Screening for Mild Cognitive Impairment in the Preoperative Setting: A Narrative Review
Abstract
:1. Background
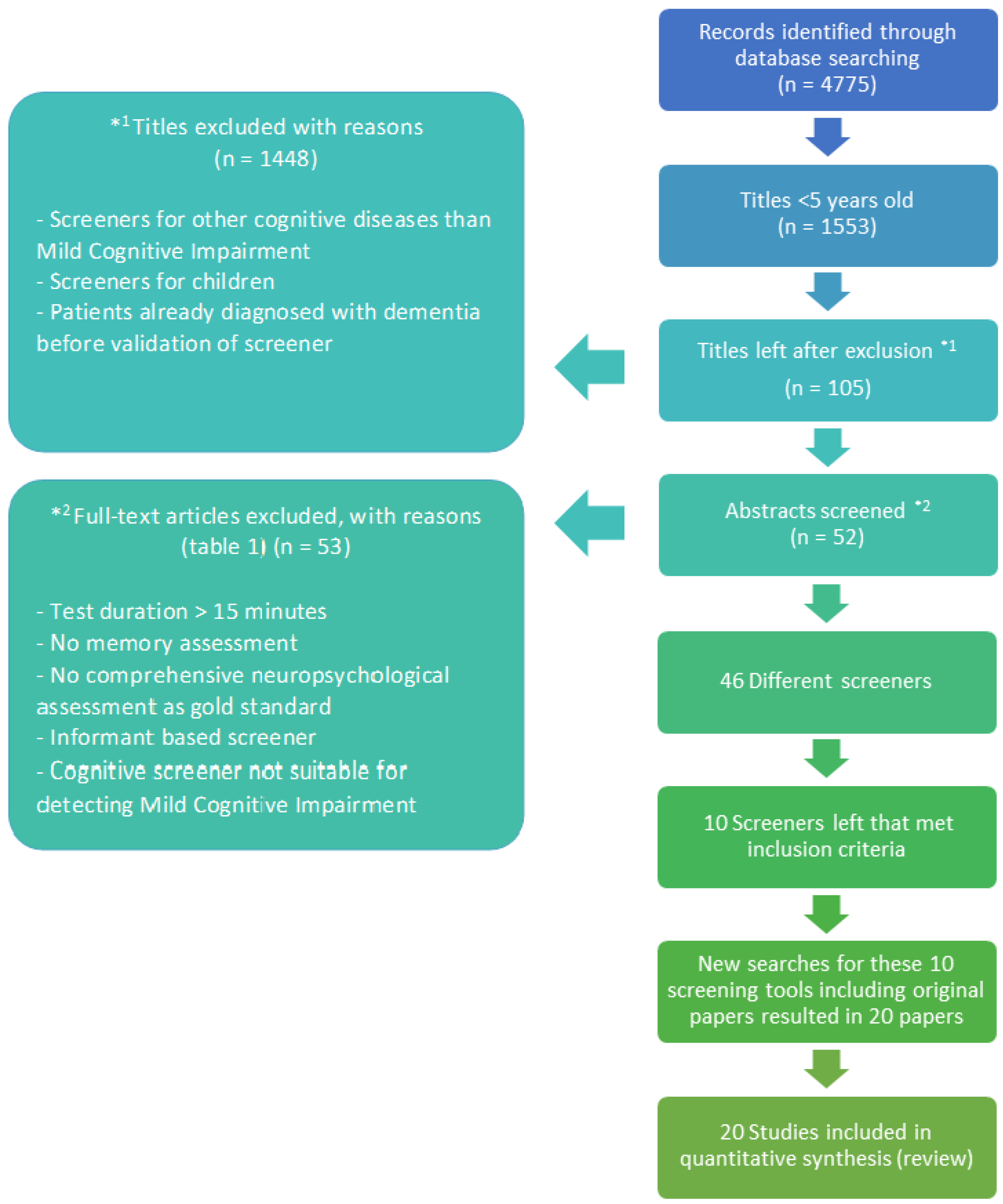
2. Methods
3. Results
4. Mini-Cog
5. Montreal Cognitive Assessment (MoCA)
6. Ottawa 3 Day Year (O3DY)
7. The 8-Item Interview to Ascertain Dementia (AD8)
8. Self-Administered Gerocognitive Examination (SAGE)
9. Saint Louis University Mental Status Examination (SLUMS)
10. Telephone Interview Cognitive Status (Modified) (TICS(-M))
11. Quick-MCI (QMCI)
12. Mini-Mental State Examination, 2nd Edition (MMSE-2)
13. Mini Addenbrooke’s Cognitive Examination (Mini-ACE/MACE)
14. Discussion
15. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AD | Alzheimer’s Disease |
| AD8 | The Washington University Dementia Screening Test, also known as “Eight-item Interview to Differentiate Aging and Dementia”/The 8-item interview to Ascertain Dementia (AD8) |
| CDR | Clinical Dementia Rating |
| CI | Cognitive Impairment |
| CT | Computed Tomography |
| DSM-IV/V | Diagnostic and Statistical Manual of Mental Disorders version IV/V |
| MCI | Mild Cognitive Impairment |
| MeSH | Medical Subject Headings |
| Mini-ACE | Mini Addenbrooke’s Cognitive Examination |
| MMSE | Mini-Mental State Examination |
| MMSE2 | Mini-Mental State Examination version 2 |
| MMSE2:BV | Mini-Mental State Examination version 2 Brief Version |
| MMSE2:EV | Mini-Mental State Examination version 2 Expanded Version |
| MMSE2:SV | Mini-Mental State Examination version 2 Standard Version |
| MoCA | Montreal Cognitive Assessment |
| O3DY | Ottawa 3 Day Year |
| POCD | Postoperative Cognitive Dysfunction |
| POD | Postoperative Delirium |
| QMCI | Quick MCI |
| ROC | Receiver operating characteristic |
| SAGE | Self-Administered Gerocognitive Exam |
| SLUMS | Saint Louis University Mental Status exam |
| STARDem | Standards for Reporting of Diagnostic Accuracy Studies (dementia) |
| TICS-(M) | Modified Telephone Interview for Cognitive Status |
References
- Lin, H.S.; McBride, R.L.; Hubbard, R.E. Frailty and Anesthesia—Risks during and Post-Surgery. Local Reg. Anesth. 2018, 11, 61–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 12 May 2020).
