A History of Heat Health Management Policies in the Singapore Military
Abstract
1. Introduction
1.1. Military Heat Stress Management
1.2. Local Historical Context and Research Questions
1.3. Research-Driven Measures and Soldier Safety
2. Methods
2.1. Collection of Documentary Sources
2.2. Use of Oral Histories
3. Medical-Historical Findings
3.1. Extent of Heat Injuries
3.2. Research-Driven Measures: Medical Shapers of Military Heat Stress Management
3.2.1. Building up Local Knowledge
3.2.2. Science-Based Interventions
- ➢
- Educating all recruits, medical officers, commanders and trainers through the use of simple messages and symposiums. Recruits, for instance, were taught how to conduct emergency first aid on their ‘buddy’ (assigned partner during basic military training) who had collapsed due to heat injury.
- ➢
- Safety regulations were incorporated into training programmes. This included a stress on ‘gradual and progressive increase in training load on a week to week basis’ to induce heat acclimatisation. Recruits were also grouped according to their physical fitness levels and prescribed appropriate training programmes.
- ➢
- Specific training regulations were introduced to set limits to training. This included defining strenuous activity types and prohibiting ‘excessive strenuous activities’ during the hottest part of the day; setting limits on training, such as prohibiting running beyond 10 km; introducing a work-rest cycle for strenuous activities (e.g., 15 min of rest for every 60 min of continuous physical exertion); and introducing water ‘parades’ which enforced pre-strenuous exercise liquid consumption ‘beyond the point of thirst’ in order to prevent dehydration and EHS.
- ➢
- The introduction of the BCU cooling system in ‘training schools where incidence[s] of heat disorders were high’, was followed by the installation of the system in almost every SAF camp by the end of the 1990s. Lee had learnt about the BCU during a trip to Israel in the early 1980s and worked with a Singapore defence engineer Koh Soo Keong to re-produce their own version of the BCU. Although the ‘gold’ standard for the rapid cooling of heat injuries is cold-water immersion, which can produce cooling rates of 0.15 to 0.24 °C/min, as compared to the SAF BCU which has produced cooling rates of 0.09 to 0.18 °C/min, the BCU was chosen as it was ‘well tolerated’ by patients and enabled ‘continuous monitoring and resuscitation’ [15,24,27,51,52].
4. Discussion
4.1. Soldier Safety: The State’s Shaping of Heat Stress Management Policy
4.2. New Context
4.3. New Standards
4.4. Soldier Safety-Shaped Measures and Research-Driven Measures
4.5. Implications
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bricknell, M.C.M. Heat Illness—A Review of Military Experience (Part 1). J. R. Med. Corps 1995, 141, 161–163. [Google Scholar] [CrossRef] [PubMed]
- Bricknell, M.C.M. Heat Illness—A Review of Military Experience (Part 2). J. R. Med. Corps 1995, 142, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Stonehill, R.B.; Keil, P.G. Successful Preventive Medical Measures Against Heat Illness at Lackland Air Force Base. AJPH 1961, 51, 586–590. [Google Scholar] [CrossRef] [PubMed]
- Minard, D. Prevention of Heat Casualties in Marine Corps Recruits: Period of 1955–60, with Comparative Incidence Rates and Climatic Heat Stresses in Other Training Categories. Mil. Med. 1961, 126, 261–272. [Google Scholar] [CrossRef]
- Ashworth, E.T.; Cotter, J.D.; Kilding, A.E. Methods for improving thermal tolerance in military personnel prior to deployment. Mil. Med. Res. 2020, 7, 58. [Google Scholar] [CrossRef] [PubMed]
- Nye, N.S.; O’Connor, F.G. Exertional Heat Illness Considerations in the Military. In Exertional Heat Illness: A Clinical and Evidence-Based Guide; Adams, W.M., Jardine, J.F., Eds.; Springer Nature: Cham, Switzerland, 2020; pp. 181–210. [Google Scholar]
- Yap, M.H.L.; Mah, P.K.; Liu, P.H.; Loong, S.C. Two Cases of Heat Stroke with Consumption Coagulopathy. Proc. Sixth Singap. Malays. Congr. Med. 1971, 6, 219–224. [Google Scholar]
- Chow, J. SAF is winning the war against heat. The Straits Times, 28 February 2011.
