Priority Criteria for Community-Based Care Resource Allocation for Health Equity: Socioeconomic Status and Demographic Characteristics in the Multicriteria Decision-Making Method
Abstract
:1. Introduction
1.1. Active Aging, SDG 10, and Health Equity
1.2. Multicriteria Decision Making (MCDM): SES, Demographic Characteristics, and Community Healthcare Equity
2. Materials and Methods
2.1. Design and Setting
2.2. Modified Delphi Method
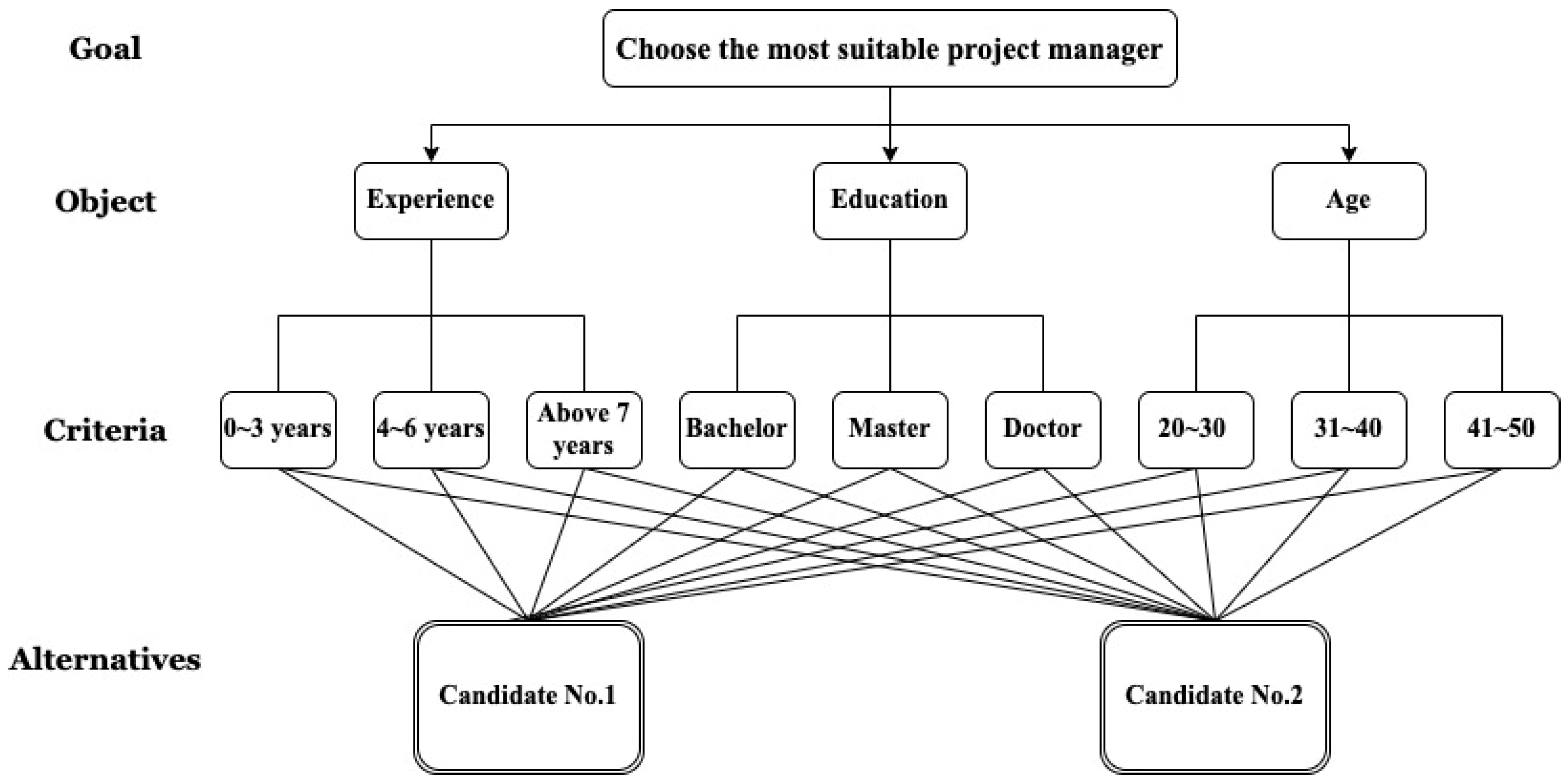
2.3. AHP Method
2.4. Statistical Hypothesis Test
3. Results
3.1. Participant Characteristics
3.2. Evaluation of Community-Based Resource Allocation Criteria by Geometric Mean
3.3. Evaluation of Community-Based Resource Allocation Criteria by Ranking
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Active Ageing: A Policy Framework. Available online: https://apps.who.int/iris/handle/10665/67215 (accessed on 1 December 2021).
