Potential Maneuvers for Providing Optimal Tidal Volume Using the One-Handed EC Technique
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Setting
2.3. Ethical Consideration and Data Collection
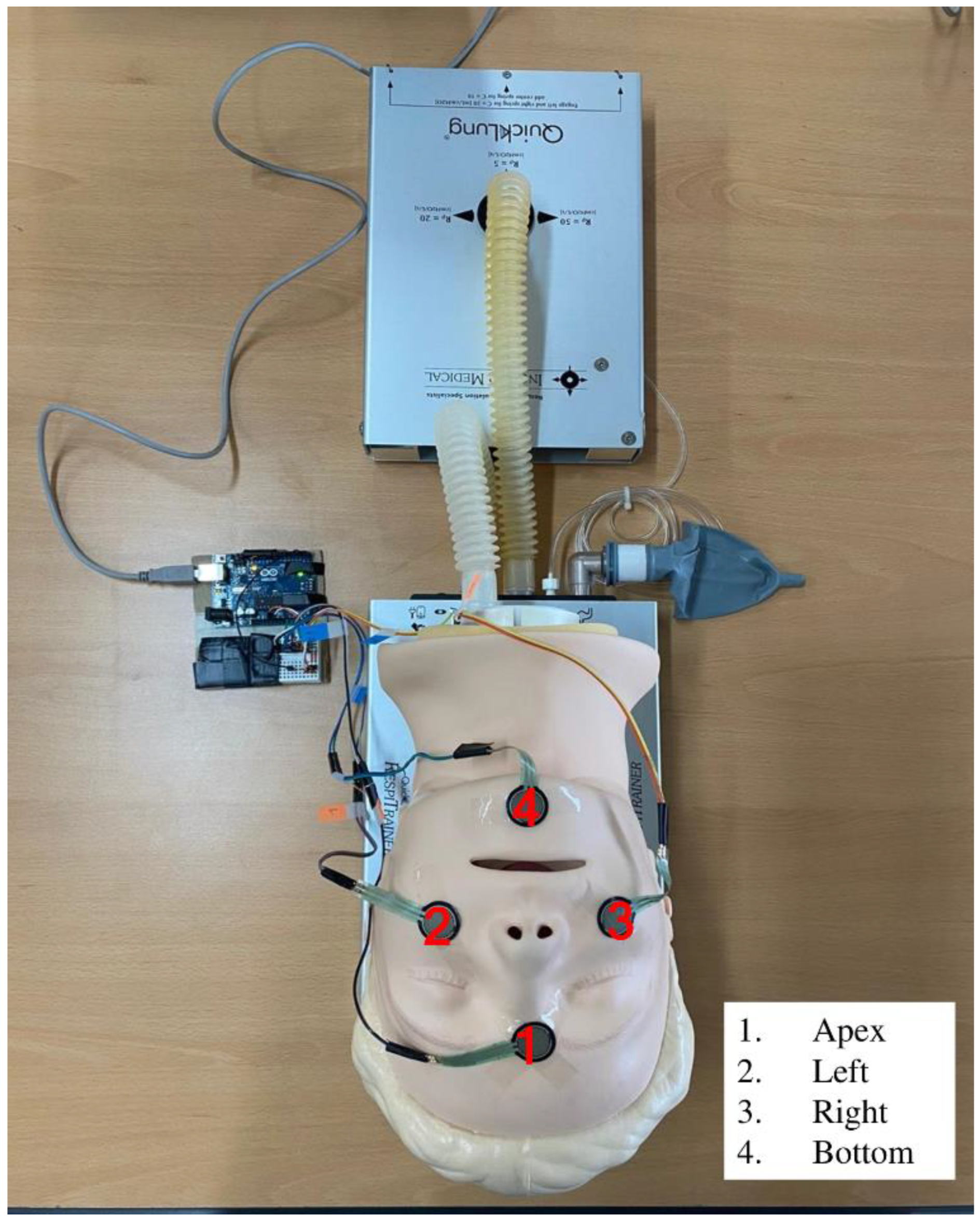
2.4. Experimental Setting and Variables
2.5. Tidal Volume and Peak Pressure
2.6. Four-Spot Adhesion Strength
2.7. Data Analyses
3. Results
3.1. General Characteristics
3.2. Correlation between Vt, PP, and 4-Spot Adhesion Strengths
3.3. Factors Influencing Vt
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Hasegawa, K.; Hiraide, A.; Chang, Y.; Brown, D.F.M. Association of Prehospital Advanced Airway Management with Neurologic Outcome and Survival in Patients with Out-of-Hospital Cardiac Arrest. JAMA 2013, 309, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Liang, H.; Li, J.; Qiu, S.; He, Z.; Li, J.; Cao, Z.; Yan, P.; Liang, Q.; Zeng, L.; et al. Comparing the Efficacy of Bag-Valve Mask, Endotracheal Intubation, and Laryngeal Mask Airway for Subjects with Out-of-Hospital Cardiac Arrest: An Indirect Meta-analysis. Ann. Transl. Med. 2019, 7, 257. [Google Scholar] [CrossRef] [PubMed]
- Young, P.; Pilcher, J.; Patel, M.; Cameron, L.; Braithwaite, I.; Weatherall, M.; Beasley, R. Delivery of Titrated Oxygen via a Self-Inflating Resuscitation Bag. Resuscitation 2013, 84, 391–394. [Google Scholar] [CrossRef] [PubMed]
- Dreyfuss, D.; Saumon, G. Ventilator-Induced Lung Injury: Lessons from Experimental Studies. Am. J. Respir. Crit. Care Med. 1998, 157, 294–323. [Google Scholar] [CrossRef]
- Aufderheide, T.P.; Lurie, K.G. Death by Hyperventilation: A Common and Life-Threatening Problem During Cardiopulmonary Resuscitation. Crit. Care Med. 2004, 32, S345–S351. [Google Scholar] [CrossRef]
