New Method to Implement and Analysis of Medical System in Real Time
Abstract
:1. Introduction
2. Experimental Methodology
- A.
- Design of a circuit for measuring vital parameters and the proportion of gases in the blood.
- B.
- Design of a circuit for measuring body resistance.
- C.
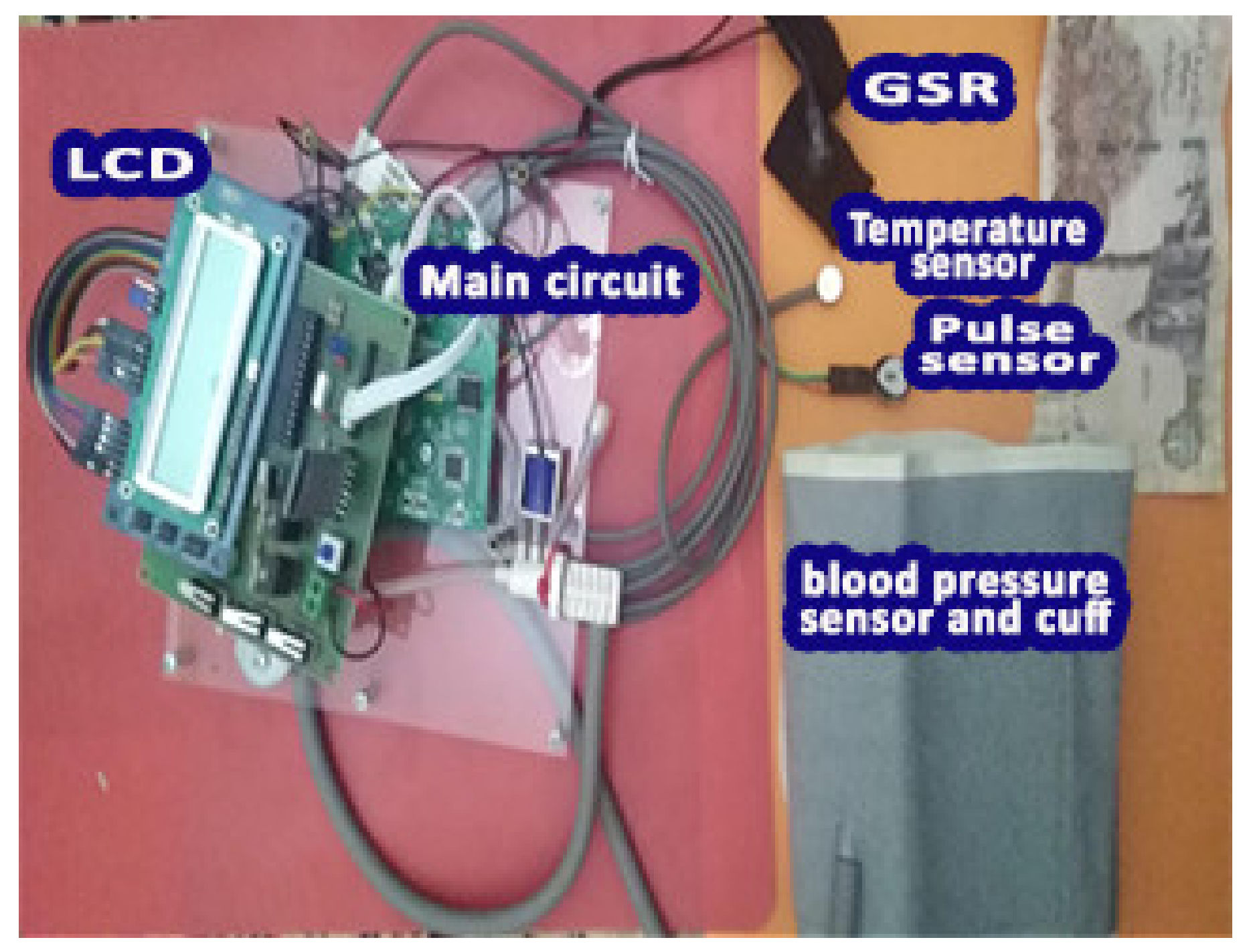
- Merging the circuits into one device.
