Patient Profile and Management of Delirium in Older Adults Hospitalized Due to COVID-19
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ticinesi, A.; Cerundolo, N.; Parise, A.; Nouvenne, A.; Prati, B.; Guerra, A.; Lauretani, F.; Maggio, M.; Meschi, T. Delirium in COVID-19: Epidemiology and clinical correlations in a large group of patients admitted to an academic hospital. Aging Clin. Exp. Res. 2020, 32, 2159–2166. [Google Scholar] [CrossRef] [PubMed]
- Poloni, T.E.; Carlos, A.F.; Cairati, M.; Cutaia, C.; Medici, V.; Marelli, E.; Ferrari, D.; Galli, A.; Bognetti, P.; Davin, A.; et al. Prevalence and prognostic value of Delirium as the initial presentation of COVID-19 in the elderly with dementia: An Italian retrospective study. EClinicalMedicine 2020, 26, 100490. [Google Scholar] [CrossRef] [PubMed]
- Carlos III Health Institute, Epidemiological Surveillance Network. [Covid- I. Informe no 81. Situación de COVID-19 en España]. ISCIII-CNE 2021. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/INFORMES%20COVID-19%202021/Informe%20n%C2%BA%2081.%20Situaci%C3%B3n%20de%20COVID-19%20en%20Espa%C3%B1a%20a%202%20de%20junio%20de%202021.pdf (accessed on 3 January 2022).
- Epidemiological Surveillance Network. Carlos III Health Institute [Covid- I. Informe sobre la situación de COVID-19 en España]. Guía COVID-19. Información para profesionales sanitarios. ISCIII -CNE. 2020. Available online: https://repisalud.isciii.es/bitstream/handle/20.500.12105/11012/14%20-%20Profesionales%2028%20Septiembre.pdf?sequence=65&isAllowed=y (accessed on 3 January 2022).
- Fisicaro, F.; Di Napoli, M.; Liberto, A.; Fanella, M.; Di Stasio, F.; Pennisi, M.; Bella, R.; Lanza, G.; Mansueto, G. Neurological Sequelae in Patients with COVID-19: A Histopathological Perspective. Int. J. Environ. Res. Public Health 2021, 18, 1415. [Google Scholar] [CrossRef] [PubMed]
- Antón Jimenez, M.; Giner Santeodoro, A.; Villalba Lancho, E. Tratado de Geriatría Para Residentes; Sociedad Española de Enfermería Geriátrica: Madrid, Spain, 2006; pp. 189–198. [Google Scholar]
- Merino Vaca, C. Prevalencia del delirium en el paciente anciano ingresado en una unidad de convalescencia: Plan de cuidados y protocolo de prevención. Inf. Psiquiátricas 2018, 232, 131–138. [Google Scholar]
- Vazquez, F.; Flaherty, M.; Michelangelo, H.; Quiros, R.; Garfi, L.; Janson, J.; Camera, L. Epidemiología del delirio en ancianos hospitalizados. Medicina 2000, 60, 555–560. [Google Scholar]
- Vreeswijk, R.; Kalisvaart, I.; Maier, A.B.; Kalisvaart, K.J. Development and validation of the delirium risk assessment score (DRAS). Eur. Geriatr. Med. 2020, 11, 307–314. [Google Scholar] [CrossRef]
- Young, J.; Cheater, F.; Collinson, M.; Fletcher, M.; Forster, A.; Godfrey, M.; Green, J.; Anwar, S.; Hartley, S.; Hulme, C.; et al. Prevention of delirium (POD) for older people in hospital: Study protocol for a randomised controlled feasibility trial. Trials 2015, 16, 340. [Google Scholar] [CrossRef]
- Sánchez García, E. Prevención del Delirium en el Paciente Anciano: Diseño y Evaluación de Una Intervención no Farmacológica en el Ámbito Hospitalario; Universidad Complutense de Madrid: Madrid, Spain, 2015. [Google Scholar]
- Mcloughlin, B.C.; Miles, A.; Webb, T.E.; Knopp, P.; Eyres, C.; Fabbri, A.; Humphries, F.; Davis, D. Functional and cognitive outcomes after COVID-19 delirium. Eur. Geriatr. Med. 2020, 11, 857–862. [Google Scholar] [CrossRef]
- Perelló Campaner, C. Valoración del riesgo de delirium en pacientes mayores hospitalizados. Rev. Esp. Geriatr. Gerontol. 2010, 45, 285–290. [Google Scholar] [CrossRef]