- Richard, J.C.; Maggiore, S.M.; Jonson, B.; Mancebo, J.; Lemaire, F.; Brochard, L. Influence of Tidal Volume on Alveolar Recruitment: Respective Role of PEEP and a Recruitment Maneuver. Am. J. Respir Crit. Care Med. 2001, 163, 1609–1613. [Google Scholar] [CrossRef]
- Potchileev, I.; Doroshenko, M.; Mohammed, A.N. Positive Pressure Ventilation; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK560916/ (accessed on 22 May 2022).
- Keszler, M. Volume-Targeted Ventilation. J. Perinatol. 2005, 25 (Suppl. 2), S19–S22. [Google Scholar] [CrossRef][Green Version]
- Otten, D.; Liao, M.M.; Wolken, R.; Douglas, I.S.; Mishra, R.; Kao, A.; Barrett, W.; Drasler, E.; Byyny, R.L.; Haukoos, J.S. Comparison of Bag-Valve-Mask Hand-Sealing Techniques in a Simulated Model. Ann. Emerg. Med. 2014, 63, 6–12.e3. [Google Scholar] [CrossRef]
- Lee, N.-J.; Baek, M.-L. Comparison of Ventilation Effects by Mask-Sealing Methods During Bag-Valve-Mask Ventilation. Korean Soc. Emerg. Med. Serv. 2018, 22, 73–82. [Google Scholar] [CrossRef]
- Strzelecki, C.; Shelton, C.L.; Cunningham, J.; Dean, C.; Naz-Thomas, S.; Stocking, K.; Dobson, A. A Randomised Controlled Trial of Bag–Valve–Mask Teaching Techniques. Clin. Teach. 2020, 17, 41–46. [Google Scholar] [CrossRef]
- Khoury, A.; Sall, F.S.; De Luca, A.; Pugin, A.; Pili-Floury, S.; Pazart, L.; Capellier, G. Evaluation of Bag-Valve-Mask Ventilation in Manikin Studies: What Are the Current Limitations? BioMed Res. Int. 2016, 2016, 4521767. [Google Scholar] [CrossRef] [PubMed]
- Kroll, M.; Das, J.; Siegler, J. Can Altering Grip Technique and Bag Size Optimize Volume Delivered with Bag-Valve-Mask by Emergency Medical Service Providers? Prehosp. Emerg. Care 2019, 23, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Ortega, R.; Mehio, A.K.; Woo, A.; Hafez, D.H. Videos in Clinical Medicine. Positive-Pressure Ventilation with a Face Mask and a Bag-Valve Device. N. Engl. J. Med. 2007, 357, e4. [Google Scholar] [CrossRef] [PubMed]