- Tan, K.P.; Seet, L.C.; Thomas, M. Heat Stress Among Soldiers in Training. Ann. Acad. Med. Singap. 1978, 7, 216–220. [Google Scholar]
- Two NS men died in running tests, coroner told. The Straits Times, 25 May 1978.
- Chong, A.; Chan, S. Militarizing civilians in Singapore: Preparing for ‘Crisis’ within a calibrated nationalism. Pac. Rev. 2017, 30, 365–384. [Google Scholar] [CrossRef]
- Tan, T.Y. The armed forces and politics in Singapore: The persistence of civil-military fusion. In The Political Resurgence of the Military in Southeast Asia; Mietzner, M., Ed.; Routledge: London, UK, 2011; pp. 148–166. [Google Scholar]
- Teh, H.F. The Soldier and the City-State: Civil-Military Relations and the Case of Singapore. Pointer 2005, 31, 46–60. [Google Scholar]
- Lee, K.Y. From Third World to First: The Singapore Story: 1965–2000; HarperCollins Publishers: New York, NY, USA, 2000. [Google Scholar]
- Lee, L. (Professor), 22 December 2020. Interview with first author.
- Our Story, DSO National Laboratories. Available online: https://www.dso.org.sg/about/history (accessed on 2 March 2022).
- Defence Scientist. 15 February 2022, Interview with first author.
- Barr, M.D. Singapore: The Limits of a Technocratic Approach to Health Care. J. Contemp. Asia 2008, 38, 395–416. [Google Scholar] [CrossRef]
- Dobbs, S.; Loh, K.S. Unsafety and Unions in Singapore’s State-led Industrialization, 1965–1994. Labor Hist. 2019, 61, 107–121. [Google Scholar] [CrossRef]
- Loh, K.S.; Hsu, L.Y. Tuberculosis—The Singapore Experience, 1867–2018: Disease, Society and the State; Routledge: New York, NY, USA, 2020. [Google Scholar]
- De Visser, M.; Straughan, P. Singapore: Technocracy and Transition. In COVID-19 in Asia: Law and Policy Contexts; Ramraj, V.V., Ed.; Oxford University Press: New York, NY, USA, 2021; pp. 221–238. [Google Scholar]
- Abdullah, W.J.; Kim, S. Singapore’s Responses to the COVID-19 Outbreak: A Critical Assessment. Am. Rev. Public Adm. 2020, 50, 770–776. [Google Scholar] [CrossRef]
- Adams, W.M.; Jardine, J.F. (Eds.) Overview of Exertional Heat Illness. In Exertional Heat Illness: A Clinical and Evidence-Based Guide; Springer Nature: Cham, Switzerland, 2020; pp. 1–16. [Google Scholar]
- Management of Heat Injuries: SAF-MOH Clinical Practice Guidelines 1/2010; SAF Medical Corps: Singapore, 2010.
- Hanna, J.M.; Brown, D.E. Human Heat Tolerance: An Anthropological Perspective. Annu. Rev. Anthropol. 1983, 12, 259–284. [Google Scholar] [CrossRef]
- Tsui, E.K.; Starecheski, A. Uses of oral history and digital storytelling in public health research and practice. Public Health 2018, 154, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.; Chia, H.P.; Tan, E.H. Prevention of Heat Disorders in the Singapore Armed Forces. Ann. Acad. Med. Singap. 1991, 20, 347–350. [Google Scholar] [PubMed]
- Low, W.M. Man in Hostile Environments: Training Injuries in the SAF. Pointer 1991, 17, 67–79. [Google Scholar]
- Koh, B.P. Better army with ISO award for medical corps. The Straits Times, 14 May 1998.
- Leong, M.K.F.; Ong, M.E.H.; Chew, K.T.L.; Teoh, C.S.; Lee, J.K.W. Heat Injury Management in the SAF: A Report by the External Review Panel on Heat Injury Management; Ministry of Defence: Singapore, 2018. Available online: https://www.mindef.gov.sg/web/wcm/connect/mindef/028fb0dc-9d5c-40dd-9302-f33a54471e9b/ERPHIM-report.pdf?MOD=AJPERES&attachment=true&CACHE=NONE&CONTENTCACHE=NONE (accessed on 30 December 2020).
