LigaSure versus Conventional Parotidectomy: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Literature Search
2.2. Study Selection and Data Extraction
2.3. Risk of Bias Assessment
2.4. Data Analysis
3. Results
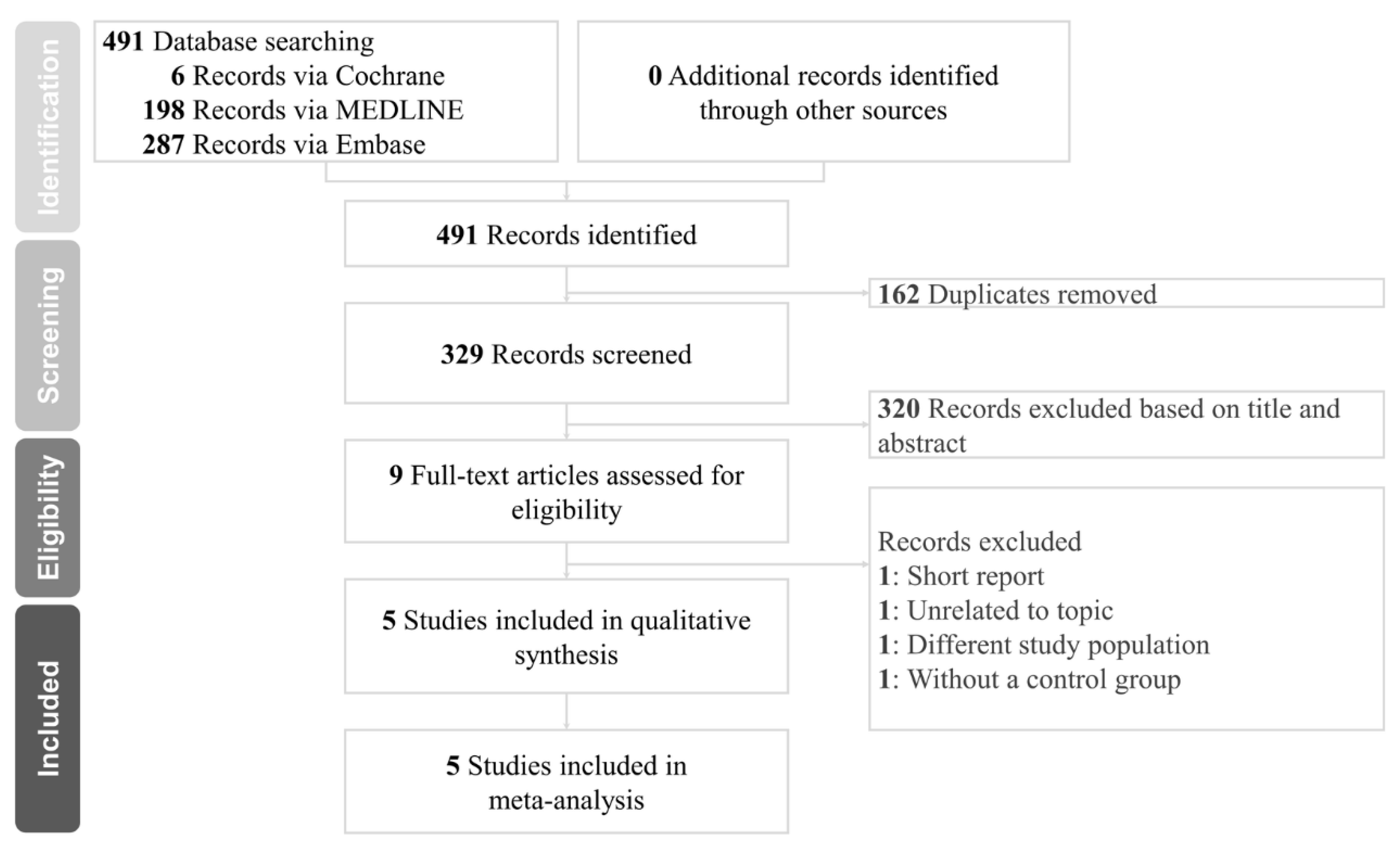
3.1. Study Selection
3.2. Demographics
3.3. Outcomes
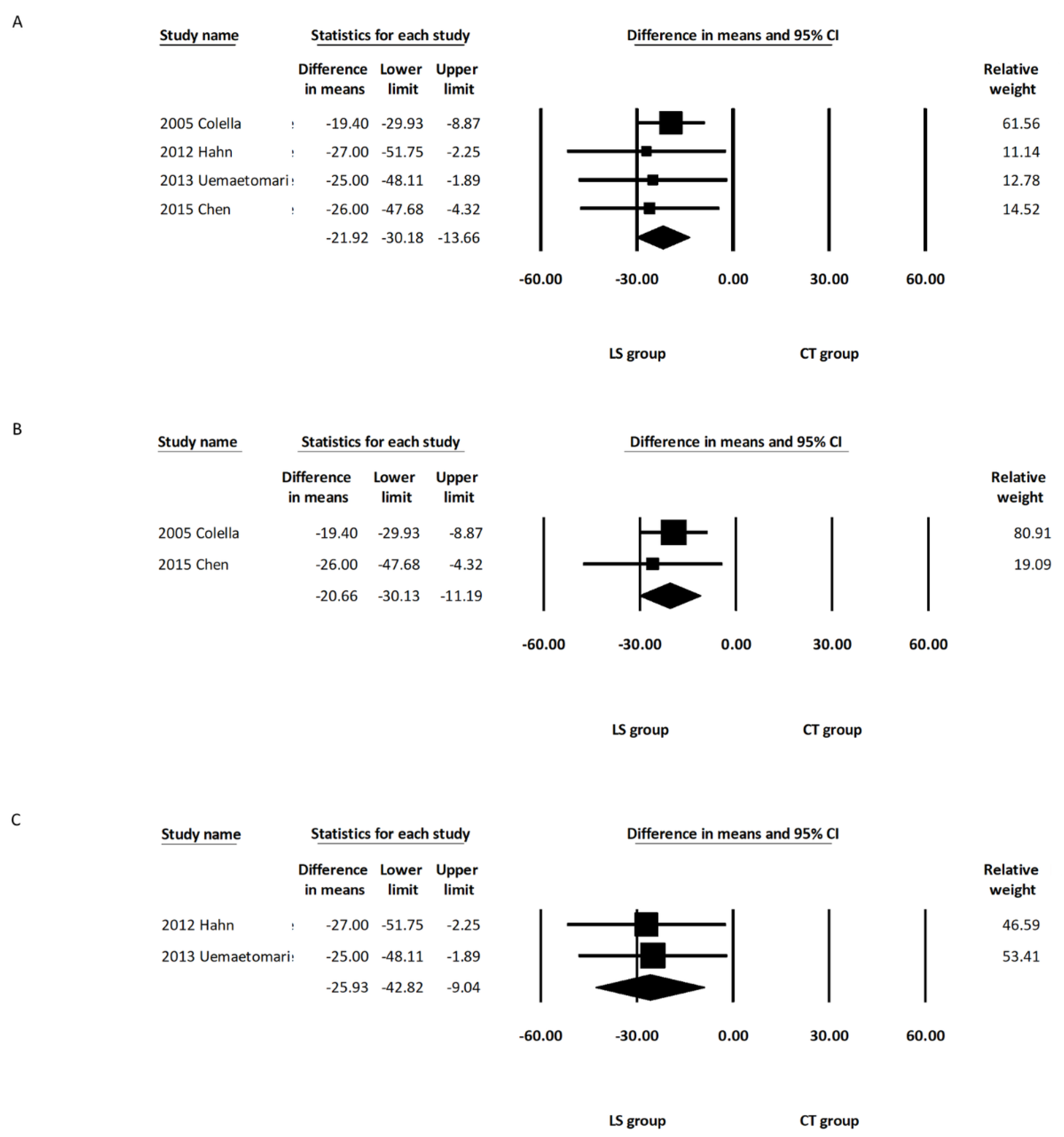
3.3.1. Operative Duration
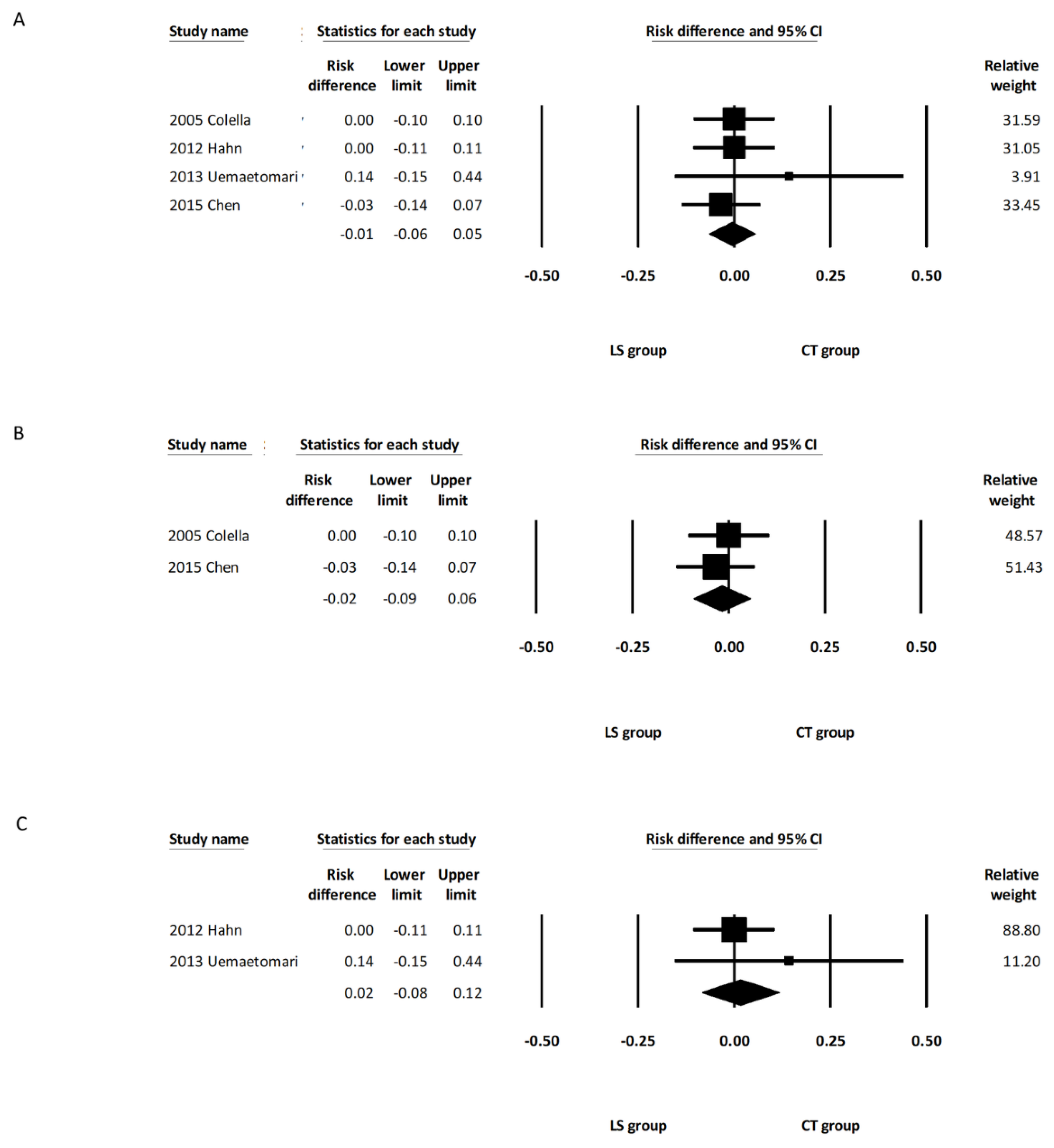
3.3.2. Postoperative Facial Palsy
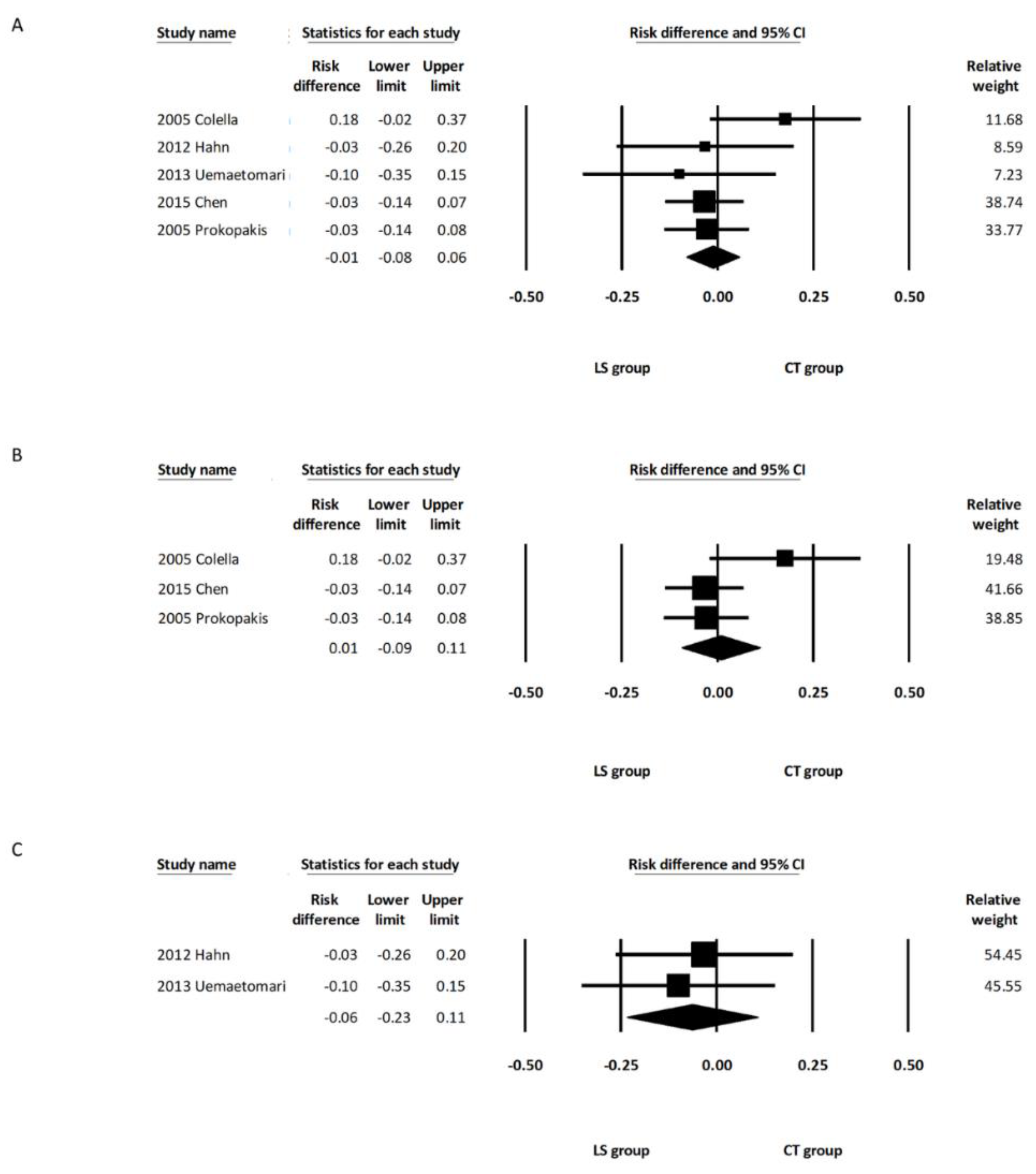
3.3.3. Postoperative Salivary Complications (Salivary Fistula/Seroma)
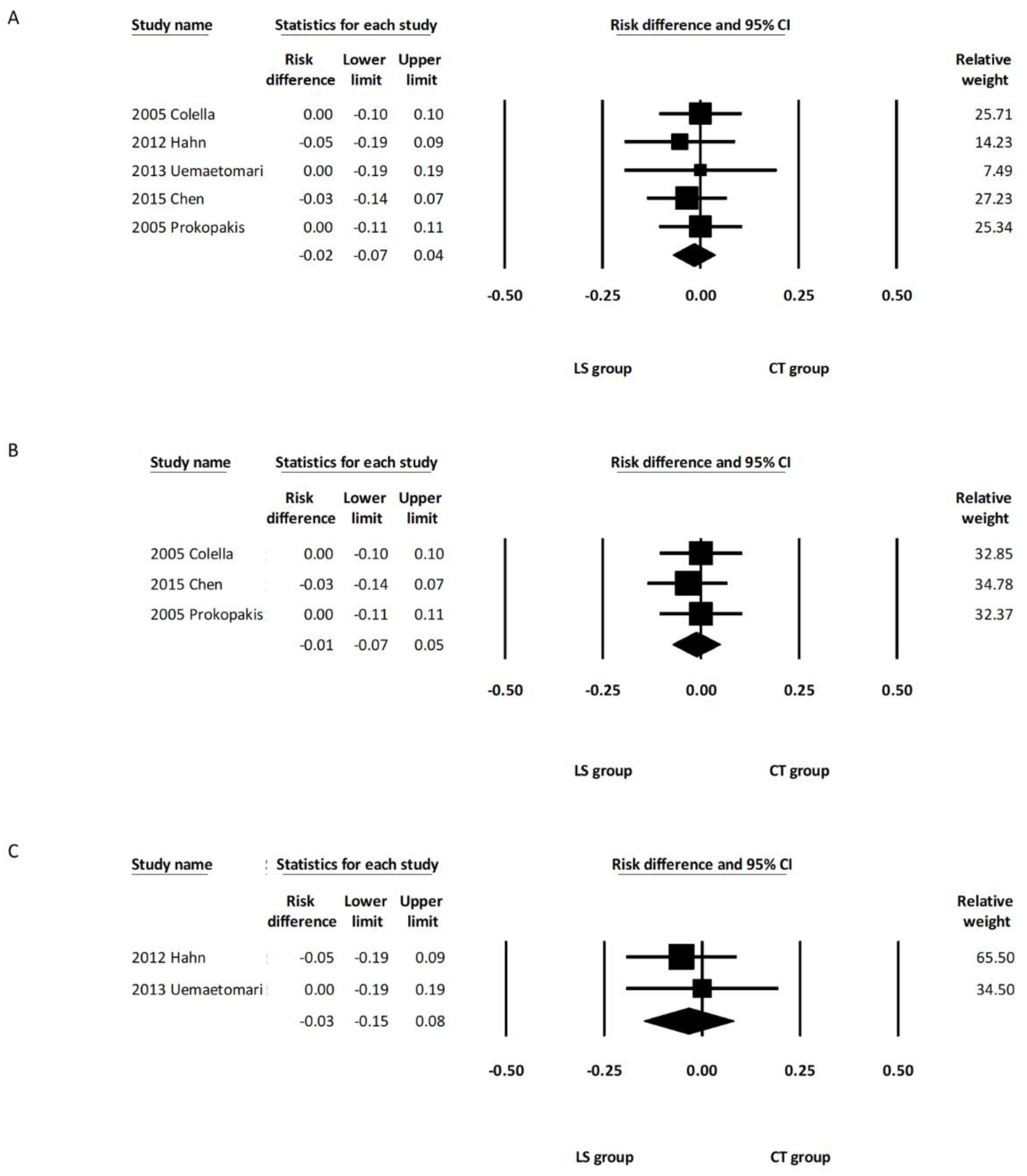
3.3.4. Postoperative Bleeding Complications
3.4. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Przewoźny, T.; Stankiewicz, C. Neoplasms of the parotid gland in northern