Severe Ground Fall Injury Associated with Alcohol Consumption in Geriatric Patients
Abstract
:1. Introduction
2. Methods
2.1. Study Design
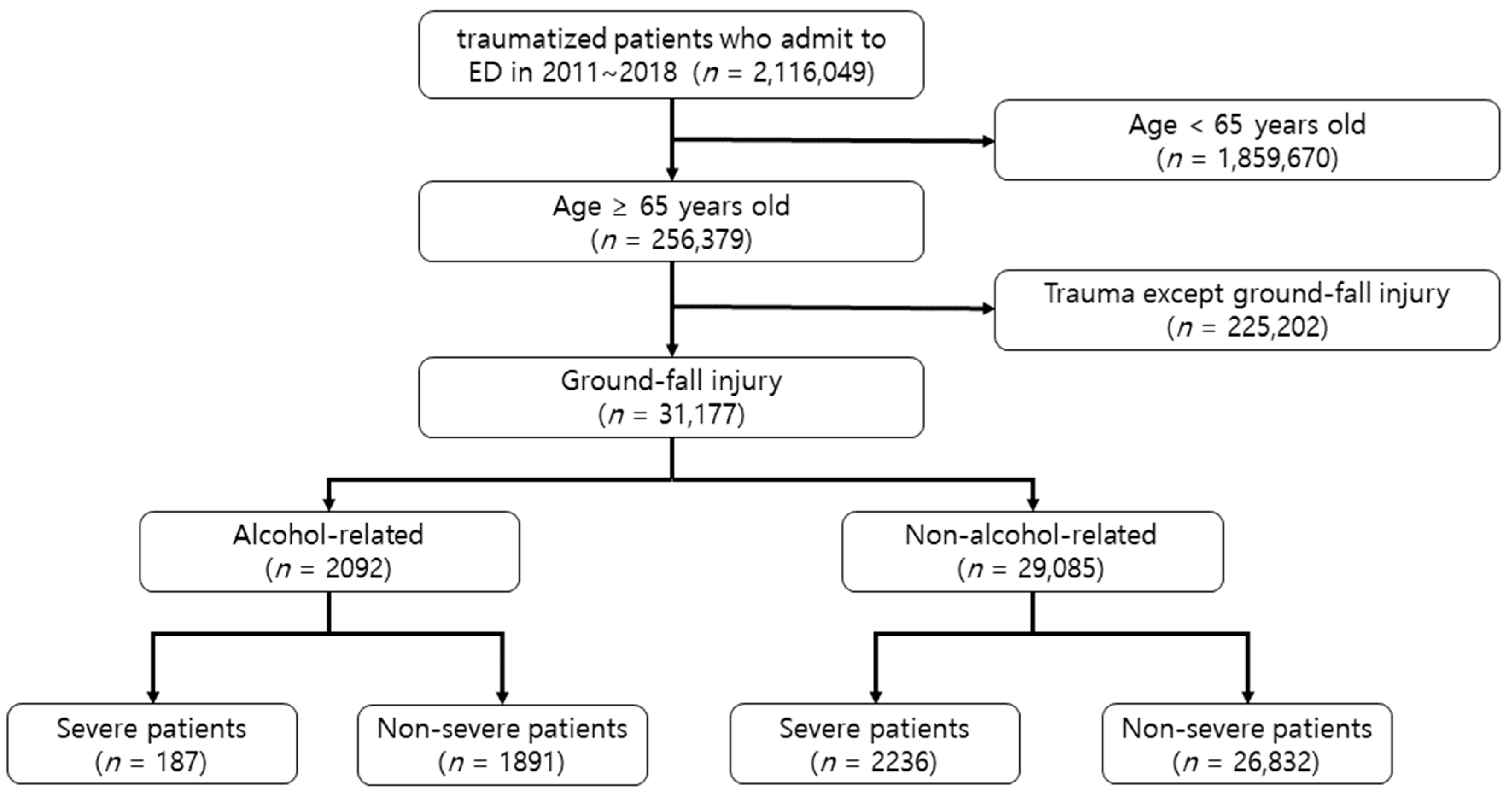
2.2. Study Setting and Population
2.3. Study Outcomes
2.4. Data Sources and Measurement
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Baseline Characteristics of All Patients | Baseline Characteristics of Propensity Score Matched Patients (2:1) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-Alcohol (N = 29,085) | Alcohol (N = 2092) | Standardized Mean Difference | p-Value | Non-alcohol (N = 4154) | Alcohol (N = 2092) | Standardized Mean Difference | p-Value | ||
| n (%) | n (%) | n (%) | n (%) | ||||||
| Sex | Male | 10,434 (35.9) | 1540 (73.6) | 0.8563 | <0.001 | 2965 (71.4) | 1540 (73.6) | 0.0500 | 0.085 |
| Female | 18,651 (64.1) | 552 (26.4) | 1189 (28.6) | 552 (26.4) | |||||
| Time of injury | 00:00–05:59 h | 2063 (7.1) | 295 (14.1) | −0.2903 | <0.001 | 382 (9.2) | 295 (14.1) | 0.0315 | 0.144 |
| 06:00–11:59 h | 8064 (27.7) | 205 (9.8) | 521 (12.5) | 205 (9.8) | |||||
| 12:00–17:59 h | 11,146 (38.3) | 452 (21.6) | 1137 (27.4) | 452 (21.6) | |||||
| 18:00~23:59 h | 7812 (26.9) | 1140 (54.5) | 2114 (50.9) | 1140 (54.5) | |||||
| Location of injury | Residential facility | 17,151 (59.0) | 430 (20.6) | −0.4346 | <0.001 | 1159 (27.9) | 430 (20.6) | 0.2630 | <0.001 |
| Transportation area | 6900 (23.7) | 1318 (63.0) | 1883 (45.3) | 1318 (63.0) | |||||
| Public or commercial facility | 1816 (6.2) | 310 (14.8) | 467 (11.2) | 310 (14.8) | |||||
| Other area | 3218 (11.1) | 34 (1.6) | 645 (15.5) | 34 (1.6) | |||||
| Activity during injury | Paid or unpaid work | 2437 (8.4) | 19 (0.9) | 0.4324 | <0.001 | 311 (7.5) | 19 (0.9) | −0.0282 | 0.273 |
| Sports or leisure activity | 2893 (9.9) | 980 (46.8) | 1475 (35.5) | 980 (46.8) | |||||
| Daily activity | 23,026 (79.2) | 1069 (51.1) | 2312 (55.7) | 1069 (51.1) | |||||
| Others | 727 (2.5) | 24 (1.1) | 56 (1.3) | 24 (1.1) | |||||
| Mean ± SD | Mean ± SD | Standardized Mean Difference | p-Value | Mean ± SD | Mean ± SD | Standardized Mean Difference | p-Value | ||
| Age | 76.7 ± 7.4 | 71.4 ± 5.2 | 1.0345 | <0.001 | 71.3 ± 5.2 | 71.4 ± 5.2 | −0.0102 | 0.654 | |
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| OR | 95% C.I. | p-Value | OR | 95% C.I. | p-Value | |
| Male sex vs. female | 1.00 | 1.00–1.00 | <0.001 | 1.01 | 1.00–1.01 | <0.001 |
| Age group, years old | ||||||
| ≥85 | 1.00 | |||||
| 65–74 years | 1.00 | 1.0–1.0 | 0.093 | |||
| 75–84 years | 1.00 | 1.0–1.0 | 0.079 | |||
| Season of injury | ||||||
| Autumn | 1.00 | |||||
| Winter | 1.00 | 1.00–1.01 | 0.296 | |||
| Spring | 1.00 | 1.00–1.01 | 0.030 | |||
| Summer | 1.00 | 1.00–1.01 | 0.091 | |||
| Time of injury | ||||||
| 06:00–11:59 h | 1.00 | |||||
| 12:00–17:59 h | 1.00 | 1.00–1.00 | 0.299 | |||
| 18:00–23:59 h | 1.00 | 1.00–1.00 | <0.001 | |||
| 00:00–05:59 h | 1.01 | 1.01–1.01 | <0.001 | |||
| Transportation to ED | ||||||
| Other medical facility | 1.00 | 1.00 | ||||
| Public ambulance | 1.02 | 1.02–1.02 | <0.001 | 1.02 | 1.01–1.02 | <0.001 |
| Individual transportation | 1.00 | 0.99–1.00 | <0.001 | 0.99 | 0.99–0.99 | <0.001 |
| Location of injury | ||||||
| Other area | 1.00 | 1.00 | ||||
| Residential facility | 1.03 | 1.02–1.03 | <0.001 | 1.03 | 1.02–1.04 | <0.001 |
| Transportation area | 1.03 | 1.03–1.03 | <0.001 | 1.03 | 1.03–1.04 | <0.001 |
| Public or commercial facility | 1.03 | 1.03–1.04 | <0.001 | 1.03 | 1.03–1.04 | <0.001 |