- Wengler, A.; Nimptsch, U.; Mansky, T. Hip and Knee Replacement in Germany and the USA. Dtsch. Arztebl. Int. 2014, 111, 407–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inouye, S.K.; Westendorp, R.G.J.; Saczynski, J.S. Delirium in Elderly People. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef] [Green Version]
- Collins, N.; Blanchard, M.R.; Tookman, A.; Sampson, E.L. Detection of Delirium in the Acute Hospital. Age Ageing 2009, 25, 131–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malik, A.; Harlan, T.; Cobb, J. Stop. Think. Delirium! A Quality Improvement Initiative to Explore Utilising a Validated Cognitive Assessment Tool in the Acute Inpatient Medical Setting to Detect Delirium and Prompt Early Intervention. J. Clin. Nurs. 2016, 25, 3400–3408. [Google Scholar] [CrossRef]
- Aldecoa, C.; Bettelli, G.; Bilotta, F.; Sanders, R.D.; Audisio, R.; Borozdina, A.; Cherubini, A.; Jones, C.; Kehlet, H.; Maclullich, A.; et al. European Society of Anaesthesiology Evidence-Based and Consensus-Based Guideline on Postoperative Delirium. Eur. J. Anaesthesiol. 2017, 34, 192–214. [Google Scholar] [CrossRef]
- Savage, S.; Ma, D. The Neurotoxicity of Nitrous Oxide: The Facts and “Putative” Mechanisms. Brain Sci. 2014, 4, 73–90. [Google Scholar] [CrossRef] [Green Version]
- Terrando, N.; Brzezinski, M.; Degos, V.; Eriksson, L.I.; Kramer, J.H.; Leung, J.M.; Miller, B.L.; Seeley, W.W.; Vacas, S.; Weiner, M.W.; et al. Perioperative Cognitive Decline in the Aging Population. Mayo Clin. Proc. 2011, 86, 885–893. [Google Scholar] [CrossRef] [Green Version]
- Bedford, P.D.; Leeds, M.R.C.P. Adverse Cerebral Effects of Anaesthesia on Old People. Lancet 1955, 6884, 259–264. [Google Scholar] [CrossRef]
- Kotekar, N.; Shenkar, A.; Nagaraj, R. Postoperative Cognitive Dysfunction—Current Preventive Strategies. Clin. Interv. Aging 2018, 13, 2267–2273. [Google Scholar] [CrossRef] [Green Version]
- Monk, T.G.; Weldon, B.C.; Garvan, C.W.; Dede, D.E.; van der Aa, M.T.; Heilman, K.M.; Gravenstein, J.S. Predictors of Cognitive Dysfunction after Major Noncardiac Surgery. Anesth. Analg. 2008, 108, 18–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Litaker, D.; Locala, J.; Franco, K.; Bronson, D.L.; Tannous, Z. Preoperative Risk Factors for Postoperative Delirium. Gen. Hosp. Psychiatry 2001, 23, 84–89. [Google Scholar] [CrossRef]
- Belrose, J.C.; Noppens, R.R. Anesthesiology and Cognitive Impairment: A Narrative Review of Current Clinical Literature. BMC Anesthesiol. 2019, 19, 241. [Google Scholar] [CrossRef] [PubMed]
- Tariq, S.H.; Tumosa, F.N.; Chibnall, J.T.; Perry, M.H.; Morley, J.E. Comparison of the Saint Louis University Mental Status Examination and the Mini-Mental State Examination for Detecting Dementia and Mild Neurocognitive Disorder—A Pilot Study. Am. J. Geriatr. Psychiatry 2006, 14, 900–910. [Google Scholar] [CrossRef] [PubMed]
- Stokin, G.B.; Krell-Roesch, J.; Petersen, R.C.; Geda, Y.E. Mild Neurocognitive Disorder: An Old Wine in a New Bottle. Harv. Rev. Psychiatry 2015, 23, 368. [Google Scholar] [CrossRef] [Green Version]
- Langa, K.M.; Levine, D.A. The Diagnosis and Management of Mild Cognitive Impairment: A Clinical Review. JAMA—J. Am. Med. Assoc. 2014, 312, 2551–2561. [Google Scholar] [CrossRef]
- Petersen, R.C. Mild Cognitive Impairment as a Diagnostic Entity. J. Intern. Med. 2004, 256, 183–194. [Google Scholar] [CrossRef]
- Sprung, J.; Roberts, R.O.; Knopman, D.S.; Petersen, R.C.; Weingarten, T.N.; Schroeder, D.R.; Warner, D.O. Perioperative Delirium and Mild Cognitive Impairment. Mayo Clin. Proc. 2016, 91, 273–274. [Google Scholar] [CrossRef] [Green Version]
- Sprung, J.; Roberts, R.O.; Weingarten, T.N.; Cavalcante, A.N.; Knopman, D.S.; Petersen, R.C.; Hanson, A.C.; Schroeder, D.R.; Warner, D.O. Postoperative Delirium in Elderly Patients Is Associated with Subsequent Cognitive Impairment. Br. J. Anaesth. 2017, 119, 316–323. [Google Scholar] [CrossRef]
- Axley, M.S.; Schenning, K.J. Preoperative Cognitive and Frailty Screening in the Geriatric Surgical Patient: A Narrative Review. Clin. Ther. 2015, 37, 2666–2675. [Google Scholar] [CrossRef] [Green Version]
- Saczynski, J.S.; Marcantonio, E.R.; Quach, L.; Fong, T.G.; Gross, A.; Inouye, S.K.; Jones, R.N. Cognitive Trajectories after Postoperative Delirium. N. Engl. J. Med. 2012, 367, 30–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saleh, A.J.; Tang, G.X.; Hadi, S.M.; Yan, L.; Chen, M.H.; Duan, K.M.; Tong, J.; Ouyang, W. Preoperative Cognitive Intervention Reduces Cognitive Dysfunction in Elderly Patients after Gastrointestinal Surgery: A Randomized Controlled Trial. Med. Sci. Monit. 2015, 21, 798–805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, T.; Chignell, M.; Tierney, M.C.; Lee, J. A Serious Game for Clinical Assessment of Cognitive Status: Validation Study. JMIR Serious Games 2016, 4, e7. [Google Scholar] [CrossRef] [PubMed]
- Lezak, M.D.; Howieson, D.B.; Bigler, E.D.; Tranel, D. Neuropsychological Assessment, 5th ed.; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Dementie|NHG-Richtlijnen. Available online: https://richtlijnen.nhg.org/standaarden/dementie#volledige-tekst (accessed on 13 May 2020).
