebenets, M.A.; Yip, H.-T.; Tang, Y.-M. Healthcare Supply Chain Management under COVID-19 Settings: The Existing Practices in Hong Kong and the United States. Healthcare 2022, 10, 1549. https://doi.org/10.3390/healthcare10081549
Lau Y-Y, Dulebenets MA, Yip H-T, Tang Y-M. Healthcare Supply Chain Management under COVID-19 Settings: The Existing Practices in Hong Kong and the United States. Healthcare. 2022; 10(8):1549. https://doi.org/10.3390/healthcare10081549
Chicago/Turabian StyleLau, Yui-Yip, Maxim A. Dulebenets, Ho-Tung Yip, and Yuk-Ming Tang. 2022. "Healthcare Supply Chain Management under COVID-19 Settings: The Existing Practices in Hong Kong and the United States" Healthcare 10, no. 8: 1549. https://doi.org/10.3390/healthcare10081549
APA StyleLau, Y.-Y., Dulebenets, M. A., Yip, H.-T., & Tang, Y.-M. (2022). Healthcare Supply Chain Management under COVID-19 Settings: The Existing Practices in Hong Kong and the United States. Healthcare, 10(8), 1549. https://doi.org/10.3390/healthcare10081549