| Activity during injury | ||||||
| Paid or unpaid work | 1.00 | 1.00 | ||||
| Sports or leisure activity | 1.03 | 1.02–1.03 | <0.001 | 1.03 | 1.02–1.03 | <0.001 |
| Daily activity | 1.02 | 1.02–1.03 | <0.001 | 1.02 | 1.01–1.02 | <0.001 |
| others | 1.03 | 1.01–1.04 | <0.001 | 1.02 | 1.01–1.03 | 0.001 |
| Non-slippery condition of floor vs. slippery | 1.01 | 1.00–1.01 | 0.004 | 1.01 | 1.01–1.02 | 0.001 |
| Sloping vs. flat floor | 1.00 | 1.00–1.00 | 0.683 | |||
| Presence of obstacles on floor | 1.00 | 1.00–1.01 | 0.243 | |||
| Absence of lights | 1.01 | 1.01–1.01 | <0.001 | 1.02 | 1.01–1.02 | <0.001 |
| Concrete floor vs. other types | 1.03 | 1.02–1.03 | <0.001 | 1.02 | 1.01–1.02 | <0.001 |
References
- Jung, H.; Kim, S.; Lee, S.; Kim, S.; Cho, G.; Kim, M.; Lee, J.; Han, C. Relating factors to severe injury from outdoor falls in older people. Geriatr. Gerontol. Int. 2017, 18, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Kim, S.; Cho, G.; Lee, J.; Park, E.; Lee, D. Characteristics of fall-related head injury versus non-head injury in the older adults. BMC Geriatr. 2021, 21, 196. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, Y.; Kondo, Y.; Hirano, Y.; Ishihara, T.; Sueyoshi, K.; Okamoto, K.; Tanaka, H. Characteristics, injuries, and clinical outcomes of geriatric trauma patients in Japan: An analysis of the nationwide trauma registry database. Sci. Rep. 2020, 10, 19148. [Google Scholar] [CrossRef] [PubMed]
- Deandrea, S.; Lucenteforte, E.; Bravi, F.; Foschi, R.; La Vecchia, C.; Negri, E. Risk factors for falls in community-dwelling older people: A systematic review and meta-analysis. Epidemiology 2010, 21, 658–668. [Google Scholar] [CrossRef]
- Bhattacharya, B.; Maung, A.; Schuster, K.; Davis, K. The older they are the harder they fall: Injury patterns and outcomes by age after ground level falls. Injury 2016, 47, 1955–1959. [Google Scholar] [CrossRef]
- Spaniolas, K.; Cheng, J.; Gestring, M.; Sangosanya, A.; Stassen, N.; Bankey, P. Ground level falls are associated with significant mortality in elderly patients. J. Trauma 2010, 69, 821–825. [Google Scholar] [CrossRef]
- Stevens, J.; Rudd, R. Circumstances and contributing causes of fall deaths among persons aged 65 and older: United States, 2010. J. Am. Geriatr. Soc. 2014, 62, 470–475. [Google Scholar] [CrossRef] [Green Version]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Lee, H.; Kim, S.; Lee, S.; Kim, S.; Cho, G.; Kim, M.; Lee, J.; Han, C. Severe Injuries from Low-height Falls in the Elderly Population. J. Korean Med. Sci. 2018, 33, e221. [Google Scholar] [CrossRef]
- Alamgir, H.; Muazzam, S.; Nasrullah, M. Unintentional falls mortality among elderly in the United States: Time for action. Injury 2012, 43, 2065–2071. [Google Scholar] [CrossRef]
- Taira, T.; Morita, S.; Umebachi, R.; Miura, N.; Icimura, A.; Inoue, S.; Nakagawa, Y.; Inokuchi, S. Risk factors for ground-level falls differ by sex. Am. J. Emerg. Med. 2015, 33, 640–644. [Google Scholar] [CrossRef]
- Glover, J.; Gold, J. Alcohol Use Increasing Among Adults 65 and Older. WMJ Off. Publ. State Med. Soc. Wis. 2017, 116, 182–183. [Google Scholar]
- Moos, R.; Schutte, K.; Brennan, P.; Moos, B. Older adults’ alcohol consumption and late-life drinking problems: A 20-year perspective. Addiction 2009, 104, 1293–1302. [Google Scholar] [CrossRef] [Green Version]
- Shakya, I.; Bergen, G.; Haddad, Y.; Kakara, R.; Moreland, B. Fall-related emergency department visits involving alcohol among older adults. J. Saf. Res. 2020, 74, 125–131. [Google Scholar] [CrossRef]