- Schmitt, E.M.; Gallagher, J.; Albuquerque, A.; Tabloski, P.; Lee, H.J.; Gleason, L.; Schulman-Green, D. Perspectives on the Delirium Experience and Its Burden: Common Themes among Older Patients, Their Family Caregivers, and Nurses. Gerontologist 2019, 59, 327–337. [Google Scholar] [CrossRef]
- González Tugas, M.; Uslar Nawrath, W.; Villarroel del Pino, L.; Calderón Pinto, J.; Palma Onetto, C.; Carrasco Gorman, M. Coste hospitalario asociado al delirium en pacientes mayores. Rev. Esp. Geriatr. Gerontol. 2012, 47, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; Bogardus, S.T.; Charpentier, P.A.; Leo-Summers, L.; Acampora, D.; Holford, T.R.; Cooney, L.M. A Multicomponent Intervention to Prevent Delirium in Hospitalized Older Patients. N. Engl. J. Med. 1999, 340, 669–676. [Google Scholar] [CrossRef] [PubMed]
- O’Hanlon, S.; Inouye, S.K. Delirium: A missing piece in the COVID-19 pandemic puzzle. Age Ageing 2020, 49, 497–498. [Google Scholar] [CrossRef] [PubMed]
- Rubin, F.H.; Bellon, J.; Bilderback, A.; Urda, K.; Inouye, S.K. Effect of the Hospital Elder Life Program on Risk of 30-Day Readmission. J. Am. Geriatr. Soc. 2018, 66, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, N.S.; Mufti, M.; Ortiz, D.; Maye, S.; Melara, J.; Lim, D.; Price, C.C. Implementing Delirium Prevention in the Era of COVID-19. J. Alzheimer’s Dis. 2021, 79, 31–36. [Google Scholar] [CrossRef] [PubMed]
- De Castro, R.E.V.; Garcez, F.B.; Avelino-Silva, T.J. Patient care during the covid-19 pandemic: Do not leave delirium behind. Braz. J. Psychiatry 2021, 43, 127–128. [Google Scholar] [CrossRef]
- Garcez, F.B.; Aliberti, M.J.R.; Poco, P.C.E.; Hiratsuka, M.; de Takahashi, S.F.; Coelho, V.A.; Salotto, D.B.; Moreira, M.L.V.; Jacob-Filho, W.; Avelino-Silva, T.J. Delirium and Adverse Outcomes in Hospitalized Patients with COVID-19. J. Am. Geriatr. Soc. 2020, 68, 2440–2446. [Google Scholar] [CrossRef]
- Mendes, A.; Herrmann, F.R.; Périvier, S.; Gold, G.; Graf, C.E.; Zekry, D. Delirium in Older Patients With COVID-19: Prevalence, Risk Factors, and Clinical Relevance. J. Gerontol. Ser. A 2021, 76, e142–e146. [Google Scholar] [CrossRef]
- Zazzara, M.B.; Penfold, R.S.; Roberts, A.L.; Lee, K.A.; Dooley, H.; Sudre, C.H.; Lochlainn, M.N. Probable delirium is a presenting sympton of COVID-19 in frail, older adults: A cohort study of 322 hospitalized and 535 comunity-based older adults. Age Ageing 2021, 50, 40–48. [Google Scholar] [CrossRef]
- [Desarrollo De Guías De Práctica Clínica En Pacientes Con Comorbilidad Y Pluripatología]. SEMI-semFYC-FAECAP. Madrid. 2013. Available online: https://www.faecap.com/publicaciones/show/desarrollo-de-guias-de-practica-clinica-en-pacientes-con-comorbilidad-y-pluripatologia (accessed on 3 January 2022).
- Buzzini, D.M.; Secundini, R.; Gazzotti, A.; Giraldes, R.L.; Alejandro, R.; Castro, A.; Druetta, S.; Se-, S.; Rodríguez, A.; Li, L. Validación del Índice de Barthel. Boletín Del Dep. De Docencia E Investig. IREP 2002, 6, 9–12. [Google Scholar]
- Martínez de la Iglesiaa, J.; DueñasHerrero, R.; Carmen Onís Vilchesa, M.; Aguado Taberné, C.; Albert Colomer, C.; Luque Luque, R. Adaptación y validación al castellano del cuestionario de Pfeiffer (SPMSQ) para detectar la existencia de deterioro cognitivo en personas mayores e 65 años. Med. Clin. 2001, 117, 129–134. [Google Scholar] [CrossRef]
- Pancorbo, P.; García, F.; Soldevilla, J.; Blasco, C. Documento Técnico Gneaupp no xi “Escalas e instrumentos de valoración del riesgo de desarrollar úlceras por presión”. Gerocomos 2009, 19, 136–144. Available online: http://gneaupp.es/app/adm/documentos-guias/archivos/81_pdf.pdf (accessed on 3 January 2022).