- Phelan, E.A.; Anderson, L.A.; Lacroix, A.Z.; Larson, E.B. Older adults’ views of “successful aging”—How do they compare with researchers’ definitions? J. Am. Geriatr. Soc. 2004, 52, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Ballesteros, R.; Olmos, R.; Santacreu, M.; Bustillos, A.; Molina, M.A. The role of perceived discrimination on active aging. Arch. Gerontol. Geriatr. 2017, 71, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Jensen, P.H.; Skjott-Larsen, J. Theoretical challenges and social inequalities in active ageing. Int. J. Environ. Res. Public Health 2021, 18, 9156. [Google Scholar] [CrossRef] [PubMed]
- Paz, A.; Doron, I.; Tur-Sinai, A. Gender, aging, and the economics of “active aging”: Setting a new research agenda. J. Women Aging 2018, 30, 184–203. [Google Scholar] [CrossRef] [PubMed]
- Barslund, M.; Von Werder, M.; Zaidi, A. Inequality in active ageing: Evidence from a new individual-level index for European countries. Ageing Soc. 2019, 39, 541–567. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare (Taiwan). Long-Term Care 2.0. Available online: https://1966.gov.tw/LTC/cp-3636-38462-201.html (accessed on 1 January 2022).
- Ministry of Health and Welfare (Taiwan). 2022 Taiwan Community Care Golden Stations Award. Available online: https://www.mohw.gov.tw/cp-5023-64558-1.html (accessed on 1 January 2022).
- Tseng, M.-H.; Wu, H.-C. The geographic accessibility and inequality of community-based elderly learning resources: A remodeling assessment, 2009~2017. Educ. Gerontol. 2018, 44, 226–246. [Google Scholar] [CrossRef]
- Wu, H.-C.; Tseng, M.-H. Evaluating disparities in elderly community care resources: Using a geographic accessibility and inequality index. Int. J. Environ. Res. Public Health 2018, 15, 1353. [Google Scholar] [CrossRef] [Green Version]
- Tseng, M.-H.; Wu, H.-C. Accessibility assessment of community care resources using maximum-equity optimization of supply capacity allocation. Int. J. Environ. Res. Public Health 2021, 18, 1153. [Google Scholar] [CrossRef]
- Tseng, M.-H.; Wu, H.-C. Integrating socioeconomic status and spatial factors to improve the accessibility of community care resources using maximum-equity optimization of supply capacity allocation. Int. J. Environ. Res. Public Health 2021, 18, 5437. [Google Scholar] [CrossRef]
- Tseng, M.-H.; Wu, H.-C.; Lin, C.-C.; Hung, S.-C. Measuring the community geographic accessibility of rehabilitation resource. In Proceedings of the 2018 IEEE Global Conference on Consumer Electronics (GCCE), Nara, Japan, 9–12 October 2018; pp. 320–324. [Google Scholar]
- Wu, H.-C.; Tseng, M.-H.; Lin, C.-C. Assessment on distributional fairness of physical rehabilitation resource allocation: Geographic accessibility analysis integrating google rating mechanism. Int. J. Environ. Res. Public Health 2020, 17, 7576. [Google Scholar] [CrossRef]
- World Health Organisation. Social Determinants of Health. Available online: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_3 (accessed on 1 January 2022).