- Siracuse, J.; Odell, D.; Gondek, S.; Odom, S.; Kasper, E.; Hauser, C.; Moorman, D. Health care and socioeconomic impact of falls in the elderly. Am. J. Surg. 2012, 203, 335–338. [Google Scholar] [CrossRef]
- Johnston, J.J.; McGovern, S.J. Alcohol related falls: An interesting pattern of injuries. Emerg. Med. J. 2004, 21, 185–188. [Google Scholar] [CrossRef]
- WHO Global Report on Falls Prevention in Older Age. Available online: https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHo-Global-report-on-falls-prevention-in-older-age.pdf (accessed on 12 April 2022).
- Kim, S. Risk factors for severe injury following indoor and outdoor falls in geriatric patients. Arch. Gerontol. Geriatr. 2016, 62, 75–82. [Google Scholar] [CrossRef]
- Harvey, L.; Close, J. Traumatic brain injury in older adults: Characteristics, causes and consequences. Injury 2012, 43, 1821–1826. [Google Scholar] [CrossRef]
- Korhonen, N.; Niemi, S.; Parkkari, J.; Sievänen, H.; Kannus, P. Incidence of fall-related traumatic brain injuries among older Finnish adults between 1970 and 2011. JAMA 2013, 309, 1891–1892. [Google Scholar] [CrossRef] [Green Version]
- O’Neill, S.; Brady, R.; Kerssens, J.; Parks, R. Mortality associated with traumatic injuries in the elderly: A population based study. Arch. Gerontol. Geriatr. 2012, 54, e426–e430. [Google Scholar] [CrossRef]
- Chatha, H.; Sammy, I.; Hickey, M.; Sattout, A.; Hollingsworth, J. Falling down a flight of stairs: The impact of age and intoxication on injury pattern and severity. Trauma 2018, 20, 169–174. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Mackey, D.; Liu-Ambrose, T.; Leung, P.; Feldman, F.; Robinovitch, S. Clinical Risk Factors for Head Impact During Falls in Older Adults: A Prospective Cohort Study in Long-Term Care. J. Head Trauma Rehabil. 2017, 32, 168–177. [Google Scholar] [CrossRef]
- Kim, J.; Shin, S.; Im, T.; Lee, K.; Ko, S.; Park, J.; Ahn, K.; Song, K. Development and validation of the Excess Mortality Ratio-adjusted Injury Severity Score Using the International Classification of Diseases 10th Edition. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2009, 16, 454–464. [Google Scholar] [CrossRef]
- Murray, C.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- Close, J.; Lord, S.; Antonova, E.; Martin, M.; Lensberg, B.; Taylor, M.; Hallen, J.; Kelly, A. Older people presenting to the emergency department after a fall: A population with substantial recurrent healthcare use. Emerg. Med. J. 2012, 29, 742–747. [Google Scholar] [CrossRef]
- Nakada, T.; Nakao, S.; Mizushima, Y.; Matsuoka, T. Association between male sex and increased mortality after falls. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2015, 22, 708–713. [Google Scholar] [CrossRef] [Green Version]
- Duckham, R.; Procter-Gray, E.; Hannan, M.; Leveille, S.; Lipsitz, L.; Li, W. Sex differences in circumstances and consequences of outdoor and indoor falls in older adults in the MOBILIZE Boston cohort study. BMC Geriatr. 2013, 13, 133. [Google Scholar] [CrossRef] [Green Version]
- Brinck, T.; Heinänen, M.; Söderlund, T.; Lefering, R.; Handolin, L. Does arrival time affect outcomes among severely injured blunt trauma patients at a tertiary trauma centre? Injury 2019, 50, 1929–1933. [Google Scholar] [CrossRef]
- Guly, H.; Leighton, G.; Woodford, M.; Bouamra, O.; Lecky, F. The effect of working hours on outcome from major trauma. Emerg. Med. J. 2006, 23, 276–280. [Google Scholar] [CrossRef] [Green Version]
