Fear of COVID-19 and Perceived Stress: The Mediating Roles of Neuroticism and Perceived Social Support
Abstract
1. Introduction
2. Materials and Methods
2.1. Measurements
2.1.1. Fear of COVID-19 and Impacts on Quality of Life Scale
2.1.2. Perceived Stress Scale-10 (PSS-10)
2.1.3. Neuroticism Inventory (NI)
2.1.4. Multidimensional Scale of Perceived Social Support (MSPSS)
2.2. Data Cleaning
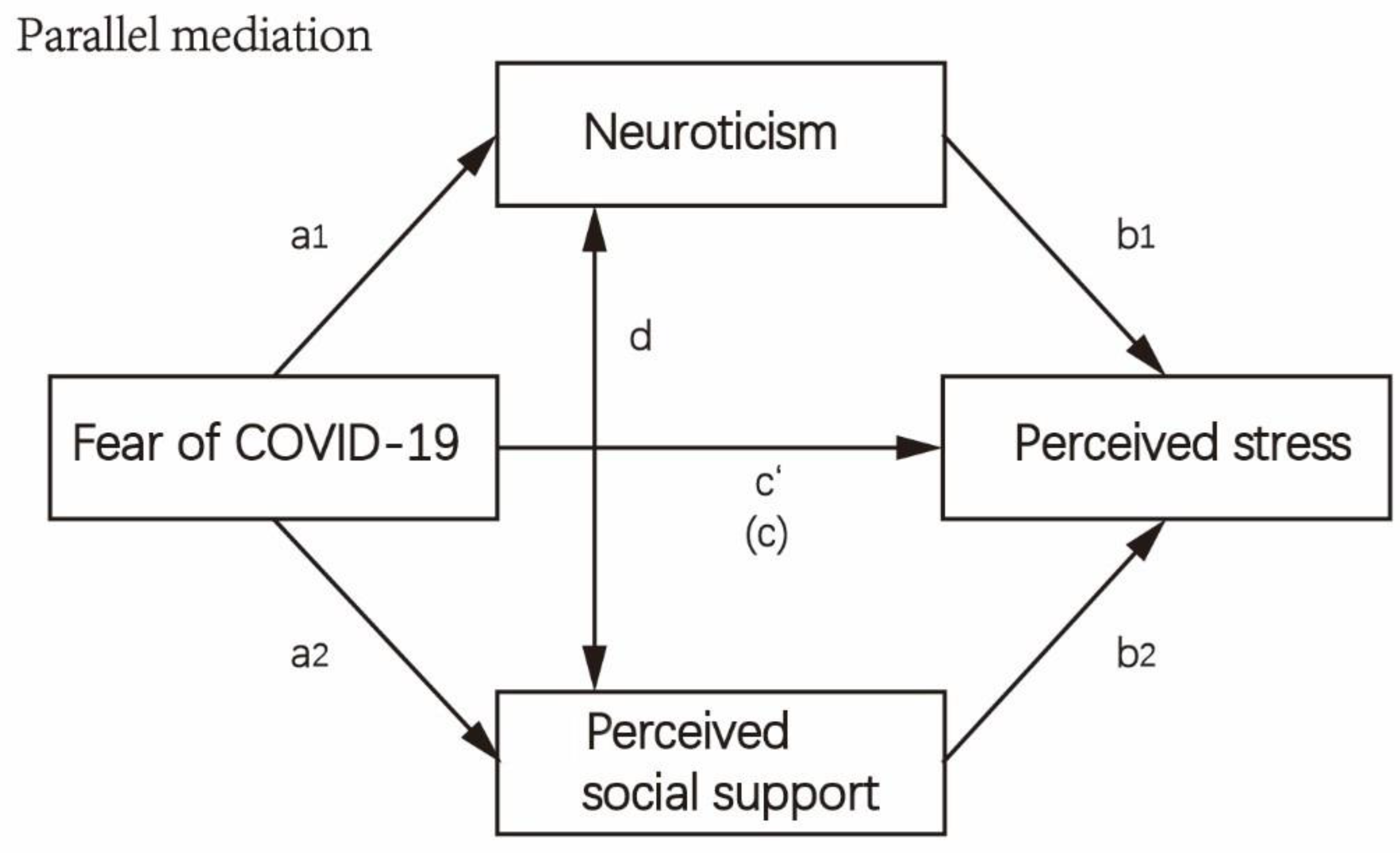
2.3. Data Analysis
3. Results
3.1. Sociodemographic and Psychological Characteristics of Participants
3.2. Psychological Variables and Characteristics of Participants
3.3. Pearson’s Correlation among Psychological Variables and Multiple Regression Analyses
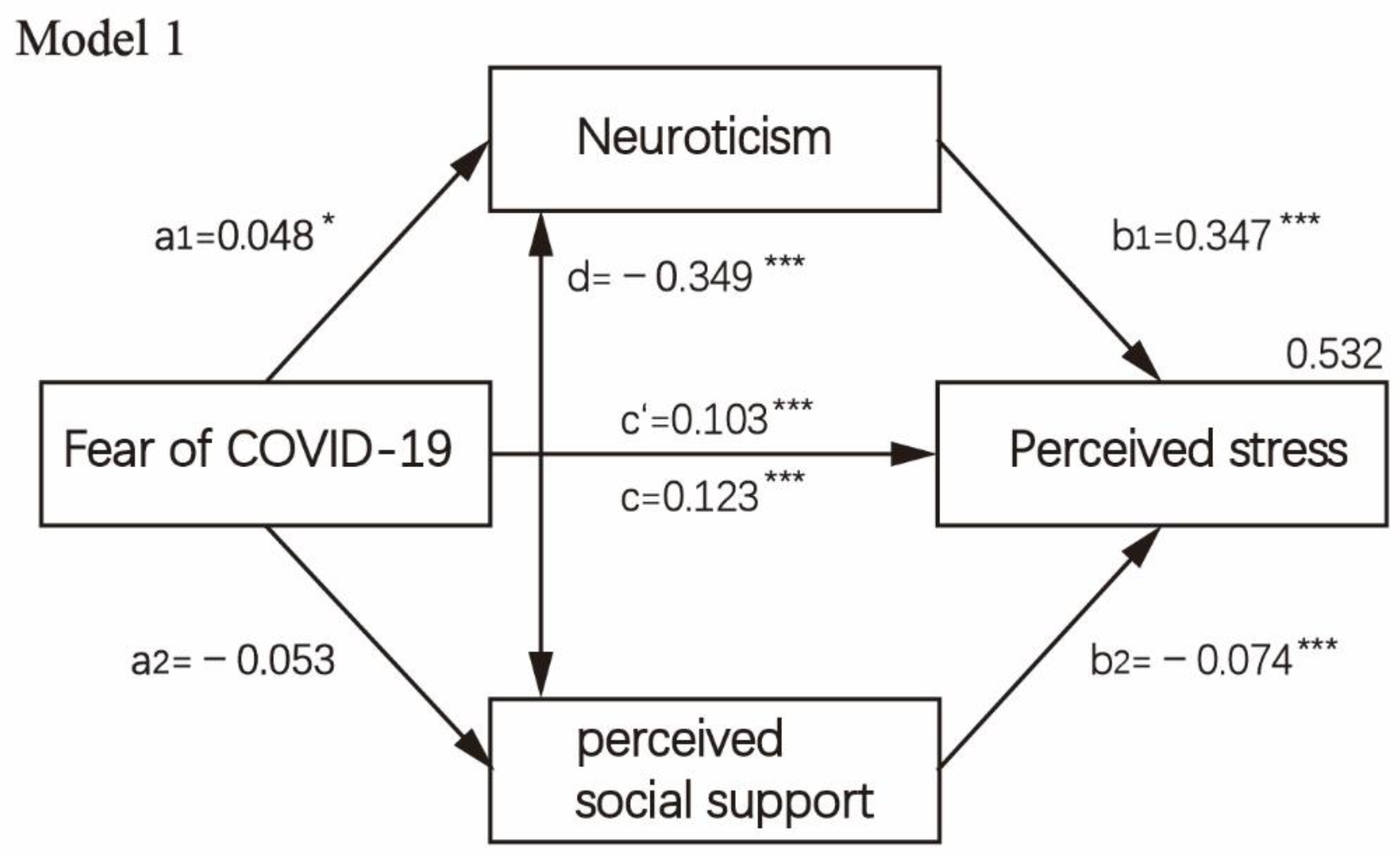
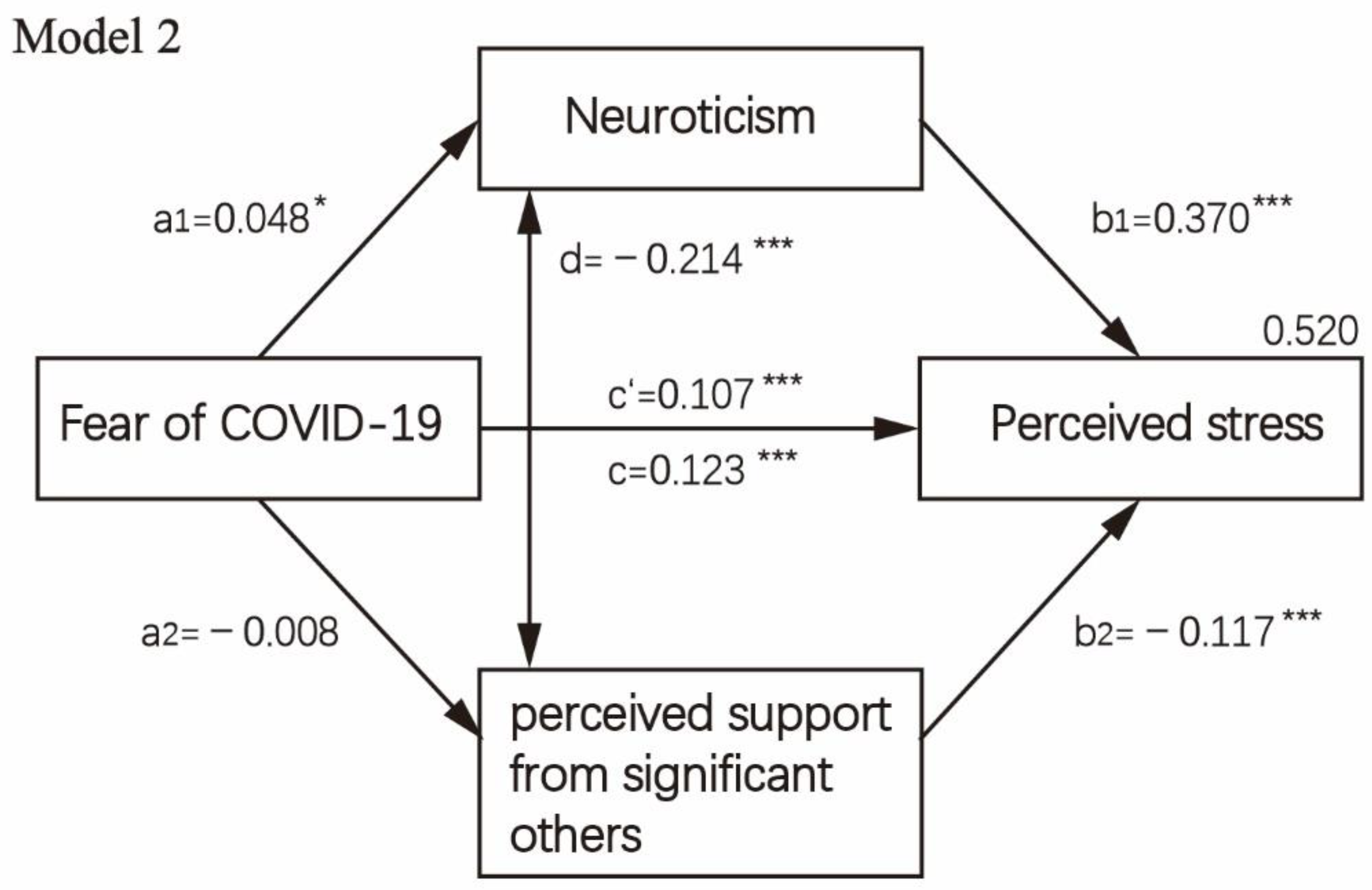
3.4. Mediation Analysis
4. Discussion
4.1. Strengths and Limitations
4.2. Practical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tsamakis, K.; Tsiptsios, D.; Ouranidis, A.; Mueller, C.; Schizas, D.; Terniotis, C.; Nikolakakis, N.; Tyros, G.; Kympouropoulos, S.; Lazaris, A.; et al. COVID-19 and its consequences on mental health (Review). Exp. Med. 2021, 21, 244. [Google Scholar] [CrossRef] [PubMed]
- Nochaiwong, S.; Ruengorn, C.; Thavorn, K.; Hutton, B.; Awiphan, R.; Phosuya, C.; Ruanta, Y.; Wongpakaran, N.; Wongpakaran, T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 10173. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.A.; Jobe, M.C.; Mathis, A.A.; Gibbons, J.A. Incremental validity of coronaphobia: Coronavirus anxiety explains depression, generalized anxiety, and death anxiety. J. Anxiety Disord. 2020, 74, 102268. [Google Scholar] [CrossRef]
- Heiat, M.; Heiat, F.; Halaji, M.; Ranjbar, R.; Tavangar Marvasti, Z.; Yaali-Jahromi, E.; Azizi, M.M.; Morteza Hosseini, S.; Badri, T. Phobia and Fear of COVID-19: Origins, complications and management, a narrative review. Ann. Ig. 2021, 33, 360–370. [Google Scholar] [CrossRef]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. 2020, 14, 779–788. [Google Scholar] [CrossRef]
- Nochaiwong, S.; Ruengorn, C.; Awiphan, R.; Ruanta, Y.; Boonchieng, W.; Nanta, S.; Kowatcharakul, W.; Pumpaisalchai, W.; Kanjanarat, P.; Mongkhon, P.; et al. Mental health circumstances among health care workers and general public under the pandemic situation of COVID-19 (HOME-COVID-19). Medicine 2020, 99, e20751. [Google Scholar] [CrossRef]
- Fernandez, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Pedreira, M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J. Affect. Disord. 2020, 277, 75–84. [Google Scholar] [CrossRef]
- Mertens, G.; Gerritsen, L.; Duijndam, S.; Salemink, E.; Engelhard, I.M. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J. Anxiety Disord. 2020, 74, 102258. [Google Scholar] [CrossRef]
- Xu, J.; Sun, G.; Cao, W.; Fan, W.; Pan, Z.; Yao, Z.; Li, H. Stigma, Discrimination, and Hate Crimes in Chinese-Speaking World amid COVID-19 Pandemic. Asian J. Criminol. 2021, 16, 51–74. [Google Scholar] [CrossRef]
- Scheid, J.L.; Lupien, S.P.; Ford, G.S.; West, S.L. Commentary: Physiological and Psychological Impact of Face Mask Usage during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6655. [Google Scholar] [CrossRef] [PubMed]