- Alonso Ganuza, Z.; González-Torres, M.Á.; Gaviria, M. El Delirium: Una revisión orientada a la práctica clínica. Rev. La Asoc. Esp. Neuropsiquiatr. 2012, 32, 247–259. [Google Scholar] [CrossRef][Green Version]
- Aguilar-Navarro, S.G.; Duarte-Flores, J.O.; Granados-Valdéz, M.C.; Suing-Ortega, M.J.; Mimenza-Alvarado, A.J. Prevention, diagnosis, and treatment of delirium in older adults with COVID-19. Literature review. Salud Ment. 2020, 43, 319–327. [Google Scholar] [CrossRef]
- Inouye, S.K. The Short Confusion Assessment Method (Short CAM): Training Manual and Coding Guide. In Hosp Elder Life Program; Harvard Medical School: Boston, MA, USA, 2014; pp. 526–533. [Google Scholar]
- Carrera Castro, C. Un análisis cualitativo del rendimiento del Método de Evaluación de la Confusión. Investig en Enfermería Imagen y Desarro. Investig. En Enferm. Imagen Desarro. 2015, 17, 95–110. [Google Scholar] [CrossRef]
- Duaso, E.; Formiga, F.; Rodríguez, D. Tratamiento farmacológico del delirium. Rev. Esp. De Geriatría Gerontol. 2008, 43, 33–38. [Google Scholar]
- Nogal, M.L. Síndrome confusional. Psicogeriatría 2009, 1, 209–221. [Google Scholar]
- Woodhouse, R.; Burton, J.K.; Rana, N.; Pang, Y.L.; Lister, J.E.; Siddiqi, N. Interventions for preventing delirium in older people in institutional long-term care. Cochrane Database Syst. Rev. 2019, 4, CD009537 . [Google Scholar] [CrossRef]
- Britton, A.M.; Russell, R. Multidisciplinary team interventions for delirium in patients with chronic cognitive impairment. Cochrane Database Syst. Rev. 2002. [Google Scholar] [CrossRef]
