Impact of a Maternal Motivational Interviewing on Oral Health in the Mother-Child Dyad
Abstract
1. Introduction
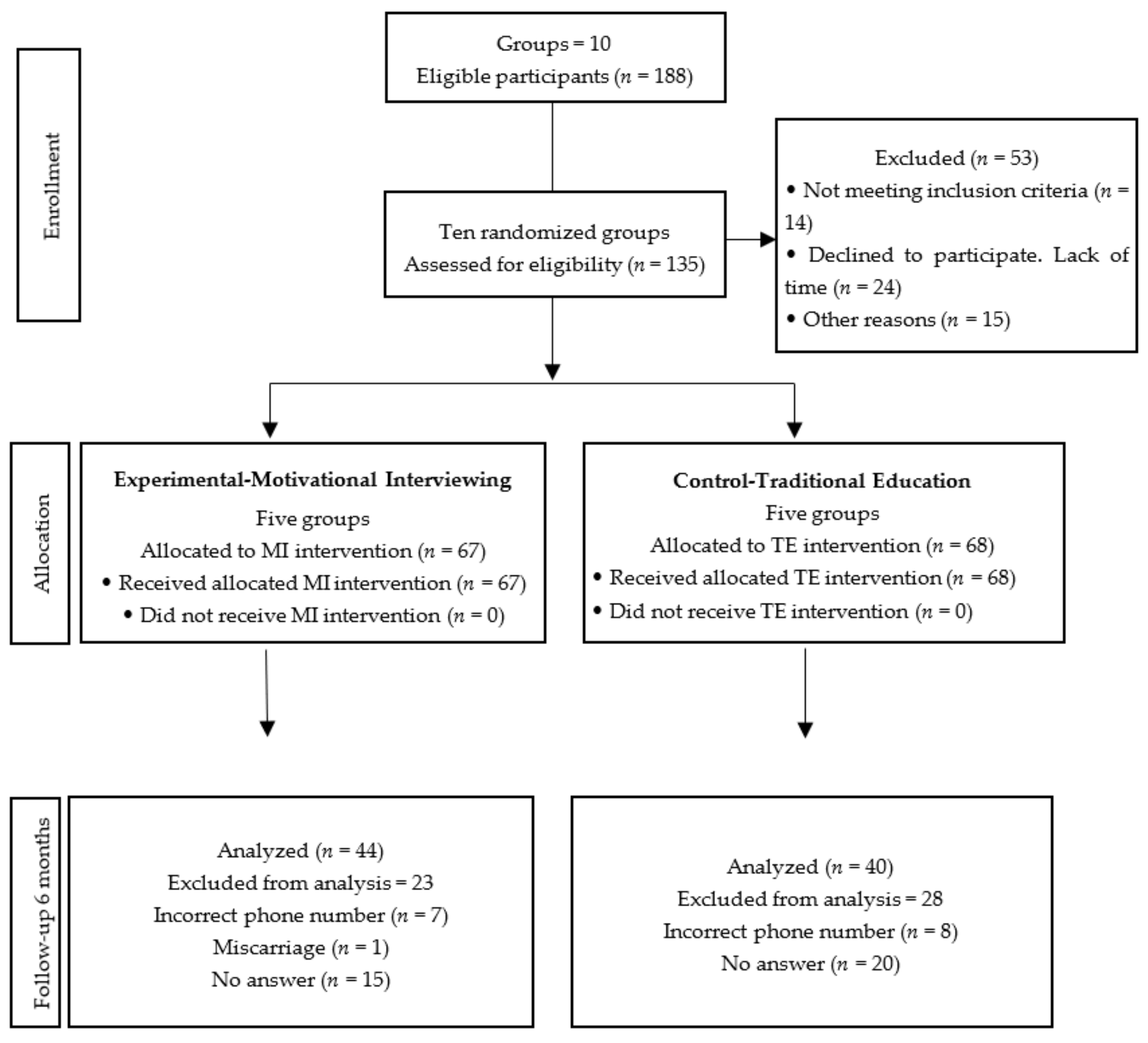
2. Materials and Methods
2.1. Participants
2.2. Sample Size
2.3. Allocation
2.4. Materials
2.5. Methods
2.6. Statistical Analysis
3. Results
3.1. Sociodemographic Data
3.2. Baseline Results
3.3. Follow-up Results
3.4. Multivariate Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hartnett, E.; Haber, J.; Krainovich-Miller Bella, A.; Vasilyeva, A.; Kessler, J. Oral Health in Pregnancy. JOGNN 2016, 45, 565–573. [Google Scholar] [CrossRef]
- Pantano, M.; Abanto, J.; Matijasevich, A.; Augusto-Cardoso, M. Primeiros 1.000 dias de vida. Rev. Assoc. Paul. Cir. Dent. 2018, 72, 490–494. [Google Scholar]
- Vamos, C.; Thompson, E.; Avendano, M.; Daley, E.; Quinonez, R.; Boggess, K. Oral health promotion interventions during pregnancy: A systematic review. Community Dent. Oral Epidemiol. 2015, 43, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Iida, H. Oral Health Interventions During Pregnancy. Dent. Clin. N. Am. 2017, 61, 467–481. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Chin Man Lo, E.; Ching Ching Kot, S.; Chi Wai Chan, K. Motivational Interviewing in Improving Oral Health: A Systematic Review of Randomized Controlled Trials. J. Periodontol. 2014, 85, 426–437. [Google Scholar] [CrossRef]
- Rollnick, S.; Kinnersley, P.; Stott, N. Methods of helping patients with behaviour change. BMJ 1993, 307, 188–190. [Google Scholar] [CrossRef][Green Version]
- Rivera-Mercado, S.; Villouta, F.; Ilabaca, F. Entrevista motivacional: Cuál es su efectividad en problemas prevalentes de la atención primaria? Aten. Primaria 2008, 40, 257–261. [Google Scholar] [CrossRef]
- Miller, W.; Rollnick, S. Motivational Interviewing: Helping People to Change, 3rd ed.; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Rollnick, S.; Miller, W.R. La Entrevista Motivacional. In Ayudar a las Personas a Cambiar; Paidós Psicología Psiquiatría Psicoterapia: Barcelona, Spain, 2015. [Google Scholar]
- Miller, W.; Rose, G. Toward a theory of motivational interviewing. Am. Psychol. 2009, 64, 527–537. [Google Scholar] [CrossRef]
- Flores-Alarcón, L.; Carranza, W. La entrevista motivacional como herramienta para el fomento de cambios en el estilo de vida de personas con enfermedades crónicas no transmisibles. Av. Psicol. Latinoam. 2007, 25, 63–82. [Google Scholar]
- World Health Organization. Ending Childhood Dental Caries: WHO Implementation Manual; OMS: Geneva, Switzerland, 2020. [Google Scholar]
- American Academy of Pediatric Dentistry. Guideline on Perinatal and Infant Oral Health Care. Oral Health Polices Ref. Man. 2016, 38, 150–154. [Google Scholar]