- Drahota, A.; Ward, D.; Udell, J.; Soilemezi, D.; Ogollah, R.; Higgins, B.; Dean, T.; Severs, M. Pilot cluster randomised controlled trial of flooring to reduce injuries from falls in wards for older people. Age Ageing 2013, 42, 633–640. [Google Scholar] [CrossRef] [Green Version]
- Gustavsson, J.; Bonander, C.; Andersson, R.; Nilson, F. Investigating the fall-injury reducing effect of impact absorbing flooring among female nursing home residents: Initial results. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2015, 21, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.; Kenny, R. Cardiovascular assessment of falls in older people. Clin. Interv. Aging 2006, 1, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Gribbin, J.; Hubbard, R.; Gladman, J.; Smith, C.; Lewis, S. Risk of falls associated with antihypertensive medication: Population-based case-control study. Age Ageing 2010, 39, 592–597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Alcohol-Related | Non-Alcohol-Related | p-Value | |
|---|---|---|---|
| (N = 2092) | (N = 29,085) | ||
| General characteristics | |||
| Sex, male (%) | 1540 (73.6) | 10,434 (35.9) | <0.001 |
| Age group, years old (%) | <0.001 | ||
| 65~74 | 1554 (74.3) | 12,129 (41.7) | |
| 75~84 | 762 (23.5) | 12,256 (42.1) | |
| ≥85 | 46 (2.2) | 4700 (16.2) | |
| Average age (years) | 71.4 ± 5.2 | 76.7 ± 7.4 | <0.001 |
| Season of injury (%) | 0.008 | ||
| Spring (March–May) | 537 (25.7) | 6552 (22.5) | |
| Summer (June–August) | 478 (22.8) | 6849 (23.5) | |
| Autumn (September–November) | 551 (26.3) | 8236 (28.3) | |
| Winter (December–February) | 526 (25.1) | 7448 (25.6) | |
| Time of injury (%) | <0.001 | ||
| 00:00–05:59 h | 295 (14.1) | 2063 (7.1) | |
| 06:00–11:59 h | 205 (9.8) | 8064 (27.7) | |
| 12:00–17:59 h | 452 (21.6) | 11,146 (38.3) | |
| 18:00–23:59 h | 1140 (54.5) | 7812 (26.9) | |
| Occupation, employed (%) | N = 388 | N = 11,792 | 0.811 |
| 92 (23.7) | 2732 (23.2) | ||
| Education (%) | N = 144 | N = 4356 | 0.001 |
| Uneducated or elementary school | 53 (36.8) | 2369 (54.4) | |
| Junior high school | 34 (23.6) | 728 (16.7) | |
| High school | 37 (25.7) | 830 (19.1) | |
| ≥College | 20 (13.9) | 429 (9.8) | |
| Transportation to ED (%) | N = 2087 | N = 29,031 | <0.001 |
| Public ambulance | 1443 (69.1) | 11,482 (39.6) | |
| Other medical facility | 142 (6.8) | 4593 (15.8) | |
| Individual transportation | 502 (24.1) | 12,956 (44.6) | |
| Location of injury (%) | <0.001 | ||
| Residential facility | 430 (20.6) | 17,151 (59.0) | |
| Transportation area | 1318 (63.0) | 6900 (23.7) | |
| Public or commercial facility | 310 (14.8) | 1816 (6.2) | |
| Other area | 34 (1.6) | 3218 (11.1) | |
| Activity during injury (%) | N = 2092 | N = 29,083 | <0.001 |
| Paid or unpaid work | 19 (0.9) | 2437 (8.4) | |
| Sports or leisure activity | 980 (46.8) | 2893 (9.9) | |
| Daily activity | 1069 (51.1) | 23,026 (79.2) | |
| Others | 24 (1.1) | 727 (2.5) | |
| Slippery or non-slippery floor (%) | N = 2092 | N = 29,079 | <0.001 |
| Slippery | 80 (3.8) | 2739 (9.4) | |
| Slope of floor, sloping or flat (%) | N = 2089 | N = 29,068 | <0.001 |
| Sloping | 333 (15.9) | 3322 (11.4) | |
| Presence of obstacles, yes or none (%) | N = 2089 | N = 29,072 | <0.001 |
| Yes | 255 (12.2) | 2807 (9.7) | |
| Presence of lights, none or yes (%) | N = 2089 | N = 29,049 | <0.001 |
| None | 576 (27.6) | 5273 (18.2) | |
| Type of floor, concrete or others (%) | N = 2088 | N = 28,982 | <0.001 |
| Concrete | 2056 (98.5) | 27,640 (95.4) | |
| Clinical characteristics | |||
