Factors Affecting Korean Medicine Health Care Use for Functional Dyspepsia: Analysis of the Korea Health Panel Survey 2017
Abstract
:1. Introduction
2. Materials and Methods
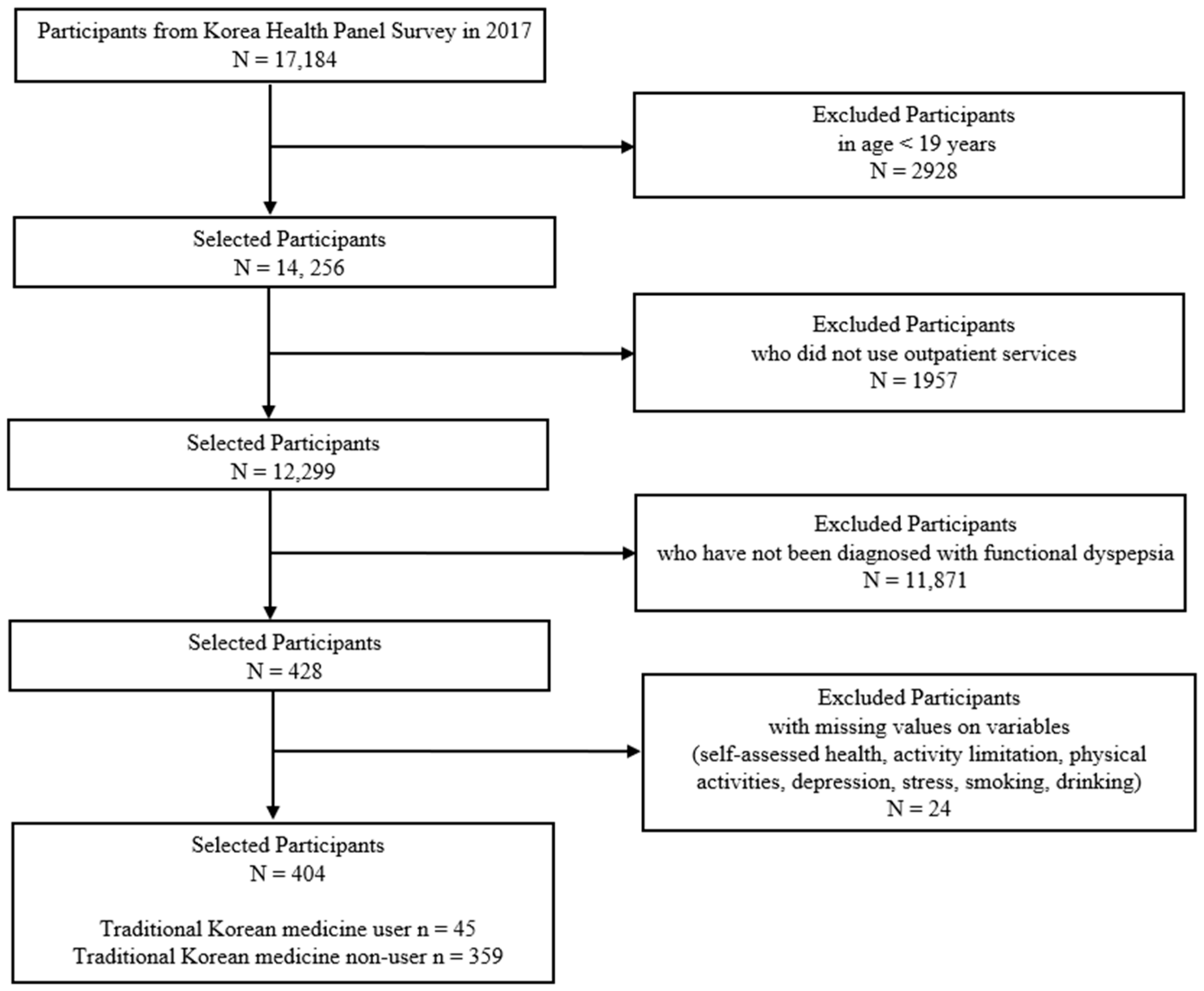
2.1. Data source and Study Participants
2.2. Definitions
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. General Participant Characteristics
3.2. Factors Affecting KMHC Use for FD
3.3. Predictive Powers of the Predisposing, Enabling, and Need Factors for KMHC Use to Treat FD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stanghellini, V.; Chan, F.K.; Hasler, W.L.; Malagelada, J.R.; Suzuki, H.; Tack, J.; Talley, N.J. Gastroduodenal disorders. Gastroenterology 2016, 150, 1380–1392. [Google Scholar] [CrossRef] [PubMed]
- Mahadeva, S.; Goh, K.L. Epidemiology of functional dyspepsia: A global perspective. World J. Gastroenterol. 2006, 12, 2661–2666. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.E.; Kim, N.; Lee, J.Y.; Park, K.S.; Shin, J.E.; Nam, K.; Kim, H.J.; Song, H.J.; Joo, Y.E.; Myung, D.S.; et al. Prevalence and Risk Factors of Functional Dyspepsia in Health Check-up Population: A Nationwide Multicenter Prospective Study. J. Neurogastroenterol. Motil. 2018, 24, 603–613. [Google Scholar] [CrossRef] [PubMed]
- Lacy, B.E.; Weiser, K.T.; Kennedy, A.T.; Crowell, M.D.; Talley, N.J. Functional dyspepsia: The economic impact to patients. Aliment. Pharmacol. Ther. 2013, 38, 170–177. [Google Scholar] [CrossRef]
- Chiarioni, G.; Pesce, M.; Fantin, A.; Sarnelli, G. Complementary and alternative treatment in functional dyspepsia. United Eur. Gastroenterol. J. 2018, 6, 5–12. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Fan, X.; Qu, H.; Gao, X.; Cheng, Y. Strategies and techniques for multi-component drug design from medicinal herbs and traditional Chinese medicine. Curr. Top. Med. Chem. 2012, 12, 1356–1362. [Google Scholar] [CrossRef]
- Chu, M.H.K.; Wu, I.X.Y.; Ho, R.S.T.; Wong, C.H.L.; Zhang, A.L.; Zhang, Y.; Wu, J.C.Y.; Chung, V.C.H. Chinese herbal medicine for functional dyspepsia: Systematic review of systematic reviews. Therap. Adv. Gastroenterol. 2018, 11, 1–24. [Google Scholar] [CrossRef]