- Inouye, S.K.; Zhang, Y.; Jones, R.N.; Kiely, D.K.; Yang, F.; Marcantonio, E.R. Risk Factors for Delirium at Discharge. Arch. Int. Med. 2007, 167, 1406. [Google Scholar] [CrossRef]
- Carignan, C.C.; Punshon, T.; Karagas, M.R.; Cottingham, K.L.; Hanover, N. HHS Public Access. Ann. Glob. Health Author Manuscr. 2018, 318, 1161–1174. [Google Scholar]
- Claver Martín, M.D. Actualización en la evaluación y tratamiento del delirium. Rev. Esp. Geriatr. Gerontol. 2008, 34. Available online: http://www.elsevier.es/es-revista-revista-espanola-geriatria-gerontologia-124-articulo-actualizacion-evaluacion-tratamiento-del-delirium-13011650 (accessed on 3 January 2022).
- Heaven, A.; Cheater, F.; Clegg, A.; Collinson, M.; Farrin, A.; Forster, A.; Siddiqi, N. Pilot trial of Stop Delirium! (PiTStop)-a complex intervention to prevent delirium in care homes for older people: Study protocol for a cluster randomised controlled trial. Trials 2014, 15, 47. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic Variables | Items | N (%) or Mean ± SD 1 |
|---|---|---|
| Age range (65–95) | 77.29 ± 7.7 | |
| 65–74 | 42 (38.9) | |
| 75–85 | 44 (40.7) | |
| >85 | 22 (20.4) | |
| Sex | Male | 63 (58.3) |
| Female | 45 (41.7) | |
| Place of residence | Urban | 62 (57.4) |
| Rural | 46 (42.6) | |
| Cohabitants | Partner or spouse | 60 (55.6) |
| Other relative | 10 (9.3) | |
| Living alone | 18 (16.7) | |