- Apisarnthanarak, A.; Apisarnthanarak, P.; Siripraparat, C.; Saengaram, P.; Leeprechanon, N.; Weber, D.J. Impact of anxiety and fear for COVID-19 toward infection control practices among Thai healthcare workers. Infect. Control. Hosp. Epidemiol. 2020, 41, 1093–1094. [Google Scholar] [CrossRef] [PubMed]
- Newby, J.M.; O’Moore, K.; Tang, S.; Christensen, H.; Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 2020, 15, e0236562. [Google Scholar] [CrossRef] [PubMed]
- Wongpakaran, T.; Wongpakaran, N.; Pinyopornpanish, M.; Srisutasanavong, U.; Lueboonthavatchai, P.; Nivataphand, R.; Apisiridej, N.; Petchsuwan, D.; Saisavoey, N.; Wannarit, K.; et al. Baseline characteristics of depressive disorders in Thai outpatients: Findings from the Thai Study of Affective Disorders. Neuropsychiatr. Dis. Treat. 2014, 10, 217–223. [Google Scholar] [CrossRef][Green Version]
- Banjongrewadee, M.; Wongpakaran, N.; Wongpakaran, T.; Pipanmekaporn, T.; Punjasawadwong, Y.; Mueankwan, S. Role of perceived stress in postoperative delirium: An investigation among elderly patients. Aging Ment. Health 2018, 24, 148–154. [Google Scholar] [CrossRef]
- Banjongrewadee, M.; Wongpakaran, N.; Wongpakaran, T.; Pipanmekaporn, T.; Punjasawadwong, Y.; Mueankwan, S. The role of perceived stress and cognitive function on the relationship between neuroticism and depression among the elderly: A structural equation model approach. BMC Psychiatry 2020, 20, 25. [Google Scholar] [CrossRef]
- Candrian, M.; Schwartz, F.; Farabaugh, A.; Perlis, R.H.; Ehlert, U.; Fava, M. Personality disorders and perceived stress in major depressive disorder. Psychiatry Res. 2008, 160, 184–191. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Brostrom, A.; Tsang, H.W.H.; Griffiths, M.D.; Haghayegh, S.; Ohayon, M.M.; Lin, C.Y.; Pakpour, A.H. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: A systematic review and meta-analysis. eClinicalMedicine 2021, 36, 100916. [Google Scholar] [CrossRef]
- Mulugeta, W.; Desalegn, H.; Solomon, S. Impact of the COVID-19 pandemic lockdown on weight status and factors associated with weight gain among adults in Massachusetts. Clin. Obes. 2021, 11, e12453. [Google Scholar] [CrossRef]
- Guerrini Usubini, A.; Cattivelli, R.; Varallo, G.; Castelnuovo, G.; Molinari, E.; Giusti, E.M.; Pietrabissa, G.; Manari, T.; Filosa, M.; Franceschini, C.; et al. The Relationship between Psychological Distress during the Second Wave Lockdown of COVID-19 and Emotional Eating in Italian Young Adults: The Mediating Role of Emotional Dysregulation. J. Pers. Med. 2021, 11, 569. [Google Scholar] [CrossRef]
- Wongpakaran, N.; Wongpakaran, T. The Thai version of the PSS-10: An Investigation of its psychometric properties. Biopsychosoc. Med. 2010, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- El Ansari, W.; Adetunji, H.; Oskrochi, R. Food and mental health: Relationship between food and perceived stress and depressive symptoms among university students in the United Kingdom. Cent. Eur. J. Public Health 2014, 22, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Gallo, L.C.; Roesch, S.C.; Fortmann, A.L.; Carnethon, M.R.; Penedo, F.J.; Perreira, K.; Birnbaum-Weitzman, O.; Wassertheil-Smoller, S.; Castañeda, S.F.; Talavera, G.A. Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the HCHS/SOL Sociocultural Ancillary Study. Psychosom. Med. 2014, 76, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Gan, Y.; Ding, X.; Wu, J.; Duan, H. The relationship between perceived stress and emotional distress during the COVID-19 outbreak: Effects of boredom proneness and coping style. J. Anxiety Disord. 2021, 77, 102328. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Mahmud, S.; Hossain, S.; Muyeed, A.; Islam, M.M.; Mohsin, M. The global prevalence of depression, anxiety, stress, and, insomnia and its changes among health professionals during COVID-19 pandemic: A rapid systematic review and meta-analysis. Heliyon 2021, 7, e07393. [Google Scholar] [CrossRef] [PubMed]
- Kuo, F.L.; Yang, P.H.; Hsu, H.T.; Su, C.Y.; Chen, C.H.; Yeh, I.J.; Wu, Y.H.; Chen, L.C. Survey on perceived work stress and its influencing factors among hospital staff during the COVID-19 pandemic in Taiwan. Kaohsiung J. Med. Sci. 2020, 36, 944–952. [Google Scholar] [CrossRef]
- Wakode, N.; Wakode, S.; Santoshi, J. Perceived stress and generalized anxiety in the Indian population due to lockdown during the COVID-19 pandemic: A cross-sectional study. F1000Research 2020, 9, 1233. [Google Scholar] [CrossRef]
- Maraqa, B.; Nazzal, Z.; Zink, T. Palestinian Health Care Workers’ Stress and Stressors During COVID-19 Pandemic: A Cross-Sectional Study. J. Prim. Care Community Health 2020, 11, 2150132720955026. [Google Scholar] [CrossRef]
- Leng, M.; Wei, L.; Shi, X.; Cao, G.; Wei, Y.; Xu, H.; Zhang, X.; Zhang, W.; Xing, S.; Wei, H. Mental distress and influencing factors in nurses caring for patients with COVID-19. Nurs. Crit. Care 2021, 26, 94–101. [Google Scholar] [CrossRef]
- Siddique, R.F.; Ahmed, O.; Hossain, K.N. Relationship between the fear of COVID-19 disease and sleep quality: The mediating role of stress. Heliyon 2021, 7, e07033. [Google Scholar] [CrossRef] [PubMed]
- Dymecka, J.; Gerymski, R.; Machnik-Czerwik, A. How does stress affect life satisfaction during the COVID-19 pandemic? Moderated mediation analysis of sense of coherence and fear of coronavirus. Psychol. Health Med. 2021, 27, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Lathabhavan, R.; Vispute, S. Examining the Mediating Effects of Stress on Fear of COVID-19 and Well-being Using Structural Equation Modeling. Int. J. Ment. Health Addict. 2021, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dymecka, J.; Gerymski, R.; Machnik-Czerwik, A. Fear of COVID-19 as a buffer in the relationship between perceived stress and life satisfaction in the Polish population at the beginning of the global pandemic. Health Psychol. Rep. 2021, 9, 149–159. [Google Scholar] [CrossRef]
- Lahey, B.B. Public health significance of neuroticism. Am. Psychol. 2009, 64, 241–256. [Google Scholar] [CrossRef]
- Ormel, J.; Jeronimus, B.F.; Kotov, R.; Riese, H.; Bos, E.H.; Hankin, B.; Rosmalen, J.G.M.; Oldehinkel, A.J. Neuroticism and common mental disorders: Meaning and utility of a complex relationship. Clin. Psychol. Rev. 2013, 33, 686–697. [Google Scholar] [CrossRef]
- Paulus, D.J.; Vanwoerden, S.; Norton, P.J.; Sharp, C. From neuroticism to anxiety: Examining unique contributions of three transdiagnostic vulnerability factors. Pers. Individ. Dif. 2016, 94, 38–43. [Google Scholar] [CrossRef]