- Health Insurance Review & Assessment Service. Healthcare Bigdata Hub. ‘Statistics of Frequent Diseases’. Available online: http://opendata.hira.or.kr/op/opc/olapHifrqSickInfo.do (accessed on 10 April 2022).
- Hajek, A.; Bock, J.O.; König, H.H. Which factors affect health care use among older Germans? Results of the German ageing survey. BMC Health Serv. Res. 2017, 17, 30. [Google Scholar] [CrossRef] [Green Version]
- Chung, V.C.; Wong, C.H.; Wu, I.X.; Ching, J.Y.; Cheung, W.K.; Yip, B.H.; Chan, K.L.; Cheong, P.K.; Wu, J.C. Electroacupuncture plus on-demand gastrocaine for refractory functional dyspepsia: Pragmatic randomized trial. J. Gastroenterol. Hepatol. 2019, 34, 2077–2085. [Google Scholar] [CrossRef]
- Lee, B.; Ahn, E.K.; Yang, C. Herbal Medicine Prescriptions for Functional Dyspepsia: A Nationwide Population-Based Study in Korea. Evid. Based Complement. Alternat. Med. 2022, 2022, 3306420. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Hirshfield, S.; Downing, M.J., Jr.; Horvath, K.J.; Swartz, J.A.; Chiasson, M.A. Adapting Andersen’s Behavioral Model of Health Service Use to Examine Risk Factors for Hypertension among U.S. MSM. Am. J. Men’s Health 2018, 12, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.; Seo, N.; Go, S.; Han, E.; Park, S.; Jung, Y.; Lee, J.; Hwang, Y. A Report on the Korea Health Panel Survey of 2008; Korea Institute for Health and Social Affairs: Seoul, Korea, 2010. [Google Scholar]
- Andersen, R.; Newman, J.F. Societal and individual determinants of medical care utilization in the United States. Milbank Mem. Fund. Q. Health Soc. 1973, 51, 95–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, R. A Behavioral Model of Families’ Use of Health Services; Center for Health Administration Studies: Chicago, IL, USA, 1968. [Google Scholar]
- World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; WHO: Geneva, Switzerland, 2000.