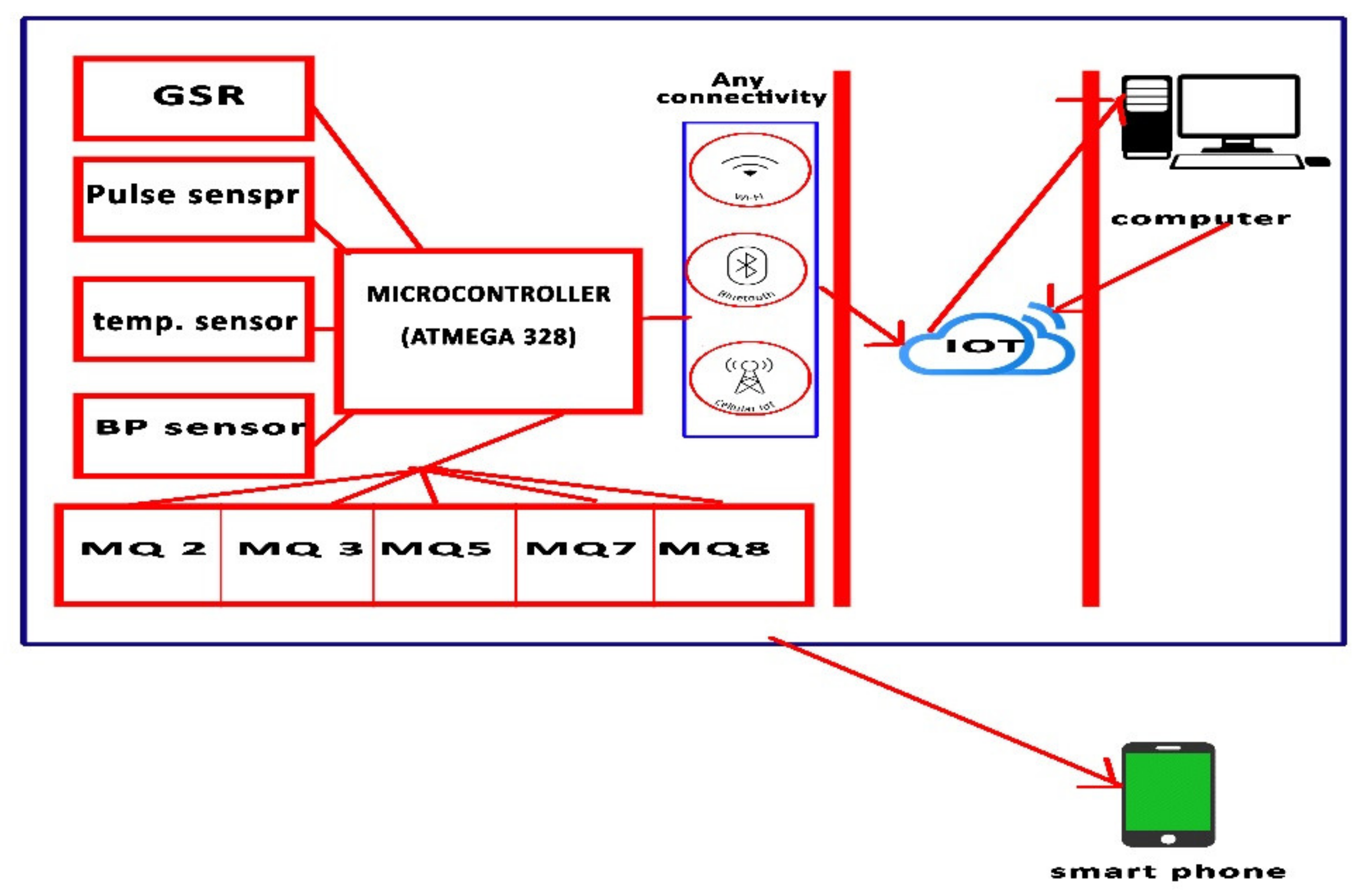
2.1. The Proposed System for Measuring Vital Parameters
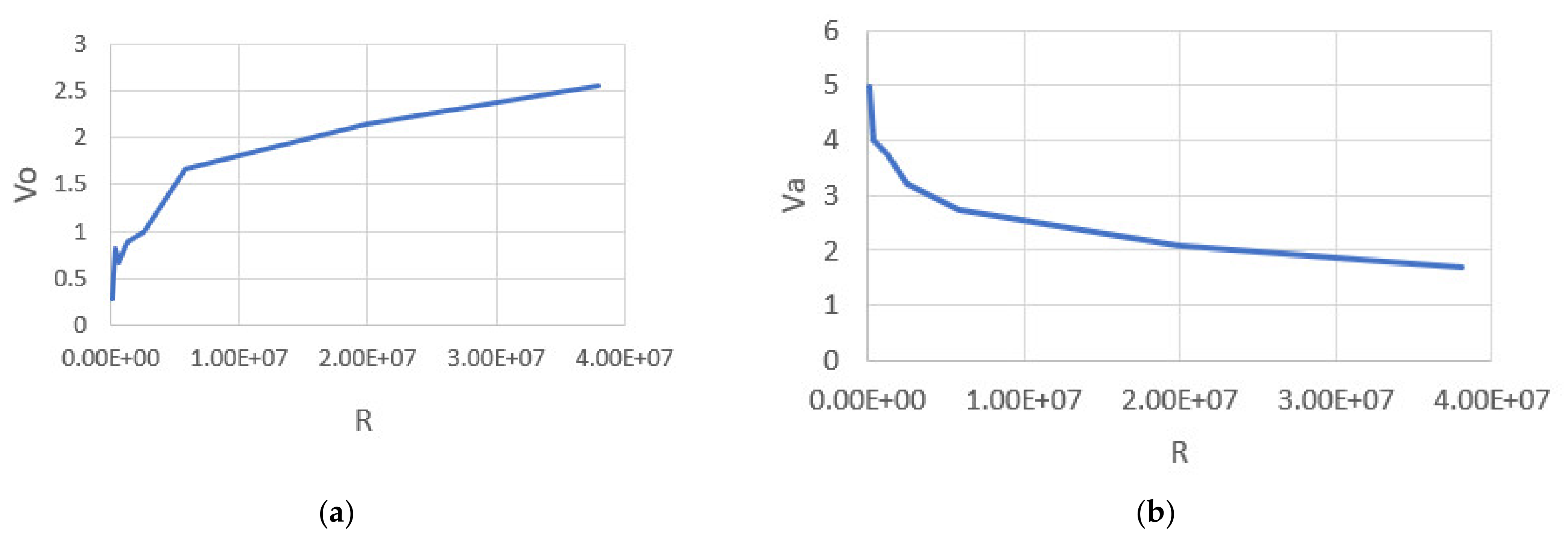
2.2. Proposed Galvanic Skin Response Circuit
2.3. Merging Circuits
3. Results
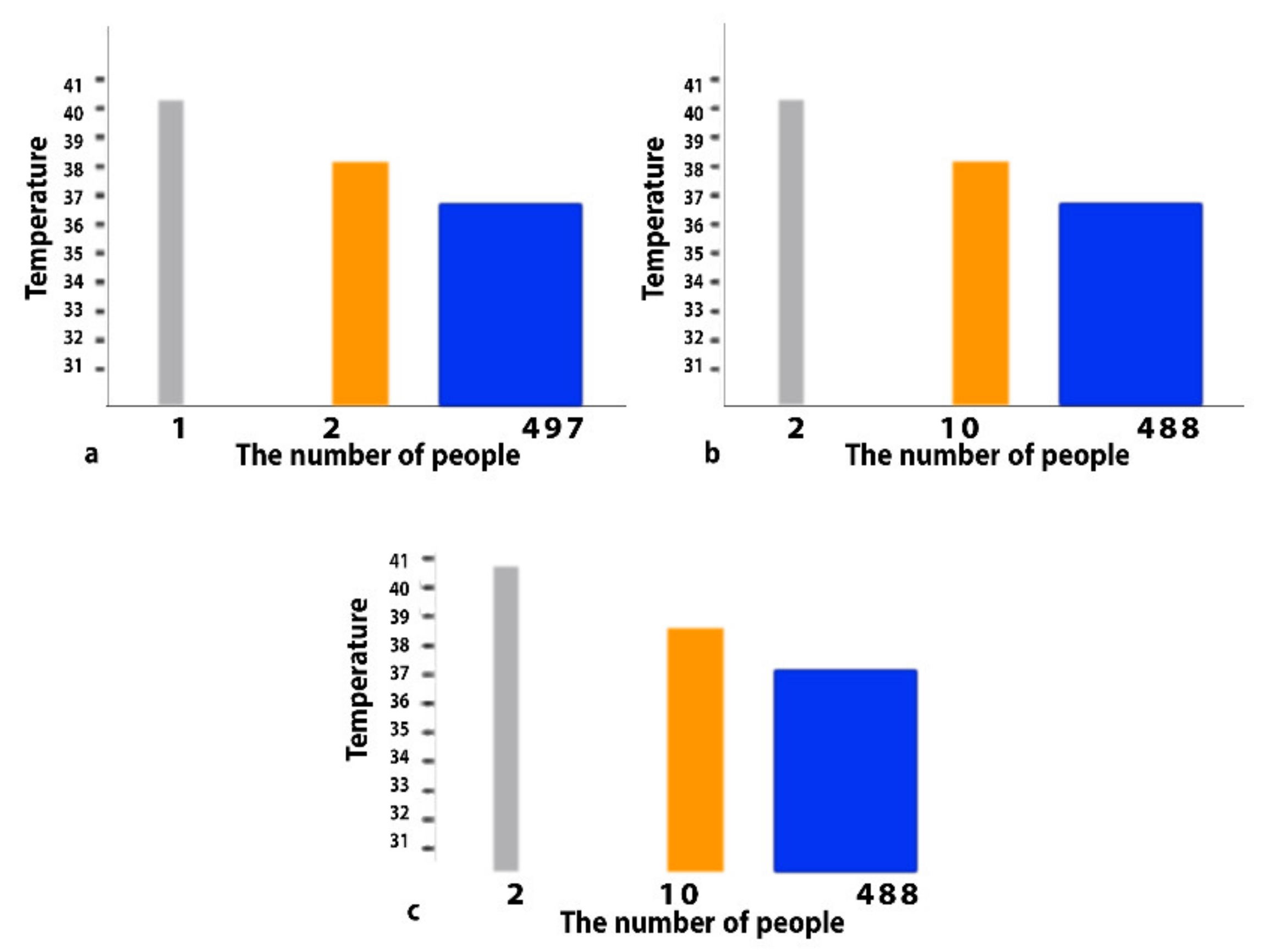