- Nieuwenhuis-Mark, R.E. The Death Knoll for the MMSE: Has It Outlived Its Purpose? J. Geriatr. Psychiatry Neurol. 2010, 23, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Evered, L.A.; Silbert, B.S. Postoperative Cognitive Dysfunction and Noncardiac Surgery. Geriatr. Anesth. 2018, 127, 496–505. [Google Scholar] [CrossRef]
- Palsetia, D.; Rao, G.; Tiwari, S.; Lodha, P.; De Sousa, A. The Clock Drawing Test versus Mini-Mental Status Examination as a Screening Tool for Dementia: A Clinical Comparison. Indian J. Psychol. Med. 2018, 40, 1–10. [Google Scholar] [CrossRef]
- Dalton, A.; Zafirova, Z. Preoperative Management of the Geriatric Patient: Frailty and Cognitive Impairment Assessment. Anesthesiol. Clin. 2018, 36, 599–614. [Google Scholar] [CrossRef]
- Gan, S.; Yu, Y.; Wu, J.; Tang, X.; Zheng, Y.; Wang, M.; Zhu, S. Preoperative Assessment of Cognitive Function and Risk Assessment of Cognitive Impairment in Elderly Patients with Orthopedics: A Cross-Sectional Study. BMC Anesthesiol. 2020, 20, 189. [Google Scholar] [CrossRef]
- Dementia. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 12 May 2021).
- Rizzi, L.; Rosset, I.; Roriz-Cruz, M. Global Epidemiology of Dementia: Alzheimer’s and Vascular Types. BioMed Res. Int. 2014, 2014, 908915. [Google Scholar] [CrossRef]
- Morris, J.C.; Storandt, M.; Miller, J.P.; McKeel, D.W.; Price, J.L.; Rubin, E.H.; Berg, L. Mild Cognitive Impairment Represents Early-Stage Alzheimer Disease. Arch. Neurol. 2001, 58, 397–405. [Google Scholar] [CrossRef] [Green Version]
- Chou, K.L.; Amick, M.M.; Brandt, J.; Camicioli, R.; Frei, K.; Gitelman, D.; Goldman, J.; Growdon, J.; Hurtig, H.I.; Levin, B.; et al. A Recommended Scale for Cognitive Screening in Clinical Trials of Parkinson’s Disease. Mov. Disord. 2010, 25, 2501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, W.T.; Tan, N.C.; Lim, J.E.; Allen, J.C.; Lee, W.S.; Quah, J.H.M.; Paulpandi, M.; Teh, T.A.; Lim, S.H.; Malhotra, R. Comparison of Time Taken to Assess Cognitive Function Using a Fully Immersive and Automated Virtual Reality System vs. the Montreal Cognitive Assessment. Front. Aging Neurosci. 2021, 13, 756891. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Rowan, M.; Nafisi, S.; Patel, A.; Burton, J.K.; Quinn, T.J. Informant-Based Screening Tools for Diagnosis of Dementia, an Overview of Systematic Reviews of Test Accuracy Studies Protocol. Syst. Rev. 2020, 9, 271. [Google Scholar] [CrossRef] [PubMed]
- Noel-Storr, A.H.; Mccleery, J.M.; Richard, E.; Ritchie, C.W.; Flicker, L.; Cullum, S.J.; Davis, D.; Quinn, T.J.; Hyde, C.; Rutjes, A.W.S.; et al. Reporting Standards for Studies of Diagnostic Test Accuracy in Dementia-The STARDdem Initiative. Neurology 2014, 83, 364–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carnero-Pardo, C.; Cruz-Orduña, I.; Espejo-Martínez, B.; Martos-Aparicio, C.; López-Alcalde, S.; Olazarán, J. Utility of the Mini-Cog for Detection of Cognitive Impairment in Primary Care: Data from Two Spanish Studies. Int. J. Alzheimer’s Dis. 2013, 2013, 285462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.; Dai, J.; Zhao, S.; Liu, W.; Li, H. Comparison of the Value of Mini-Cog and MMSE Screening in the Rapid Identification of Chinese Outpatients with Mild Cognitive Impairment. Medicine 2018, 97, e10966. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Freitas, S.; Simões, M.R.; Alves, L.S.I. Montreal Cognitive Assessment Validation Study for Mild Cognitive Impairment and Alzheimer Disease. Alzheimer Dis. Assoc. Disord. 2013, 27, 37–43. [Google Scholar] [CrossRef]
- Sokolowska, N.; Sokolowski, R.; Polak-sZabela, A.; Mazur, E.; Podhorecka, M.; Kedziora-Kornatowska, K. Comparison of the Effectiveness of the Montreal Cognitive Assessment 7. 2 and the Mini-Mental State Examination in the Detection of Mild Neurocognitive Disorder in People over 60 Years of Age. Preliminary Study. Psychiatr. Pol. 2018, 52, 843–857. [Google Scholar] [CrossRef]
- Fujiwara, Y.; Suzuki, H.; Yasunaga, M.; Sugiyama, M.; Ijuin, M.; Sakuma, N.; Inagaki, H.; Iwasa, H.; Ura, C.; Yatomi, N.; et al. Brief Screening Tool for Mild Cognitive Impairment in Older Japanese: Validation of the Japanese Version of the Montreal Cognitive Assessment. Geriatr. Gerontol. Int. 2010, 10, 225–232. [Google Scholar] [CrossRef]
