Interactive Video Games as a Method to Increase Physical Activity Levels in Children Treated for Leukemia
Abstract
1. Introduction
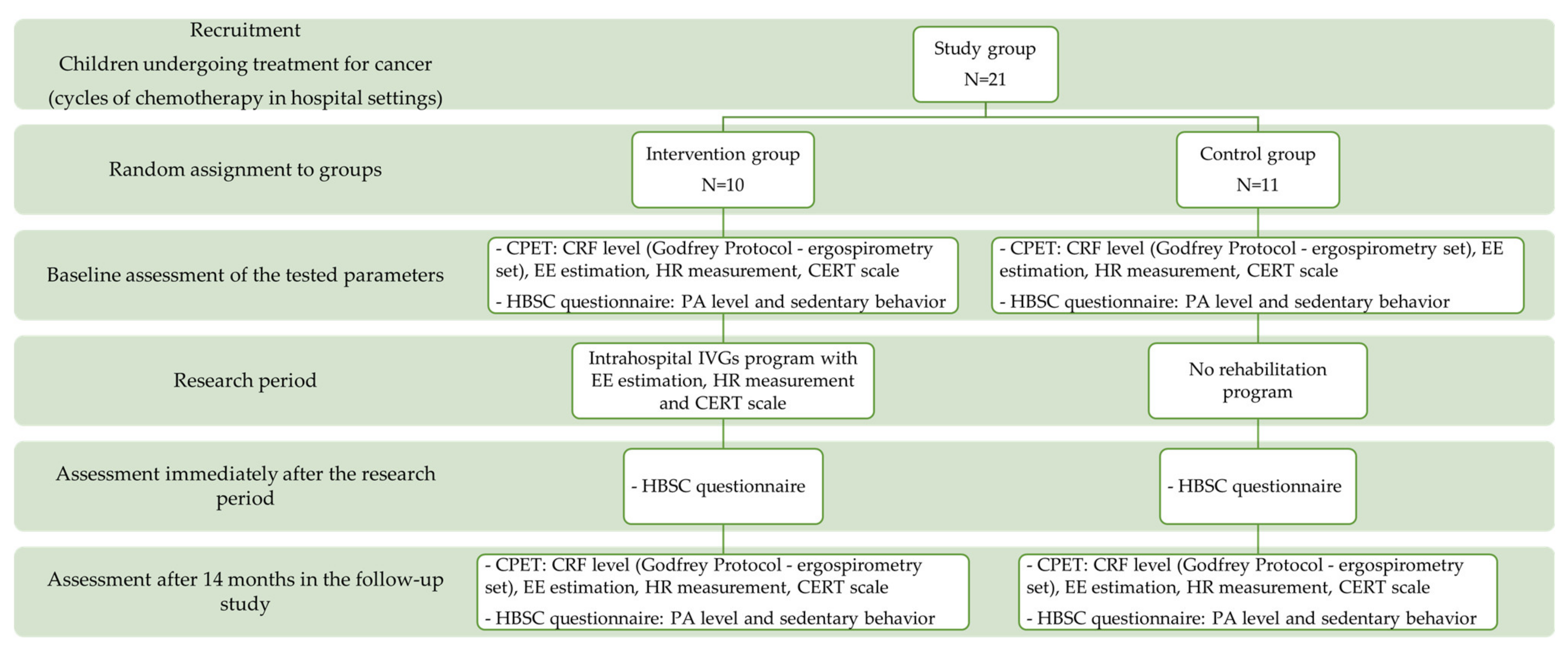