- World Health Organization. About the Health Equity Monitor. Available online: https://www.who.int/data/gho/health-equity/about (accessed on 20 January 2021).
- Culyer, A.J.; Wagstaff, A. Equity and equality in health and health care. J. Health Econ. 1993, 12, 431–457. [Google Scholar] [CrossRef]
- Braveman, P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014, 129 (Suppl. S2), 5–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marsh, M.T.; Schilling, D.A. Equity measurement in facility location analysis: A review and framework. Eur. J. Oper. Res. 1994, 74, 1–17. [Google Scholar] [CrossRef]
- Mooney, G. What does equity in health mean? World Health Stat. Q. 1987, 40, 296–303. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. Communities in Action: Pathways to Health Equity; The National Academies Press: Washington, DC, USA, 2017; 582p. [Google Scholar] [CrossRef]
- Wang, F. Why public health needs GIS: A methodological overview. Ann. GIS 2020, 26, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Rowe, J.W.; Kahn, R.L. Successful aging. Gerontologist 1997, 37, 433–440. [Google Scholar] [CrossRef]
- Wiles, J.L.; Leibing, A.; Guberman, N.; Reeve, J.; Allen, R.E.S. The meaning of “Aging in Place” to older people. Gerontologist 2012, 52, 357–366. [Google Scholar] [CrossRef]
- United Nations. Sustainable Development Goals: Goal 10 Reduce Inequality within and among Countries. Available online: https://sdgs.un.org/goals/goal10 (accessed on 3 November 2021).
- Guindo, L.A.; Wagner, M.; Baltussen, R.; Rindress, D.; van Til, J.; Kind, P.; Goetghebeur, M.M. From efficacy to equity: Literature review of decision criteria for resource allocation and healthcare decisionmaking. Cost Eff. Resour. Alloc. 2012, 10, 9. [Google Scholar] [CrossRef] [Green Version]
- Dukhanin, V.; Searle, A.; Zwerling, A.; Dowdy, D.W.; Taylor, H.A.; Merritt, M.W. Integrating social justice concerns into economic evaluation for healthcare and public health: A systematic review. Soc. Sci. Med. 2018, 198, 27–35. [Google Scholar] [CrossRef]
- Lane, H.; Sarkies, M.; Martin, J.; Haines, T. Equity in healthcare resource allocation decision making: A systematic review. Soc. Sci. Med. 2017, 175, 11–27. [Google Scholar] [CrossRef]
- Gordon-Hecker, T.; Choshen-Hillel, S.; Shalvi, S.; Bereby-Meyer, Y. Resource allocation decisions: When Do we sacrifice efficiency in the name of equity? In Interdisciplinary Perspectives on Fairness, Equity, and Justice; Li, M., Tracer, D.P., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 93–105. [Google Scholar] [CrossRef]
- Eichler, H.-G.; Kong, S.X.; Gerth, W.C.; Mavros, P.; Jönsson, B. Use of cost-effectiveness analysis in health-care resource allocation decision-making: How are cost-effectiveness thresholds expected to emerge? Value Health 2004, 7, 518–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mueller, C.W.; Parcel, T.L. Measures of socioeconomic status: Alternatives and recommendations. Child Dev. 1981, 52, 13–30. [Google Scholar] [CrossRef]
- Liberatos, P.; Link, B.G.; Kelsey, J.L. The measurement of social class in epidemiology. Epidemiol. Rev. 1988, 10, 87–121. [Google Scholar] [CrossRef]
- Ross, C.E.; Wu, C.-L. The Links Between Education and Health. Am. Sociol. Rev. 1995, 60, 719–745. [Google Scholar] [CrossRef]
- Marmot, M.; Ryff, C.D.; Bumpass, L.L.; Shipley, M.; Marks, N.F. Social inequalities in health: Next questions and converging evidence. Soc. Sci. Med. 1997, 44, 901–910. [Google Scholar] [CrossRef]
- Smith, J.P.; Kington, R. Demographic and economic correlates of health in old age. Demography 1997, 34, 159–170. [Google Scholar] [CrossRef]
- Winkleby, M.A.; Jatulis, D.E.; Frank, E.; Fortmann, S.P. Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. Am. J. Public Health 1992, 82, 816–820. [Google Scholar] [CrossRef] [Green Version]
- World Health Organisation. 9th Global Conference on Health Promotion. Available online: https://www.who.int/healthpromotion/conferences/9gchp/about/en/ (accessed on 1 January 2022).