- Molnar, F.J.; Wells, G.A.; Mcdowell, I. The Derivation and Validation of the Ottawa 3D and Ottawa 3DY Three- and Four-Question Screens for Cognitive Impairment. Clin. Med. Insights Geriatr. 2008, 2, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Galvin, J.E.; Roe, C.M.; Powlishta, K.K.; Coats, M.A.; Muich, S.J.; Grant, E.; Miller, J.P.; Storandt, M.; Morris, J.C. The AD8: A Brief Informant Interview to Detect Dementia. Neurology 2005, 65, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Galvin, J.E.; Roe, C.M.; Coats, M.A.; Morris, J.C. Patient’s Rating of Cognitive Ability. Arch. Neurol. 2007, 64, 725. [Google Scholar] [CrossRef] [PubMed]
- Scharre, D.W.; Chang, S.I.; Murden, R.A.; Lamb, J.; Beversdorf, D.Q.; Kataki, M.; Nagaraja, H.N.; Bornstein, R.A. Self-Administered Gerocognitive Examination (SAGE): A Brief Cognitive Assessment Instrument for Mild Cognitive Impairment (MCI) and Early Dementia. Alzheimer Dis. Assoc. Disord. 2010, 24, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Scharre, D.W.; Chang, S.I.; Nagaraja, H.N.; Vrettos, N.E.; Bornstein, R.A. Digitally Translated Self-Administered Gerocognitive Examination (ESAGE): Relationship with Its Validated Paper Version, Neuropsychological Evaluations, and Clinical Assessments. Alzheimer’s Res. Ther. 2017, 9, 44. [Google Scholar] [CrossRef] [Green Version]
- Shwartz, S.K.; Morris, R.D.; Penna, S. Psychometric Properties of the Saint Louis University Mental Status Examination. Appl. Neuropsychol. Adult 2019, 26, 101–110. [Google Scholar] [CrossRef]
- Cook, S.E.; Marsiske, M.; Mccoy, K.J.M. The Use of the Modified Telephone Interview for Cognitive Status (TICS-M) in the Detection of Amnestic Mild Cognitive Impairment. J. Geriatr. Psychiatry Neurol. 2009, 22, 103–109. [Google Scholar] [CrossRef] [Green Version]
- Knopman, D.S.; Roberts, R.O.; Geda, Y.E.; Pankratz, V.S.; Christianson, T.J.; Petersen, R.C.; Rocca, W.A. Validation of the Telephone Interview for Cognitive Status-Modified in Subjects with Normal Cognition, Mild Cognitive Impairment. Neuroepidemiology 2010, 34, 34–42. [Google Scholar] [CrossRef] [Green Version]
- Caoimh, R.O.; Gao, Y.; Mcglade, C.; Healy, L.; Gallagher, P.; Timmons, S.; Molloy, D.W. Comparison of the Quick Mild Cognitive Impairment (Qmci) Screen and the SMMSE in Screening for Mild Cognitive Impairment. Age Ageing 2012, 41, 624–629. [Google Scholar] [CrossRef] [Green Version]
- Bunt, S.; Caoimh, R.O.; Krijnen, W.P.; Molloy, D.W.; Goodijk, G.P.; Van Der Schans, C.P.; Hobbelen, H.J.S.M. Validation of the Dutch Version of the Quick Mild Cognitive Impairment Screen (Q Mci -D). BMC Geriatr. 2015, 15, 115. [Google Scholar] [CrossRef] [Green Version]
- Glynn, K.; Coen, R.; Lawlor, B.A. Is the Quick Mild Cognitive Impairment Screen (QMCI) More Accurate at Detecting Mild Cognitive Impairment than Existing Short Cognitive Screening Tests ? A Systematic Review of the Current Literature. Int. J. Geriatr. Psychiatry 2019, 34, 1739–1746. [Google Scholar] [CrossRef] [PubMed]
- Baek, M.J.; Kim, K.; Park, Y.H.; Kim, S. The Validity and Reliability of the Mini- Mental State Examination-2 for Detecting Mild Cognitive Impairment and Alzheimer’s Disease in a Korean Population. PLoS ONE 2016, 11, e0163792. [Google Scholar] [CrossRef] [PubMed]
- Larner, A.J. MACE for Diagnosis of Dementia and MCI: Examining Cut-Offs and Predictive Values. Diagnostics 2019, 9, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borson, S.; Scanlan, J.M.; Watanabe, J.; Tu, S.P.; Lessig, M. Simplifying Detection of Cognitive Impairment: Comparison of the Mini-Cog and Mini-Mental State Examination in a Multiethnic Sample. J. Am. Geriatr. Soc. 2005, 53, 871–874. [Google Scholar] [CrossRef]
- Hsu, J.-L.; Fan, Y.-C.; Huang, Y.-L.; Wang, J.; Chen, W.-H.; Chiu, H.-C.; Bai, C.-H. Improved Predictive Ability of the Montreal Cognitive Assessment for Diagnosing Dementia in a Community-Based Study. Alzheimer’s Res. Ther. 2015, 7, 69. [Google Scholar] [CrossRef] [Green Version]
- Kempen, G.I.J.M.; Meier, A.J.L.; Bouwens, S.F.M.; van Deursen, J.; Verhey, F.R.J. Telefonisch Interview Cognitieve Status (TICS): Psychometrische Aspecten. Tijdschr. Voor Gerontol. Geriatr. 2007, 38, 38–45. [Google Scholar] [CrossRef]
- Seo, E.H.; Lee, D.Y.; Kim, S.G.; Kim, K.W.; Kim, H.; Kim, B.J.; Kim, M.-D.; Kim, S.Y.; Kim, Y.H.; Kim, J.-L.; et al. Validity of the Telephone Interview for Cognitive Status (TICS) and Modified TICS (TICSm) for Mild Cognitive Imparment (MCI) and Dementia Screening. Arch. Gerontol. Geriatr. 2011, 52, 26–30. [Google Scholar] [CrossRef]
- Cahn-Hidalgo, D.; Estes, P.W.; Benabou, R. Validity, Reliability, and Psychometric Properties of a Computerized, Cognitive Assessment Test (Cognivue®). World J. Psychiatry 2020, 10, 1–11. [Google Scholar] [CrossRef]