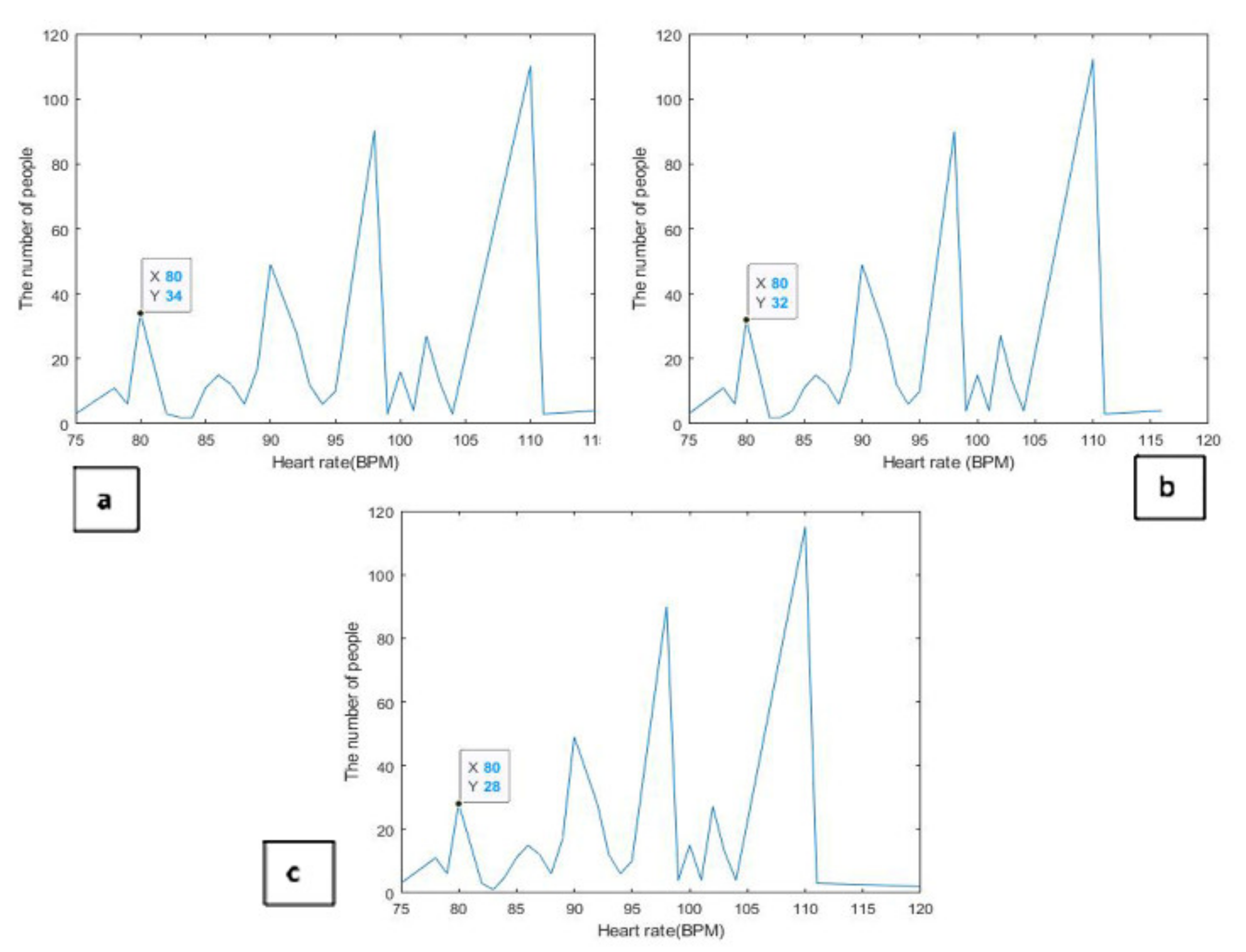
3.1. Effect of Emotions on Vital Parameters
3.2. The Proportion of Some Gases in the Blood
3.3. Machine Learning Model for Diagnosis and Prediction
- A.
- A part that categorizes and predicts the level of gases in the blood based on measurements of gas levels taken.