- Lippold, J.V.; Laske, J.I.; Hogeterp, S.A.; Duke, E.; Grunhage, T.; Reuter, M. The Role of Personality, Political Attitudes and Socio-Demographic Characteristics in Explaining Individual Differences in Fear of Coronavirus: A Comparison over Time and Across Countries. Front. Psychol. 2020, 11, 552305. [Google Scholar] [CrossRef]
- Dlugosz, P.; Kryvachuk, L. Neurotic Generation of COVID-19 in Eastern Europe. Front. Psychiatry 2021, 12, 654590. [Google Scholar] [CrossRef]
- Pradhan, M.; Chettri, A.; Maheshwari, S. Fear of death in the shadow of COVID-19: The mediating role of perceived stress in the relationship between neuroticism and death anxiety. Death Stud. 2022, 46, 1106–1110. [Google Scholar] [CrossRef]
- Kroencke, L.; Geukes, K.; Utesch, T.; Kuper, N.; Back, M.D. Neuroticism and emotional risk during the COVID-19 pandemic. J. Res. Pers. 2020, 89, 104038. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Lithopoulos, A.; Zhang, C.-Q.; Garcia-Barrera, M.A.; Rhodes, R.E. Personality and perceived stress during COVID-19 pandemic: Testing the mediating role of perceived threat and efficacy. Pers. Individ. Dif. 2021, 168, 110351. [Google Scholar] [CrossRef] [PubMed]
- Engert, V.; Blasberg, J.U.; Kohne, S.; Strauss, B.; Rosendahl, J. Resilience and personality as predictors of the biological stress load during the first wave of the COVID-19 pandemic in Germany. Transl. Psychiatry 2021, 11, 443. [Google Scholar] [CrossRef] [PubMed]
- Gori, A.; Topino, E.; Palazzeschi, L.; Di Fabio, A. Which personality traits can mitigate the impact of the pandemic? Assessment of the relationship between personality traits and traumatic events in the COVID-19 pandemic as mediated by defense mechanisms. PLoS ONE 2021, 16, e0251984. [Google Scholar] [CrossRef]
- Taylor, S.E. Social support: A review. In The Oxford Handbook of Health Psychology; Friedman, H.S., Ed.; Oxford University Press Inc.: New York, NY, USA, 2011; pp. 189–214. [Google Scholar]
- Uchino, B.N. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. J. Behav. Med. 2006, 29, 377–387. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, Y.; Zhang, Y.; Li, Z.; Zhou, T. The Effect of Fear of the COVID-19 on Depression Among Chinese Outbound Students Studying Online in China Amid the COVID-19 Pandemic Period: The Role of Resilience and Social Support. Front. Psychol. 2021, 12, 750011. [Google Scholar] [CrossRef]
- Yenen, E.T.; Carkit, E. Fear of COVID-19 and general self-efficacy among Turkish teachers: Mediating role of perceived social support. Curr. Psychol. 2021, 1–9. [Google Scholar] [CrossRef]
- Alnazly, E.; Khraisat, O.M.; Al-Bashaireh, A.M.; Bryant, C.L. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One 2021, 16, e0247679. [Google Scholar] [CrossRef]
- Muyor-Rodriguez, J.; Caravaca-Sanchez, F.; Fernandez-Prados, J.S. COVID-19 Fear, Resilience, Social Support, Anxiety, and Suicide among College Students in Spain. Int. J. Environ. Res. Public Health 2021, 18, 8156. [Google Scholar] [CrossRef]
- Alan, S.; Vurgec, B.A.; Cevik, A.; Gozuyesil, E.; Surucu, S.G. The Effects of COVID-19 Pandemic on Pregnant Women: Perceived Stress, Social Support and Sleep Quality. Yonago Acta Med. 2020, 63, 360–367. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- Wongpakaran, T. Fear of COVID-19 and impact on QoL Scale. Available online: http://www.wongpakaran.com/index.php?lay=show&ac=article&Id=2147599077 (accessed on 3 April 2022).