- Chua, I. National serviceman, 19, died after heat stroke. The Straits Times, 30 April 2018.
- Lim, S.W.; Pang, A.S.; Tan, K.P. Heat disorders: The Singapore Armed Forces experience 1980–1984. In Heat Disorders; Yeo, P.P.B., Lim, M.K., Eds.; Headquarters Medical Services, Singapore Armed Forces and Ministry of Health: Singapore, 1988; pp. 55–61. [Google Scholar]
- Lee, T. Fewer SAF soldiers hit by heat stroke. The Straits Times, 28 June 1997.
- Lim, Y.L. NSF who died had heart condition. The Straits Times, 28 February 2013.
- Abisheganaden, J.; Koh, A. Medical Corps: The Story of the SAF Medical Services; Headquarters Medical Services, Singapore Armed Forces: Singapore, 1992. [Google Scholar]
- Yeo, P.P.B.; Tay, H.H.; Tan, K.P.; Kwa, S.B. Heat disorders: Hospital survey 1974–1979. In Heat Disorders; Yeo, P.P.B., Lim, M.K., Eds.; Headquarters Medical Services, Singapore Armed Forces and Ministry of Health: Singapore, 1988; pp. 26–51. [Google Scholar]
- Bartley, J.D. Heat Stroke: Is Total Prevention Possible? Mil. Med. 1977, 142, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Choo, M.H.H. Clinical presentation of heat disorders. In Heat Disorders; Yeo, P.P.B., Lim, M.K., Eds.; Headquarters Medical Services, Singapore Armed Forces and Ministry of Health: Singapore, 1988; pp. 6–15. [Google Scholar]
- NS recruit died after running an extra 300m. The Straits Times, 25 July 1984.
- Yeo, P.P.B.; Lim, M.K. (Eds.) Preface. In Heat Disorders; Headquarters Medical Services, Singapore Armed Forces and Ministry of Health: Singapore, 1988; unpaginated. [Google Scholar]
- Lee, L.K.H. Heat stroke: Preventive measures. In Heat Disorders; Yeo, P.P.B., Lim, M.K., Eds.; Headquarters Medical Services, Singapore Armed Forces and Ministry of Health: Singapore, 1988; pp. 62–72. [Google Scholar]
- Lambert, H. Accounting for EBM: Notions of evidence in medicine. Soc. Sci. Med. 2006, 62, 2633–2645. [Google Scholar] [CrossRef]
- Lambert, H.; Gordon, E.J.; Bogdan-Lovis, E.A. Introduction: Gift horse or Trojan horse? Social science perspectives on evidence-based health care. Soc. Sci. Med. 2006, 62, 2613–2620. [Google Scholar] [CrossRef]
- Denny, K. Evidence-Based Medicine and Medical Authority. J. Med. Humanit. 1999, 20, 247–263. [Google Scholar] [CrossRef]
- In Loving Memory of Dr. Teh KC, Sports Medicine Association Singapore. Available online: https://www.sportsmedicine.org.sg/in-loving-memory-drtehkc/ (accessed on 19 October 2022).
- Lee, P. Healthcare pioneer Kwa Soon Bee dies. The Straits Times, 31 October 2016.
- Tan, J.H.S. Winston Choo. In Singapore Infopedia. Available online: https://eresources.nlb.gov.sg/infopedia/articles/SIP_1852_2011-11-01.html (accessed on 1 March 2022).
- SAF plan for fitter, strong soldiers. The Straits Times, 27 July 1985.
- Lim, F. (Associate Professor). Interview with first author. 30 December 2020.
- Lee, L. (Hong Kong Baptist University, Hong Kong). Personal communication, 26 February 2022.
- Soldiers drink their fill to beat the heat. The Straits Times, 24 December 1987.
- Chua, C.C. Coloured plates help reduce heat stroke in NS recruits. The Straits Times, 26 August 1987.