- B.
- The other part analyzes, classifies and predicts (emotions and diseases) based on the measured vital parameters.
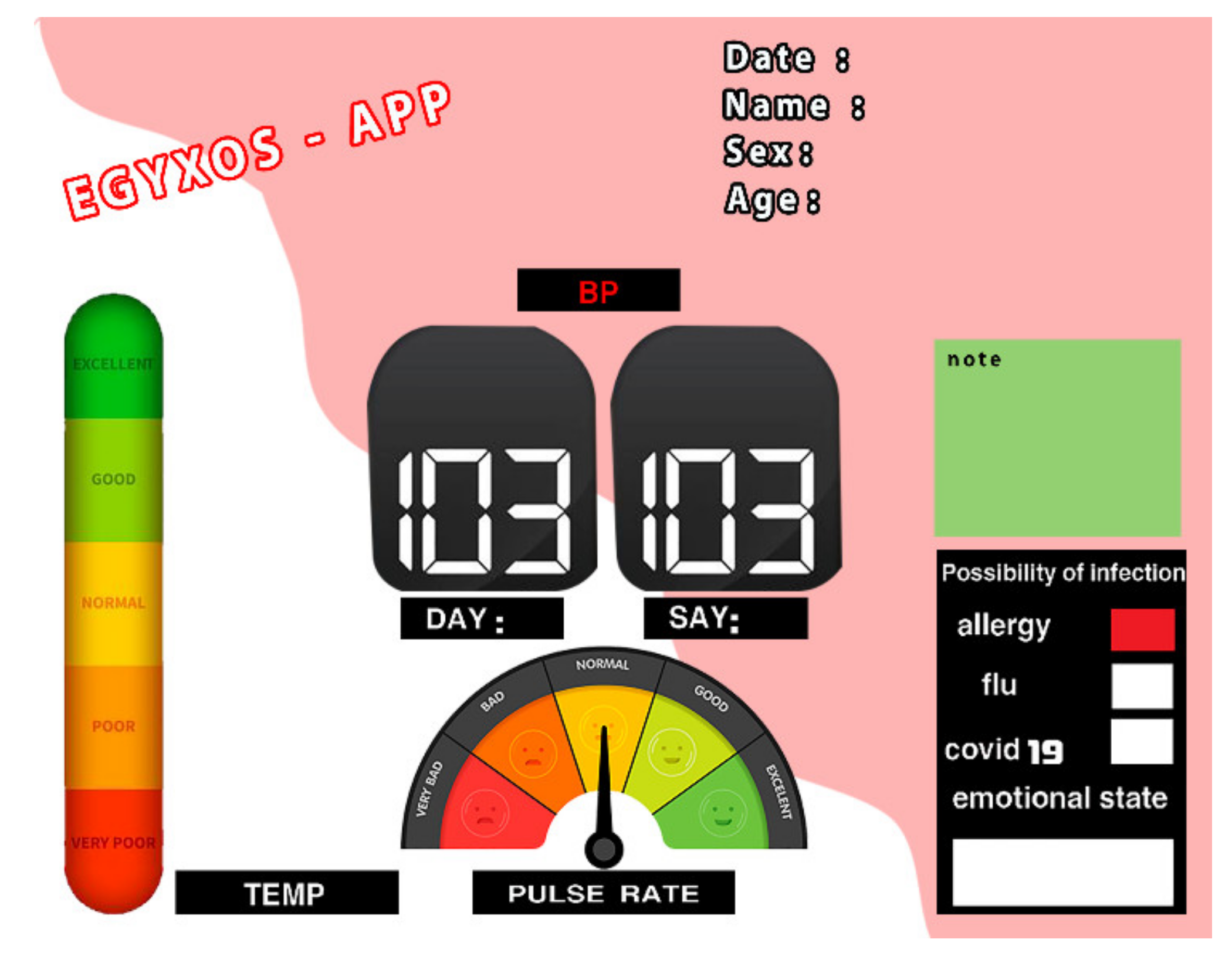
3.4. Internet of Things Application
- LR1 (human/patient)
- 2.