- Naidu, R.; Nunn, J.; Irwin, J. The effect of Motivational Interviewing on oral healthcare knowledge, attitudes and behaviour of parents and caregivers of preschool children: An exploratory randomized controlled study. BMC Oral Health 2015, 15, 101. [Google Scholar] [CrossRef]
- Harrison, R. Motivational interviewing (MI) compared to conventional education (CE) has potential to improving oral health behaviors. J. Evid.-Based Dent. Pract. 2014, 14, 124–126. [Google Scholar] [CrossRef]
- Freudenthal, J. Motivational Interviewing (MI) as An Intervention for Early Childhood Caries Risk-Related Behaviors. J. Dent. Hyg. 2008, 82, 1. [Google Scholar]
- Faustino-Silva, D.; Carriconde, B.; Meyer, E.; Neves, F.; Keller, R.; Balbinot, J. Motivational interviewing effects on caries prevention in children differ by income: A randomized cluster trial. Community Dent. Oral Epidemiol. 2019, 47, 477–484. [Google Scholar] [CrossRef]
- Fleiss, J. Statistical Methods for Rates and Proportions; John Wiley & Sons: New York, NY, USA, 1981. [Google Scholar]
- Ramírez-Trujillo, M.A.; Villanueva-Vilchis, M.C.; Aguilar-Díaz, F.C.; de la Fuente-Hernández, J.; Faustino-Silva, D.D.; Gaitán-Cepeda, L.A. Validation of an Instrument to Determine Oral Health Knowledge, Attitudes, and Practices During Pregnancy. BMC Oral Health 2021, 21, 554. [Google Scholar] [CrossRef]
- Asociación Española de Neuropsiquiatría. Psiquiatría Perinatal y del Niño de 0–3 Años; AEN (Sección de Infantil) Y SEPYPNA: Madrid, Spain, 2015. [Google Scholar]
- Finlayson, T.; Siefert, K.; Ismail, A.; Sohn, W. Maternal self-efficacy and 1- to 5-year-old children’s brushing habits. Community Dent. Oral Epidemiol. 2007, 35, 272–281. [Google Scholar] [CrossRef]
- Weinstein, P.; Harrison, R.; Benton, T. Motivating mothers to prevent caries: Confirming the benefit of counseling. J. Am. Dent. Assoc. 2006, 137, 789–793. [Google Scholar] [CrossRef]
- Borrelli, B.; Tooley, E.; Scott-Sheldon, L. Motivational Interviewing for Parent-child Health Interventions: A Systematic Review and Meta-Analysis. Pediatr. Dent. 2015, 37, 254–265. [Google Scholar]
- Flórez-Alarcón, L.; Gantiva, C. Terapias motivacionales breves: Diferencias entre la aplicación individual y grupal para la moderación del consumo de alcohol y de las variables psicológicas asociadas al cambio. Acta Colomb. Psicol. 2009, 12, 13–26. [Google Scholar]
- Melnick, R.; Schilling, C.; Meyer, E.; Faustino-Silva, D. Effectiveness of motivational interviewing in smoking groups in primary healthcare: A community-based randomized cluster trial. Cad. Saúde Pública 2020, 36, e00038820. [Google Scholar] [CrossRef]
- Seff, I.; Vahedi, L.; McNelly, S.; Kormawa, E.; Stark, L. Remote evaluations of violence against women and girls interventions: A rapid scoping review of tools, ethics and safety. BMJ Glob. Health 2021, 6, e006780. [Google Scholar] [CrossRef]