- Fox, J.; Monette, G. Generalized collinearity diagnostics. J. Am. Stat. Assoc. 1992, 87, 178–183. [Google Scholar] [CrossRef]
- LeDell, E.; Petersen, M.; van der Laan, M. Computationally efficient confidence intervals for cross-validated area under the ROC curve estimates. Electron. J. Stat. 2015, 9, 1583. [Google Scholar] [CrossRef]
- Geisser, S. The predictive sample reuse method with applications. J. Am. Stat. Assoc. 1975, 70, 320–328. [Google Scholar] [CrossRef]
- Stone, M. Cross-validatory choice and assessment of statistical predictions. J. R. Stat. Soc. Ser. B (Methodol.) 1974, 36, 111–147. [Google Scholar] [CrossRef]
- Hanley, J.A.; McNeil, B.J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982, 143, 29–36. [Google Scholar] [CrossRef] [Green Version]
- Ju, Y.J.; Kim, T.H.; Han, K.T.; Lee, H.J.; Kim, W.; Ah Lee, S.; Park, E.C. Association between unmet healthcare needs and health-related quality of life: A longitudinal study. Eur. J. Public Health 2017, 27, 631–637. [Google Scholar] [CrossRef] [Green Version]
- Lee, W.J.; Han, C.H.; Yang, C.; Lee, S.H.; Kim, D.; Ha, I.; Song, H.J.; Lee, Y.J. Analysis of outpatient expenditure trends using Korean Health Panel Survey data of patients diagnosed with lumbar intervertebral disc herniation. J. Int. Med. Res. 2021, 49, 03000605211051583. [Google Scholar] [CrossRef]
- Ford, A.C.; Marwaha, A.; Sood, R.; Moayyedi, P. Global prevalence of, and risk factors for, uninvestigated dyspepsia: A meta-analysis. Gut 2015, 64, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.; Heo, S.; Kim, D.; Kang, S.; Woo, J.M. Changes in trust and the use of Korean medicine in South Korea: A comparison of surveys in 2011 and 2014. BMC Complement. Altern. Med. 2017, 17, 463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sackett, K.; Carter, M.; Stanton, M. Elders’ use of folk medicine and complementary and alternative therapies: An integrative review with implications for case managers. Prof. Case Manag. 2014, 19, 113–123, quiz 124–115. [Google Scholar] [CrossRef] [PubMed]
- Boon, H.; Stewart, M.; Kennard, M.A.; Gray, R.; Sawka, C.; Brown, J.B.; McWilliam, C.; Gavin, A.; Baron, R.A.; Aaron, D.; et al. Use of complementary/alternative medicine by breast cancer survivors in Ontario: Prevalence and perceptions. J. Clin. Oncol. 2000, 18, 2515–2521. [Google Scholar] [CrossRef]
- Astin, J.A. Why patients use alternative medicine: Results of a national study. JAMA 1998, 279, 1548–1553. [Google Scholar] [CrossRef] [Green Version]
- Jung, B.; Kim, J.; Ha, I.H.; Lee, J. Factors affecting utilisation of traditional Korean medical services by privately insured persons: A retrospective study using Korean Health Panel Survey (KHPS). BMJ Open 2020, 10, e033159. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.J.; Lee, J. Effect of private health insurance on health care utilization in a universal health insurance system: A case of South Korea. Korea J. Hosp. Manag. 2018, 23, 42–53. [Google Scholar]
- Park, S.B.; Jeong, K.H. The determinants of private health insurance and its effects on medical utilization in Korea. Korean Insur. Acad. Soc. 2011, 88, 23–49. [Google Scholar]
- You, C.H.; Kang, S.W.; Kwon, Y.D.; Oh, E.H. The effects of supplementary private health insurance on healthcare utilization and expenditures: Indemnity vs. fixed-benefit. Korean Soc. Secur. Stud. 2011, 27, 277–292. [Google Scholar]
- Ministry of Health and Welfare, National Institute for Korean Medicine Development, Gallup. Basic Report on the Use of Traditional Korean Medicine in 2020; Ministry of Health and Welfare, National Institute for Korean Medicine Development, Gallup: Seoul, Korea, 2021; p. 58.