Poland, 1991–2000: An epidemiologic study. Eur. Arch. Oto-Rhino-Laryngol. Head Neck 2004, 261, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Liao, W.C.; Yang, S.W.; Luo, C.M.; Tsai, Y.T.; Tsai, M.S.; Lee, Y.H.; Hsin, L.J. Systematic review and meta-analysis of modified facelift incision versus modified Blair incision in parotidectomy. Sci. Rep. 2021, 11, 24106. [Google Scholar] [CrossRef] [PubMed]
- Harell, M.; Levy, D.; Elam, M. Superficial parotidectomy for benign parotid lesions. Oper. Tech. Otolaryngol. Head Neck Surg. 1996, 7, 315–322. [Google Scholar] [CrossRef]
- Dubuc-Lissoir, J. Use of a new energy-based vessel ligation device during laparoscopic gynecologic oncologic surgery. Surg. Endosc. Other Interv. Tech. 2003, 17, 466–468. [Google Scholar] [CrossRef] [PubMed]
- Kim, F.J.; Chammas, M.; Gewehr, E.; Morihisa, M.; Caldas, F.; Hayacibara, E.; Baptistussi, M.; Meyer, F.; Martins, A.C. Temperature safety profile of laparoscopic devices: Harmonic ACE (ACE), Ligasure V (LV), and plasma trisector (PT). Surg. Endosc. 2008, 22, 1464–1469. [Google Scholar] [CrossRef]
- Youssef, T.; Mahdy, T.; Farid, M.; Latif, A.A. Thyroid surgery: Use of the LigaSure Vessel Sealing System versus conventional knot tying. Int. J. Surg. 2008, 6, 323–327. [Google Scholar] [CrossRef]
- Person, B.; Vivas, D.A.; Ruiz, D.; Talcott, M.; Coad, J.E.; Wexner, S.D. Comparison of four energy-based vascular sealing and cutting instruments: A porcine model. Surg. Endosc. 2008, 22, 534–538. [Google Scholar] [CrossRef]