- Miech, R.A.; Hauser, R.M. Socioeconomic status and health at midlife: A comparison of educational attainment with occupation-based indicators. Ann. Epidemiol. 2001, 11, 75–84. [Google Scholar] [CrossRef]
- Shavers, V.L. Measurement of socioeconomic status in health disparities research. J. Natl. Med. Assoc. 2007, 99, 1013–1023. [Google Scholar]
- House, J.S.; Kessler, R.C.; Herzog, A.R. Age, socioeconomic status, and health. Milbank Q. 1990, 68, 383–411. [Google Scholar] [CrossRef] [Green Version]
- Hayes, S.C.; Villatte, M.; Levin, M.; Hildebrandt, M. Open, aware, and active: Contextual approaches as an emerging trend in the behavioral and cognitive therapies. Annu. Rev. Clin. Psychol. 2011, 7, 141–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Triantaphyllou, E. Multi-criteria decision making methods. In Multi-Criteria Decision Making Methods: A Comparative Study; Springer: Boston, MA, USA, 2000; pp. 5–21. [Google Scholar] [CrossRef]
- Velasquez, M.; Hester, P.T. An analysis of multi-criteria decision making methods. Int. J. Oper. Res. 2013, 10, 56–66. [Google Scholar]
- Ho, W.; Xu, X.; Dey, P.K. Multi-criteria decision making approaches for supplier evaluation and selection: A literature review. Eur. J. Oper. Res. 2010, 202, 16–24. [Google Scholar] [CrossRef]
- Gavade, R.K. Multi-criteria decision making: An overview of different selection problems and methods. Int. J. Comput. Sci. Inf. Technol. 2014, 5, 5643–5646. [Google Scholar]
- Minstry of Health and Welfare. Introduction of Community Care Stations. Available online: https://ccare.sfaa.gov.tw/home/other/about (accessed on 1 June 2020).