| Result of ED treatment (%) | N = 2078 | N = 29,068 | <0.001 |
| Discharge | 1679 (80.8) | 16,995 (58.5) | |
| Transfer to other facility | 47 (2.3) | 780 (2.7) | |
| Admission to general ward | 201 (9.7) | 9655 (33.2) | |
| Admission to ICU | 145 (7.0) | 1497 (5.1) | |
| Death at ED | 6 (0.3) | 141 (0.5) | |
| Severe patients (%) | N = 2078 | N = 29,068 | 0.033 |
| 187 (9.0) | 2236 (7.7) | ||
| Major injury location (%) | N = 2082 | N = 29,048 | <0.001 |
| Head and neck | 1660 (79.7) | 10,964 (37.7) | |
| Thorax | 45 (2.2) | 1735 (6.0) | |
| Abdomen | 36 (1.7) | 2581 (8.9) | |
| Upper extremity | 116 (5.6) | 3919 (13.5) | |
| Hip and thigh | 40 (1.9) | 6368 (21.9) | |
| Lower extremity | 33 (1.6) | 2058 (7.1) | |
| Multiple body regions | 152 (7.3) | 1423 (4.9) | |
| Consciousness at ED (%) | N = 1651 | N = 22,619 | <0.001 |
| Alert | 1470 (89.0) | 21,812 (96.4) | |
| Verbal response | 132 (8.0) | 441 (1.9) | |
| Pain response | 38 (2.3) | 242 (1.1) | |
| Unresponsive | 11 (0.7) | 124 (0.5) | |
| Blood pressure (mmHg) | N = 1728 | N = 23,993 | <0.001 |
| Systolic blood pressure | 130.3 ± 24.4 | 143.4 ± 27.5 | <0.001 |
| Diastolic blood pressure | 76.0 ± 14.4 | 79.2 ± 15.0 | |
| EMR-ISS | N = 2087 | N = 29,033 | <0.001 |
| 15.4 ± 12.2 | 14.0 ± 10.3 | ||
| Univariate | Multivariate | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% C.I. | p-Value | OR | 95% C.I. | p-Value | ||
| Male sex vs. female | 4.99 | 4.51–5.51 | <0.001 | Male sex vs. female | 4.07 | 3.63–4.57 | <0.001 |
| Age group, years old | Age group, years old | ||||||
| ≥85 | 1.00 | ≥85 | 1.00 | ||||
| 65–74 years | 13.09 | 9.75–17.59 | <0.001 | 65–74 years | 8.31 | 6.10–11.32 | <0.001 |
| 75–84 years | 4.10 | 3.03–5.56 | <0.001 | 75–84 years | 3.14 | 2.28–4.31 | <0.001 |
| Season of injury | |||||||
| Autumn | 1.00 | ||||||
| Winter | 1.06 | 0.93–1.19 | 0.390 | ||||
| Spring | 1.23 | 1.08–1.39 | 0.001 | ||||
| Summer | 1.04 | 0.92–1.18 | 0.513 | ||||
| Time of injury | Time of injury | ||||||
| 06:00–11:59 h | 1.00 | 06:00–11:59 h | 1.00 | ||||
| 12:00–17:59 h | 1.60 | 1.35–1.89 | <0.001 | 12:00–17:59 h | 1.41 | 1.18–1.70 | <0.001 |
| 18:00–23:59 h | 5.74 | 4.93–6.68 | <0.001 | 18:00–23:59 h | 4.22 | 3.56–5.00 | <0.001 |
| 00:00–05:59 h | 5.63 | 4.68–6.77 | <0.001 | 00:00–05:59 h | 4.76 | 3.84–5.91 | <0.001 |
| Transportation to ED | Transportation to ED | ||||||
| Other medical facility | 1.00 | Other medical facility | 1.00 | ||||
| Public ambulance | 4.07 | 3.41–4.85 | <0.001 | Public ambulance | 3.89 | 3.44–4.40 | <0.001 |
| Individual transportation | 1.25 | 1.04–1.51 | 0.019 | Individual transportation | 1.24 | 1.00–1.54 | 0.048 |
| Location of injury | Location of injury | ||||||
| Other area | 1.00 | Other area | 1.00 | ||||
| Residential facility | 2.37 | 1.67–3.37 | <0.001 | Residential facility | 3.91 | 2.62–5.84 | <0.001 |
| Transportation area | 18.08 | 12.83–25.48 | <0.001 | Transportation area | 16.15 | 10.93–23.85 | <0.001 |
| Public or commercial facility | 16.16 | 11.29–23.13 | <0.001 | Public or commercial facility | 12.15 | 8.10–18.24 | <0.001 |
| Activity during injury | Activity during injury | ||||||
| Paid or unpaid work | 1.00 | Paid or unpaid work | 1.00 | ||||
| Sports or leisure activity | 43.45 | 27.51–68.63 | <0.001 | Sports or leisure activity | 33.09 | 20.54–53.29 | <0.001 |
| Daily activity | 5.96 | 3.78–9.39 | <0.001 | Daily activity | 6.17 | 3.85–9.89 | <0.001 |
| Others | 4.23 | 2.31–7.77 | <0.001 | Others | 6.28 | 3.27–12.04 | <0.001 |