- LR2 (cloud)
- 3.
- LR3 (doctor/hospital/patient’s relatives)
3.5. Comparing the Proposed Work with Other Works That Support Similar Ideas
3.6. Statistical Analysis of the Proposed System Measurements
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- El Mashade, M.B.; Zakaria, Y.; Elgawad, A.; Nasser, T.M. Fuzzy Logic Controller of New Strategy of Biomedical Measurement. Int. J. Online Biomed. Eng. 2020, 16, 133–150. [Google Scholar] [CrossRef]
- Eesee, A.K. The suitability of the Galvanic Skin Response (GSR) as a measure of emotions and the possibility of using the scapula as an alternative recording site of GSR. In Proceedings of the 2nd International Conference on Electrical, Communication, Computer, Power and Control Engineering (ICECCPCE), Mosul, Iraq, 13–14 February 2019; pp. 80–84. [Google Scholar] [CrossRef]
- Karanchery, S.; Palaniswamy, S. Emotion recognition using one-shot learning for human-computer interactions. In Proceedings of the International Conference on Communication, Control and Information Sciences (ICCISc), Idukki, India, 16–18 June 2021; pp. 1–8. [Google Scholar] [CrossRef]
- Azgomi, H.F.; Cajigas, I.; Faghih, R.T. Closed-Loop Cognitive Stress Regulation Using Fuzzy Control in Wearable-Machine Interface Architectures. IEEE Access 2021, 9, 106202–106219. [Google Scholar] [CrossRef]
- Satti, F.A.; Hussain, M.; Hussain, J.; Kim, T.-S.; Lee, S.; Chung, T. User Stress Modeling through Galvanic Skin Response. In Proceedings of the 15th International Conference on Ubiquitous Information Management and Communication (IMCOM), Seoul, Korea, 4–6 January 2021; pp. 1–6. [Google Scholar] [CrossRef]
- Hanoon, I.K.; Aal-Nouman, M.I. Cloud-based COVID-19 Patient Monitoring using Arduino. In Proceedings of the 3rd East Indonesia Conference on Computer and Information Technology (EIConCIT), Surabaya, Indonesia, 9–11 April 2021; pp. 292–296. [Google Scholar] [CrossRef]
- De Palma, L.; Scarpetta, M.; Spadavecchia, M. Characterization of Heart Rate Estimation Using Piezoelectric Plethysmography in Time- and Frequency-domain. In Proceedings of the IEEE International Symposium on Medical Measurements and Applications (MeMeA), Bari, Italy, 1 June–1 July 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Rahman, J.R.; Sanshi, S.; Ahamed, N.N. Health Monitoring and Predicting System using Internet of Things & Machine Learning. In Proceedings of the 7th International Conference on Advanced Computing and Communication Systems (ICACCS), Coimbatore, India, 19–20 March 2021; pp. 223–226. [Google Scholar] [CrossRef]
- Dilip, R.; Borole, Y.D.; Sumalatha, S.; Nethravathi, H. Speech Based Biomedical Devices Monitoring Using LabVIEW. In Proceedings of the 9th International Conference on Cyber and IT Service Management (CITSM), Bengkulu, Indonesia, 22–23 September 2021; pp. 1–7. [Google Scholar] [CrossRef]
- Singh, N.; Dehuri, S.; Tripathy, D.; Sahoo, A.B. Real Time Heart Beat Monitoring with LABVIEW. In Proceedings of the 19th OITS International Conference on Information Technology (OCIT), Bhubaneswar, India, 16–18 December 2021; pp. 10–13. [Google Scholar] [CrossRef]
- Setyohadi, D.B.; Kusrohmaniah, S.; Gunawan, S.B.; Pranowo, P. Galvanic Skin Response Data Classification for Emotion Detection. Int. J. Electr. Comput. Eng. (IJECE) 2018, 8, 31–41. [Google Scholar] [CrossRef] [Green Version]
- Santamaria-Granados, L.; Munoz-Organero, M.; Ramirez-Gonzalez, G.; Abdulhay, E.; Arunkumar, N.J. Using deep convolutional neural network for emotion detection on a physiological signals dataset (AMIGOS). IEEE Access 2018, 7, 57–67. [Google Scholar] [CrossRef]