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J Health Soc Behav 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The multidimensional scale of perceived social support. J Pers Assess 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Mongkhon, P.; Ruengorn, C.; Awiphan, R.; Thavorn, K.; Hutton, B.; Wongpakaran, N.; Wongpakaran, T.; Nochaiwong, S. Exposure to COVID-19-Related Information and its Association With Mental Health Problems in Thailand: Nationwide, Cross-sectional Survey Study. J. Med. Internet Res. 2021, 23, e25363. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cut off criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equat. Mod. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Masjoudi, M.; Aslani, A.; Seifi, M.; Khazaeian, S.; Fathnezhad-Kazemi, A. Association between perceived stress, fear and anxiety of COVID 19 with self-care in pregnant women: A cross-sectional study. Psychol. Health Med. 2022, 27, 289–300. [Google Scholar] [CrossRef]
- Yang, C.; Chen, A.; Chen, Y. College students’ stress and health in the COVID-19 pandemic: The role of academic workload, separation from school, and fears of contagion. PLoS ONE 2021, 16, e0246676. [Google Scholar] [CrossRef]
- Peker, A.; Cengiz, S. Covid-19 fear, happiness and stress in adults: The mediating role of psychological resilience and coping with stress. Int. J. Psychiatry Clin. Pr. 2021, 1–9. [Google Scholar] [CrossRef]
- Rodriguez-Hidalgo, A.J.; Pantaleon, Y.; Dios, I.; Falla, D. Fear of COVID-19, Stress, and Anxiety in University Undergraduate Students: A Predictive Model for Depression. Front. Psychol. 2020, 11, 591797. [Google Scholar] [CrossRef]
- Montag, C.; Sindermann, C.; Rozgonjuk, D.; Yang, S.; Elhai, J.D.; Yang, H. Investigating Links Between Fear of COVID-19, Neuroticism, Social Networks Use Disorder, and Smartphone Use Disorder Tendencies. Front. Psychol. 2021, 12, 682837. [Google Scholar] [CrossRef] [PubMed]
- Caci, B.; Miceli, S.; Scrima, F.; Cardaci, M. Neuroticism and Fear of COVID-19. The Interplay Between Boredom, Fantasy Engagement, and Perceived Control Over Time. Front. Psychol. 2020, 11, 574393. [Google Scholar] [CrossRef] [PubMed]
- Schaller, M.; Norenzayan, A.; Heine, S.J.; Yamagishi, T.; Kameda, T. Evolution, Culture, and the Human Mind; Psychology Press: New York, NY, USA, 2009. [Google Scholar]
- Barrett, L.F.; Lewis, M.; Haviland-Jones, M.J. Handbook of Emotions, Fourth edition ed.; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, K.M.; Harris, C.; Drawve, G. Fear of COVID-19 and the mental health consequences in America. Psychol. Trauma 2020, 12, S17–S21. [Google Scholar] [CrossRef]
- Labrague, L.J.; de Los Santos, J.A.A. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J. Nurs. Manag. 2021, 29, 395–403. [Google Scholar] [CrossRef]
- Natsu Sasaki, R.K. Fear, Worry and Workplace Harassment Related to the COVID-19 Epidemic Among Employees in Japan Prevalence and Impact on Mental and Physical Health. Available online: https://ssrn.com/abstract=3569887 (accessed on 3 April 2022).
- Hossain, M.A.; Jahid, M.I.K.; Hossain, K.M.A.; Walton, L.M.; Uddin, Z.; Haque, M.O.; Kabir, M.F.; Arafat, S.M.Y.; Sakel, M.; Faruqui, R.; et al. Knowledge, attitudes, and fear of COVID-19 during the Rapid Rise Period in Bangladesh. PLoS ONE 2020, 15, e0239646. [Google Scholar] [CrossRef]
- Olsson, A.; Phelps, E.A. Social learning of fear. Nat. Neurosci. 2007, 10, 1095–1102. [Google Scholar] [CrossRef]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef]
- Maeng, L.Y.; Milad, M.R. Sex differences in anxiety disorders: Interactions between fear, stress, and gonadal hormones. Horm. Behav. 2015, 76, 106–117. [Google Scholar] [CrossRef]
- Ruengorn, C.; Awiphan, R.; Wongpakaran, N.; Wongpakaran, T.; Nochaiwong, S.; Health, O.; Mental Health Care Evaluation Survey Research, G. Association of job loss, income loss, and financial burden with adverse mental health outcomes during coronavirus disease 2019 pandemic in Thailand: A nationwide cross-sectional study. Depress. Anxiety 2021, 38, 648–660. [Google Scholar] [CrossRef]
- Turska, E.; Stepien-Lampa, N. Well-being of Polish university students after the first year of the coronavirus pandemic: The role of core self-evaluations, social support and fear of COVID-19. PLoS ONE 2021, 16, e0259296. [Google Scholar] [CrossRef] [PubMed]
- Özer, Ö.; Özkan, O.; Budak, F.; Özmen, S. Does social support affect perceived stress? A research during the COVID-19 pandemic in Turkey. J. Hum. Behav. Soc. Environ. 2020, 31, 134–144. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, e923549. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Wei, Y. Social support as a moderator of the relationship between anxiety and depression: An empirical study with adult survivors of Wenchuan earthquake. PLoS ONE 2013, 8, e79045. [Google Scholar] [CrossRef]
- Chen, W. Academic Stress, Depression, and Social Support: A Comparison of Chinese Students in International Baccalaureate Programs and Key Schools; University of South Florida: Tampa, FL, USA, 2018. [Google Scholar]
- Cheng, C. Role of perceived social support on depression in Chinese adolescents: A prospective study examining the buffering model. J. Appl. Soc. Psychol. 1997, 27, 800–820. [Google Scholar] [CrossRef]
- Hornstein, E.A.; Eisenberger, N.I. Unpacking the buffering effect of social support figures: Social support attenuates fear acquisition. PLoS ONE 2017, 12, e0175891. [Google Scholar] [CrossRef]