- Campbell, M.; Piaggio, G.; Elbourne, D. Consort 2010 statement: Extension to cluster randomised trials. BMJ 2012, 345, e5661. [Google Scholar] [CrossRef] [PubMed]
| Participants Commencing the Study | Participants Abandoning the Study | |||||||
|---|---|---|---|---|---|---|---|---|
| MI (n = 67) | TE (n = 68) | Total (n = 135) | pa | MI (n = 67) | TE (n = 68) | Total (n = 51) | pa | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |||
| Educational level | ||||||||
| Elementary | 12 (18) | 16 (24) | 28 (21) | 0.41 | 1 (4.4) | 7 (25) | 8 (15.7) | 0.11 |
| Secondary | 38 (57) | 32 (47) | 70 (53) | 17 (73.9) | 11 (39.3) | 28 (54.9) | ||
| High school and more | 17 (25) | 20 (22) | 37(27) | 5 (21.7) | 10 (35.7) | 15 (29.4) | ||
| Marital status | ||||||||
| No partner | 14 (21) | 18 (26) | 32 (24) | 0.52 | 4 (17.4) | 5 (17.9) | 9 (17.6) | 0.99 |
| Cohabiting | 40 (60) | 34 (50) | 74 (55) | 15 (65.2) | 18 (64.2) | 33 (64.8) | ||
| Married | 13(19) | 16 (24) | 29 (21) | 4 (17.4) | 5 (17.9) | 9 (17.6) | ||
| First pregnancy | ||||||||
| Yes | 31 (46) | 41 (60) | 72 (53) | 0.10 | 12 (52.2) | 15 (53.6) | 27(52.9) | 0.92 |
| No | 36 (54) | 27 (40) | 63 (47) | 11 (47.8) | 13 (46.4) | 24 (47.1) | ||
| Use of dental services during pregnancy | ||||||||
| Yes | 36 (54) | 31 (46) | 67 (49.6) | 0.39 | 9 (39.1) | 15 (53.6) | 24 (47.1) | 0.40 |
| No | 31 (46) | 37 (54) | 68 (50.4) | 14 (60.9) | 13 (46.4) | 27 (52.9) | ||
| Psychoprophylactic course | ||||||||
| Yes | 5 (8) | 11 (17) | 16 (12) | 0.52 | 0 (0) | 4 (14) | 4 (8) | 0.82 |
| No | 62 (92) | 57 (83) | 119 (88) | 23 (100) | 24 (86) | 47 (92) | ||
| Variable | Motivational Interview | Traditional Education | Total | Mann Whitney Test | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD a | n | Mean | SD | n | Mean | SD | p | ||
| COHKAP | Knowledge BL b | 67 | 4.15 | 1.85 | 68 | 3.87 | 1.93 | 135 | 4.01 | 1.89 | 0.34 |
| Knowledge 6M c | 44 | 5.11 | 1.16 | 40 | 3.92 | 1.16 | 84 | 4.54 | 1.7 | p < 0.001 | |
| Wilcoxon | p < 0.001 | 0.83 | p < 0.001 | ||||||||
| Attitudes BL | 67 | 15.25 | 3.17 | 68 | 14.82 | 3.99 | 135 | 15.04 | 3.6 | 0.64 | |
| Attitudes 6M | 44 | 17.38 | 2.87 | 40 | 15.17 | 3.65 | 84 | 16.33 | 3.43 | p < 0.001 | |
| Wilcoxon | p < 0.001 | 0.09 | p < 0.001 | ||||||||
| Practices BL | 67 | 11.73 | 2.78 | 68 | 11.41 | 3.63 | 135 | 11.57 | 3.23 | 0.94 | |
| Practices 6M | 44 | 13.65 | 2.38 | 40 | 11.80 | 3.26 | 84 | 12.77 | 2.97 | p < 0.001 | |
| Wilcoxon | p < 0.001 | 0.07 | p < 0.001 | ||||||||
| Total BL | 67 | 31.13 | 6.18 | 68 | 30.10 | 8.35 | 135 | 30.61 | 7.35 | 0.61 | |
| Total 6M | 44 | 36.15 | 5.32 | 40 | 30.90 | 7.79 | 84 | 33.65 | 7.08 | p < 0.001 | |
| Wilcoxon | p < 0.001 | 0.69 | p < 0.001 | ||||||||
| MOHKAP | Knowledge BL b | 67 | 1.97 | 1.19 | 68 | 2.03 | 1.19 | 135 | 2.00 | 1.19 | 0.77 |