- Siam, A.I.; Abou Elazm, A.; El-Bahnasawy, N.A.; El Banby, G.; Abd El-Samie, F.E.; Abd El-Samie, F.E. Smart Health Monitoring System based on IoT and Cloud Computing. In Proceedings of the 1st International Conference on Electronic Engineering, Shibin El Kom, Egypt, 7–8 December 2019; pp. 37–42. [Google Scholar]
- Yew, H.T.; Ng, M.F.; Ping, S.Z.; Chung, S.K.; Chekima, A.; Dargham, J.A. IoT Based Real-Time Remote Patient Monitoring System. In Proceedings of the 16th IEEE International Colloquium on Signal Processing & Its Applications (CSPA), Langkawi, Malaysia, 28–29 February 2020; pp. 176–179. [Google Scholar]
- Tamilselvi, V.; Sribalaji, S.; Vigneshwaran, P.; Vinu, P.; Geetha Ramani, J. IoT Based Health Monitoring System. In Proceedings of the 6th International Conference on Advanced Computing and Communication Systems (ICACCS), Piscataway, NJ, USA, 6–7 March 2022; pp. 386–389. [Google Scholar]
- Ruman, M.R.; Barua, A.; Rahman, W.; Jahan, K.R.; Roni, M.J.; Rahman, M.F. IoT Based Emergency Health Monitoring System. In Proceedings of the International Conference on Industry 4.0 Technology (I4Tech), Pune, India, 13–15 February 2020; pp. 159–162. [Google Scholar]
- Kumar, S.A.; Gopinath, B.; Kavinraj, A.; Sasikala, S. Towards Improving Patient Health Monitoring System using Machine Learning and Internet of Things. In Proceedings of the International Conference on Advancements in Electrical, Electronics, Communication, Computing and Automation (ICAECA), Coimbatore, India, 8–9 October 2021; pp. 1–5. [Google Scholar] [CrossRef]
- Shalini, V.B. Smart Health Care Monitoring System based on Internet of Things (IOT). In Proceedings of the International Conference on Artificial Intelligence and Smart Systems (ICAIS), Coimbatore, India, 25–27 March 2021; pp. 1449–1453. [Google Scholar] [CrossRef]
- Akram, P.S.; Ramesha, M.; Valiveti, S.A.S.; Sohail, S.; Rao, K.T.S.S. IoT based Remote Patient Health Monitoring system. In Proceedings of the 7th International Conference on Advanced Computing and Communication Systems (ICACCS), Coimbatore, India, 19–20 March 2021; pp. 1519–1524. [Google Scholar]
- Bhardwaj, H.; Bhatia, K.; Jain, A.; Verma, N. IOT Based Health Monitoring System. In Proceedings of the 6th International Conference on Communication and Electronics Systems (ICCES), Coimbatore, India, 8–10 July 2021; pp. 1–6. [Google Scholar]
- Visvesvaran, C.; Shankar, B.M.; Kaviya, S.; Kaviya, P.; Monika, K.; Kumar, I.J.J.B. Quarcare-IoT Based Patient Health Monitoring System. In Proceedings of the Second International Conference on Electronics and Sustainable Communication Systems (ICESC), Coimbatore, India, 4–6 August 2021; pp. 870–874. [Google Scholar]
- Jeon, J.; Kim, S.; Kang, G.H.; Suh, K. Analysis of Emergency Medical Vulnerability and Survival Rates Following Real-Time Traffic Information. Appl. Sci. 2020, 10, 6492. [Google Scholar] [CrossRef]
- Sakphrom, S.; Limpiti, T.; Funsian, K.; Chandhaket, S.; Haiges, R.; Thinsurat, K. Intelligent Medical System with Low-Cost Wearable Monitoring Devices to Measure Basic Vital Signals of Admitted Patients. Micromachines 2021, 12, 918. [Google Scholar] [CrossRef] [PubMed]
- Hedderich, D.M.; Keicher, M.; Wiestler, B.; Gruber, M.J.; Burwinkel, H.; Hinterwimmer, F.; Czempiel, T.; Spiro, J.E.; Pinto dos Santos, D.; Heim, D.; et al. AI for Doctors—A Course to Educate Medical Professionals in Artificial Intelligence for Medical Imaging. Healthcare 2021, 9, 1278. [Google Scholar] [CrossRef] [PubMed]
- Garcés-Jiménez, A.; Calderón-Gómez, H.; Gómez-Pulido, J.M.; Gómez-Pulido, J.A.; Vargas-Lombardo, M.; Castillo-Sequera, J.L.; Aguirre, M.P.; Sanz-Moreno, J.; Polo-Luque, M.-L.; Rodríguez-Puyol, D. Medical Prognosis of Infectious Diseases in Nursing Homes by Applying Machine Learning on Clinical Data Collected in Cloud Microservices. Int. J. Environ. Res. Public Health 2021, 18, 13278. [Google Scholar] [CrossRef] [PubMed]