- Jacobs, S.; Holtzer, R. Predicting change in perceived social support in late life: The role of personality and gender. Aging Ment. Health 2021, 25, 107–117. [Google Scholar] [CrossRef]
- Yu, Y.; Zhao, Y.; Li, D.; Zhang, J.; Li, J. The Relationship Between Big Five Personality and Social Well-Being of Chinese Residents: The Mediating Effect of Social Support. Front. Psychol. 2020, 11, 613659. [Google Scholar] [CrossRef]
- Eysenck, H.J.; Eysenck, M.W. Personality and Individual Differences; Plenum: New York, NY, USA, 1987. [Google Scholar]
- Swickert, R.; Owens, T. The interaction between neuroticism and gender influences the perceived availability of social support. Pers. Individ. Dif. 2010, 48, 385–390. [Google Scholar] [CrossRef]
- Bentall, R.P.; Lloyd, A.; Bennett, K.; McKay, R.; Mason, L.; Murphy, J.; McBride, O.; Hartman, T.K.; Gibson-Miller, J.; Levita, L.; et al. Pandemic buying: Testing a psychological model of over-purchasing and panic buying using data from the United Kingdom and the Republic of Ireland during the early phase of the COVID-19 pandemic. PLoS ONE 2021, 16, e0246339. [Google Scholar] [CrossRef]
- Perez-Mengual, N.; Aragones-Barbera, I.; Moret-Tatay, C.; Moliner-Albero, A.R. The Relationship of Fear of Death Between Neuroticism and Anxiety During the COVID-19 Pandemic. Front. Psychiatry 2021, 12, 648498. [Google Scholar] [CrossRef] [PubMed]
- Canli, T. Toward a neurogenetic theory of neuroticism. Ann. N. Y. Acad. Sci. 2008, 1129, 153–174. [Google Scholar] [CrossRef] [PubMed]
- Bellingtier, J.A.; Mund, M.; Wrzus, C. The role of extraversion and neuroticism for experiencing stress during the third wave of the COVID-19 pandemic. Curr. Psychol. 2021, 47, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hankin, B.L.; Stone, L.; Wright, P.A. Corumination, interpersonal stress generation, and internalizing symptoms: Accumulating effects and transactional influences in a multiwave study of adolescents. Dev. Psychopathol. 2010, 22, 217–235. [Google Scholar] [CrossRef] [PubMed]
- Middeldorp, C.M.; Cath, D.C.; Beem, A.L.; Willemsen, G.; Boomsma, D.I. Life events, anxious depression and personality: A prospective and genetic study. Psychol. Med. 2008, 38, 1557–1565. [Google Scholar] [CrossRef] [PubMed]
- Kercher, A.J.; Rapee, R.M.; Schniering, C.A. Neuroticism, life events and negative thoughts in the development of depression in adolescent girls. J. Abnorm. Child Psychol. 2009, 37, 903–915. [Google Scholar] [CrossRef]
- Cross, R.; Parker, A.; Sasson, L. Networks in the Knowledge Economy; Oxford University Press: Oxford, UK, 2003. [Google Scholar]
- Nkire, N.; Mrklas, K.; Hrabok, M.; Gusnowski, A.; Vuong, W.; Surood, S.; Abba-Aji, A.; Urichuk, L.; Cao, B.; Greenshaw, A.J.; et al. COVID-19 Pandemic: Demographic Predictors of Self-Isolation or Self-Quarantine and Impact of Isolation and Quarantine on Perceived Stress, Anxiety, and Depression. Front. Psychiatry 2021, 12, 553468. [Google Scholar] [CrossRef]
- Ruksee, N.; Donjdee, K.; Songsiri, N.; Seesaws, W.; Janjaroen, S.; Yupu, A. A study of the stress, anxiety and family relationships among Thai people after the COVID-19 pandemic in the early stages. Qual. Life Law J. 2021, 17, 94–108. [Google Scholar]
- Panteli, M.; Vaiouli, P.; Leonidou, C.; Panayiotou, G. Perceived stress of Cypriot college students during COVID-19: The predictive role of social skills and social support. Eur. J. Psychol. Open 2021, 80, 31–39. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef]
- Hornstein, E.A.; Fanselow, M.S.; Eisenberger, N.I. A Safe Haven: Investigating Social-Support Figures as Prepared Safety Stimuli. Psychol. Sci. 2016, 27, 1051–1060. [Google Scholar] [CrossRef] [PubMed]
- Hostinar, C.E.; Gunnar, M.R. Social Support Can Buffer against Stress and Shape Brain Activity. AJOB Neurosci. 2015, 6, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zilioli, S.; Jiang, Y.; Wang, X.; Lin, D. Perceived social support and children’s physiological responses to stress: An examination of the stress-buffering hypothesis. Psychosom. Med. 2021, 83, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Rogowska, A.M.; Kusnierz, C.; Bokszczanin, A. Examining Anxiety, Life Satisfaction, General Health, Stress and Coping Styles During COVID-19 Pandemic in Polish Sample of University Students. Psychol. Res. Behav. Manag. 2020, 13, 797–811. [Google Scholar] [CrossRef]
- Duan, H.; Yan, L.; Ding, X.; Gan, Y.; Kohn, N.; Wu, J. Impact of the COVID-19 pandemic on mental health in the general Chinese population: Changes, predictors and psychosocial correlates. Psychiatry Res. 2020, 293, 113396. [Google Scholar] [CrossRef]
- Dechsupa, S.; Assawakosri, S.; Phakham, S.; Honsawek, S. Positive impact of lockdown on COVID-19 outbreak in Thailand. Travel Med. Infect. Dis. 2020, 36, 101802. [Google Scholar] [CrossRef]
- World Health Organization (Thailand). COVID-19-WHO Thailand Situation Reports, WHO Thailand Situation Report-71. Available online: https://cdn.w.who.int/media/docs/default-source/searo/thailand/2020-05-04-tha-sitrep-71-COVID19-final.pdf?sfvrsn=5766517c_2 (accessed on 3 April 2022).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://serotracker.com/en/unity (accessed on 3 April 2022).


| Variables | Mean (SD) or n (%) |
|---|---|
| Age (Years), 18–59 Mean (SD) | 28.52 (9.88) |
| Sex, n (%) | |
| Male | 1025 (31.1) |
| Female | 2274 (68.9) |
| Education level, n (%) | |
| Bachelor’s degree or higher | 1670 (50.6) |
| Below bachelor’s degree | 1629 (49.4) |
| Marital status, n (%) | |
| Single | 2715 (82.3) |