- National Institute for Korean Medicine Development. Korean Medicine Clinical Practice Guideline for Functional Dyspepsia; Koonja Publishing Inc.: Seoul, Korea, 2021.
- Deding, U.; Torp-Pedersen, C.; Bøggild, H. Perceived stress as a risk factor for dyspepsia: A register-based cohort study. Eur. J. Gastroenterol. Hepatol. 2017, 29, 560–567. [Google Scholar] [CrossRef] [Green Version]
- Nam, Y.; Kwon, S.C.; Lee, Y.J.; Jang, E.C.; Ahn, S.H. Relationship between job stress and functional dyspepsia in display manufacturing sector workers: A cross-sectional study. Ann. Occup. Environ. Med. 2018, 30, 62. [Google Scholar] [CrossRef] [PubMed]
- Song, T. An Anderson model approach to the mediation effect of stress vulnerability factors on the use of outpatient care by the elderly. Health Soc. Welf. Rev. 2013, 33, 547–576. [Google Scholar]
- Pirraglia, P.A.; Hampton, J.M.; Rosen, A.B.; Witt, W.P. Psychological distress and trends in healthcare expenditures and outpatient healthcare. Am. J. Manag. Care 2011, 17, 319–328. [Google Scholar] [PubMed]
- Lee, M.S.; Park, K.W.; Moon, S.R. Effects of a Korean traditional herbal remedy on psychoneuroendocrine responses to examination stress in medical students: A randomized placebo-controlled trial. Hum. Psychopharmacol. 2004, 19, 537–543. [Google Scholar] [CrossRef]
| Variables | KMHC Use of Functional Dyspepsia | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Non-Use | Use | ||||||
| Total | % | N | % | N | % | ||
| Number of participants | 404 | 359 | 45 | ||||
| Predisposing factors | |||||||
| Sex | 0.16 | ||||||
| Men | 132 | 32.67 | 122 | 33.98 | 10 | 22.22 | |
| Women | 272 | 67.33 | 237 | 66.02 | 35 | 77.78 | |
| Age (years) | <0.001 | ||||||
| 19–34 | 30 | 7.43 | 22 | 6.13 | 8 | 17.78 | |
| 35–49 | 72 | 17.82 | 61 | 16.99 | 11 | 24.44 | |
| 50–64 | 102 | 25.25 | 86 | 23.96 | 16 | 35.56 | |
| 65 or older | 200 | 49.50 | 190 | 52.92 | 10 | 22.22 | |
| Education | <0.01 | ||||||
| Elementary school or below | 139 | 34.41 | 132 | 36.77 | 7 | 15.56 | |
| Middle/high school | 190 | 47.03 | 166 | 46.24 | 24 | 53.33 | |
| College or above | 75 | 18.56 | 61 | 16.99 | 14 | 31.11 | |
| Region | 0.15 † | ||||||
| Seoul/Gyeonggi/Incheon | 163 | 40.35 | 145 | 40.39 | 18 | 40.00 | |
| Gangwon | 35 | 8.66 | 32 | 8.91 | 3 | 6.67 | |
| Daejeon/Chungcheong/Sejong | 69 | 17.08 | 63 | 17.55 | 6 | 13.33 | |
| Gwangju/Jeolla/Jeju | 48 | 11.88 | 46 | 12.81 | 2 | 4.44 | |