2. Study Design
2.1. Participants and Recruitment
2.2. Intervention Group
2.3. Control Group
2.4. Participants Characteristics
3. Research Methods
3.1. Cardiorespiratory Fitness
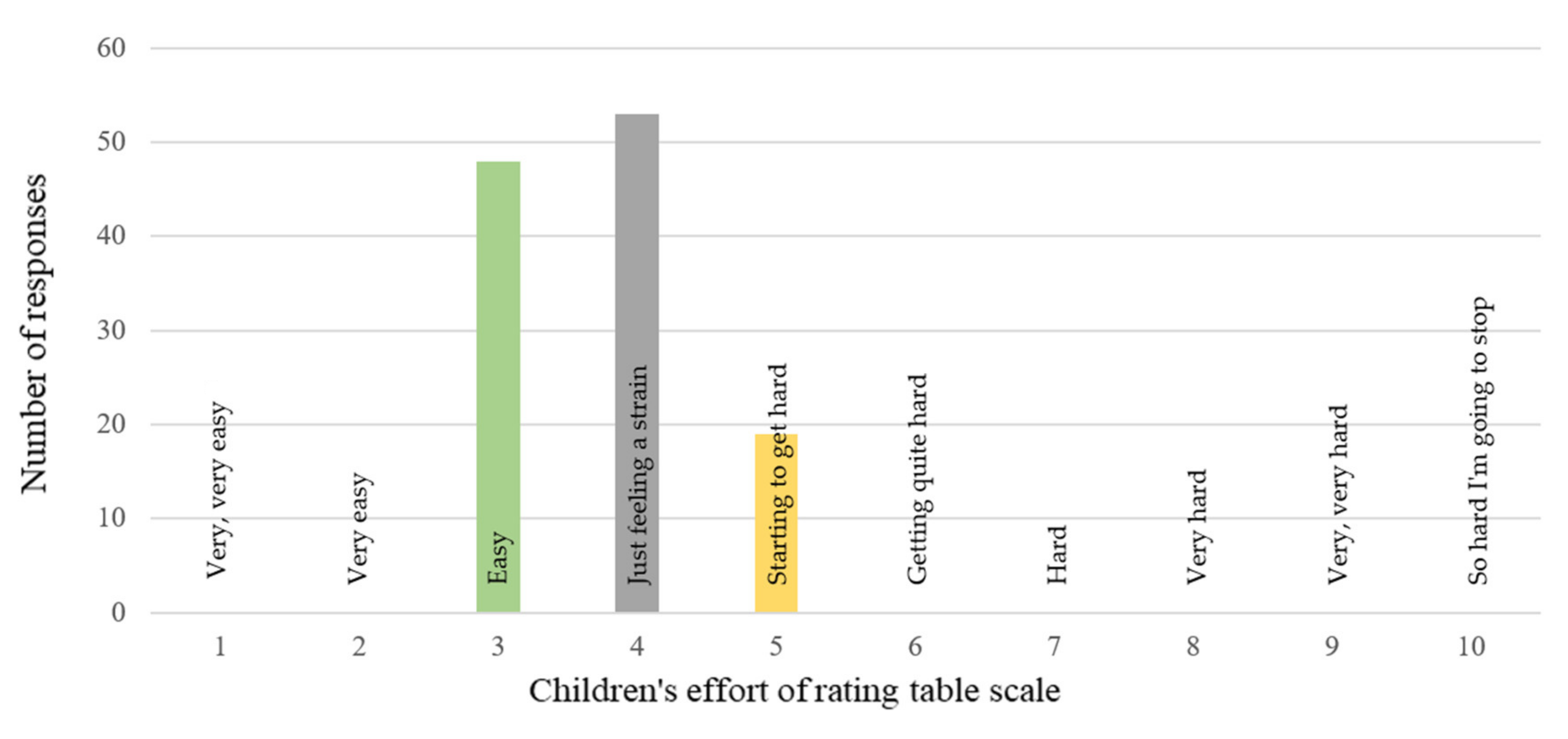
3.2. Children’s Effort Rating Table (CERT) Scale
3.3. Energy Expenditure during the IVGs Intervention