- Lee, M.-T.; Chang, W.-Y.; Jang Id, Y. Psychometric and Diagnostic Properties of the Taiwan Version of the Quick Mild Cognitive Impairment Screen. PLoS ONE 2018, 13, e0207851. [Google Scholar] [CrossRef]
- Caoimh, R.O.; Gao, Y.; Gallagher, P.F.; Eustace, J.; McGlade, C.; Molloy, D.W. Which Part of the Quick Mild Cognitive Impairment Screen (Qmci) Discriminates between Normal Cognition, Mild Cognitive Impairment and Dementia? Age Ageing 2013, 42, 324–330. [Google Scholar] [CrossRef] [Green Version]
- Galvin, J.E.; Roe, C.M.; Xiong, C.; Morris, J.C. Validity and Reliability of the AD8 Informant Interview in Dementia. Neurology 2006, 67, 1942–1948. [Google Scholar] [CrossRef] [PubMed]
- Ryu, H.J.; Kim, H.J.; Han, S.H. Validity and Reliability of the Korean Version of the AD8 Informant Interview (K-AD8) in Dementia. Alzheimer Dis. Assoc. Disord. 2009, 23, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Barbic, D.; Kim, B.; Salehmohamed, Q.; Kemplin, K.; Carpenter, C.R.; Barbic, S.P. Diagnostic Accuracy of the Ottawa 3DY and Short Blessed Test to Detect Cognitive Dysfunction in Geriatric Patients Presenting to the Emergency Department. BMJ Open 2018, 8, e019652. [Google Scholar] [CrossRef] [PubMed]
- Hobson, P.; Rohoma, K.H.; Wong, S.P.; Kumwenda, M.J. The Utility of the Mini-Addenbrooke’s Cognitive Examination as a Screen for Cognitive Impairment in Elderly Patients with Chronic Kidney Disease and Diabetes. Dement. Geriatr. Cogn. Disord. EXTRA 2016, 6, 541. [Google Scholar] [CrossRef] [PubMed]
- Borson, S.O.O.; Scanlan, J.; Brush, M.; Vitaliano, P.; Dokmak, A. The Mini-Cog: A Cognitive “vital Signs” Measure for Dementia Screening in Multi-Lingual Elderly. Int. J. Geriatr. Psychiatry 2000, 15, 1021–1027. [Google Scholar] [CrossRef]
- Scoring the Mini-Cog©—Mini-Cog©. Available online: https://mini-cog.com/mini-cog-instrument/scoring-the-mini-cog/ (accessed on 13 May 2020).
- Borson, S.; Scanlan, J.M.; Chen, P.; Ganguli, M. The Mini-Cog as a Screen for Dementia: Validation in a Population-Based Sample. J. Am. Geriatr. Soc. 2003, 51, 1451–1454. [Google Scholar] [CrossRef]
- About|MoCA Montreal—Cognitive Assessment. Available online: https://www.mocatest.org/about/ (accessed on 13 May 2020).
- Jeste, D.V.; Lieberman, J.A.; Fassler, D.; Peele, R. Diagnostic and Statistical Manuel of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013; Volume 17, ISBN 9780890425541. [Google Scholar]
- Canadian Study of Health and Aging Working Group. The incidence of dementia in Canada. Neurology 2000, 55, 66–73. [Google Scholar] [CrossRef]
- Trowbridge, E.R.; Kim, D.; Barletta, K.; Fitz, V.; Larkin, S.; Hullfish, K.L. Prevalence of Positive Screening Test for Cognitive Impairment among Elderly Urogynecologic Patients. Am. J. Obstet. Gynecol. 2016, 215, 663.e1–663.e6. [Google Scholar] [CrossRef]
- Galvin, J.E. The AD8: The Washington University Dementia Screening Test (“Eight-Item Interview to Differentiate Aging and Dementia”). Fam. Med. 2005, 25, 367–382. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV; American Psychiatric Association: Washington, DC, USA, 1994; ISBN 0890420629. [Google Scholar]
- Brandt, J.; Spencer, M.; Folstein, M. The Telephone Interview for Cognitive Status. Neuropsychiatry Neuropsychol. Behav. Neurol. 1988, 1, 111–117. [Google Scholar]
- Caoimh, R.O.; Svendrovski, A.; Johnston, B.C.; Gao, Y.; Mcglade, C.; Eustace, J.; Timmons, S.; Guyatt, G.; Molloy, D.W. The Quick Mild Cognitive Impairment Screen Correlated with the Standardized Alzheimer’ s Disease Assessment Scale—Cognitive Section in Clinical Trials. J. Clin. Epidemiol. 2014, 67, 87–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mckhann, G.; Drachman, D.; Folstein, M.; Katzman, R.; Price, D.; Stadlan, E.M. Clinical Diagnosis of Alzheimer’s Disease: Report of the NINCDS-ADRDA Work Group* under the Auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 1984, 34, 939–944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albanna, M.; Yehya, A.; Khairi, A.; Dafeeah, E.; Elhadi, A.; Rezgui, L.; Al Kahlout, S.; Yousif, A.; Uthman, B.; Al-Amin, H. Validation and Cultural Adaptation of the Arabic Versions of the Mini–Mental Status Examination—2 and Mini-Cog Test. Neuropsychiatr. Dis. Treat. 2017, 13, 793–801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arias, F.; Wiggins, M.; Urman, R.D.; Armstrong, R.; Pfeifer, K.; Bader, A.M.; Libon, D.J.; Chopra, A.; Price, C.C. Rapid In-Person Cognitive Screening in the Preoperative Setting: Test Considerations and Recommendations from the Society for Perioperative Assessment and Quality Improvement (SPAQI). J. Clin. Anesth. 2020, 62, 109724. [Google Scholar] [CrossRef] [PubMed]