| Busan/Daegu/Ulsan/Gyeongsang | 89 | 22.03 | 73 | 20.33 | 16 | 35.56 | |
| Enabling factors | |||||||
| Household income | <0.01 † | ||||||
| 1st quintile (lowest) | 97 | 24.01 | 94 | 26.18 | 3 | 6.67 | |
| 2nd quintile | 99 | 24.50 | 93 | 25.91 | 6 | 13.33 | |
| 3rd quintile | 70 | 17.33 | 60 | 16.71 | 10 | 22.22 | |
| 4th quintile | 81 | 20.05 | 67 | 18.66 | 14 | 31.11 | |
| 5th quintile (highest) | 57 | 14.11 | 45 | 12.53 | 12 | 26.67 | |
| Employment status | 0.19 † | ||||||
| Unemployed | 226 | 55.94 | 206 | 57.38 | 20 | 44.44 | |
| Employed | 138 | 34.16 | 117 | 32.59 | 21 | 46.67 | |
| Self-employed | 40 | 9.90 | 36 | 10.03 | 4 | 8.89 | |
| Health insurance type | 0.24 † | ||||||
| Employee health insurance | 296 | 73.27 | 259 | 72.14 | 37 | 82.22 | |
| Local subscriber | 73 | 18.07 | 66 | 18.38 | 7 | 15.56 | |
| Medical aid or others | 35 | 8.66 | 34 | 9.47 | 1 | 2.22 | |
| Private health insurance | <0.01 | ||||||
| No | 137 | 33.91 | 131 | 36.49 | 6 | 13.33 | |
| Yes | 267 | 66.09 | 228 | 63.51 | 39 | 86.67 | |
| Number of household members | 0.34 | ||||||
| 1 | 64 | 16.70 | 58 | 16.16 | 6 | 13.33 | |
| 2 | 163 | 42.72 | 149 | 41.50 | 14 | 31.11 | |
| 3 | 67 | 17.23 | 59 | 16.43 | 8 | 17.78 | |
| 4 or more | 110 | 23.34 | 93 | 25.91 | 17 | 37.78 | |
| Need factor | |||||||
| Disability | 0.40 † | ||||||
| No | 370 | 91.58 | 327 | 91.09 | 43 | 95.56 | |
| Yes | 34 | 8.42 | 32 | 8.91 | 2 | 4.44 | |
| Self-assessed health | 0.08 | ||||||
| Poor | 95 | 23.51 | 87 | 24.23 | 8 | 17.78 | |
| Fair | 180 | 44.55 | 164 | 45.68 | 16 | 35.56 | |
| Good | 129 | 31.93 | 108 | 30.08 | 21 | 46.67 | |
| Number of chronic diseases | <0.05 † | ||||||
| 0 | 140 | 34.65 | 116 | 32.31 | 24 | 53.33 | |
| 1 | 90 | 22.28 | 82 | 22.84 | 8 | 17.78 | |
| 2 | 84 | 20.79 | 76 | 21.17 | 8 | 17.78 | |
| 3 or more | 90 | 22.28 | 85 | 23.68 | 5 | 11.11 | |
| Depressed mood | 0.76 † | ||||||
| No | 374 | 92.57 | 333 | 92.76 | 41 | 91.11 | |
| Yes | 30 | 7.43 | 26 | 7.24 | 4 | 8.89 | |
| Stress | 0.10 † | ||||||
| Never or rarely | 324 | 80.20 | 287 | 79.94 | 37 | 82.22 | |
| Sometimes | 49 | 12.13 | 47 | 13.09 | 2 | 4.44 | |
| Frequently or always | 31 | 7.67 | 25 | 6.96 | 6 | 13.33 | |
| BMI (kg/m2) | 0.61 † | ||||||
| <18.5 | 21 | 5.20 | 19 | 5.29 | 2 | 4.44 | |
| 18.5–22.9 | 179 | 44.31 | 154 | 42.90 | 25 | 55.56 | |
| 23.0–24.9 | 117 | 28.96 | 107 | 29.81 | 10 | 22.22 | |
