Differential Screening of Herniated Lumbar Discs Based on Bag of Visual Words Image Classification Using Digital Infrared Thermographic Images
Abstract
:1. Introduction
2. Materials and Methods
2.1. Dataset and IRBs
2.2. Inclusion and Exclusion Criteria
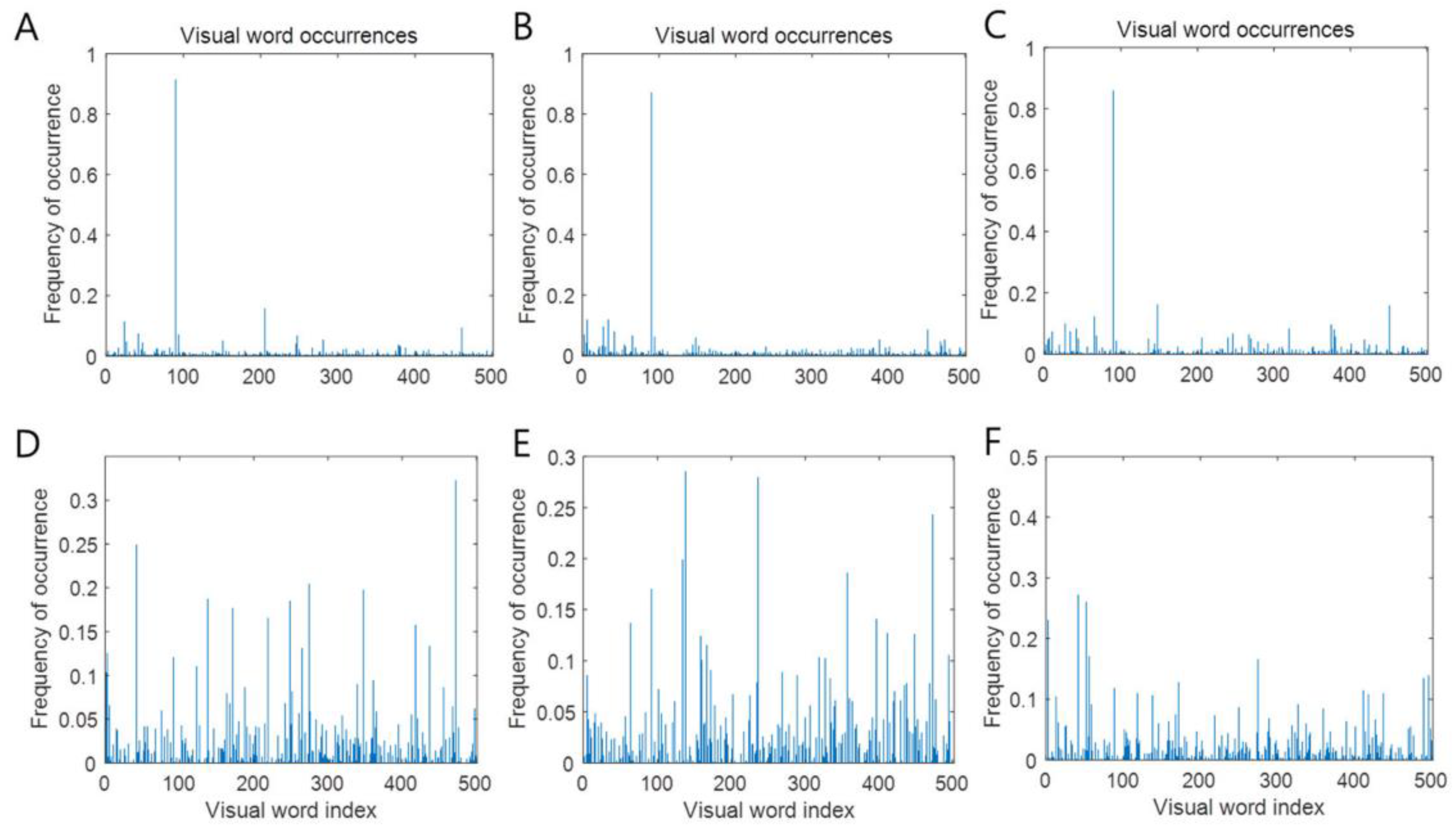
2.3. Clinical Data Collection, Labeling, Preprocessing, and Bag of Words Machine-Learning-Based Classification Modeling
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lauder, T.D. Physical examination signs, clinical symptoms, and their relationship to electrodiagnostic findings and the presence of radiculopathy. Phys. Med. Rehabil. Clin. 2002, 13, 451–467. [Google Scholar] [CrossRef]
- Van Der Windt, D.A.; Simons, E.; Riphagen, I.I.; Ammendolia, C.; Verhagen, A.P.; Laslett, M.; Devillé, W.; Deyo, R.A.; Bouter, L.M.; de Vet, H.C. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst. Rev. 2010, 2, CD007431. [Google Scholar] [CrossRef] [PubMed]
- Modic, M.T.; Obuchowski, N.A.; Ross, J.S.; Brant-Zawadzki, M.N.; Grooff, P.N.; Mazanec, D.J.; Benzel, E.C. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology 2005, 237, 597–604. [Google Scholar] [CrossRef] [Green Version]
- Wassenaar, M.; van Rijn, R.M.; van Tulder, M.W.; Verhagen, A.P.; van der Windt, D.A.; Koes, B.W.; de Boer, M.R.; Ginai, A.Z.; Ostelo, R.W. Magnetic resonance imaging for diagnosing lumbar spinal pathology in adult patients with low back pain or sciatica: A diagnostic systematic review. Eur. Spine J. 2012, 21, 220–227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fisher, M.A. Electrophysiology of radiculopathies. Clin. Neurophysiol. 2002, 113, 317–335. [Google Scholar] [CrossRef]
- Pochaczevsky, R.; Wexler, C.E.; Meyers, P.H.; Epstein, J.A.; Marc, J.A. Liquid crystal thermography of the spine and extremities: Its value in the diagnosis of spinal root syndromes. J. Neurosurg. 1982, 56, 386–395. [Google Scholar] [CrossRef]
- Al-Nakhli, H.H.; Petrofsky, J.S.; Laymon, M.S.; Berk, L.S. The use of thermal infra-red imaging to detect delayed onset muscle soreness. J. Vis. Exp. 2012, 59, e3551. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.Y. Infrared thermography and pain scale correlation in lumbar disc herniation. J. Korean Neurosurg. Soc. 1999, 28, 253–258. [Google Scholar]
- Brelsford, K.L.; Uematsu, S. Thermographic presentation of cutaneous sensory and vasomotor activity in the injured peripheral nerve. J. Neurosurg. 1985, 62, 711–715. [Google Scholar] [CrossRef]
- Tuzgen, S.; Dursun, S.; Abuzayed, B. Electrical skin resistance and thermal findings in patients with lumbar disc herniation. J. Clin. Neurophysiol. 2010, 27, 303–307. [Google Scholar] [CrossRef]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H.J. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Zhang, F.; Li, X. Machine learning in ultrasound computer-aided diagnostic systems: A survey. BioMed Res. Int. 2018, 2018, 1–10. [Google Scholar] [CrossRef]