- Uhm, T.-H.; Jung, H.-K. Comparison of Cardiopulmonary Resuscitation Quality Using the Over-the-Head and Lateral Conventional Positions with a Bag-Valve-Mask Device Performed by a Single Rescuer: A Manikin Study. Korean J. Emerg. Med. Serv. 2016, 20, 7–15. [Google Scholar] [CrossRef]
- Oh, J.H. Effects of Bed Height on the Performance of Endotracheal Intubation and Bag Mask Ventilation. J. Intesive Care Emerg. Med. 2016, 12, 47–51. [Google Scholar] [CrossRef][Green Version]
- Jo, S.-M.; Jung, H.-K. Differentiation of Tidal Volume & Mean Airway Pressure with Different Bag-Valve-Mask Compression Depth and Compression Rate. Korean J. Emerg. Med. Serv. 2012, 16, 67–74. [Google Scholar]
- Shin, S.-Y.; Lee, J.-G.; Roh, S.-G. Comparative Analysis of Tidal Volume and Airway Pressure with a Bag-Valve Mask Using RespiTrainer. Fire Sci. Eng. 2014, 28, 76–81. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Umesh, G.; Gotur, G.V.; Rao, A.K.; Joseph, T.T. EO Technique Provides Better Mask Seal than the EC Clamp Technique during Single Handed Mask Holding by Novices in Anaesthetised and Paralysed Patients. Indian J. Anaesth. 2018, 62, 780–785. [Google Scholar] [CrossRef]
- Lee, H.Y.; Jeung, K.W.; Lee, B.K.; Lee, S.J.; Jung, Y.H.; Lee, G.S.; Min, Y.I.; Heo, T. The Performances of Standard and ResMed Masks During Bag–Valve–Mask Ventilation. Prehosp. Emerg. Care 2013, 17, 235–240. [Google Scholar] [CrossRef]
- National Health Insurance Service. National Health Screening Statistics; National Health Insurance Service: Seoul, Korea, 2022. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=DT_35007_N132 (accessed on 9 February 2022).
- Cassone, M.; Cocciolone, A.; Melnychuk, E. EM Resident. Your First Shift in the Unit: Demystifying Ventilator Alarms. 2019. Available online: https://www.emra.org/emresident/article/demystifying_ventilator_alarms/ (accessed on 9 February 2022).