- Petrakis, I.E.; Kogerakis, N.E.; Lasithiotakis, K.G.; Vrachassotakis, N.; Chalkiadakis, G.E. LigaSure versus clamp-and-tie thyroidectomy for benign nodular disease. Head Neck J. Sci. Spec. Head Neck 2004, 26, 903–909. [Google Scholar] [CrossRef]
- Ding, Z.; Wable, M.; Rane, A. Use of LigaSure™ bipolar diathermy system in vaginal hysterectomy. J. Obstet. Gynaecol. 2005, 25, 49–51. [Google Scholar] [CrossRef]
- Chen, T.-Y.; Hsin, L.-J.; Lin, W.-N.; Tsai, M.-S.; Tsai, Y.-T.; Lee, Y.-C. LigaSure small jaw versus conventional neck dissection: A systematic review and meta-analysis. J. Otolaryngol. Head Neck Surg. 2021, 50, 1–8. [Google Scholar] [CrossRef]
- Uemaetomari, I.; Wada, T.; Nishimura, B.; Tanaka, S.; Nakayama, M.; Ashizawa, K.; Tabuchi, K.; Minami, Y.; Hara, A. Vessel Sealing Device in Parotid Gland Surgery: Clinical and Pathological Study. Adv. Cancer Res. Treat. 