| Paid carer | 5 (4.6) | |
| Nursing home | 15 (13.9) | |
| Clinical history Comorbidities 2 | <2 | 36 (32.4) |
| x > 2 | 56 (52.8) | |
| No comorbidities | 16 (14.8) |
| Variable | N (%) | No ADOP n (%) | ADOP n (%) | Chi2/Fisher (p) |
|---|---|---|---|---|
| Age | ||||
| 65–75 | 50 (46.3) | 42 (55.3) | 8 (25) | 0.001 |
| 76–85 | 38 (35.2) | 26 (34.2) | 12 (37.5) | |
| >86 | 22 (18.5) | 8 (10.5) | 12 (37.5) | |
| Male sex | 45 (41.7) | 33 (43.5) | 12 (37.5) | 0.569 |
| Comorbidity | 57 (52.8) | 38 (50) | 19 (59.4) | 0.021 |
| Medical diagnosis of dementia | 15 (13.8) | 6 (7.9) | 9 (28.2) | 0.021 |
| Severe dependent (Barthel < 35) | 3 (2.8) | 0 | 3 (9.4) | 0.000 |
| Moderate dependent (Barthel 35–65) | 27 (25) | 13 (17.1) | 14 (43.8) | |
| Slight dependent or independent | 78 (72.2) | 63 (82.9) | 15 (46.9) | |
| Severe cognitive impairment (Pfeiffer 7–10) | 6 (5.6) | 2 (2.6) | 4 (12.5) | 0.000 |
| Moderate cognitive impartment (Pfeiffer 3–7) | 16 (14.8) | 2 (2.6) | 14 (43.8) | |
| No cognitive impairment | 86 (79.6) | 72 (94.7) | 14 (43.8) | |
| Auditive sensorial deterioration | 19 (17.6) | 10 (13.2) | 9 (28.1) | 0.021 |
| Visual sensorial deterioration | 8 (7.4) | 4 (5.3) | 4 (12.5) | |
| Auditive and visual sensorial deterioration | 3 (2.8) | 1 (1.3) | 2 (6.3) | |
| Average nutritional status | 47 (43.5) | 34 (44.7) | 13 (40.6) | 0.407 |
| Mediocre nutritional status | 28 (25.9) | 17 (22.4) | 11 (34.4) | |
| Dehydrated | 2 (1.9) | 0 | 2 (6.3) | 0.086 |