- Wong, S.T. Is pathology prepared for the adoption of artificial intelligence? Cancer Cytopathol. 2018, 126, 373–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Connor, C.W. Artificial intelligence and machine learning in anesthesiology. Anesthesiology 2019, 131, 1346–1359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ellahham, S. Artificial intelligence: The future for diabetes care. Am. J. Med. 2020, 133, 895–900. [Google Scholar] [CrossRef]
- Zhou, L.-Q.; Wang, J.-Y.; Yu, S.-Y.; Wu, G.-G.; Wei, Q.; Deng, Y.-B.; Wu, X.-L.; Cui, X.-W.; Dietrich, C.F. Artificial intelligence in medical imaging of the liver. World J. Gastroenterol. 2019, 25, 672. [Google Scholar] [CrossRef]
- Friberg, S.; Hirsch, C. Anatomical and clinical studies on lumbar disc degeneration. Acta Orthop. Scand. 1949, 19, 222–242. [Google Scholar] [CrossRef] [Green Version]
- Hsu, K.; Zucherman, J.; Shea, W.; Kaiser, J.; White, A.; Schofferman, J.; Amelon, C. High lumbar disc degeneration. Incidence and etiology. Spine 1990, 15, 679–682. [Google Scholar] [CrossRef]
- Jordon, J.; Konstantinou, K.; O’Dowd, J. Herniated lumbar disc. BMJ Clin. Evid. 2009, 2009, 1118. [Google Scholar]
- Csurka, G.; Dance, C.; Fan, L.; Willamowski, J.; Bray, C. Visual categorization with bags of keypoints. In Proceedings of the Workshop on Statistical Learning in Computer Vision, ECCV, Prague, Czech Republic, 15–16 May 2004; pp. 1–2. [Google Scholar]
- Frymoyer, J. Lumbar disk disease: Epidemiology. Instr. Course Lect. 1992, 41, 217–223. [Google Scholar]
- Wu, A.-M.; Zou, F.; Cao, Y.; Xia, D.-D.; He, W.; Zhu, B.; Chen, D.; Ni, W.-F.; Wang, X.-Y.; Kwan, K. Lumbar spinal stenosis: An update on the epidemiology, diagnosis and treatment. AME Med. J. 2017, 2, 1–14. [Google Scholar] [CrossRef]
- Ring, E.; Ammer, K. Infrared thermal imaging in medicine. Physiol. Meas. 2012, 33, R33. [Google Scholar] [CrossRef] [PubMed]
- Ammer, K.; Ring, F. The Thermal Human Body: A Practical Guide to Thermal Imaging; Jenny Stanford Publishing: New York, NY, USA, 2019. [Google Scholar]
- Vreugdenburg, T.D.; Willis, C.D.; Mundy, L.; Hiller, J.E. A systematic review of elastography, electrical impedance scanning, and digital infrared thermography for breast cancer screening and diagnosis. Breast Cancer Res. Treat. 2013, 137, 665–676. [Google Scholar] [CrossRef] [PubMed]