| Non-single | 584 (17.7) |
| Religion, n (%) | |
| Buddhist | 2864 (86.8) |
| Non-Buddhist | 435 (13.2) |
| Occupation, n (%) | |
| College student | 1313 (39.8) |
| Self-employed/private-enterprise employee | 776 (23.5) |
| Farmer/laborer freelance/others | 467 (14.1) |
| Government/state-enterprise employee | 430 (13.1) |
| Unemployed/retired | 313 (9.5) |
| Region of residence, n (%) | |
| Capital and vicinity | 1153 (35.0) |
| Northern | 1083 (32.8) |
| Central | 396 (12.1) |
| Southern | 224 (6.8) |
| Northeastern | 222 (6.7) |
| Eastern | 143 (4.3) |
| Western | 78 (2.3) |
| Living status, n (%) | |
| Live with family | 2599 (78.8) |
| Live alone | 474 (14.3) |
| Live with others | 226 (6.9) |
| Income (Thai Baht), n (%) | |
| ≤10,000 | 1593 (48.3) |
| >10,000 | 1706 (51.7) |
| Health insurance, n (%) | |
| Non-Universal Coverage Scheme | 2217 (67.2) |
| Universal Coverage Scheme | 1082 (32.8) |
| History of chronic non-communicable disease, n (%) | |
| No | 2847 (86.3) |
| Yes | 452 (13.7) |
| Work from home, n (%) | |
| No | 733 (22.2) |
| Yes | 2566 (78.8) |
| Quarantine status, n (%) | |
| Never | 1440 (43.6) |
| Was quarantined | 1329 (40.3) |
| During quarantine | 530 (16.1) |
| Scores of psychological measures, Mean (SD) | |
| Perceived stress (range 0–36) | 17.61 (5.76) |
| Fear of COVD-19 (range 0–36) | 20.84 (7.07) |
| Neuroticism (range 15–60) | 36.27 (9.57) |
| Perceived social support—Total score (range 12–84) | 59.01 (13.48) |
| -Perceived social support from significant others (range 4–28) | 19.09 (5.74) |
| -Perceived social support from family members (range 4–28) | 20.07 (5.60) |
| -Perceived social support from friends (range 4–28) | 19.85 (5.20) |
| Variables | n | Perceived Stress | Fear of COVID-19 | Neuroticism | Perceived Social Support | ||||
|---|---|---|---|---|---|---|---|---|---|
| Age | Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value | |
| <21 | 644 (19.6) | 19.10 ± 5.64 | <0.001 | 21.33 ± 6.82 | 0.017 | 39.47 ± 8.57 | <0.001 | 58.66 ± 13.41 | 0.074 |
| 21–30 | 1574 (47.7) | 18.31 ± 5.61 | 20.44 ± 6.95 | 37.84 ± 9.30 | 59.50 ± 13.44 | ||||
| 31–40 | 640 (19.4) | 16.61 ± 5.25 | 21.32 ± 7.22 | 32.89 ± 9.27 | 57.79 ± 13.95 | ||||
| 41–50 | 288 (8.7) | 15.27 ± 5.70 | 21.12 ± 7.61 | 32.02 ± 9.09 | 59.37 ± 13.22 | ||||
| 51–60 | 153 (4.6) | 12.77 ± 5.40 | 20.41 ± 7.58 | 28.86 ± 7.68 | 59.86 ± 12.30 | ||||
| Sex | |||||||||
| Male | 1025 (31.1) | 15.84 ± 5.55 | <0.001 | 19.44 ± 7.12 | <0.001 | 33.27 ± 9.28 | <0.001 | 58.36 ± 13.17 | 0.066 |
| Female | 2274 (68.9) | 18.41 ± 5.68 | 21.47 ± 6.96 | 37.63 ± 9.39 | 59.30 ± 13.60 | ||||
| Education level | |||||||||
| Bachelor’s degree or higher | 1670 (50.6) | 18.27 ± 5.66 | 21.27 ± 6.79 | 37.43 ± 9.50 | 58.20 ± 13.49 | ||||
| Below bachelor’s degree | 1629 (49.4) | 16.94 ± 5.78 | <0.001 | 20.40 ± 7.33 | <0.001 | 35.09 ± 9.50 | <0.001 | 59.84 ± 13.42 | <0.001 |
| Marital status | |||||||||
| Single | 2715 (82.3) | 17.99 ± 5.72 | <0.001 | 20.56 ± 6.98 | <0.001 | 37.19 ± 9.40 | <0.001 | 59.03 ± 13.32 | 0.856 |
| Non-single | 584 (17.7) | 15.88 ± 5.64 | 22.16 ± 7.37 | 32.02 ± 9.19 | 58.92 ± 14.19 | ||||
| Religion | |||||||||
| Buddhist | 2864 (86.8) | 17.35 ± 5.69 | <0.001 | 21.05 ± 6.97 | <0.001 | 35.83 ± 9.48 | <0.001 | 59.66 ± 13.13 | <0.001 |
| Non-Buddhist | 435 (13.2) | 19.38 ± 5.89 | 19.49 ± 7.62 | 39.18 ± 9.64 | 54.73 ± 14.89 | ||||
| Occupation | |||||||||
| College student | 1313 (39.8) | 18.40 ± 5.73 | <0.001 | 20.55 ± 6.70 | 0.054 | 38.51 ± 8.89 | <0.001 | 59.60 ± 12.96 | 0.040 |
| Other occupations | 1986 (60.2) | 17.09 ± 5.72 | 21.03 ± 7.31 | 34.79 ± 9.72 | 58.62 ± 13.80 | ||||
| Region of residence | |||||||||
| Non-capital city and its vicinity | 2146 (65.0) | 17.37 ± 5.41 | 0.001 | 21.44 ± 7.09 | <0.001 | 35.57 ± 9.43 | <0.001 | 59.21 ± 13.25 | 0.238 |
| Capital city and its vicinity | 1153 (35.0) | 18.07 ± 6.33 | 19.72 ± 6.91 | 37.57 ± 9.71 | 58.63 ± 13.88 | ||||
| Residence | |||||||||
| Not residing with family | 700 (21.2) | 17.68 ± 5.96 | 0.736 | 20.12 ± 7.29 | 0.002 | 36.52 ± 9.43 | 0.447 | 58.13 ± 13.34 | 0.052 |
| Residing with family | 2599 (78.8) | 17.60 ± 5.70 | 21.04 ± 7.00 | 36.21 ± 9.61 | 59.24 ± 13.51 | ||||
| Income (THB) | |||||||||
| ≤10,000 | 1593 (48.3) | 18.53 ± 5.67 | <0.001 | 21.34 ± 6.85 | <0.001 | 38.30 ± 9.28 | <0.001 | 58.67 ± 13.42 | 0.162 |
| >10,000 | 1706 (51.7) | 16.76 ± 5.71 | 20.37 ± 7.25 | 34.37 ± 9.45 | 59.33 ± 13.52 | ||||
| Health insurance | |||||||||
| Non-Universal Coverage Scheme | 2217 (67.2) | 17.36 ± 5.79 | <0.001 | 20.73 ± 7.19 | 0.206 | 35.83 ± 9.61 | <0.001 | 59.49 ± 13.56 | 0.003 |
| Universal Coverage Scheme | 1082 (32.8) | 18.14 ± 5.67 | 21.06 ± 6.83 | 37.17 ± 9.43 | 58.02 ± 13.25 | ||||
| History of chronic noncommunicable disease | |||||||||
| No | 2847 (86.3) | 17.54 ± 5.69 | 0.056 | 20.72 ± 7.07 | 0.013 | 36.21 ± 9.44 | 0.337 | 59.50 ± 13.35 | <0.001 |
| Yes | 452 (13.7) | 18.10 ± 6.15 | 21.61 ± 7.04 | 36.67 ± 10.38 | 55.90 ± 13.88 | ||||
| Work from home | |||||||||
| No | 733 (22.2) | 17.37 ± 5.37 | 0.199 | 21.26 ± 7.26 | 0.067 | 34.93 ± 9.38 | <0.001 | 56.26 ± 13.29 | <0.001 |
| Yes | 2566 (78.8) | 17.68 ± 5.87 | 20.72 ± 7.02 | 36.65 ± 9.59 | 59.79 ± 13.43 | ||||
| Quarantine status | |||||||||
| Never | 1440 (43.6) | 16.61 ± 5.78 | <0.001 | 20.34 ± 7.50 | 0.002 | 34.76 ± 9.65 | <0.001 | 59.19 ± 13.47 | 0.720 |
| Was quarantined | 1329 (40.3) | 18.18 ± 5.37 | 21.28 ± 6.53 | 36.74 ± 9.27 | 58.96 ± 13.01 | ||||