- Dalkey, N.; Helmer, O. An experimental application of the DELPHI method to the use of experts. Manag. Sci. 1963, 9, 458–467. [Google Scholar] [CrossRef]
- Murry, J.W., Jr.; Hammons, J.O. Delphi: A versatile methodology for conducting qualitative research. Rev. High. Educ. 1995, 18, 423–436. [Google Scholar] [CrossRef]
- Linstone, H.A.; Turoff, M. The Delphi Method; Addison-Wesley Publishing Company: Boston, MA, USA, 1975. [Google Scholar]
- Hsu, C.-C.; Sandford, B.A. The Delphi technique: Making sense of consensus. Pract. Assess. Res. Eval. 2007, 12, 10. [Google Scholar]
- Dalkey, N. An experimental study of group opinion: The Delphi method. Futures 1969, 1, 408–426. [Google Scholar] [CrossRef]
- Adler, M.; Ziglio, E. (Eds.) Gazing into the Oracle: The Delphi Method and Its Application to Social Policy and Public Health; Jessica Kingsley Publishers: London, UK, 1996. [Google Scholar]
- Loo, R. The Delphi method: A powerful tool for strategic management. Polic. Int. J. 2002, 25, 762–769. [Google Scholar] [CrossRef]
- Dalkey, N. Delphi; The RAND Corporation: Santa Monica, CA, USA, 1967. [Google Scholar]
- Rowe, G.; Wright, G. The Delphi technique as a forecasting tool: Issues and analysis. Int. J. Forecast. 1999, 15, 353–375. [Google Scholar] [CrossRef]
- Gordon, T.J.; Helmer, O. Report on a Long-Range Forecasting Study; The Rand Corporation: Santa Monoca, CA, USA, 1964. [Google Scholar]
- Hasson, F.; Keeney, S. Enhancing rigour in the Delphi technique research. Technol. Forecast. Soc. Change 2011, 78, 1695–1704. [Google Scholar] [CrossRef]
- Hasson, F.; Keeney, S.; McKenna, H. Research guidelines for the Delphi survey technique. J. Adv. Nurs. 2000, 32, 1008–1015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saaty, T.L. How to make a decision: The analytic hierarchy process. Eur. J. Oper. Res. 1990, 48, 9–26. [Google Scholar] [CrossRef]
- Saaty, T.L. Decision making with the analytic hierarchy process. Int. J. Serv. Sci. 2008, 1, 83–98. [Google Scholar] [CrossRef] [Green Version]
- Creative Decisions Foundation. Super Decisions. Available online: https://www.superdecisions.com/ (accessed on 1 December 2021).
- Stoline, M.R. The status of multiple comparisons: Simultaneous estimation of all pairwise comparisons in one-way ANOVA designs. Am. Stat. 1981, 35, 134–141. [Google Scholar] [CrossRef]
- Park, H.M. Comparing Group Means: T-tests and One-Way ANOVA Using Stata, SAS, R, and SPSS. Available online: https://hdl.handle.net/2022/19735 (accessed on 1 December 2021).
- Kim, T.K. Understanding one-way ANOVA using conceptual figures. Korean J. Anesthesiol. 2017, 70, 22–26. [Google Scholar] [CrossRef] [Green Version]
- Moser, B.K.; Stevens, G.R. Homogeneity of variance in the two-sample means test. Am. Stat. 1992, 46, 19–21. [Google Scholar] [CrossRef]
- Cressie, N.A.C.; Whitford, H.J. How to use the two sample t-test. Biom. J. 1986, 28, 131–148. [Google Scholar] [CrossRef]
- Kim, T.K. T test as a parametric statistic. Korean J. Anesthesiol. 2015, 68, 540–546. [Google Scholar] [CrossRef] [Green Version]
- Chan, Y.; Walmsley, R.P. Learning and understanding the Kruskal-Wallis one-way analysis-of-variance-by-ranks test for differences among three or more independent groups. Phys. Ther. 1997, 77, 1755–1761. [Google Scholar] [CrossRef]