- Zachos, G.; Essop, I.; Mantas, G.; Porfyrakis, K.; Ribeiro, J.C.; Rodriguez, J. An Anomaly-Based Intrusion Detection System for Internet of Medical Things Networks. Electronics 2021, 10, 2562. [Google Scholar] [CrossRef]

| Age (Years Old) | Systolic BP | Diastolic BP | Time (s) | Emotion Type | |||
|---|---|---|---|---|---|---|---|
| Microcontroller | Omron | Microcontroller | Omron | Microcontroller | Omron | ||
| 20 | 126 | 120 | 80 | 80 | 21 | 20 | Neutral (calm) |
| 40 | 120 | 120 | 80 | 80 | 25 | 21 | |
| 60 | 121 | 121 | 80 | 80 | 25 | 20 | |
| 20 | 133 | 131 | 82 | 85 | 23 | 22 | Angry |
| 40 | 155 | 150 | 94 | 91 | 24 | 21 | |
| 60 | 153 | 153 | 105 | 100 | 26 | 20 | |
| 20 | 113 | 113 | 75 | 75 | 26 | 20 | Sad |
| 40 | 95 | 95 | 65 | 70 | 24 | 23 | |
| 60 | 98 | 98 | 70 | 70 | 25 | 23 | |
| 20 | 126 | 120 | 81 | 81 | 26 | 21 | Happy |
| 40 | 120 | 120 | 79 | 80 | 24 | 20 | |
| 60 | 120 | 120 | 81 | 80 | 23 | 21 | |
| 20 | 115 | 115 | 62 | 60 | 24 | 20 | Fearful |
| 40 | 155 | 159 | 96 | 92 | 24 | 20 | |
| 60 | 139 | 144 | 90 | 94 | 24 | 21 | |
| Age (Years Old) | Heart Rate (Pulse Per min) | Time (s) | Emotion Type | ||
|---|---|---|---|---|---|
| Microcontroller | Omron | Microcontroller | Omron | ||
| 20 | 75 | 80 | 21 | 20 | Neutral (calm) |
| 40 | 85 | 80 | 21 | 20 | |
| 60 | 90 | 79 | 25 | 21 | |
| 20 | 96 | 95 | 20 | 20 | Angry |
| 40 | 110 | 100 | 21 | 20 | |
| 60 | 95 | 99 | 26 | 20 | |
| 20 | 74 | 70 | 28 | 22 | Sad |
| 40 | 69 | 66 | 25 | 21 | |
| 60 | 61 | 64 | 18 | 20 | |
| 20 | 80 | 80 | 19 | 20 | Happy |
| 40 | 89 | 81 | 23 | 23 | |
| 60 | 79 | 79 | 21 | 20 | |
| 20 | 92 | 95 | 21 | 20 | Fearful |
| 40 | 99 | 92 | 21 | 20 | |
| 60 | 100 | 100 | 21 | 20 | |
| Age (Years Old) | Temperature Measurements (Degrees Celsius) | Time (s) | Emotion Type | ||
|---|---|---|---|---|---|
| Microcontroller | Reference Value | Microcontroller | Reference Value | ||
| 20 | 36.9 | 36.5 | 60 | 60 | Neutral (calm) |
| 40 | 37 | 36.8 | 60 | 60 | |
| 20 | 37 | 37.5 | 60 | 60 | Angry |
| 40 | 37.2 | 37.6 | 60 | 60 | |
| 20 | 36.1 | 36.5 | 60 | 60 | Sad |
| 40 | 36.4 | 36.6 | 60 | 60 | |
| 20 | 37.2 | 37 | 60 | 60 | Happy |
| 40 | 36.9 | 36.8 | 60 | 60 | |
| 20 | 36.5 | 36.3 | 60 | 60 | Fearful |
| 40 | 36.5 | 36.2 | 60 | 60 | |
| Age (Years Old) | R (kOhms) | (Volt) | (Volt) | Emotion |
|---|---|---|---|---|
| 20 | 1.00E+05 | 0.291 | 4.993 | neutral |
| 60 | 3.80E+05 | 0.812 | 3.992 | |
| 20 | 6.10E+05 | 0.664 | 3.942 | angry |
| 60 | 1.30E+06 | 0.881 | 3.767 | |
| 20 | 2.60E+06 | 0.983 | 3.197 | sad |
| 60 | 5.80E+06 | 1.667 | 2.743 | |
| 20 | 2.00E+07 | 2.141 | 2.083 | happy |
| 60 | 3.80E+07 | 2.551 | 1.677 | |
| 20 | 6.60E+05 | 0.464 | 3.642 | fearful |
| 60 | 1.00E+06 | 0.581 | 3.467 |
| Normal People (ppm) | People Exposed to Methane (ppm) |
|---|---|
| 5.44 | 1003 |
| 2.23 | 560.40 |
| 0.811 | 283.25 |
| 2.91 | 854 |
| 2.72 | 776.9 |
| Normal People (ppm) | People Exposed to Alcohol (ppm) |
|---|---|
| 0.85 | 498 |
| 1.00 | 325 |
| 0.98 | 315 |
| 1.01 | 328 |
| 0.88 | 300 |
| Normal People (ppm) | People Exposed to Natural Gas (ppm) |
|---|---|
| 40 | 798 |
| 39 | 802 |
| 29 | 850 |
| 20 | 791 |
| 25 | 815 |
| Normal People (ppm) | People Exposed to Carbon Monoxide (ppm) |
|---|---|
| 100.1 | 600 |
| 125.02 | 506 |
| 89.07 | 340.40 |
| 90.22 | 390 |
| 50.65 | 429 |
| Normal People (ppm) | People Exposed to Hydrogen (ppm) |
|---|---|
| 4.7 | 50 |
| 6.8 | 54 |
| 7.6 | 68 |
| 5.4 | 62 |
| 8.7 | 70 |
| Attribute | Description |
|---|---|
| Br | Breath rate |
| HR | Heart rate |
| TEMP | Body temperature |