| Non-slippery condition of floor vs. slippery | 2.62 | 2.08–3.28 | <0.001 | Non-slippery condition of floor vs. slippery | 3.14 | 2.42–4.08 | <0.001 |
| Sloping vs. flat floor | 1.47 | 1.30–1.66 | <0.001 | ||||
| Presence of obstacles on floor | 1.30 | 1.14–1.49 | <0.001 | Presence of obstacles on floor | 1.33 | 1.13–1.58 | 0.001 |
| Absence of lights | 1.72 | 1.55–1.90 | <0.001 | Absence of lights | 2.13 | 1.87–2.42 | <0.001 |
| Concrete floor vs. other types | 3.12 | 2.19–4.44 | <0.001 | Concrete floor vs. other types | 1.92 | 1.25–2.94 | <0.001 |
| Alcohol-Related | Non-Alcohol-Related | ||||||
|---|---|---|---|---|---|---|---|
| Severe (N = 187) | Non-Severe (N = 1891) | p-Value | Severe (N = 2236) | Non-Severe (N = 26,832) | p-Value | ||
| Sex, male (%) | 154 (82.4) | 1378 (72.9) | 0.005 | Sex, male (%) | 1090 (48.7) | 9334 (34.8) | <0.001 |
| Age group, years old (%) | 0.775 | Age group, years old (%) | 0.053 | ||||
| 65–74 years | 141 (75.4) | 1399 (74.0) | 65–74 years | 964 (43.1) | 11,155 (41.6) | ||
| 75–84 years | 41 (21.9) | 451 (23.8) | 75–84 years | 950 (42.5) | 11,301 (42.1) | ||
| ≥85 | 5 (2.7) | 41 (2.2) | ≥85 | 322 (14.4) | 4376 (16.3) | ||
| Average age (years) | 71.2 ± 5.1 | 17.4 ± 5.2 | 0.527 | Average age (years) | 76.4 ± 7.2 | 76.7 ± 7.4 | 0.019 |
| Season of injury (%) | 0.401 | Season of injury (%) | 0.045 | ||||
| Spring | 49 (26.2) | 486 (25.7) | Spring | 503 (22.5) | 6041 (22.5) | ||
| Summer | 51 (27.3) | 422 (22.3) | Summer | 524 (2.4) | 6321 (23.6) | ||
| Autumn | 43 (23.0) | 504 (26.7) | Autumn | 682 (30.5) | 7551 (28.1) | ||
| Winter | 44 (23.5) | 479 (25.3) | Winter | 527 (23.6) | 6919 (25.8) | ||
| Time of injury (%) | 0.001 | Time of injury (%) | 0.165 | ||||
| 00:00–05:59 h | 26 (13.9) | 265 (14.0) | 00:00–05:59 h | 171 (7.6) | 1889 (7.0) | ||
| 06:00–11:59 h | 31 (16.6) | 174 (9.2) | 06:00–11:59 h | 579 (25.9) | 7482 (27.9) | ||
| 12:00–17:59 h | 49 (26.2) | 401 (21.2) | 12:00–17:59 h | 886 (39.6) | 10,253 (38.2) | ||
| 18:00–23:59 h | 81 (43.3) | 1051 (55.6) | 18:00–23:59 h | 600 (26.8) | 7208 (26.9) | ||
| Occupation, employed (%) | N = 16151 (31.7) | N = 22741 (18.1) | 0.002 | Occupation, employed (%) | N = 1934519 (26.8) | N = 98572213 (22.5) | <0.001 |
| Education (%) | N = 68 | N = 76 | 0.687 | Education (%) | N = 740 | N = 3616 | 0.015 |
| Uneducated or elementary school | 23 (33.8) | 30 (39.5) | Uneducated or elementary school | 363 (49.1) | 2006 (55.5) | ||
| Junior high school | 18 (26.5) | 16 (21.1) | Junior high school | 141 (19.1) | 587 (16.2) | ||
| High school | 16 (23.5) | 21 (27.6) | High school | 153 (20.7) | 677 (18.7) | ||
| ≥college | 11 (16.2) | 9 (11.8) | ≥college | 83 (11.2) | 346 (9.6) | ||
| Transportation to ED (%) | N = 187 | N = 1886 | <0.001 | Transportation to ED (%) | N = 2233 | N = 26,781 | <0.001 |
| Public ambulance | 109 (58.3) | 1323 (70.1) | Public ambulance | 1004 (45.0) | 10,467 (39.1) | ||
| Other medical facility | 54 (28.9) | 88 (4.7) | Other medical facility | 792 (35.5) | 3800 (14.2) | ||
| Individual transportation | 24 (12.8) | 475 (25.2) | Individual transportation | 437 (19.6) | 12,514 (46.7) | ||
| Location of injury (%) | <0.001 | Location of injury (%) | <0.001 | ||||
| Residential facility | 62 (33.2) | 367 (19.4) | Residential facility | 1318 (58.9) | 15,830 (59.0) | ||
| Transportation area | 84 (44.9) | 1225 (64.8) | Transportation area | 395 (17.7) | 6495 (24.2) | ||
| Public or commercial facility | 35 (18.7) | 272 (14.4) | Public or commercial facility | 125 (5.6) | 1690 (6.3) | ||