| 25.0–29.9 | 78 | 19.31 | 71 | 19.78 | 7 | 15.56 | |
| ≥30 | 9 | 2.23 | 8 | 2.23 | 1 | 2.22 | |
| Smoking | 0.24 † | ||||||
| Never smoked | 300 | 74.26 | 262 | 72.98 | 38 | 84.44 | |
| Quit smoking | 71 | 17.57 | 67 | 18.66 | 4 | 8.89 | |
| Smoking | 33 | 8.17 | 30 | 8.36 | 3 | 6.67 | |
| Drinking | 0.29 † | ||||||
| Never drunk | 136 | 33.66 | 119 | 33.15 | 17 | 37.78 | |
| Monthly or less | 146 | 36.14 | 132 | 36.77 | 14 | 31.11 | |
| 2 to 4 times a month | 69 | 17.08 | 58 | 16.16 | 11 | 24.44 | |
| 2 times a week or more | 53 | 13.12 | 50 | 13.93 | 3 | 6.67 | |
| Physical activities | 0.52 | ||||||
| Not at all | 273 | 67.57 | 245 | 68.25 | 28 | 62.22 | |
| Once a week or more | 131 | 32.43 | 114 | 31.75 | 17 | 37.78 | |
| Variables | Crude | Adjusted 1 | Adjusted 2 | Adjusted 3 | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Predisposing factors | ||||||||
| Sex | ||||||||
| Men | 1 | 1 | 1 | 1 | ||||
| Women | 1.8 (0.86–3.76) | 0.12 | 1.78 (0.82–3.88) | 0.15 | 1.86 (0.79–4.39) | 0.16 | 1.82 (0.47–7.01) | 0.38 |
| Age (years) | ||||||||
| 19–34 | 1 | 1 | 1 | 1 | ||||
| 35–49 | 0.5 (0.18–1.39) | 0.18 | 0.44 (0.15–1.31) | 0.14 | 0.39 (0.13–1.22) | 0.11 | 0.42 (0.11–1.55) | 0.19 |
| 50–64 | 0.51 (0.19–1.35) | 0.16 | 0.52 (0.18–1.52) | 0.23 | 0.4 (0.12–1.3) | 0.13 | 0.26 (0.06–1.1) | 0.07 |
| 65 or older | 0.14 (0.05–0.4) | <0.001 | 0.19 (0.05–0.7) | <0.05 | 0.23 (0.05–1.1) | 0.07 | 0.14 (0.02–0.93) | <0.05 |
| Education | ||||||||
| Elementary or below | 1 | 1 | 1 | 1 | ||||
| Middle/high school | 2.73 (1.14–6.52) | <0.05 | 1.7 (0.6–4.79) | 0.31 | 1.53 (0.51–4.53) | 0.45 | 1.98 (0.58–6.83) | 0.28 |
| College or above | 4.33 (1.66–11.26) | <0.01 | 1.98 (0.56–7.03) | 0.29 | 1.74 (0.46–6.55) | 0.41 | 2.38 (0.54–10.43) | 0.25 |
| Region | ||||||||
| Seoul/Gyeonggi/Incheon | 1 | 1 | 1 | 1 | ||||
| Gangwon | 0.76 (0.21–2.72) | 0.67 | 0.98 (0.26–3.69) | 0.97 | 0.85 (0.21–3.45) | 0.82 | 0.94 (0.21–4.16) | 0.93 |
| Daejeon/Chungcheong/Sejong | 0.77 (0.29–2.02) | 0.59 | 1.22 (0.44–3.4) | 0.70 | 1.48 (0.5–4.35) | 0.48 | 1.36 (0.41–4.53) | 0.61 |
| Gwangju/Jeolla/Jeju | 0.35 (0.08–1.57) | 0.17 | 0.49 (0.11–2.28) | 0.37 | 0.55 (0.11–2.66) | 0.46 | 0.44 (0.08–2.46) | 0.35 |
| Busan/Daegu/Ulsan/Gyeongsang | 1.76 (0.85–3.66) | 0.13 | 2.29 (1.06–4.92) | <0.05 | 2.53 (1.14–5.61) | <0.05 | 2.45 (1.02–5.88) | <0.05 |
| Enabling factors | ||||||||
| Household income | ||||||||