- Long, L.S.; Shapiro, W.A.; Leung, J.M. A Brief Review of Practical Preoperative Cognitive Screening Tools. Can. J. Anesth. 2012, 59, 798–804. [Google Scholar] [CrossRef] [Green Version]
- De Roeck, E.E.; De Deyn, P.P.; Dierckx, E.; Engelborghs, S. Brief Cognitive Screening Instruments for Early Detection of Alzheimer’s Disease: A Systematic Review. Alzheimers Res. Ther. 2019, 11, 21. [Google Scholar] [CrossRef] [Green Version]
- Chow, W.B.; Rosenthal, R.A.; Merkow, R.P.; Ko, C.Y.; Esnaola, N.F. Optimal Preoperative Assessment of the Geriatric Surgical Patient: A Best Practices Guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J. Am. Coll. Surg. 2012, 215, 453–466. [Google Scholar] [CrossRef]
- Roebuck-Spencer, T.M.; Glen, T.; Puente, A.E.; Denney, R.L.; Ruff, R.M.; Hostetter, G.; Bianchini, K.J. Cognitive Screening Tests Versus Comprehensive Neuropsychological Test Batteries: A National Academy of Neuropsychology Education Paper. Arch. Clin. Neuropsychol. 2017, 32, 491–498. [Google Scholar] [CrossRef] [Green Version]
- Nelson, A.P.; O’Connor, M.G. Mild Cognitive Impairment: A Neuropsychological Perspective. CNS Spectr. 2008, 13, 56–64. [Google Scholar] [CrossRef]
- Wada-Isoe, K.; Kikuchi, T.; Umeda-Kameyama, Y.; Mori, T.; Akishita, M.; Nakamura, Y. Global Clinical Dementia Rating Score of 0.5 May Not Be an Accurate Criterion to Identify Individuals with Mild Cognitive Impairment. J. Alzheimer’s Dis. Rep. 2019, 3, 233–239. [Google Scholar] [CrossRef]
- Mielke, M.M.; Ferretti, M.T.; Iulita, M.F.; Hayden, K.; Khachaturian, A.S. Sex and Gender in Alzheimer’s Disease—Does It Matter? Alzheimer’s Dement. 2018, 14, 1101–1103. [Google Scholar] [CrossRef] [PubMed]
- Sohn, D.; Shpanskaya, K.; Lucas, J.E.; Petrella, J.R.; Saykin, A.J.; Tanzi, R.E.; Samatova, N.F.; Doraiswamy, P.M. Sex Differences in Cognitive Decline in Subjects with High Likelihood of Mild Cognitive Impairment Due to Alzheimer’s Disease. Sci. Rep. 2018, 8, 7490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, K.A.; Choudhury, K.R.; Rathakrishnan, B.G.; Marks, D.M.; Petrella, J.R.; Doraiswamy, P.M. Marked Gender Differences in Progression of Mild Cognitive Impairment over 8 Years. Alzheimer’s Dement. Transl. Res. Clin. Interv. 2015, 1, 103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, C.B.; Derosa, J.T.; Moon, M.P.; Strobino, K.; Decarli, C.; Cheung, Y.K.; Assuras, S.; Levin, B.; Stern, Y.; Sun, X.; et al. Race/Ethnic Disparities in Mild Cognitive Impairment and Dementia: The Northern Manhattan Study. J. Alzheimer’s Dis. 2021, 80, 1129. [Google Scholar] [CrossRef]
- Ysea-Hill, O.; Gomez, C.; Shah, A.; Hammel, I.; Rodriguez-Suarez, M.; Ruiz, J.G. Race-Based Differences in MCI And Dementia: A Propensity Score Matching Study. Am. J. Geriatr. Psychiatry 2021, 29, S48–S49. [Google Scholar] [CrossRef]
- Mclennan, S.N.; Mathias, J.L.; Brennan, L.C.; Stewart, S. Validity of the Montreal Cognitive Assessment (MoCA) as a Screening Test for Mild Cognitive Impairment (MCI) in a Cardiovascular Population. J. Geriatr. Psychiatry Neurol. 2011, 24, 33–38. [Google Scholar] [CrossRef]
- Daniels, A.; Daiello, L.; Lareau, C.; Robidoux, K.; Luo, W.; Ott, B.; Hayda, R.; Born, C. Preoperative Cognitive Impairment and Psychological Distress in Hospitalized Elderly Hip Fracture Patients. Am. J. Orthop. 2014, 43, 146–152. [Google Scholar]
- Puustinen, J.; Luostarinen, L.; Luostarinen, M.; Pulliainen, V.; Huhtala, H.; Soini, M.; Suhonen, J. The Use of MoCA and Other Cognitive Tests in Evaluation of Cognitive Impairment in Elderly Patients Undergoing Arthroplasty. Geriatr. Orthop. Surg. Rehabil. 2016, 7, 183–187. [Google Scholar] [CrossRef]
- Milani, S.A.; Marsiske, M.; Cottler, L.B.; Chen, X.; Striley, C.W. Optimal Cutoffs for the Montreal Cognitive Assessment Vary by Race and Ethnicity. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2018, 10, 773–781. [Google Scholar] [CrossRef]
- Crosby, G.; Culley, D.J.; Hyman, B.T. Preoperative Cognitive Assessment of the Elderly Surgical Patient: A Call for Action. Anesthesiology 2011, 114, 1265–1268. [Google Scholar] [CrossRef] [Green Version]
- Aalbers, T.; Baars, M.A.E.; Rikkert, M.G.M.O.; Kessels, R.P.C. Puzzling with Online Games (BAM-COG): Reliability, Validity, and Feasibility of an Online Self-Monitor for Cognitive Performance in Aging Adults. J. Med. Internet Res. 2013, 15, e270. [Google Scholar] [CrossRef] [PubMed]