- Ostertagová, E.; Ostertag, O.; Kováč, J. Methodology and application of the Kruskal-Wallis test. Appl. Mech. Mater. 2014, 611, 115–120. [Google Scholar] [CrossRef]
- Hecke, T.V. Power study of anova versus Kruskal-Wallis test. J. Stat. Manag. Syst. 2012, 15, 241–247. [Google Scholar] [CrossRef]
- McKnight, P.E.; Najab, J. Mann-Whitney U Test. In The Corsini Encyclopedia of Psychology; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar] [CrossRef]
- Ruxton, G.D. The unequal variance t-test is an underused alternative to Student’s t-test and the Mann–Whitney U test. Behav. Ecol. 2006, 17, 688–690. [Google Scholar] [CrossRef]
- Nachar, N. The Mann-Whitney U: A test for assessing whether two independent samples come from the same distribution. Tutor. Quant. Methods Psychol. 2008, 4, 13–20. [Google Scholar] [CrossRef]
- Shimada, K.; Yamazaki, S.; Nakano, K.; Ngoma, A.M.; Takahashi, R.; Yasumura, S. Prevalence of social isolation in community-dwelling elderly by differences in household composition and related factors: From a social network perspective in urban Japan. J. Aging Health 2014, 26, 807–823. [Google Scholar] [CrossRef] [Green Version]
- Morris, J. Independent Lives?: Community Care and Disabled People; Macmillan International Higher Education: London, UK, 1993. [Google Scholar]
- Intagliata, J. Improving the quality of community care for the chronically mentally disabled: The role of case management. Schizophr. Bull. 1982, 8, 655–674. [Google Scholar] [CrossRef] [Green Version]
- Iparraguirre, J. Household composition and the dynamics of community-based social care in England. Ageing Soc. 2020, 40, 1631–1646. [Google Scholar] [CrossRef]
- Phillipson, C.; Bernard, M.; Phillips, J.; Ogg, J.I.M. The family and community life of older people: Household composition and social networks in three urban areas. Ageing Soc. 1998, 18, 259–289. [Google Scholar] [CrossRef]
- Wolf, D.A.; Soldo, B.J. Household composition choices of older unmarried women. Demography 1988, 25, 387–403. [Google Scholar] [CrossRef]
- Means, R.; Richards, S.; Smith, R. Community Care: Policy and Practice; Palgrave Macmillan: New York, NY, USA, 2008. [Google Scholar]
- Dean, H. Welfare Rights and Social Policy; Routledge: London, UK, 2014. [Google Scholar]


| Criterion A | Is More Important ← Equally Important → Is More Important | Criterion B | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 9:1 | 7:1 | 5:1 | 3:1 | 1:1 | 1:3 | 1:5 | 1:7 | 1:9 | ||
| Age | √ | Gender | ||||||||
| Criteria | Description |
|---|---|
| Age | Population aged 55 or older |
| Gender | Population aged 55 or older distinguished by women and men. |
| Marital status | Population aged 55 or older distinguished by single, married, divorced, and spouse deceased. |
| Educational attainment | Population aged 55 or older distinguished by education degree. |
| Ethnicity | Population aged 55 or older distinguished by nonindigenous, indigenous, and immigrant. |
| Household composition | Population aged 55 or older distinguished by living alone, living with spouse, living with children, living with relatives and friends, and living in long-term-care institutions. |
| Disability level | Population aged 55 or older distinguished by profound, severe, moderate, and mild disability. |