- Khoo, B.T.; Tadem, T.S.E.; Takashi, S. Technocracy and Economic Decision-Making in Southeast Asia: An Overview. Southeast Asian Stud. 2014, 3, 241–253. [Google Scholar]
- Barr, M.D. New Politics and Old Managerialism: Welcome to the New Normal. In The Limits of Authoritarian Governance in Singapore’s Developmental State; Rahim, L.Z., Barr, M.D., Eds.; Palgrave Macmillan: Singapore, 2019; pp. 131–149. [Google Scholar]
- Senior SAF Medical Officer. 16 Mar 2022, Interview with first author.
- Tan, T. Injuries Resulting from Military Training; Singapore Parliament Hansard: Singapore, 17 January 2000. [Google Scholar]
- Chan, S.L.W. Aristocracy of Armed Talent: The Military Elite in Singapore; NUS Press: Singapore, 2019. [Google Scholar]
- Kuek, D. Rising to Army 21: Adding Value, Holding Values. Pointer 1999, 25, 25–35. [Google Scholar]
- Goh, K.N.; Tan, B.; Lim, D. Learning Army Thinking Soldier. Pointer 2008, 33, 13–25. [Google Scholar]
- Quek, S. Gearing up for networked urban operations. Cyberpioneer 8 September 2008. Available online: https://web.archive.org/web/20130516110529/http://www.mindef.gov.sg/imindef/publications/cyberpioneer/news/2008/September/08sep08_news.html (accessed on 2 March 2021).
- Chan, K.M. High-tech soldiers of the future. The Straits Times, 30 November 2000.
- Boey, D. Singapore Armed Forces’ new firepower to make public debut. The Straits Times, 29 August 2002.
- Fang, I.J.L. Grooming and Grounding Heartware: SAF Leadership Challenges at the Dawn of the 21st Century. Pointer 1999, 25, 11–29. [Google Scholar]
- Teo, C.H. Ministerial Statement on the Recent Deaths of Three SAF Servicemen. 16 October 2003. Available online: https://www.nas.gov.sg/archivesonline/data/pdfdoc/MINDEF_20031016001.pdf (accessed on 2 March 2021).
- Goh, C.T. Training of SAF Personnel (Safety Measures); Singapore Parliament Hansard: Singapore, 20 November 1984. [Google Scholar]
- Lee, H.L. National Servicemen (Injuries and Suicides); Singapore Parliament Hansard: Singapore, 27 March 1986. [Google Scholar]
- Teh, J.L.; Chow, J. SAF suspends physical training for three days. The Straits Times, 13 June 2008.
- Almenoar, M. Soldiers’ deaths: No foul play or safety lapses. The Straits Times, 22 October 2008.
- 2 Deaths 7 Suspensions what’s next? The New Paper, 15 November 2012.
- Chow, J. Commando trainee in hospital after suffering heat injury. The Straits Times, 15 June 2011.
- Chow, J. SAF halts training following NSF’s death. The Straits Times, 4 August 2011.
- Lim, M.Z. Army training to resume in Singapore and Australia from Nov 8 after safety timeout. The Straits Times, 7 November 2018.
- Boey, D. Can the SAF achieve zero training fatalities again? Today, 25 January 2019 (Updated 18 April 2019).
- Ng, E.H. Death of NSF Dave Lee: Full text of Dr Ng Eng Hen’s ministerial statement in Parliament. Channel NewsAsia (CNA), 6 August 2018.
- Lo, H.Y. (Colonel [Dr]), 19 Jan 2021. Interview with first author.
- Lim, M.Z. SAF to roll out arm immersion drill, cooling pads to better manage heat injury. The Straits Times, 6 August 2018.
- Immersing arms in ice water, special pads to keep troops cool. The Straits Times, 7 August 2018.
- DeGroot, D.W.; Gallimore, R.P.; Thompson, S.M.; Kenefick, R.W. Extremity cooling for heat stress mitigation in military and occupational settings. J. Therm. Biol. 2013, 38, 305–310. [Google Scholar] [CrossRef]
- Army Safety Day Seminar 2019, The Singapore Army Facebook Page. Available online: https://www.facebook.com/oursingaporearmy/posts/10156844528191063 (accessed on 2 March 2021).