| Other area | 6 (3.2) | 27 (1.4) | Other area | 398 (17.8) | 2817 (10.5) | ||
| Activity during injury (%) | 0.149 | Activity during injury (%) | N = 2236 | N = 26,830 | <0.001 | ||
| Paid or unpaid work | 3 (1.6) | 16 (0.8) | Paid or unpaid work | 344 (15.4) | 2093 (7.8) | ||
| Sports or leisure activity | 84 (44.9) | 888 (47.0) | Sports or leisure activity | 173 (7.7) | 2717 (10.1) | ||
| Daily activity | 95 (50.8) | 968 (51.2) | Daily activity | 1580 (70.7) | 21,432 (79.9) | ||
| Others | 5 (2.7) | 19 (1.0) | Others | 139 (6.2) | 588 (2.2) | ||
| Slippery or non-slippery floor (%) | 0.110 | Slippery or non-slippery floor (%) | <0.001 | ||||
| Slippery | 3 (1.6) | 76 (4.0) | Slippery | 119 (5.3) | 2618 (9.8) | ||
| Slope of floor, sloping or flat (%) | N = 186 | N = 1889 | <0.001 | Slope of floor, sloping or flat (%) | N = 2233 | N = 26,818 | <0.001 |
| Sloping | 49 (26.3) | 282 (14.9) | Sloping | 310 (13.9) | 3010 (11.2) | ||
| Presence of obstacles, yes or none (%) | N = 186 | N = 1889 | 0.007 | Presence of obstacles, yes or none (%) | N = 2233 | N = 26,822 | <0.001 |
| Yes | 35 (18.8) | 219 (11.6) | Yes | 265 (11.9) | 2540 (9.5) | ||
| Presence of lights, none or yes (%) | N = 186 | N = 1889 | 0.048 | Presence of lights, none or yes (%) | N = 2233 | N = 26,799 | 0.016 |
| None | 63 (33.9) | 509 (26.9) | None | 448 (20.1) | 4822 (18.0) | ||
| Type of floor, concrete or others (%) | N = 186 | N = 1888 | 0.061 | Type of floor, concrete or others (%) | N = 2220 | N = 26,745 | <0.001 |
| Concrete | 180 (96.8) | 1862 (98.6) | Concrete | 2062 (92.9) | 25,562 (95.6) | ||
| Univariate | Multivariate | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% C.I. | p-Value | OR | 95% C.I. | p-Value | ||
| Male sex vs. female | 1.74 | 1.18–2.56 | 0.005 | Male sex vs. female | 1.78 | 1.18–2.70 | 0.007 |
| Age group, years old | |||||||
| 75-84 | 1.00 | ||||||
| 65-74 | 1.11 | 0.77–1.60 | 0.578 | ||||
| ≥85 | 1.34 | 0.50–3.59 | 0.558 | ||||
| Season of injury | |||||||
| Autumn | 1.00 | ||||||
| Winter | 1.08 | 0.69–1.67 | 0.741 | ||||
| Spring | 1.18 | 0.77–1.81 | 0.445 | ||||
| Summer | 1.42 | 0.93–2.17 | 0.109 | ||||
| Time of injury | Time of injury | ||||||
| 18:00–23:59 h | 1.00 | 18:00–23:59 h | 1.00 | ||||
| 00:00–05:59 h | 1.27 | 0.80–2.02 | 0.306 | ||||
| 06:00–11:59 h | 2.31 | 1.48–3.60 | <0.001 | 06:00–11:59 h | 1.66 | 1.02–2.71 | 0.043 |
| 12:00–17:59 h | 1.59 | 1.09–2.30 | 0.015 | 12:00–17:59 h | 1.58 | 1.06–2.34 | 0.024 |
| Transportation to ED | Transportation to ED | ||||||
| Individual transportation | 1.00 | Individual transportation | 1.00 | ||||
| Public ambulance | 1.63 | 1.04–2.57 | 0.035 | Public ambulance | 1.69 | 1.06–2.70 | 0.028 |
| Other medical facility | 12.15 | 7.14–20.67 | <0.001 | Other medical facility | 12.69 | 7.30–22.08 | <0.001 |
| Location of injury | Location of injury | ||||||
| Transportation area | 1.00 | Transportation area | 1.00 | ||||
| Public or commercial facility | 1.88 | 1.24–2.84 | 0.003 | ||||
| Other area | 3.24 | 1.30–8.07 | 0.011 | ||||
| Residential facility | 2.46 | 1.74–3.49 | <0.001 | Residential facility | 2.26 | 1.55–3.30 | <0.001 |
| Activity during injury | |||||||
| Sports or leisure activity | 1.00 | ||||||
| Paid or unpaid work | 1.98 | 0.57–6.94 | 0.285 | ||||
| Daily activity | 1.04 | 0.76–1.41 | 0.814 | ||||
| Others | 2.78 | 1.01–7.64 | 0.047 | ||||
| Non-slippery condition of floor vs. slippery | 2.57 | 0.80–8.22 | 0.112 | ||||