3.4. Health Behavior Based on the School-Aged Children (HBSC 2018) Questionnaire
4. Training with IVGs—Intervention Group
5. Ethics
6. Statistical Analysis
7. Results
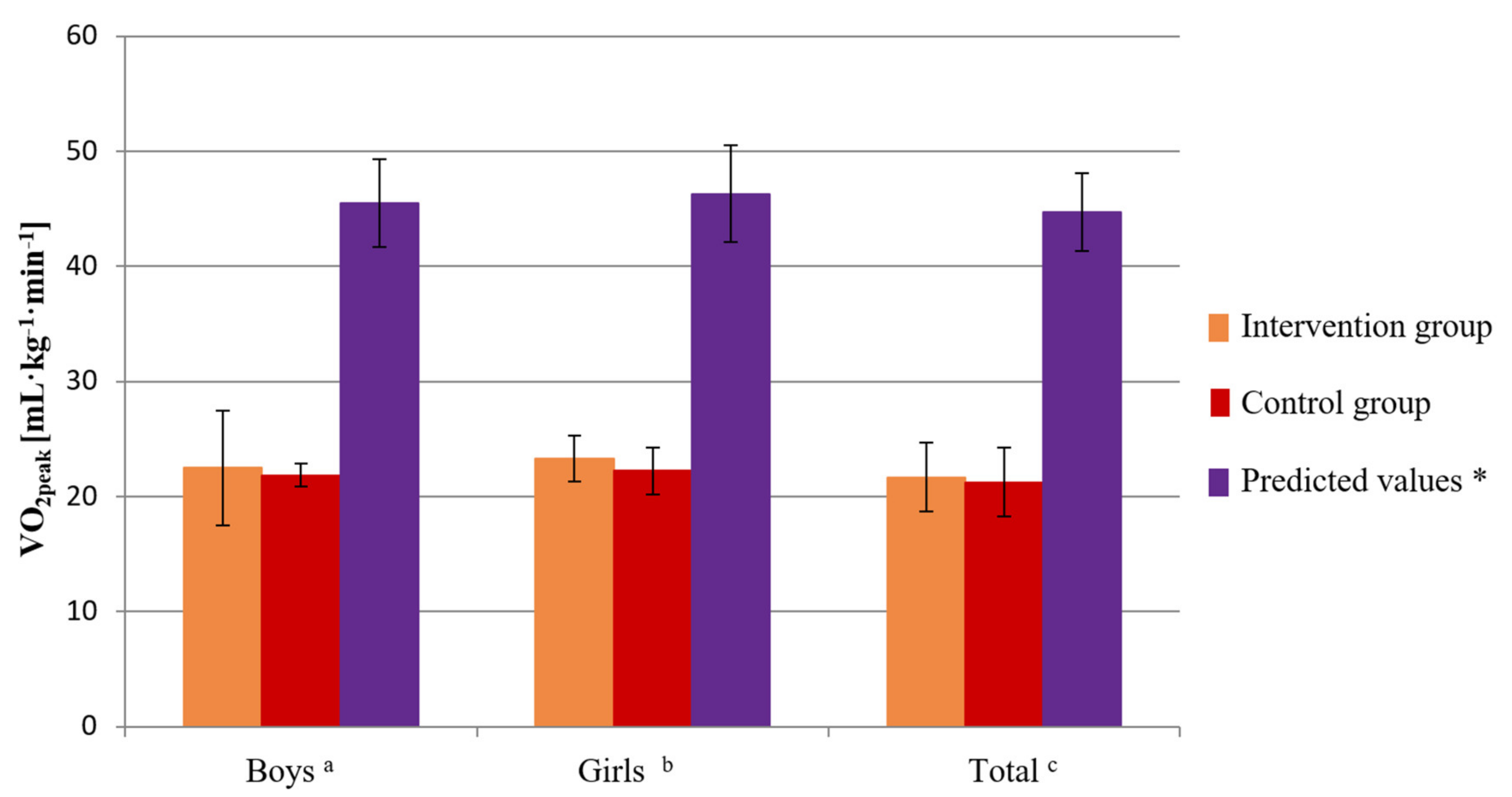