2013, 2013, 992721. [Google Scholar] [CrossRef]
- Prokopakis, E.P.; Lachanas, V.A.; Helidonis, E.S.; Velegrakis, G.A. The use of the Ligasure Vessel Sealing System in parotid gland surgery. Otolaryngol. Head Neck Surg. 2005, 133, 725–728. [Google Scholar] [CrossRef] [PubMed]
- Hahn, C.H.; Sørensen, C.H. LigaSure small jaws versus cold knife dissection in superficial parotidectomy. Eur. Arch. Oto-Rhino-Laryngol. 2013, 270, 1489–1492. [Google Scholar] [CrossRef] [PubMed]
- Colella, G.; Giudice, A.; Vicidomini, A.; Sperlongano, P. Usefulness of the LigaSure vessel sealing system during superficial lobectomy of the parotid gland. Arch. Otolaryngol. Head Neck Surg. 2005, 131, 413–416. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, W.; Chuang, H.; Su, Y.; Chien, C. Predictive factors for post-operative drainage after partial superficial parotidectomy: A case-control study. J. Laryngol. Otol. 2015, 129, 1020. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Kennedy, J.; Stranahan, P.; Taylor, K.; Chandler, J. High-burst-strength, feedback-controlled bipolar vessel sealing. Surg. Endosc. 1998, 12, 876–878. [Google Scholar] [CrossRef]
- Družijanić, N.; Pogorelić, Z.; Perko, Z.; Mrklić, I.; Tomić, S. Comparison of lateral thermal damage of the human peritoneum using monopolar diathermy, Harmonic scalpel and LigaSure. Can. J. Surg. 2012, 55, 317. [Google Scholar] [CrossRef]
- Milito, G.; Gargiani, M.; Cortese, F. Randomised trial comparing LigaSure haemorrhoidectomy with the diathermy dissection operation. Tech. Coloproctol. 2002, 6, 171–175. [Google Scholar] [CrossRef]
- Prokopakis, E.; Lachanas, V.; Vardouniotis, A.; Velegrakis, G. The use of the Ligasure™ Vessel Sealing System in head and neck surgery: A report on six years of experience and a review of the literature. Acta Oto-Rhino-Laryngol. Belg. 2010, 6, 19. [Google Scholar]
- Lachanas, V.A.; Prokopakis, E.P.; Bourolias, C.A.; Karatzanis, A.D.; Malandrakis, S.G.; Helidonis, E.S.; Velegrakis, G.A. Ligasure versus cold knife tonsillectomy. The Laryngoscope 2005, 115, 1591–1594. [Google Scholar] [CrossRef] [PubMed]
- Covidien. Available online: https://www.medtronic.com/covidien/en-us/products/vessel-sealing/ligasure-small-jaw.html (accessed on 20 February 2022).