- Tong, T.; Chignell, M. Developing a Serious Game for Cognitive Assessment: Choosing Settings and Measuring Performance. In Proceedings of the Second International Symposium of Chinese CHI, Toronto, ON, Canada, 26–27 April 2014; pp. 70–79. [Google Scholar] [CrossRef]
| Screener | Exclusion Criterion |
|---|---|
| Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) | <2 domains of cognitive functioning and informant based screener |
| NeuroCogFX | Test duration > 15 min |
| National Institutes of Health Toolbox Cognitive Battery (NIHTB-CB) | Test duration > 15 min |
| Short Blessed Test (SBT) | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| National Institutes of Health Toolbox Cognitive Battery (AMNART) | <2 domains of cognitive functioning No memory assessment |
| Auditory Verbal Learning Test (AVLT) | Test duration > 15 min |
| Clock drawing test (CDT) | No memory assessment |
| Clock in the box | No memory assessment |
| Cognitive Disorder Examination (CODEX) | Not a real test, it is a decision tree of the Mini-Cog/too much overlap with Mini-Cog |
| Cognitive Activity Scale | No memory assessment |
| Controlled Oral Word Association Test (COWAT) | No memory assessment |
| Verbal fluency test | No memory assessment |
| DemTect | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Hasegawa Dementia Scale (HDS) | Screener for delirium |
| Identification of Seniors At Risk (ISAR) | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Stroop color word test (SCWT) | No memory assessment |
| Addenbrooke’s Cognitive Examination (ACE) | Test duration > 15 min |
| Animal fluency test | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Brief Screen Cognitive Impairment (BSCI) | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Geriatric 8 (G8) | No memory assessment |
| Mail-in Cognitive Function Screening Instrument (MCFSI) | No memory assessment and study partner or informant is needed |
| Month Backward Test (MBT) | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Time & Change | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Trail making A&B | No memory assessment |
| Brief Neuropsychological Battery (BNB) | Test duration > 15 min |
| Cognitive Performance Scale (CPS) | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Literacy Independent Cognitive Assessment (LICA) | Test duration > 15 min and no articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Memory Fluency and Orientation (MEFO) | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Rapid Cognitive Screen (RCS) | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Computerized Assessment of Mild Cognitive Impairment (CAMCI) | Test duration > 15 min |
| Short Portable Mental Status Questionnaire (SPMSQ) | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| The 5 object test | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Brief Memory and Executive Test (BMET) | No articles with comprehensive neuropsychological assessment as gold standard for detecting MCI |
| Dementia Rating Scale 2 | Test duration > 15 min |
| Frontal Assessment Battery (FAB) | Specific for frontal lobe dysfunction |
| Cogstate Brief Battery (CBB) | Specific for nondementia brain injuries |
| Tool | Items/Cognitive Domains | Author/Setting Recruitment | N | Average Age (years) | Admin Time (min) | TP/Cutoff Score | Blinding Index Test/Reference Test | Sensitivity + Specificity MCI | Sensitivity + Specificity CI |
|---|---|---|---|---|---|---|---|---|---|
| Mini-Cog |
| Carnero-Pardo and colleagues [39]/Primary care Madrid and Granada | 307 | All 72 | 3 | 5/≤1 | Yes | - | Sen 60% Spe 90% |
| Li and colleagues [40]/Neurological outpatient department Cangzhou City Central Hospital | 229 | MCI 68.7 Non-MCI 66.1 | 5/≤1 | NR | Sen 85.71% Spe 79.41% | - | |||
| MoCA |
| Nasreddine and colleagues [41]/Jewish General Hospital (JGH) Memory Clinic in Montreal and University of Sherbrooke NRS memory clinic | 277 | NC 72.84 MCI 75.19 Dementia 76.72 | 10 | 30/≤25 | NR | Sen 90% Spe 87% | - |
| Freitas and colleagues [42]/Dementia Clinic, Neurology Department of the Coimbra University Hospital | 360 | NC 71.34 MCI 70.52 Dementia 74.22 | 30/≤21 | NR | Sen 81% Spe 77% | - | |||
| Sokolowska and colleagues [43]/Department of Geriatrics, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University, Torun | 131 | MCI 79.06 Non-MCI 74.8 | 30/≤24 | Yes | Sen 89.5% Spe 74.1% | - | |||
| Fujiwara and colleagues [44]/Memory Clinic of Tokyo Metropolitan Geriatric Hospital, Tokyo | 96 | NC 76.4 MCI 77.3 Dementia 77.5 | 30/≤25 | Yes | Sen 93% Spe 89% | - | |||
| O3DY |
| Molnar and colleagues [45]/randomly selected samples throughout Canada | 1560 | All 79.5 | 2–3 | 4/≤3 | Yes | - | Sen 80% Spe 56% |