| Daily use of hypnotics | 35 (32.4) | 22 (28.9) | 13 (40.6) | 0.477 |
| Previous ADOP | 8 (7.4) | 3 (3.9) | 5 (15.6) | 0.048 |
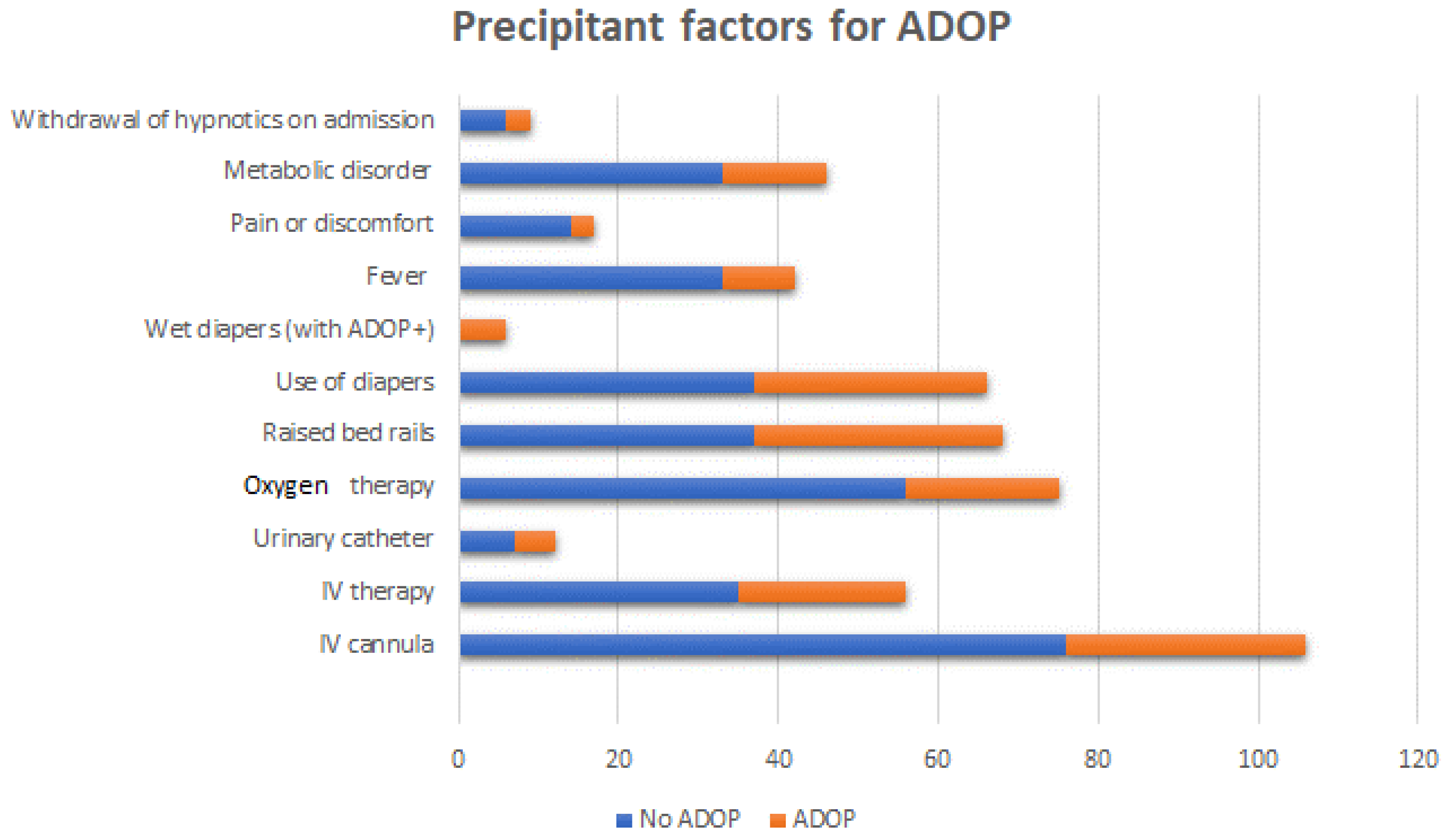
| Variable | Total (%) | No ADOP (%) | ADOP (%) | Chi2/Fisher (p) |
|---|---|---|---|---|
| IV cannula | 106 (98.1) | 76 (100) | 30 (96.8) | 0.116 |
| IV therapy | 56 (51.9) | 35 (47.3) | 21 (70) | 0.035 |
| Urinary catheter | 12 (11.1) | 7 (9.2) | 5 (16.1) | 0.323 |
| Oxygen therapy | 92 (85.2) | 56 (88.9) | 19 (65.5) | 0.021 |
| Raised bed rails | 68 (63) | 37 (48.7) | 31 (100) | 0.000 |
| Use of diapers | 66 (61.1) | 37 (48.7) | 29 (93.5) | 0.000 |
| Wet diapers (with ADOP+) | 6 (5.6) | 0 | 6 (21.4) | 0.557 |
| Fever | 42 (38.9) | 33 (44) | 9 (28.1) | 0.124 |
| Pain or discomfort | 17 (15.7) | 14 (18.9) | 3 (9.7) | 0.241 |
| Metabolic disorder | 51 (47.2) | 33 (43.4) | 13 (62.5) | 0.135 |
| Withdrawal of hypnotics on admission | 9 (8.3) | 6 (27.3) | 3 (9.4) | 1.0 |
| Variable | Verbal n (%) | Verbal and Pharmacologic n (%) | Pharmacologic and Physical n (%) | p | |
|---|---|---|---|---|---|
| Barthel Index | Severe dependent | 0 | 2 (10.5) | 0 | 0.511 |
| Moderate dependent | 4 (50) | 8 (42.1) | 2 (100) | ||
| Independent | 4 (50) | 9 (47.4) | 0 | ||
| Pfeiffer’s SPMSQ | Normal | 3 (37.5) | 9 (47.4) | 1 (50) | 0.976 |
| Slight–moderate | 4 (50) | 8 (42.1) | 1 (50) | ||
| Severe | 1 (12.5) | 2 (10.5) | 0 | ||
| Age | 65–75 | 3 (37.5) | 4 (21.1) | 1 (50) | 0.266 |
| 76–85 | 4 (50) | 5 (26.3) | 1 (50) | ||
| >86 | 1 (12.5) | 10 (52.6) | 0 | ||