| 1st quintile (lowest) | 1 | 1 | 1 | |||||
| 2nd quintile | 2.02 (0.49–8.32) | 0.33 | 1.15(0.23–5.62) | 0.87 | 1.11 (0.2–6.27) | 0.91 | ||
| 3rd quintile | 5.22 (1.38–19.76) | <0.05 | 3 (0.62–14.61) | 0.17 | 2.72 (0.5–14.77) | 0.25 | ||
| 4th quintile | 6.55 (1.81–23.68) | <0.01 | 2.98 (0.56–15.99) | 0.20 | 3.13 (0.51–19.16) | 0.22 | ||
| 5th quintile (highest) | 8.36 (2.25–31.07) | <0.01 | 4.19 (0.73–23.87) | 0.11 | 4 (0.6–26.45) | 0.15 | ||
| Employment status | ||||||||
| Unemployed | 1 | 1 | 1 | |||||
| Employed | 1.85 (0.96–3.55) | 0.07 | 0.97 (0.43–2.19) | 0.95 | 0.89 (0.37–2.18) | 0.80 | ||
| Self-employed | 1.14 (0.37–3.55) | 0.82 | 2.2 (0.6–8.11) | 0.24 | 1.85 (0.42–8.11) | 0.42 | ||
| Health insurance type | ||||||||
| Employee health insurance | 1 | 1 | 1 | |||||
| Local-subscriber health insurance | 0.74 (0.32–1.74) | 0.49 | 1 (0.39–2.61) | 0.99 | 0.95 (0.34–2.71) | 0.93 | ||
| Medical aid or others | 0.21 (0.03–1.55) | 0.13 | 0.44 (0.05–3.97) | 0.46 | 0.3 (0.03–3.51) | 0.34 | ||
| Private health insurance | ||||||||
| No | 1 | 1 | 1 | |||||
| Yes | 3.74 (1.54–9.06) | <0.01 | 2.09 (0.72–6.06) | 0.17 | 3.41 (1.02–11.42) | <0.05 | ||
| Number of household members | ||||||||
| 1 | 1 | 1 | 1 | |||||
| 2 | 0.91 (0.33–2.48) | 0.85 | 0.65 (0.2–2.14) | 0.48 | 0.53 (0.14–1.91) | 0.33 | ||
| 3 | 1.31 (0.43–4.02) | 0.64 | 0.32 (0.08–1.3) | 0.11 | 0.26 (0.05–1.22) | 0.09 | ||
| 4 or more | 1.77 (0.66–4.73) | 0.26 | 0.35 (0.09–1.28) | 0.11 | 0.28 (0.07–1.17) | 0.08 | ||
| Need factor | ||||||||
| Disability | ||||||||
| No | 1 | 1 | ||||||
| Yes | 0.48 (0.11–2.05) | 0.32 | 1.19 (0.17–8.2) | 0.86 | ||||
| Self-assessed health | ||||||||
| Poor | 1 | 1 | ||||||
| Fair | 1.06 (0.44–2.58) | 0.90 | 0.72 (0.23–2.26) | 0.57 | ||||
| Good | 2.11 (0.89–5.01) | 0.09 | 1.07 (0.32–3.53) | 0.92 | ||||
| Number of chronic diseases | ||||||||
| 0 | 1 | 1 | ||||||
| 1 | 0.47 (0.2–1.1) | 0.08 | 0.98 (0.34–2.88) | 0.98 | ||||
| 2 | 0.51 (0.22–1.19) | 0.12 | 1.71 (0.49–6.03) | 0.40 | ||||
| 3 or more | 0.28 (0.1–0.78) | <0.01 | 0.94 (0.22–4.03) | 0.93 | ||||
| Depressed mood | ||||||||
| No | 1 | 1 | ||||||
| Yes | 1.25 (0.42–3.76) | 0.69 | 2.39 (0.56–10.16) | 0.24 | ||||
| Stress | ||||||||
| Never or rarely | 1 | 1 | ||||||
| Sometimes | 0.33 (0.08–1.42) | 0.14 | 0.26 (0.05–1.37) | 0.11 | ||||
| Frequently or always | 1.86 (0.72–4.83) | 0.20 | 3.26 (0.85–12.51) | 0.09 | ||||
| BMI (kg/m2) | ||||||||