| Temp Sensor | Breath Sensor | Pulse Sensor Per min | Action | Risk Level |
|---|---|---|---|---|
| <37 °C | 89–98% | 60 to 115 | No action | 1 |
| 37–38 °C | 70–88% | 40–59 or 116–120 | Inform family | 2 |
| <38 °C | 45–69% | 40–59 or 120–129 | Inform doctor | 3 |
| <38 °C | >45% | >40 or <130 | Critical | 4 |
| Criterion | NB | SVM | RF | SL | KNN |
|---|---|---|---|---|---|
| Accuracy | 90.40% | 98.56% | 95.98% | 95.65 | 87.39 |
| Sensitivity | 89.40 | 98.50 | 96.80 | 96.10 | 87.40 |
| F-score | 88.40 | 98.72 | 96.70 | 96.00 | 86.90 |
| Elements of Comparison | This Work (EGYXOS) | [1] | [2] | [3] | [5] | [6] | [8] | [13] | [17] | |
|---|---|---|---|---|---|---|---|---|---|---|
| Sensors | 9 | 3 | 1 | 1 (Camera) | 1 | 3 | 2 | 2 | 3 | |
| Datasets | Group of 500 people | Group of 400 people | n/a | From 200–400 | 12 | 5 | n/a | n/a | n/a | |
| DAQ circuit | yes | n/a | n/a | n/a | yes | n/a | n/a | n/a | n/a | |
| Noise-cancellation circuit | yes | n/a | n/a | n/a | No | n/a | n/a | n/a | n/a | |
| The number of emotions studied | 5 emotions (Photos–videos) | n/a | 3 emotions (Photos only) | 5 emotions (Photos only) | 1 | n/a | n/a | n/a | n/a | |
| Integration of more than one database of vital parameters | yes | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| The blood gas measurement system is integrated with the vital parameter measurement system | yes | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| Machine learning algorithms used | 5 | n/a | n/a | 1 | 9 | n/a | 1 | n/a | 1 | |
| IoT | app | yes | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| web interface | yes | n/a | n/a | n/a | n/a | yes | yes | yes | Yes | |
| Parameters | Heart Rate | Blood Pressure (Diastolic) | Blood Pressure (Systolic) | Temperature | ||||
|---|---|---|---|---|---|---|---|---|
| Reference Device | This Work (EGYXOS) | Reference Device | This Work (EGYXOS) | Reference Device | This Work (EGYXOS) | Reference Device | This Work (EGYXOS) | |
| Min | 75 | 75.3 | 80 | 80 | 75 | 76 | 77 | 77 |
| Max | 98 | 98 | 98 | 95 | 98 | 98 | 99 | 99 |
| Mean | 86.5 | 85.3 | 87.8 | 86.9 | 86 | 87 | 87.9 | 87.9 |
| Median | 86.5 | 85.9 | 88.5 | 88 | 86.5 | 86.5 | 88.7 | 88.7 |
| Heart Rate | Blood Pressure (Diastolic) | Blood Pressure (Systolic) | Temperature | |
|---|---|---|---|---|
| Percentage Error | 0.9249% | 1.6185% | 0.911% | 0.1138% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abd Elgawad, Y.Z.; Youssef, M.I.; Nasser, T.M.; Almslmany, A.; S. I. Amar, A.; Mohamed, A.A.; Parchin, N.O.; Abd-Alhameed, R.A.; Mohamed, H.G.; Moussa, K.H. New Method to Implement and Analysis of Medical System in Real Time. Healthcare 2022, 10, 1357. https://doi.org/10.3390/healthcare10071357
Abd Elgawad YZ, Youssef MI, Nasser TM, Almslmany A, S. I. Amar A, Mohamed AA, Parchin NO, Abd-Alhameed RA, Mohamed HG, Moussa KH. New Method to Implement and Analysis of Medical System in Real Time. Healthcare. 2022; 10(7):1357. https://doi.org/10.3390/healthcare10071357
Chicago/Turabian StyleAbd Elgawad, Yahia Zakria, Mohamed I. Youssef, Tarek Mahmoud Nasser, Amir Almslmany, Ahmed S. I. Amar, Abdelrhman Adel Mohamed, Naser Ojaroudi Parchin, Raed A. Abd-Alhameed, Heba G. Mohamed, and Karim H. Moussa. 2022. "New Method to Implement and Analysis of Medical System in Real Time" Healthcare 10, no. 7: 1357. https://doi.org/10.3390/healthcare10071357
APA StyleAbd Elgawad, Y. Z., Youssef, M. I., Nasser, T. M., Almslmany, A., S. I. Amar, A., Mohamed, A. A., Parchin, N. O., Abd-Alhameed, R. A., Mohamed, H. G., & Moussa, K. H. (2022). New Method to Implement and Analysis of Medical System in Real Time. Healthcare, 10(7), 1357. https://doi.org/10.3390/healthcare10071357