| Sex | Male | 2 (25) | 9 (47.4) | 1 (50) | 0.541 |
| Female | 6 (75) | 10 (52.6) | 1 (50) | ||
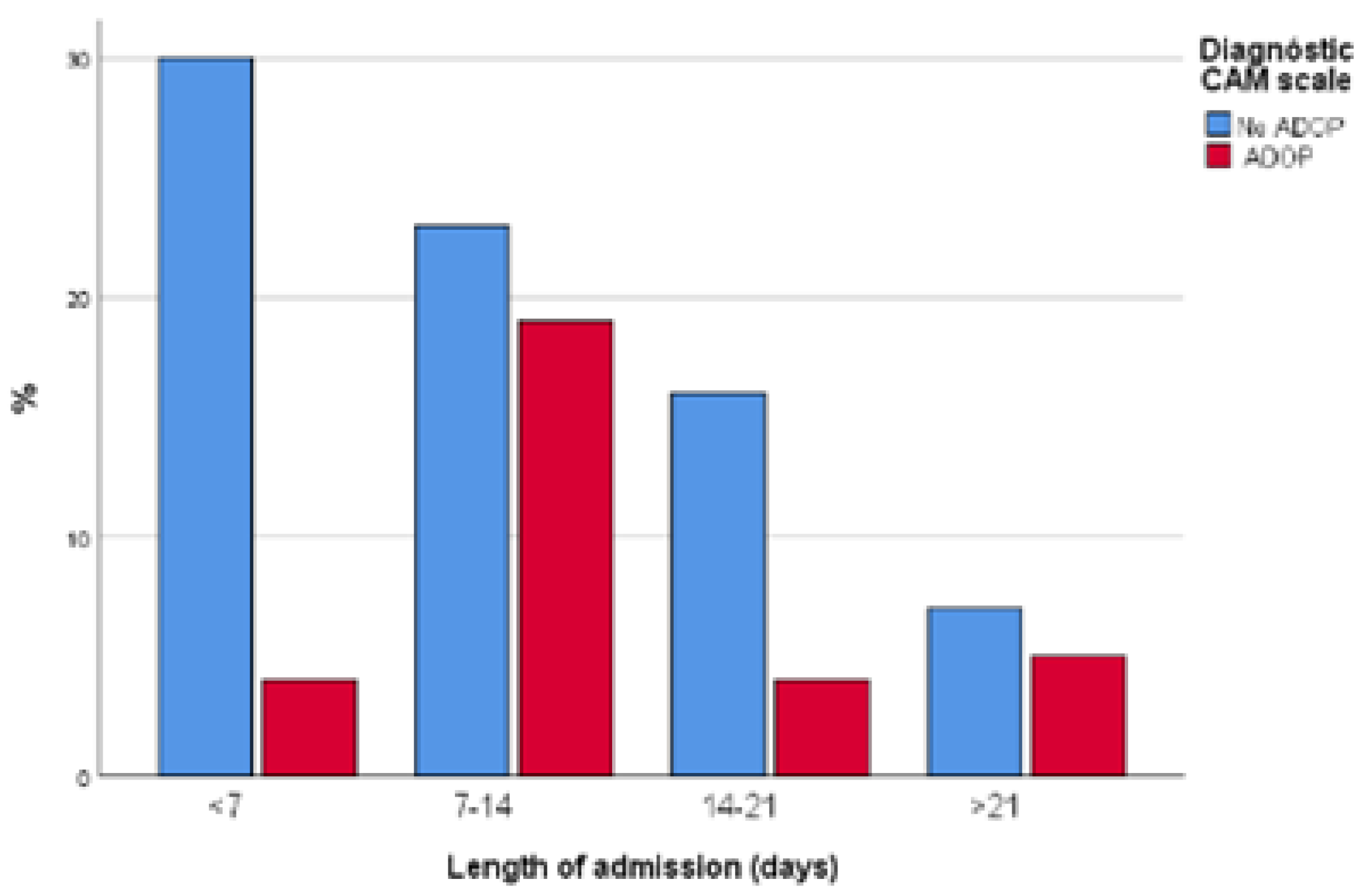
| Variable | NO ADOP n (%) | ADOP n (%) | (p) | ||||
| Length of admission | <7 days | 30 (39.5) | 4 (12.5) | 0.006 | |||
| 7–14 days | 23 (30.3) | 19 (59.4) | |||||
| 14–21 days | 16 (21.1) | 4 (12.5) | |||||
| >21 days | 7 (9.2) | 5 (15.6) | |||||
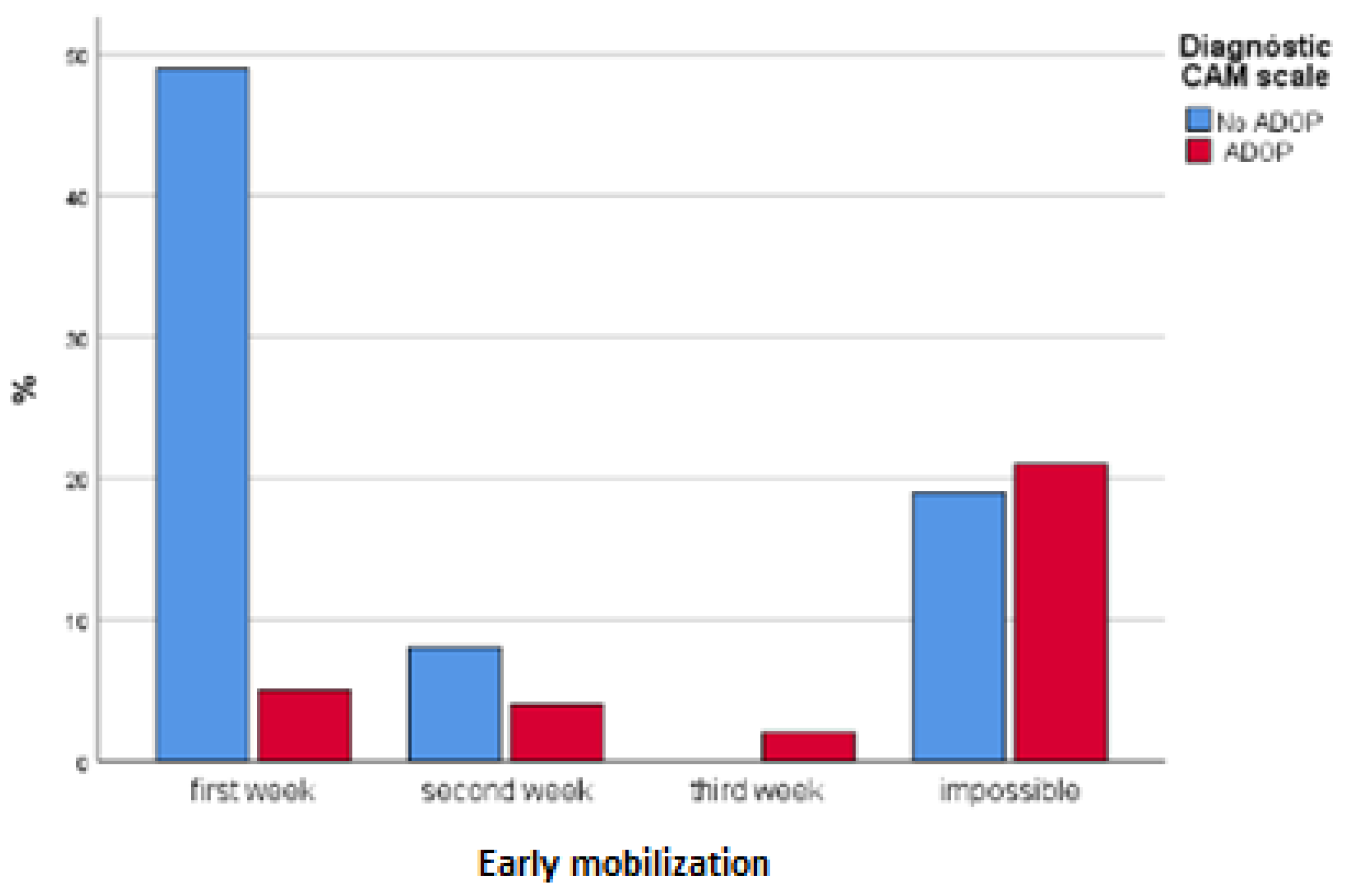
| Early mobilization | First week | 49 (64.5) | 5 (15.6) | 0.000 | |||
| Second week | 8 (10.5) | 4 (12.5) | |||||
| Third week | 0 | 2 (6.3) | |||||
| No early mobilization | 19 (25) | 21 (65.6) | |||||
|
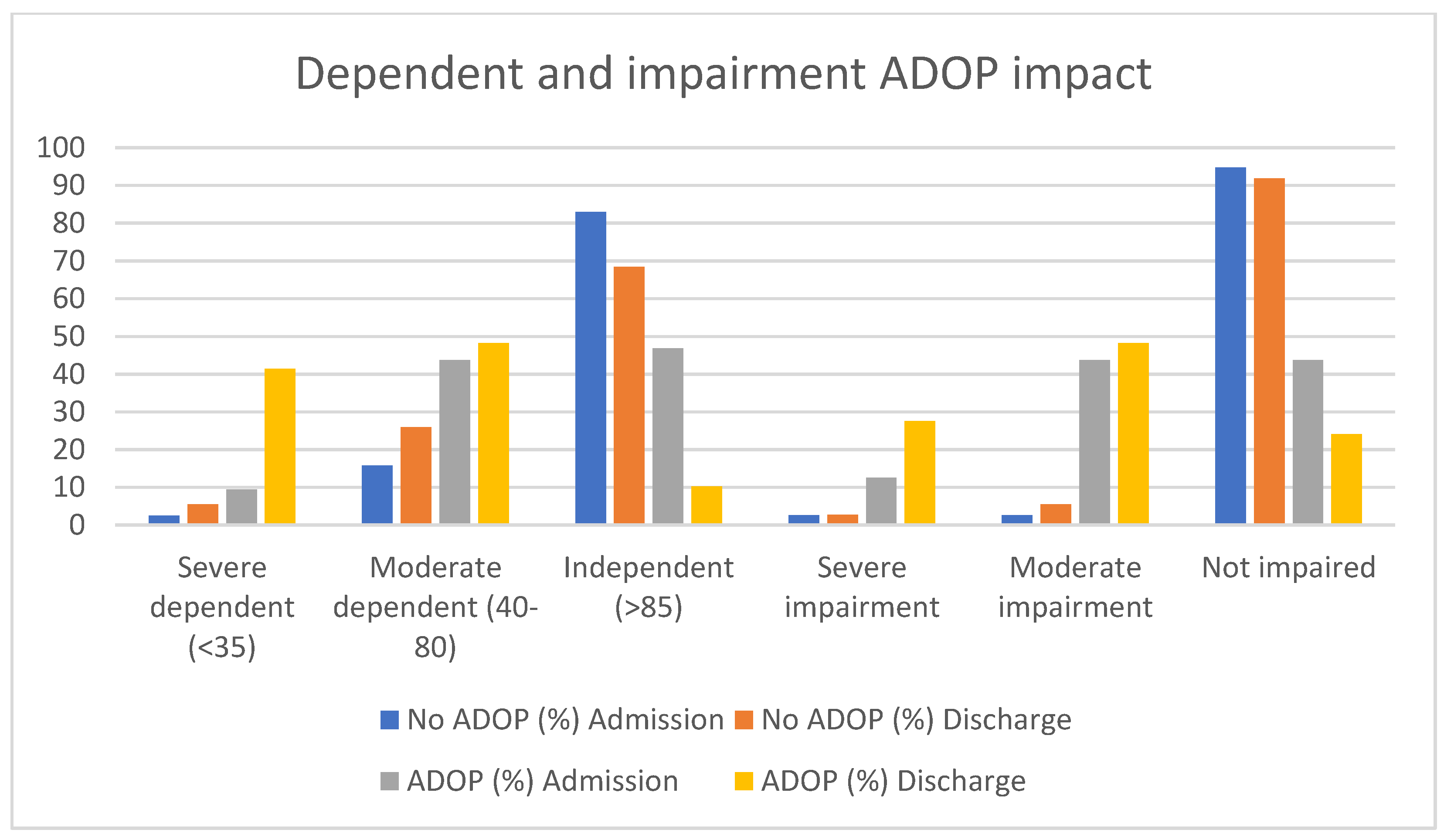
Barthel Index (on discharge) | Severe dependent (<35) | 4 (5.5) | 12 (37.9) | 0.000 | |||
| Moderate dependent (40–80) | 19 (26) | 14 (48.3) | |||||
| Independent (>85) | 50 (68.6) | 3 (10.3) | |||||
| Pfeiffer’s SPMSQ (on discharge) | Severe impairment (8–10) | 2 (2.6) | 8 (27.6) | 0.000 | |||
| Moderate impairment (4–7) | 4 (5.2) | 14 (48.3) | |||||
| No impairment (0–3) | 67 (91.8) | 7 (24.1) | |||||
| No ADOP n/(%) | (p) | ADOP n/(%) | (p) | ||||
| Admission | Discharge | Admission | Discharge | ||||
| Barthel Index | Severe dependent (<35) | 1/2.5 | 4/5.5 | 3/9.4 | 12/41.4 | ||
| Moderate dependent (40–80) | 12/15.8 | 19/26 | 14/43.8 | 14/48.3 | |||
| Independent (>85) | 63/82.9 | 50/68.5 | 0.112 | 15/46.9 | 3/10.3 | 0.01 | |
| Pfeiffer’s SPMSQ | Severe impairment | 2/2.6 | 2/2.7 | 4/12.5 | 8/27.6 | ||