| During quarantine | 530 (16.1) | 18.91 ± 6.19 | 21.09 ± 7.11 | 39.20 ± 9.29 | 58.65 ± 14.60 | ||||
| VARIABLE | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Fear of COVD-19 | 1 | ||||||
| 2. Perceived stress | 0.176 *** | 1 | |||||
| 3. Neuroticism | 0.050 *** | 0.685 *** | 1 | ||||
| 4. Perceived social support-Total | −0.037 ** | −0.381 *** | −0.330 *** | 1 | |||
| 5. Perceived social support from significant others | 0.007 | −0.259 *** | −0.216 *** | 0.820 *** | 1 | ||
| 6. Perceived social support from family members | −0.024 | −0.385 *** | −0.329 *** | 0.815 *** | 0.483 *** | 1 | |
| 7. Perceived social support from friends | −0.076 *** | −0.285 *** | −0.262 *** | 0.807 *** | 0.498 *** | 0.500 *** | 1 |
| Path | Coeff. | 95% LL-CI | 95% UL-CI | SE | p-Value |
|---|---|---|---|---|---|
| Model 1 | |||||
| Total effect (c) | 0.123 | 0.095 | 0.152 | 0.014 | <0.01 |
| Direct effect (c’) | 0.103 | 0.083 | 0.123 | 0.010 | <0.01 |
| Fear of COVID—Neuroticism (a1) | 0.048 | 0.01 | 0.095 | 0.024 | 0.047 |
| Fear of COVID—Total perceived social support (a2) | −0.053 | −0.123 | 0.017 | 0.036 | 0.140 |
| Neuroticism—Perceived stress (b1) | 0.347 | 0.330 | 0.363 | 0.08 | <0.01 |
| Total perceived social support—Perceived stress (b2) | −0.074 | −0.085 | −0.063 | 0.05 | <0.01 |
| Neuroticism—Total perceived social support | −0.349 | −0.382 | −0.316 | 0.017 | <0.01 |
| Total indirect effect | 0.020 | 0.02 | 0.039 | 0.010 | 0.032 |
| Fear of COVID—Neuroticism—Perceived stress | 0.018 | 0.00 | 0.036 | 0.09 | 0.047 |
| Fear of COVID—Perceived social support—Perceived stress | 0.08 | −0.03 | 0.019 | 0.06 | 0.141 |
| Model 2 | |||||
| Total effect (c) | 0.123 | 0.095 | 0.152 | 0.014 | <0.01 |
| Direct effect (c’) | 0.107 | 0.086 | 0.127 | 0.010 | <0.01 |
| Fear of COVID—Neuroticism (a1) | 0.048 | 0.01 | 0.095 | 0.024 | 0.047 |
| Fear of COVID—Perceived social support from significant others (a2) | 0.08 | −0.021 | 0.036 | 0.015 | 0.60 |
| Neuroticism—Perceived stress (b1) | 0.370 | 0.353 | 0.386 | 0.08 | <0.01 |
| Perceived social support from significant others—Perceived stress (b2) | −0.117 | −0.142 | −0.092 | 0.013 | <0.01 |
| Neuroticism—Perceived social support from significant others | −0.214 | −0.246 | −0.181 | 0.017 | <0.01 |
| Total indirect effect | 0.017 | −0.02 | 0.035 | 0.09 | 0.074 |
| Fear of COVID—Neuroticism—Perceived stress | 0.018 | 0.00 | 0.036 | 0.09 | 0.047 |
| Fear of COVID—Perceived social support from significant others—Perceived stress | −0.02 | −0.09 | 0.05 | 0.04 | 0.599 |
| Model 3 | |||||
| Total effect (c) | 0.123 | 0.095 | 0.152 | 0.014 | <0.01 |
| Direct effect (c’) | 0.104 | 0.084 | 0.124 | 0.010 | <0.01 |
| Fear of COVID—Neuroticism (a1) | 0.048 | 0.01 | 0.095 | 0.024 | 0.047 |
| Fear of COVID—Perceived social support from family members (a2) | −0.014 | −0.043 | 0.015 | 0.015 | 0.348 |
| Neuroticism—Perceived stress (b1) | 0.351 | 0.334 | 0.368 | 0.08 | <0.01 |
| Perceived social support from family members—Perceived stress (b2) | −0.176 | −0.203 | −0.150 | 0.014 | <0.01 |
| Neuroticism—Perceived social support from family members | −0.317 | −0.350 | −0.284 | 0.017 | <0.01 |
| Total indirect effect | 0.019 | 0.01 | 0.038 | 0.09 | 0.043 |
| Fear of COVID—Neuroticism—Perceived stress | 0.018 | 0.00 | 0.036 | 0.09 | 0.047 |
| Fear of COVID—Perceived social support from family members—Perceived stress | 0.05 | −0.05 | 0.015 | 0.05 | 0.348 |
| Model 4 * | |||||
| Total effect (c) | 0.123 | 0.095 | 0.152 | 0.014 | <0.01 |
| Direct effect (c’) | 0.10 | 0.080 | 0.121 | 0.010 | <0.01 |
| Fear of COVID—Neuroticism (a1) | 0.048 | 0.01 | 0.095 | 0.024 | 0.047 |
| Fear of COVID—Perceived social support from friends (a2) | −0.047 | −0.074 | −0.019 | 0.014 | 0.01 |
| Neuroticism—Perceived stress (b1) | 0.361 | 0.344 | 0.378 | 0.08 | <0.01 |
| Perceived social support from friends—Perceived stress (b2) | −0.131 | −0.160 | −0.102 | 0.015 | <0.01 |
| Neuroticism—Perceived social support from friends | −0.326 | −0.358 | −0.294 | 0.016 | <0.01 |
| Total indirect effect | 0.023 | 0.05 | 0.042 | 0.09 | 0.013 |
| Fear of COVID—Neuroticism—Perceived stress | 0.018 | 0.00 | 0.036 | 0.09 | 0.047 |
| Fear of COVID—Perceived social support from friends—Perceived stress | 0.016 | 0.06 | 0.025 | 0.05 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Q.; Kanjanarat, P.; Wongpakaran, T.; Ruengorn, C.; Awiphan, R.; Nochaiwong, S.; Wongpakaran, N.; Wedding, D. Fear of COVID-19 and Perceived Stress: The Mediating Roles of Neuroticism and Perceived Social Support. Healthcare 2022, 10, 812. https://doi.org/10.3390/healthcare10050812
Yang Q, Kanjanarat P, Wongpakaran T, Ruengorn C, Awiphan R, Nochaiwong S, Wongpakaran N, Wedding D. Fear of COVID-19 and Perceived Stress: The Mediating Roles of Neuroticism and Perceived Social Support. Healthcare. 2022; 10(5):812. https://doi.org/10.3390/healthcare10050812
Chicago/Turabian StyleYang, Qiuyi, Penkarn Kanjanarat, Tinakon Wongpakaran, Chidchanok Ruengorn, Ratanaporn Awiphan, Surapon Nochaiwong, Nahathai Wongpakaran, and Danny Wedding. 2022. "Fear of COVID-19 and Perceived Stress: The Mediating Roles of Neuroticism and Perceived Social Support" Healthcare 10, no. 5: 812. https://doi.org/10.3390/healthcare10050812
APA StyleYang, Q., Kanjanarat, P., Wongpakaran, T., Ruengorn, C., Awiphan, R., Nochaiwong, S., Wongpakaran, N., & Wedding, D. (2022). Fear of COVID-19 and Perceived Stress: The Mediating Roles of Neuroticism and Perceived Social Support. Healthcare, 10(5), 812. https://doi.org/10.3390/healthcare10050812