- Au-Yong, R. 900 bid farewell to late NSF in military funeral. The Straits Times, 6 May 2018.
- Yang, C. Hundreds show up to bid farewell to late NSF. The Straits Times, 6 November 2018.
- Toh, Y.C. HomeFront; Soldier’s death: Questions need answering. The Straits Times, 10 May 2018.
- Chief of Army assures soldiers of thorough investigation into death of NSF Dave Lee. CNA, 4 May 2018.
- Lim, M.Z. Home Front; NS training deaths: Train hard but train safe—Striking a balance. The Straits Times, 16 August 2018.
- Ng, E.H. National Service Training Deaths and Safety Enhancements for the SAF; Singapore Parliament Hansard: Singapore, 11 February 2019. [Google Scholar]
- Au Yong, E. Lighter, smarter army fatigues. My Paper, 3 September 2008.
- Lee, J.K.W.; Nio, A.Q.; Fun, D.C.; Teo, Y.S.; Von Chia, E.; Lim, C.L. Effects of heat acclimatisation on work tolerance and thermoregulation in trained tropical natives. J. Therm. Biol. 2012, 37, 366–373. [Google Scholar] [CrossRef]
- Tan, P.M.S.; Teo, E.Y.; Ali, N.B.; Ang, B.C.; Iskandar, I.; Law, L.Y.; Lee, J.K. Evaluation of Various Cooling Systems After Exercise-Induced Hyperthermia. J. Athl. Train. 2017, 52, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.W.; Yeo, Z.W.; Nio, A.Q.; Ang, W.H.; Fan, P.W. Ice Slurry Ingestion Improves Subsequent Outdoor 10 km Running Performance in the Heat. Med. Sci. Sport. Exerc. 2011, 43, 74. [Google Scholar] [CrossRef]
- Yeo, Z.W.; Fan, P.W.P.; Nio, A.Q.X.; Byrne, C.; Lee, J.K.W. Ice Slurry on Outdoor Running Performance in Heat. Int. J. Sport. Med. 2012, 33, 859–886. [Google Scholar] [CrossRef]
- Lee, J.K.W.; Yeo, Z.W.; Nio, A.Q.X.; Koh, A.C.H.; Teo, Y.S.; Goh, L.F.; Byrne, C. Cold Drink Attenuates Heat Strain during Work-rest Cycles. Int. J. Sport. Med. 2013, 34, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- Tay, C.S.; Lee, J.K.; Teo, Y.S.; Foo, P.Q.; Tan, P.M.; Kong, P.W. Using gait parameters to detect fatigue and responses to ice slurry during prolonged load carriage. Gait Posture 2016, 42, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.W.; Law, Y.L.; Ong, J.; Fun, C.D.; Alexander, G.; Tan, M.P. Heat tolerance in wet tropical natives using an established heat tolerance test. J. Sci. Med. Sport 2017, 20S, S58. [Google Scholar] [CrossRef]
- Poon, B.H.; Prakaash, S.; Teo, Y.S.; Fan, P.W.; Lee, J.K.W. Thermal strain and fluid balance during a 72 km military route march in the field setting. Singap. Med. J. 2021, 63, 497–502. [Google Scholar]
- Poon, B.H.; Gorny, A.W.; Zheng, K.; Cheong, W.K. Relationship between weather parameters and risk of exertional heat injuries during military training. Singap. Med. J. 2021, 63, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, Y.; Casa, D.J.; Trtanj, J.M.; Belval, L.N.; Deuster, P.A.; Giltz, S.M.; Williams, W.J. Activity modification in heat: Critical assessment of guidelines across athletic, occupation, and military settings in the USA. Int. J. Biometeorol. 2019, 63, 405–427. [Google Scholar] [CrossRef]
- Nazarian, N.; Krayenhoff, E.S.; Bechtel, B.; Hondula, D.M.; Paolini, R.; Vanos, J.; Santamouris, M. Integrated assessment of urban overheating impacts on human life. Earth’s Future 2022, 10, e2022EF002682. [Google Scholar] [CrossRef]
- Fact Sheet: Leveraging Digital Technology and Research to Enhance Safety of National Servicemen, MINDEF Singapore, 3 March 2022. Available online: https://www.mindef.gov.sg/web/portal/mindef/news-and-events/latest-releases/article-detail/2022/March/03mar22_fs2 (accessed on 3 November 2022).