| AD8 |
| Galvin and colleagues [46]/Community-dwelling volunteers who enrolled in a longitudinal study of healthy aging and dementia. | 236 | All 78.1 | 2–3 | 8/≤1 | Yes | Sen 74% Spe 86% | Sen 85% Spe 86% |
| Galvin and colleagues [47]/Community-dwelling volunteers who enrolled in a longitudinal study of healthy aging and dementia. | 325 | All 76.8 | 8/<1 | Yes | - | Sen 80% Spe 59% | |||
| SAGE |
| Scharre and colleagues [48]/geriatric outpatient clinics, educational talks to lay public, independent and assisted living facilities, senior centers, free memory screens through newspaper advertisement, and Memory Disorders Clinic at Ohio State University. | 63 | All 78.0 | 15 | 22/≤16 | Yes | Sen 62% Spe 95% | Sen 79% Spe 95% |
| Scharre and colleagues [49]/educational talks to lay public, independent and assisted living facilities, senior centers, free memory screens, or at the Memory Disorders Clinic at The Ohio State University. | 66 | All 75.2 | 22/≤15 | Yes | Sen 69% Spe 86% | Sen 71% Spe 90% | |||
| SLUMS |
| Tariq and colleagues [15]/Geriatric Research Education and Clinical Center (GRECC), Veterans’ Affairs Medical Center (VAMC) hospitals in Saint Louis. | 702 | All 75.3 | 7 | 30/≤23.5 * 30/≤25.5 * | NR | Sen 92% Spe 81% Sen 95% Spe 76% | - - |
| Shwartz and colleagues [50]/Mild Cognitive Impairment (MCI) Clinic at the Atlanta Veterans Affairs Medical Center (VAMC). | 148 | All 68.48 | 30/≤25 | No | Sen 81% Spe 68% | - | |||
| TICS-M |
| Cook and colleagues [51]/Community-dwelling older adults. Articles in a local senior newspaper, advertisements in the community, and from the participant pools of other local aging investigators. | 71 | All 74.9 167 | 10 | 50/≤34 | Yes | Sen 82.4% Spe 87.0% | - |
| Knopman and colleagues [52]/Mayo Clinic Study of Aging and the Mayo Clinic Alzheimer’s Disease Research Center (ADRC). | 167 | NC 81 MCI 84 Dementia 80 | 50/≤31 | Yes | Sen 82.4% Spe 87.0% | - | |||
| Quick-MCI |
| O’Caoimh and colleagues [53]/four memory clinics across Ontario, Canada (Hamilton, Paris, Niagara Falls, and Grand Bend). | 965 | NC 67 MCI 75.5 Dementia 79 | 3–5 | 100/NR | Yes | Sen 82% Spe 70% | Sen 91% Spe 80% |
| Bunt and colleagues [54]/a geriatric outpatient department in a regional hospital, in the North of the Netherlands. | 90 | NC 68.7 MCI 79.1 Dementia 79.2 | 100/≤51.5 | Yes | Sen 82% Spe 90% | - | |||
| Glynn and colleagues [55]/electronic journal databases EBSCO, Psych info, and Science Direct. | NR | NR | NR | Yes | Sen 82% Spe 82% | Sen 95% Spe 83% | |||
| MMSE2 BV |
| Baek and colleagues [56]/outpatients and inpatients at the Clinical Neuroscience Center at the Seoul National University Bundang Hospital. | 414 | NC 67.05 MCI 71.05 Dementia 75.38 | 5 | 16/≤14 | NR | Sen 60% Spe 75% | - |
| MMSE2 SV | 10–15 | 30/≤26 | NR | Sen 74% Spe 59% | - | ||||
| Mini-ACE |
| Larner [57]/Cognitive Function Clinic, Walton Centre for Neurology and Neurosurgery, Liverpool. | 755 | All 60 | 5–10 | 30/≤25 | NR | - | Sen 91% Spe 71% |
| 30/≤24 | Sen 90% Spe 57% | - |
| Interrater Reliability (Correlation) | Test-Retest Reliability (Correlation) | |
|---|---|---|
| Mini Cog | 0.95 [58] | - |
| MoCA | 0.852 [59] | 0.92 [41] |
| MMSE-2 BV | 0.94–0.99 [56] | 0.76 [56] |
| MMSE-2 SV | 0.94–0.99 [56] | 0.82 [56] |
| TICS-M | 0.90 [60] | 0.91–0.95 [60,61] |
| SAGE | 0.96 [48] | 0.86 [48] |
| SLUMS | - | 0.82 [62] |
| Quick MCI | 1.00 [63] | 0.86–0.87 [63,64] |
| AD8 | 0.80–0.89 [65,66] | 0.67–0.81 [65,66] |
| O3DY | 0.64 [67] | - |
| Mini-ACE | - | 0.64 [68] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pas, M.t.; Olde Rikkert, M.; Bouwman, A.; Kessels, R.; Buise, M. Screening for Mild Cognitive Impairment in the Preoperative Setting: A Narrative Review. Healthcare 2022, 10, 1112. https://doi.org/10.3390/healthcare10061112
Pas Mt, Olde Rikkert M, Bouwman A, Kessels R, Buise M. Screening for Mild Cognitive Impairment in the Preoperative Setting: A Narrative Review. Healthcare. 2022; 10(6):1112. https://doi.org/10.3390/healthcare10061112
Chicago/Turabian StylePas, Mariska te, Marcel Olde Rikkert, Arthur Bouwman, Roy Kessels, and Marc Buise. 2022. "Screening for Mild Cognitive Impairment in the Preoperative Setting: A Narrative Review" Healthcare 10, no. 6: 1112. https://doi.org/10.3390/healthcare10061112
APA StylePas, M. t., Olde Rikkert, M., Bouwman, A., Kessels, R., & Buise, M. (2022). Screening for Mild Cognitive Impairment in the Preoperative Setting: A Narrative Review. Healthcare, 10(6), 1112. https://doi.org/10.3390/healthcare10061112