- Mambou, S.J.; Maresova, P.; Krejcar, O.; Selamat, A.; Kuca, K. Breast cancer detection using infrared thermal imaging and a deep learning model. Sensors 2018, 18, 2799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magalhaes, C.; Vardasca, R.; Mendes, J. Recent use of medical infrared thermography in skin neoplasms. Skin Res. Technol. 2018, 24, 587–591. [Google Scholar] [CrossRef]
- Adam, M.; Ng, E.Y.; Tan, J.H.; Heng, M.L.; Tong, J.W.; Acharya, U.R. Computer aided diagnosis of diabetic foot using infrared thermography: A review. Comput. Biol. Med. 2017, 91, 326–336. [Google Scholar] [CrossRef]
- Park, D.; Kim, B.H.; Lee, S.-E.; Kim, D.Y.; Eom, Y.S.; Cho, J.M.; Yang, J.W.; Kim, M.; Kwon, H.D.; Lee, J.W. Application of digital infrared thermography for carpal tunnel syndrome evaluation. Sci. Rep. 2021, 11, 1–11. [Google Scholar] [CrossRef]
- Cho, Y.E.; Kim, Y.S.; Zhang, H.Y. In Multiple Lumbar Intervvertebral Herniation, the Diagnostic Value of Computed Infrared Whole Body Thermography. J. Korean Neurosurg. Soc. 1998, 27, 237–245. [Google Scholar]
- Ryu, S.J.; Zhang, H.Y. Neurilemmoma of deep peroneal nerve sensory branch: Thermographic findings with compression test. J. Korean Neurosurg. Soc. 2015, 58, 286. [Google Scholar] [CrossRef]
- Park, T.Y.; Son, S.; Lim, T.G.; Jeong, T. Hyperthermia associated with spinal radiculopathy as determined by digital infrared thermographic imaging. Medicine 2020, 99, e19483. [Google Scholar] [CrossRef]


| HLD L4/5 | HLD L5/S1 | |||
|---|---|---|---|---|
| Age Group | Male | Female | Male | Female |
| 0–19 | 2 | 1 | 2 | 0 |
| 20–29 | 18 | 15 | 17 | 10 |
| 30–39 | 33 | 30 | 30 | 26 |
| 40–49 | 55 | 43 | 19 | 27 |
| 50–59 | 49 | 57 | 24 | 28 |
| 60–69 | 62 | 68 | 31 | 45 |
| 70 | 46 | 55 | 28 | 21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, G.N.; Zhang, H.Y.; Cho, Y.E.; Ryu, S.J. Differential Screening of Herniated Lumbar Discs Based on Bag of Visual Words Image Classification Using Digital Infrared Thermographic Images. Healthcare 2022, 10, 1094. https://doi.org/10.3390/healthcare10061094
Kim GN, Zhang HY, Cho YE, Ryu SJ. Differential Screening of Herniated Lumbar Discs Based on Bag of Visual Words Image Classification Using Digital Infrared Thermographic Images. Healthcare. 2022; 10(6):1094. https://doi.org/10.3390/healthcare10061094
Chicago/Turabian StyleKim, Gi Nam, Ho Yeol Zhang, Yong Eun Cho, and Seung Jun Ryu. 2022. "Differential Screening of Herniated Lumbar Discs Based on Bag of Visual Words Image Classification Using Digital Infrared Thermographic Images" Healthcare 10, no. 6: 1094. https://doi.org/10.3390/healthcare10061094
APA StyleKim, G. N., Zhang, H. Y., Cho, Y. E., & Ryu, S. J. (2022). Differential Screening of Herniated Lumbar Discs Based on Bag of Visual Words Image Classification Using Digital Infrared Thermographic Images. Healthcare, 10(6), 1094. https://doi.org/10.3390/healthcare10061094