- Impact of Climate Change on Singapore, National Climate Change Secretariat, Singapore. Available online: https://www.nccs.gov.sg/singapores-climate-action/impact-of-climate-change-in-singapore/ (accessed on 22 October 2022).
- Pradhan, B.; Kjellstrom, T.; Atar, D.; Sharma, P.; Kayastha, B.; Bhandari, G.; Pradhan, P.K. Heat Stress Impacts on Cardiac Mortality in Nepali Migrant Workers in Qatar. Cardiology 2019, 143, 37–48. [Google Scholar] [CrossRef]
- Wegman, D.H.; Neupane, D.; Sharma, S.; Glaser, J. Dying for sport. Occup. Environ. Med. 2022, 79, 73–74. [Google Scholar] [CrossRef]
- Dhakal, N.; Bhurtyal, N.; Singh, P.; Singh, D.S. Chronic Kidney Disease in Migrant Workers in Nepal. Kidney Int. Rep. 2020, 5, S58. [Google Scholar] [CrossRef]
- DeGroot, D.W.; Mok, G.; Hathaway, N.E. International Classification of Disease Coding of Exertional Heat Illness in U.S. Army Soldiers. Mil. Med. 2017, 182, e1946. [Google Scholar] [CrossRef]
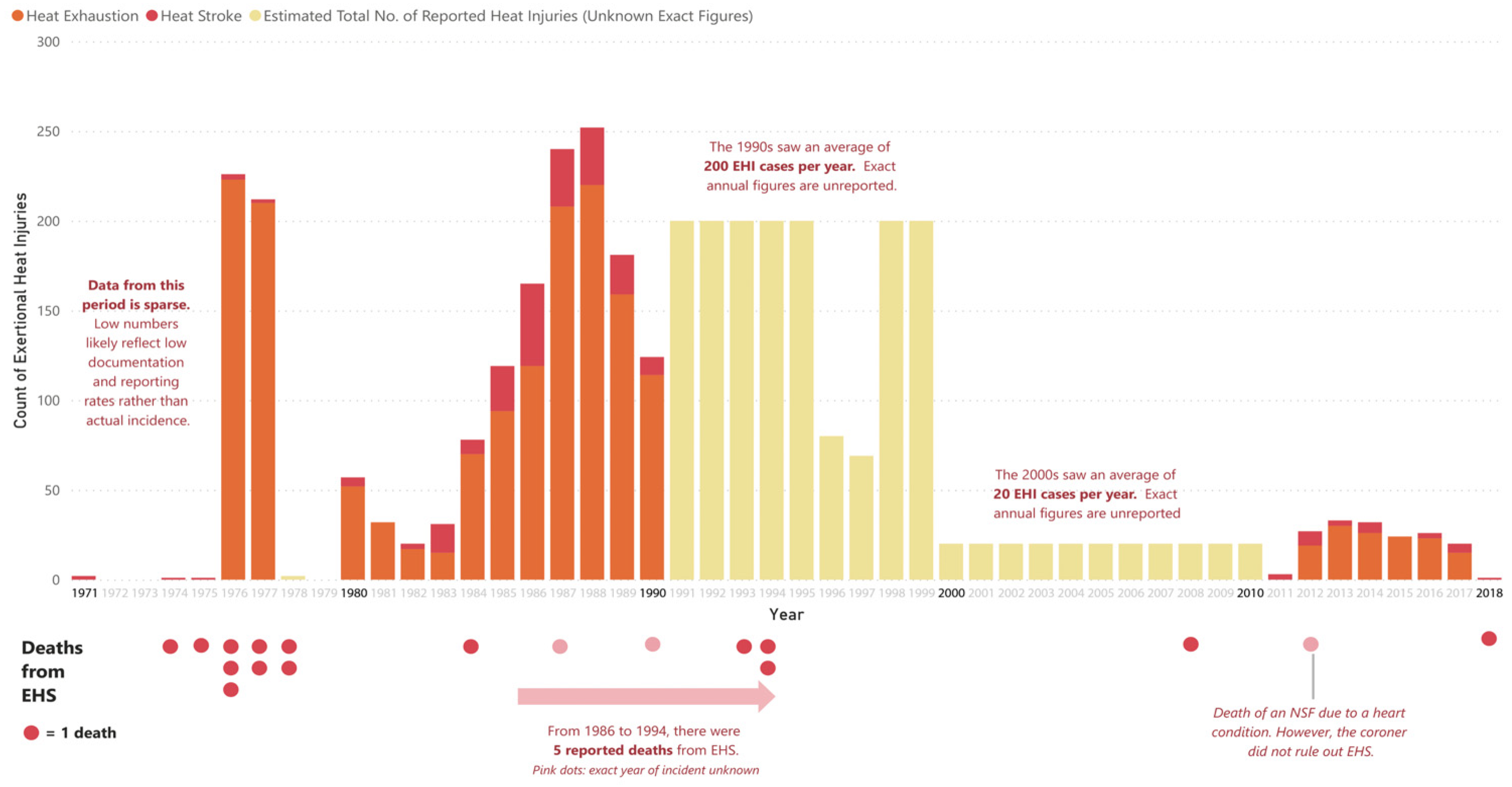
| Year | Heat Stroke | Heat Exhaustion | All Heat Injuries | Deaths Due to EHS |
|---|---|---|---|---|
| 1971 | 2 | Not reported | Not reported | Not reported |
| 1974 | 1 | Not reported | Not reported | 1 |
| 1975 | 1 | Not reported | Not reported | 1 |
| 1976 | 3 | 223 | 226 | 3 |
| 1977 | 2 | 210 | 212 | 2 |
| 1978 | Not reported | Not reported | Not reported | 2 |
| 1980 | 5 | 52 | 67 | 0 |
| 1981 | 0 | 32 | 56 | 0 |
| 1982 | 3 | 17 | 30 | 0 |
| 1983 | 16 | 15 | 97 [32] | 0 |
| 1984 | 8 | 70 | 78 [32] | 1 |
| 1985 | 25 | 94 | 119 | Not reported |
| 1986 | 46 | 119 | 165 | Not reported |