| Family income | Households’ annual income distinguished by percentile. |
| Social welfare identity | Households distinguished by low income and low–middle income. |
| Characteristics | Group A | Group B | Group C | Total | ||||
|---|---|---|---|---|---|---|---|---|
| Number of cases | 13 | 10 | 11 | 34 | ||||
| Gender | ||||||||
| Woman | 6 | 46% | 7 | 70% | 8 | 73% | 21 | 62% |
| Man | 7 | 54% | 3 | 30% | 3 | 27% | 13 | 38% |
| Age | ||||||||
| 20–30 years | 0 | 0% | 1 | 10% | 0 | 0% | 1 | 3% |
| 31–40 years | 0 | 0% | 5 | 50% | 1 | 9% | 6 | 18% |
| 41–50 years | 1 | 8% | 4 | 40% | 0 | 0% | 5 | 15% |
| 51–60 years | 8 | 62% | 0 | 0% | 3 | 27% | 11 | 32% |
| 61 years and above | 4 | 31% | 0 | 0% | 7 | 64% | 11 | 32% |
| Work experience | ||||||||
| 0–5 years | 0 | 0% | 1 | 10% | 0 | 0% | 1 | 3% |
| 6–10 years | 0 | 0% | 5 | 50% | 4 | 36% | 9 | 26% |
| 11 years and above | 13 | 100% | 4 | 40% | 7 | 64% | 24 | 71% |
| Group | Group A | Group B | Group C | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| Criteria | Geometric Mean | Geometric SD | Geometric Mean | Geometric SD | Geometric Mean | Geometric SD | ||
| Age | 0.175 | 0.092 | 0.098 | 0.114 | 0.156 | 0.100 | 0.198 | |
| Gender | 0.042 | 0.048 | 0.030 | 0.042 | 0.058 | 0.069 | 0.500 | |
| Marital status | 0.058 | 0.027 | 0.038 | 0.048 | 0.070 | 0.055 | 0.258 | |
| Educational attainment | 0.033 | 0.059 | 0.047 | 0.060 | 0.050 | 0.050 | 0.735 | |
| Ethnicity | 0.047 | 0.074 | 0.083 | 0.084 | 0.053 | 0.055 | 0.467 | |
| Household composition | 0.108 | 0.090 | 0.140 | 0.104 | 0.096 | 0.095 | 0.562 | |
| Disability level | 0.173 | 0.110 | 0.156 | 0.093 | 0.116 | 0.136 | 0.477 | |
| Family income | 0.074 | 0.105 | 0.080 | 0.092 | 0.092 | 0.064 | 0.885 | |
| Social welfare identity | 0.067 | 0.095 | 0.106 | 0.088 | 0.081 | 0.103 | 0.628 | |
| Group | p-Value | |||
|---|---|---|---|---|
| Criteria | Group A vs. B | Group A vs. C | Group B vs. C | |
| Age | 0.087 | 0.099 | 0.229 | |
| Gender | 0.012 | 0.511 | 0.281 | |
| Marital status | 0.218 | 0.520 | 0.174 | |
| Educational attainment | 0.581 | 0.459 | 0.902 | |
| Ethnicity | 0.288 | 0.827 | 0.341 | |
| Household composition | 0.438 | 0.754 | 0.324 | |
| Disability level | 0.699 | 0.268 | 0.446 | |
| Family income | 0.888 | 0.625 | 0.730 | |
| Social welfare identity | 0.325 | 0.733 | 0.559 | |
| Values | Group A | Group B | Group C | H Statistic | p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Criteria | Weighting Values | Ranking | Weighting Values | Ranking | Weighting Values | Ranking | |||
| Age | 0.225 | 1 | 0.126 | 9 | 0.202 | 3 | 0.213 | 0.899 | |
| Gender | 0.054 | 24 | 0.039 | 27 | 0.075 | 18 | |||
| Marital status | 0.075 | 19 | 0.049 | 25 | 0.091 | 16 | |||
| Educational attainment | 0.042 | 26 | 0.060 | 22.5 | 0.065 | 21 | |||
| Ethnicity | 0.060 | 22.5 | 0.107 | 12 | 0.069 | 20 | |||
| Household composition | 0.139 | 7 | 0.180 | 5 | 0.124 | 10 | |||
| Disability level | 0.223 | 2 | 0.201 | 4 | 0.150 | 6 | |||
| Family income | 0.095 | 15 | 0.103 | 14 | 0.119 | 11 | |||
| Social welfare identity | 0.086 | 17 | 0.136 | 8 | 0.105 | 13 | |||
| A. Group A vs. Group B | ||||||||
| Values | Group A | Group B | z-Score | Standard Deviation | p-Value | |||
| Criteria | Weighting Values | Ranking | Weighting Values | Ranking | ||||