| Moderate impairment | 2/2.6 | 14/5.5 | 14/43.8 | 14/48.3 | |||
| Not impaired | 72/94.7 | 67/91.8 | 0.00 | 14/43.8 | 7/24.1 | 0.17 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jorge-Samitier, P.; Juárez-Vela, R.; Santolalla-Arnedo, I.; Antón-Solanas, I.; Gea-Caballero, V.; Sánchez-González, J.L.; Fernández-Rodrigo, M.T. Patient Profile and Management of Delirium in Older Adults Hospitalized Due to COVID-19. Healthcare 2022, 10, 724. https://doi.org/10.3390/healthcare10040724
Jorge-Samitier P, Juárez-Vela R, Santolalla-Arnedo I, Antón-Solanas I, Gea-Caballero V, Sánchez-González JL, Fernández-Rodrigo MT. Patient Profile and Management of Delirium in Older Adults Hospitalized Due to COVID-19. Healthcare. 2022; 10(4):724. https://doi.org/10.3390/healthcare10040724
Chicago/Turabian StyleJorge-Samitier, Pablo, Raúl Juárez-Vela, Iván Santolalla-Arnedo, Isabel Antón-Solanas, Vicente Gea-Caballero, Juan Luis Sánchez-González, and María Teresa Fernández-Rodrigo. 2022. "Patient Profile and Management of Delirium in Older Adults Hospitalized Due to COVID-19" Healthcare 10, no. 4: 724. https://doi.org/10.3390/healthcare10040724
APA StyleJorge-Samitier, P., Juárez-Vela, R., Santolalla-Arnedo, I., Antón-Solanas, I., Gea-Caballero, V., Sánchez-González, J. L., & Fernández-Rodrigo, M. T. (2022). Patient Profile and Management of Delirium in Older Adults Hospitalized Due to COVID-19. Healthcare, 10(4), 724. https://doi.org/10.3390/healthcare10040724