- Kanno, C.; Masubuchi, T.; Tada, Y.; Fushimi, C.; Matsuki, T.; Takahashi, H.; Okada, T.; Inomata, T.; Sasaki, M.; Niwa, K.; et al. Efficacy and safety of a vessel sealing system in oral cancer resection and reconstructive surgery. Acta Oto-Laryngol. 2018, 138, 759–762. [Google Scholar] [CrossRef] [PubMed]
- Mehle, M.E.; Kraus, D.H.; Wood, B.G.; Benninger, M.S.; Eliachar, I.; Levine, H.L.; Tucker, H.M.; Lavertu, P. Facial nerve morbidity following parotid surgery for benign disease: The Cleveland Clinic Foundation experience. Laryngoscope 1993, 103, 386–388. [Google Scholar] [CrossRef]
- Lin, C.-C.; Tsai, M.-H.; Huang, C.-C.; Hua, C.-H.; Tseng, H.-C.; Huang, S.-T. Parotid tumors: A 10-year experience. Am. J. Otolaryngol. 2008, 29, 94–100. [Google Scholar] [CrossRef]
- Hotton, M.; Huggons, E.; Hamlet, C.; Shore, D.; Johnson, D.; Norris, J.H.; Kilcoyne, S.; Dalton, L. The psychosocial impact of facial palsy: A systematic review. Br. J. Health Psychol. 2020, 25, 695–727. [Google Scholar] [CrossRef]
- Britt, C.J.; Stein, A.P.; Gessert, T.; Pflum, Z.; Saha, S.; Hartig, G.K. Factors influencing sialocele or salivary fistula formation postparotidectomy. Head Neck 2017, 39, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Herbert, H.A.; Morton, R.P. Sialocele after parotid surgery: Assessing the risk factors. Otolaryngol. Head Neck Surg. 2012, 147, 489–492. [Google Scholar] [CrossRef]
- Kilavuz, A.E.; Songu, M.; Pinar, E.; Ozkul, Y.; Ozturkcan, S.; Aladag, I. Superficial parotidectomy versus partial superficial parotidectomy: A comparison of complication rates, operative time, and hospital stay. J. Oral Maxillofac. Surg. 2018, 76, 2021–2032. [Google Scholar] [CrossRef]

| Authors | Year | Country | Study Design | Number of Patients | Mean Age (Years) | Gender (M/F) | Surgery Type | LigaSure Type | Final Diagnosis | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LS | CT | LS | CT | LS | CT | |||||||
| Colella et al. | 2005 | Italy | Prospective | 17 | 18 | 45 | 49 | 8/9 | 7/11 | SP | LSP | PA, WT, LP, MY |
| Prokopakis et al. | 2005 | Greece | Prospective | 12 | 103 | 51 | 54 | 3/9 | 24/79 | SP | LSP | N/A |
| Hahn et al. | 2013 | Denmark | Prospective | 16 | 19 | 59 | 53 | 6/10 | 12/7 | SP | LSJ | PA, WT, ON, SA, LC |
| Uemaetomari et al. | 2013 | Japan | Retrospective | 8 | 10 | 54.5 | 50.4 | N/A | N/A | SP, TP | LSJ | PA, WT |
| Chen et al. | 2015 | Taiwan | Prospective | 20 | 29 | 51.6 | 51.4 | 13/7 | 21/8 | SP | LSP | PA, WT, OTH |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.W.-T.; Hsin, L.-J.; Lin, W.-N.; Tsai, Y.-T.; Tsai, M.-S.; Lee, Y.-C. LigaSure versus Conventional Parotidectomy: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 706. https://doi.org/10.3390/healthcare10040706
Chen SW-T, Hsin L-J, Lin W-N, Tsai Y-T, Tsai M-S, Lee Y-C. LigaSure versus Conventional Parotidectomy: A Systematic Review and Meta-Analysis. Healthcare. 2022; 10(4):706. https://doi.org/10.3390/healthcare10040706
Chicago/Turabian StyleChen, Sonia Wei-Ting, Li-Jen Hsin, Wan-Ni Lin, Yao-Te Tsai, Ming-Shao Tsai, and Yi-Chan Lee. 2022. "LigaSure versus Conventional Parotidectomy: A Systematic Review and Meta-Analysis" Healthcare 10, no. 4: 706. https://doi.org/10.3390/healthcare10040706
APA StyleChen, S. W.-T., Hsin, L.-J., Lin, W.-N., Tsai, Y.-T., Tsai, M.-S., & Lee, Y.-C. (2022). LigaSure versus Conventional Parotidectomy: A Systematic Review and Meta-Analysis. Healthcare, 10(4), 706. https://doi.org/10.3390/healthcare10040706