| Knowledge 6M c | 44 | 3.25 | 0.89 | 40 | 2.57 | 10.5 | 84 | 2.92 | 1.02 | p < 0.001 | |
| Wilcoxon | p < 0.001 | 0.002 | p < 0.001 | ||||||||
| Attitudes BL | 67 | 6.28 | 1.2 | 68 | 5.99 | 2.12 | 135 | 6.13 | 1.72 | 0.93 | |
| Attitudes 6M | 44 | 7.22 | 0.85 | 40 | 6.35 | 2.13 | 84 | 6.80 | 1.64 | 0.057 | |
| Wilcoxon | p < 0.001 | 0.16 | p < 0.001 | ||||||||
| Practices BL | 67 | 11.51 | 3.11 | 68 | 10.93 | 2.96 | 135 | 11.21 | 3.04 | 0.12 | |
| Practices 6M | 44 | 13.81 | 2.17 | 40 | 11.52 | 2.77 | 84 | 12.72 | 2.71 | p < 0.001 | |
| Wilcoxon | p < 0.001 | 0.096 | p < 0.001 | ||||||||
| Total BL | 67 | 19.76 | 4.22 | 68 | 18.94 | 5.14 | 135 | 19.35 | 4.71 | 0.28 | |
| Total 6M | 44 | 24.30 | 2.83 | 40 | 20.45 | 4.82 | 84 | 22.46 | 4.33 | p < 0.001 | |
| Wilcoxon | p < 0.001 | p < 0.001 | p < 0.001 | ||||||||
| Variable | COHKAP | Variable | MOHKAP | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| β c | CI95% d | p | β | CI95% | p | ||||||
| Intervention | TE f | Ref | Intervention | TE | Ref | ||||||
| MI e | 3.75 | 1.13 | 6.37 | 0.005 | MI | 3.54 | 1.78 | 5.30 | <0.001 | ||
| Marital Status | No partner | Ref | Marital Status | No partner | Ref | ||||||
| With partner | 1.16 | −1.42 | 3.74 | 0.37 | With partner | 1.06 | −0.94 | 3.06 | 0.29 | ||
| Psychoprophylactic course | No | Ref | Use of dental services | No | Ref | ||||||
| Yes | −3.10 | −7.40 | 1.19 | 0.15 | Yes | 0.92 | −0.77 | 2.61 | 0.28 | ||
| MSE g | 0.52 | 0.26 | 0.78 | <0.001 | |||||||
| p < 0.001; R-squared = 0.46 | p = 0.003; R-squared = 0.22 | ||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramírez-Trujillo, M.Á.; Villanueva-Vilchis, M.C.; Gaitán-Cepeda, L.A.; Aguilar-Díaz, F.C.; Rojas-Russell, M.E.; Fuente-Hernández, J. Impact of a Maternal Motivational Interviewing on Oral Health in the Mother-Child Dyad. Healthcare 2022, 10, 1044. https://doi.org/10.3390/healthcare10061044
Ramírez-Trujillo MÁ, Villanueva-Vilchis MC, Gaitán-Cepeda LA, Aguilar-Díaz FC, Rojas-Russell ME, Fuente-Hernández J. Impact of a Maternal Motivational Interviewing on Oral Health in the Mother-Child Dyad. Healthcare. 2022; 10(6):1044. https://doi.org/10.3390/healthcare10061044
Chicago/Turabian StyleRamírez-Trujillo, M. Á., M. C. Villanueva-Vilchis, L. A. Gaitán-Cepeda, F. C. Aguilar-Díaz, M. E. Rojas-Russell, and J. Fuente-Hernández. 2022. "Impact of a Maternal Motivational Interviewing on Oral Health in the Mother-Child Dyad" Healthcare 10, no. 6: 1044. https://doi.org/10.3390/healthcare10061044
APA StyleRamírez-Trujillo, M. Á., Villanueva-Vilchis, M. C., Gaitán-Cepeda, L. A., Aguilar-Díaz, F. C., Rojas-Russell, M. E., & Fuente-Hernández, J. (2022). Impact of a Maternal Motivational Interviewing on Oral Health in the Mother-Child Dyad. Healthcare, 10(6), 1044. https://doi.org/10.3390/healthcare10061044