| Sloping vs. flat floor | 2.04 | 1.44–2.89 | <0.001 | Sloping vs. flat floor | 1.83 | 1.22–2.75 | 0.004 |
| Presence of obstacles on floor | 1.77 | 1.19–2.62 | 0.005 | ||||
| Absence of lights | 1.39 | 1.01–1.91 | 0.044 | ||||
| Other types vs. concrete | 2.39 | 0.97–5.88 | 0.058 | ||||
| Univariate | Multivariate | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% C.I. | p-Value | OR | 95% C.I. | p-Value | ||
| Male sex vs. female | 1.78 | 1.64–1.94 | <0.001 | Male sex vs. female | 1.67 | 1.52–1.83 | <0.001 |
| Age group, years old | Age group, years old | ||||||
| ≥85 | 1.00 | ≥85 | 1.00 | ||||
| 75–84 years | 1.17 | 1.03–1.34 | 0.016 | 75–84 years | 1.33 | 1.16–1.53 | <0.001 |
| 65–74 years | 1.14 | 1.00–1.30 | 0.047 | 65–74 years | 1.20 | 1.05–1.37 | 0.008 |
| Season of injury | |||||||
| Winter | 1.00 | ||||||
| Spring | 1.09 | 0.96–1.24 | 0.169 | ||||
| Summer | 1.09 | 0.96–1.23 | 0.186 | ||||
| Autumn | 1.19 | 1.05–1.34 | 0.005 | ||||
| Time of injury | |||||||
| 06:00–11:59 h | 1.00 | ||||||
| 00:00–05:59 h | 1.17 | 0.98–1.40 | 0.084 | ||||
| 12:00–17:59 h | 1.12 | 1.00–1.25 | 0.047 | ||||
| 18:00–23:59 h | 1.08 | 0.96–1.21 | 0.228 | ||||
| Transportation to ED | Transportation to ED | ||||||
| Individual transportation | 1.00 | Individual transportation | 1.00 | ||||
| Public ambulance | 2.75 | 2.45–3.08 | <0.001 | Public ambulance | 2.77 | 2.47–3.12 | <0.001 |
| Other medical facility | 5.97 | 5.28–6.75 | <0.001 | Other medical facility | 5.83 | 5.14–6.62 | <0.001 |
| Location of injury | Location of injury | ||||||
| Transportation area | 1.00 | Transportation area | 1.00 | ||||
| Public or commercial facility | 1.22 | 0.99–1.50 | 0.065 | ||||
| Other area | 2.32 | 2.01–2.69 | <0.001 | Other area | 1.27 | 1.07–1.50 | 0.005 |
| Residential facility | 1.37 | 1.2–1.54 | <0.001 | Residential facility | 1.24 | 1.10–1.41 | <0.001 |
| Activity during injury | Activity during injury | ||||||
| Sports or leisure activity | 1.00 | Sports or leisure activity | 1.00 | ||||
| Daily activity | 1.16 | 0.99–1.36 | 0.076 | ||||
| Others | 3.71 | 2.92–4.72 | <0.001 | Others | 2.80 | 2.17–3.62 | <0.001 |
| Paid or unpaid work | 2.58 | 2.13–3.13 | <0.001 | Paid or unpaid work | 1.84 | 1.50–2.26 | <0.001 |
| Non-slippery condition of floor vs. slippery | 1.92 | 1.59–2.32 | <0.001 | Non-slippery condition of floor vs. slippery | 1.64 | 1.36–1.99 | <0.001 |
| Sloping floor vs. flat | 1.28 | 1.12–1.45 | <0.001 | ||||
| Presence of obstacles on floor | 1.29 | 1.13–1.47 | <0.001 | Presence of obstacles on floor | 1.40 | 1.21–1.61 | <0.001 |
| Absence of lights | 1.14 | 1.03–1.28 | 0.015 | Absence of lights | 0.86 | 0.76–0.96 | 0.010 |
| Other types vs. concrete | 1.66 | 1.39–1.97 | <0.001 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, J.S.; Kim, S.H. Severe Ground Fall Injury Associated with Alcohol Consumption in Geriatric Patients. Healthcare 2022, 10, 1111. https://doi.org/10.3390/healthcare10061111
Hwang JS, Kim SH. Severe Ground Fall Injury Associated with Alcohol Consumption in Geriatric Patients. Healthcare. 2022; 10(6):1111. https://doi.org/10.3390/healthcare10061111
Chicago/Turabian StyleHwang, Jung Sung, and Sun Hyu Kim. 2022. "Severe Ground Fall Injury Associated with Alcohol Consumption in Geriatric Patients" Healthcare 10, no. 6: 1111. https://doi.org/10.3390/healthcare10061111
APA StyleHwang, J. S., & Kim, S. H. (2022). Severe Ground Fall Injury Associated with Alcohol Consumption in Geriatric Patients. Healthcare, 10(6), 1111. https://doi.org/10.3390/healthcare10061111