| 1987 | 32 | 208 | 240 | Not reported |
| 1988 | 32 | 220 | 252 | Not reported |
| 1989 | 22 | 159 | 181 | Not reported |
| 1990 | 10 | 114 | 124 | Not reported |
| 1993 | Not reported | Not reported | Not reported | 1 |
| 1994 | Not reported | Not reported | Not reported | 2 (1986-1994: 5 deaths) [33] |
| 1996 | Not reported | Not reported | 80 (1990s: 200 per year) [33] | 0 |
| 1997 | Not reported | Not reported | 69 | 0 |
| 2008 | Not reported | Not reported | Not reported | 1 |
| 2011 | 2 + 1? | Not reported | 2000s: 20 per year [8] | 1? [34] |
| 2012 | 8 | 19 | 27 | 0 |
| 2013 | 3 | 30 | 33 | 0 |
| 2014 | 6 | 26 | 32 | 0 |
| 2015 | 0 | 24 | 24 | 0 |
| 2016 | 3 | 23 | 26 | 0 |
| 2017 | 5 | 15 | 20 | 0 |
| 2018 | 1 | Not reported | Not reported | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sim, J.D.W.; Lee, J.K.W. A History of Heat Health Management Policies in the Singapore Military. Healthcare 2023, 11, 211. https://doi.org/10.3390/healthcare11020211
Sim JDW, Lee JKW. A History of Heat Health Management Policies in the Singapore Military. Healthcare. 2023; 11(2):211. https://doi.org/10.3390/healthcare11020211
Chicago/Turabian StyleSim, Joshua Dao Wei, and Jason Kai Wei Lee. 2023. "A History of Heat Health Management Policies in the Singapore Military" Healthcare 11, no. 2: 211. https://doi.org/10.3390/healthcare11020211
APA StyleSim, J. D. W., & Lee, J. K. W. (2023). A History of Heat Health Management Policies in the Singapore Military. Healthcare, 11(2), 211. https://doi.org/10.3390/healthcare11020211