| Age | 0.225 | 1 | 0.126 | 7 | 0.044 | 11.325 | 0.968 | |
| Gender | 0.054 | 15 | 0.039 | 18 | ||||
| Marital status | 0.075 | 12 | 0.049 | 16 | ||||
| Educational attainment | 0.042 | 17 | 0.060 | 13.5 | ||||
| Ethnicity | 0.060 | 13.5 | 0.107 | 8 | ||||
| Household composition | 0.139 | 5 | 0.180 | 4 | ||||
| Disability level | 0.223 | 2 | 0.201 | 3 | ||||
| Family income | 0.095 | 10 | 0.103 | 9 | ||||
| Social welfare identity | 0.086 | 11 | 0.136 | 6 | ||||
| B. Group A vs. Group C | ||||||||
| Values | Group A | Group C | z-score | Standard Deviation | p-value | |||
| Criteria | Weighting Values | Ranking | Weighting Values | Ranking | ||||
| Age | 0.225 | 1 | 0.202 | 3 | 0.530 | 11.325 | 0.596 | |
| Gender | 0.054 | 17 | 0.075 | 12 | ||||
| Marital status | 0.075 | 13 | 0.091 | 10 | ||||
| Educational attainment | 0.042 | 18 | 0.065 | 15 | ||||
| Ethnicity | 0.060 | 16 | 0.069 | 14 | ||||
| Household composition | 0.139 | 5 | 0.124 | 6 | ||||
| Disability level | 0.223 | 2 | 0.150 | 4 | ||||
| Family income | 0.095 | 9 | 0.119 | 7 | ||||
| Social welfare identity | 0.086 | 11 | 0.105 | 8 | ||||
| C. Group B vs. Group C | ||||||||
| Values | Group B | Group C | z-score | Standard Deviation | p-value | |||
| Criteria | Weighting Values | Ranking | Weighting Values | Ranking | ||||
| Age | 0.126 | 6 | 0.202 | 1 | 0.088 | 11.325 | 0.928 | |
| Gender | 0.039 | 18 | 0.075 | 13 | ||||
| Marital status | 0.049 | 17 | 0.091 | 12 | ||||
| Educational attainment | 0.060 | 16 | 0.065 | 15 | ||||
| Ethnicity | 0.107 | 9 | 0.069 | 14 | ||||
| Household composition | 0.180 | 3 | 0.124 | 7 | ||||
| Disability level | 0.201 | 2 | 0.150 | 4 | ||||
| Family income | 0.103 | 11 | 0.119 | 8 | ||||
| Social welfare identity | 0.136 | 5 | 0.105 | 10 | ||||
| Values | Weighting Values | Ranking | |
|---|---|---|---|
| Criteria | |||
| Disability level | 0.194 | 1 | |
| Age | 0.186 | 2 | |
| Household composition | 0.147 | 3 | |
| Social welfare identity | 0.108 | 4 | |
| Family income | 0.106 | 5 | |
| Ethnicity | 0.076 | 6 | |
| Marital status | 0.072 | 7 | |
| Educational attainment | 0.055 | 8 | |
| Gender | 0.055 | 8 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, H.-C. Priority Criteria for Community-Based Care Resource Allocation for Health Equity: Socioeconomic Status and Demographic Characteristics in the Multicriteria Decision-Making Method. Healthcare 2022, 10, 1358. https://doi.org/10.3390/healthcare10071358
Wu H-C. Priority Criteria for Community-Based Care Resource Allocation for Health Equity: Socioeconomic Status and Demographic Characteristics in the Multicriteria Decision-Making Method. Healthcare. 2022; 10(7):1358. https://doi.org/10.3390/healthcare10071358
Chicago/Turabian StyleWu, Hui-Ching. 2022. "Priority Criteria for Community-Based Care Resource Allocation for Health Equity: Socioeconomic Status and Demographic Characteristics in the Multicriteria Decision-Making Method" Healthcare 10, no. 7: 1358. https://doi.org/10.3390/healthcare10071358
APA StyleWu, H.-C. (2022). Priority Criteria for Community-Based Care Resource Allocation for Health Equity: Socioeconomic Status and Demographic Characteristics in the Multicriteria Decision-Making Method. Healthcare, 10(7), 1358. https://doi.org/10.3390/healthcare10071358