| <18.5 | 1 | 1 | ||||||
| 18.5–22.9 | 1.54 (0.34–7.03) | 0.58 | 1.35 (0.22–8.18) | 0.74 | ||||
| 23.0–24.9 | 0.89 (0.18–4.38) | 0.88 | 0.87 (0.13–5.97) | 0.88 | ||||
| 25.0–29.9 | 0.94 (0.18–4.88) | 0.94 | 1.07 (0.15–7.52) | 0.95 | ||||
| ≥30 | 1.19 (0.09–15.03) | 0.89 | 0.96 (0.03–27) | 0.98 | ||||
| Smoking | ||||||||
| Never smoked | 1 | 1 | ||||||
| Quit smoking | 0.41 (0.14–1.19) | 0.10 | 1.46 (0.24–8.96) | 0.68 | ||||
| Smoking | 0.69 (0.2–2.37) | 0.56 | 1 (0.14–7.13) | 0.99 | ||||
| Drinking | ||||||||
| Never drunk | 1 | 1 | ||||||
| Monthly or less | 0.74 (0.35–1.57) | 0.44 | 0.56 (0.22–1.46) | 0.24 | ||||
| 2 to 4 times a month | 1.33 (0.58–3.02) | 0.50 | 0.63 (0.21–1.9) | 0.41 | ||||
| 2 times a week or more | 0.42 (0.12–1.49) | 0.18 | 0.28 (0.05–1.47) | 0.13 | ||||
| Physical activities | ||||||||
| Not at all | 1 | 1 | ||||||
| Once a week or more | 1.3 (0.69–2.48) | 0.42 | 0.69 (0.31–1.56) | 0.38 | ||||
| Mean GVIF | 1.161 | 1.291 | 1.547 | |||||
| Model | Factor | Selected Variables | Mean GVIF | AUC (95% CI) | AIC |
|---|---|---|---|---|---|
| Model 1 | Predisposing | Sex, Age, Region | 1.022 | 0.701 (0.626–0.777) | 273.127 |
| Model 2 | Predisposing + Enabling | Sex, Age, Region, Private health insurance | 1.088 | 0.696 (0.623–0.768) | 272.558 |
| Model 3 | Predisposing + Enabling + Need | Sex, Age, Private health insurance, Stress | 1.138 | 0.709 (0.637–0.781) | 264.762 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, B.; Yang, C.; Yim, M.H. Factors Affecting Korean Medicine Health Care Use for Functional Dyspepsia: Analysis of the Korea Health Panel Survey 2017. Healthcare 2022, 10, 1192. https://doi.org/10.3390/healthcare10071192
Lee B, Yang C, Yim MH. Factors Affecting Korean Medicine Health Care Use for Functional Dyspepsia: Analysis of the Korea Health Panel Survey 2017. Healthcare. 2022; 10(7):1192. https://doi.org/10.3390/healthcare10071192
Chicago/Turabian StyleLee, Boram, Changsop Yang, and Mi Hong Yim. 2022. "Factors Affecting Korean Medicine Health Care Use for Functional Dyspepsia: Analysis of the Korea Health Panel Survey 2017" Healthcare 10, no. 7: 1192. https://doi.org/10.3390/healthcare10071192
APA StyleLee, B., Yang, C., & Yim, M. H. (2022). Factors Affecting Korean Medicine Health Care Use for Functional Dyspepsia: Analysis of the Korea Health Panel Survey 2017. Healthcare, 10(7), 1192. https://doi.org/10.3390/healthcare10071192