- Uhm, D.; Kim, A. Tidal Volume according to the 4-Point Sealing Forces of a Bag-Valve-Mask: An Adult Respiratory Arrest Simulator-Based Prospective, Descriptive Study. BMC Emerg. Med. 2021, 21, 57. [Google Scholar] [CrossRef]
- Joffe, A.M.; Hetzel, S.; Liew, E.C. A Two-Handed Jaw-Thrust Technique Is Superior to the One-Handed “EC-Clamp” Technique for Mask Ventilation in the Apneic Unconscious Person. Anesthesiology 2010, 113, 873–879. [Google Scholar] [CrossRef] [PubMed]
| N (%) | ||
|---|---|---|
| Sex | Male | 41 (46.1) |
| Female | 48 (53.9) | |
| School year | Sophomore | 28 (31.5) |
| Junior | 31 (34.8) | |
| Senior | 30 (33.7) | |
| Hand holding the mask | Left | 82 (92.1) |
| Right | 7 (7.9) | |
| N | (%) | Mean (±SD) | Measuring Range | |||
|---|---|---|---|---|---|---|
| General characteristics as the control variables | Sex | Male | 764 | (50.1) | ||
| Female | 760 | (49.9) | ||||
| School year | Sophomore | 519 | (34.1) | |||
| Junior | 552 | (36.2) | ||||
| Senior | 453 | (29.7) | ||||
| Hand holding the mask | Left | 1411 | (92.6) | |||
| Right | 113 | (7.4) | ||||
| PP (cmH2O) | 15.56 (±5.62) | 5–200 cmH2O/L/s | ||||
| Experimental variables | 4-spot adhesion strength -ln(apex) (N) | 0.03 (±0.07) | 0–100 N | |||
| 4-spot adhesion strength- ln(bottom) (N) | 0.17 (±0.29) | 0–100 N | ||||
| 4-spot adhesion strength- left (N) | 0.62 (±0.49) | 0–100 N | ||||
| 4-spot adhesion strength- right (N) | 0.69 (±0.63) | 0–100 N | ||||
| Dependent variable | Tidal Volume (mL) | 415.98 (±102.4) | 0–1200 mL | |||
| r | (p) | |
|---|---|---|
| Tidal Volume | 1 | |
| PP | 0.744 *** | (<0.001) |
| ln(apex) | 0.083 ** | (0.001) |
| ln(bottom) | −0.057 * | (0.025) |
| Left | 0.280 *** | (<0.001) |
| Right | 0.227 *** | (<0.001) |
| B | S.E. | β | t | p | |
|---|---|---|---|---|---|
| (constant) | 199.804 | 6.053 | 33.011 *** | <0.001 | |
| ln(apex) | −32.060 | 25.522 | −0.021 | −1.256 | 0.209 |
| ln(bottom) | −65.440 | 5.781 | −0.186 | −11.320 *** | <0.001 |
| Left | 35.766 | 3.576 | 0.172 | 10.002 *** | <0.001 |
| Right | −20.156 | 3.281 | −0.123 | −6.144 *** | <0.001 |
| PP | 14.519 | 0.315 | 0.797 | 46.084 *** | <0.001 |
| Sex (male = ref.) | |||||
| Female | −27.241 | 3.430 | −0.133 | −7.942 *** | <0.001 |
| School year (sophomore = ref.) | |||||
| Junior | 22.574 | 3.918 | 0.106 | 5.761 *** | <0.001 |
| Senior | −1.082 | 4.387 | −0.005 | −0.247 | 0.805 |
| Hand holding the mask (left = ref.) | |||||
| Right | −4.643 | 6.205 | −0.012 | −0.748 | 0.454 |
| F = 302.865 ***, R2(adjR2) = 0.643 (0.641) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uhm, D.; Kim, A. Potential Maneuvers for Providing Optimal Tidal Volume Using the One-Handed EC Technique. Healthcare 2022, 10, 1365. https://doi.org/10.3390/healthcare10081365
Uhm D, Kim A. Potential Maneuvers for Providing Optimal Tidal Volume Using the One-Handed EC Technique. Healthcare. 2022; 10(8):1365. https://doi.org/10.3390/healthcare10081365
Chicago/Turabian StyleUhm, Dongchoon, and Ajung Kim. 2022. "Potential Maneuvers for Providing Optimal Tidal Volume Using the One-Handed EC Technique" Healthcare 10, no. 8: 1365. https://doi.org/10.3390/healthcare10081365
APA StyleUhm, D., & Kim, A. (2022). Potential Maneuvers for Providing Optimal Tidal Volume Using the One-Handed EC Technique. Healthcare, 10(8), 1365. https://doi.org/10.3390/healthcare10081365