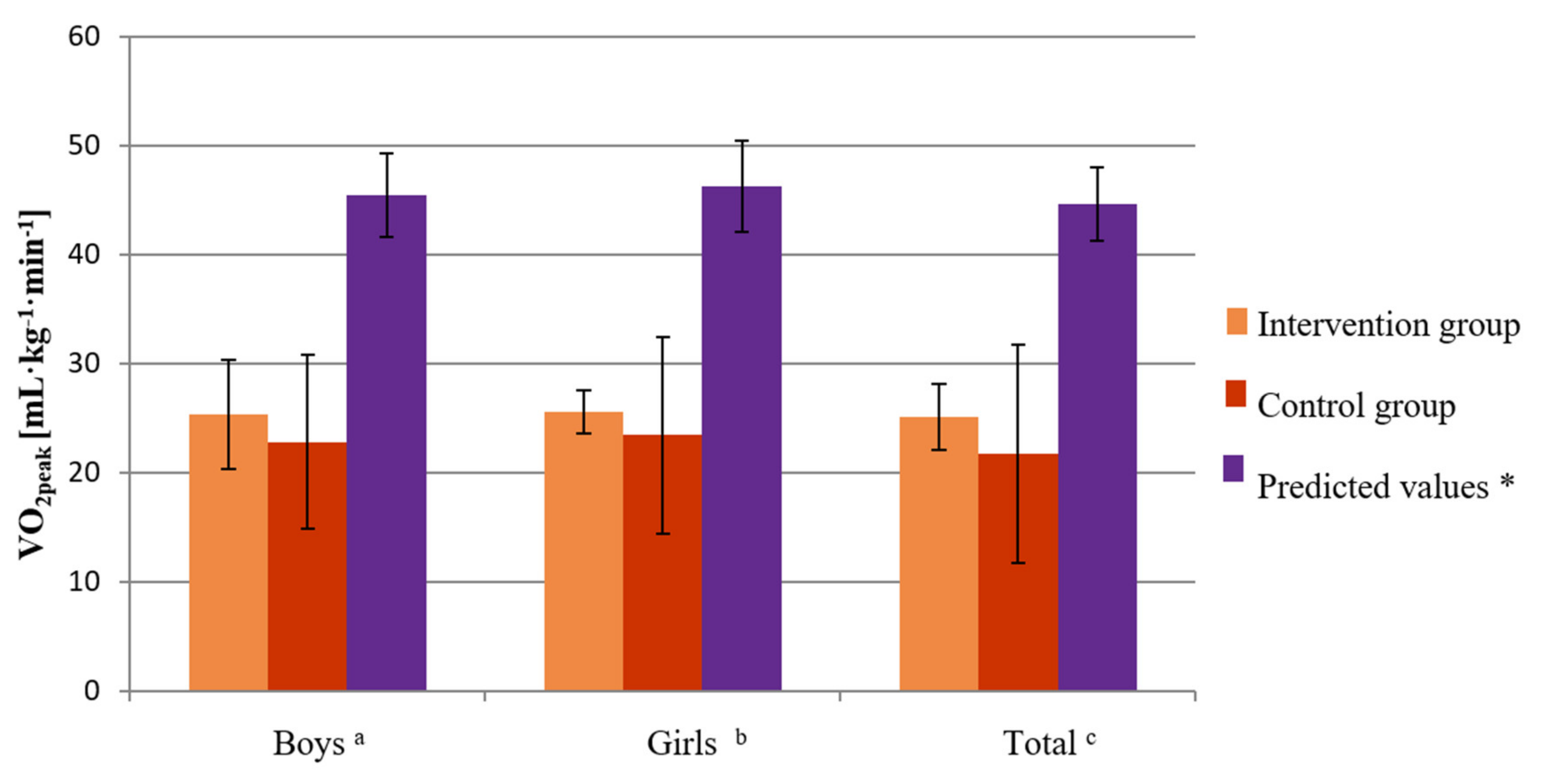
7.1. Cardiorespiratory Fitness before the IVGs Intervention—CPET Results
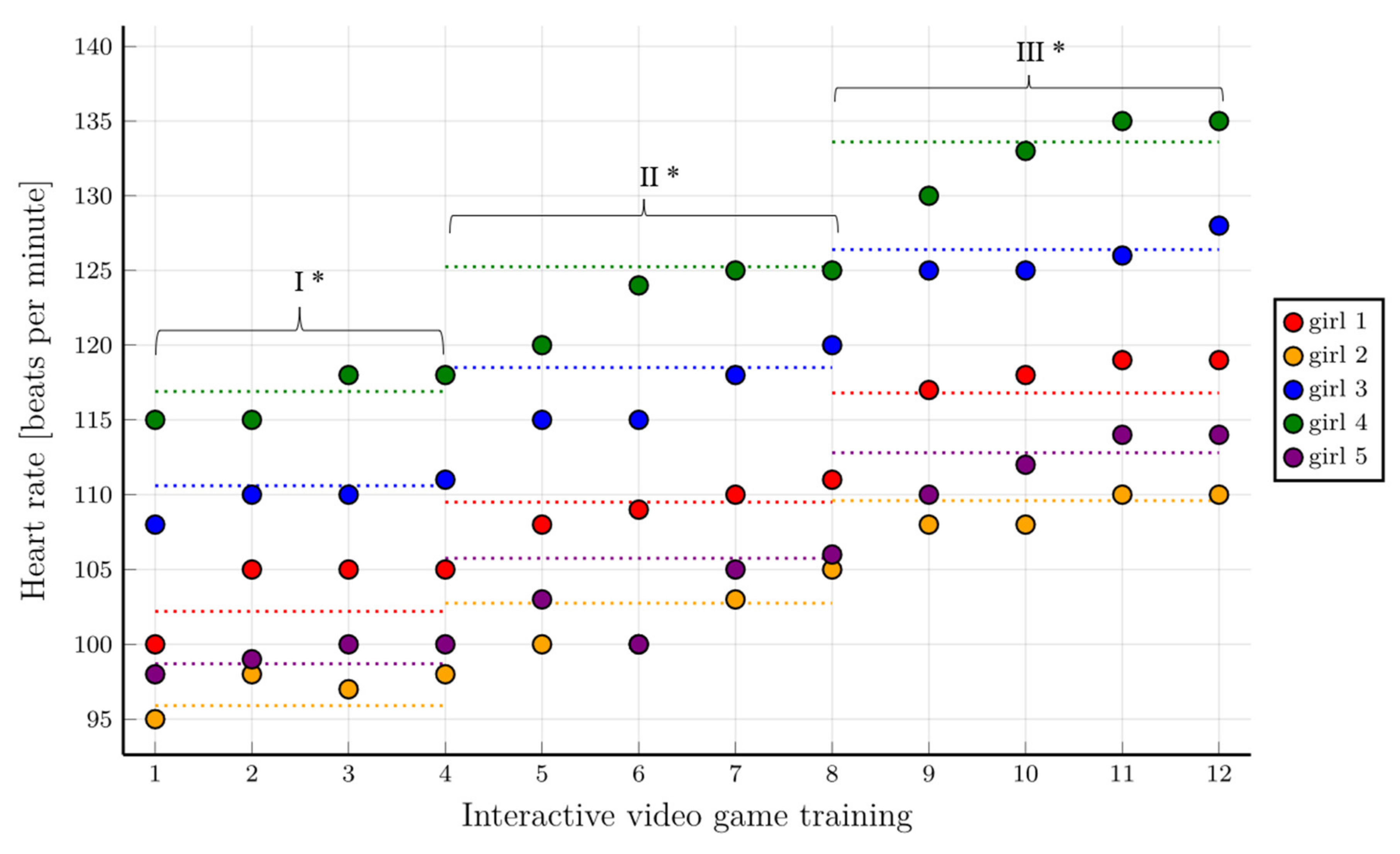
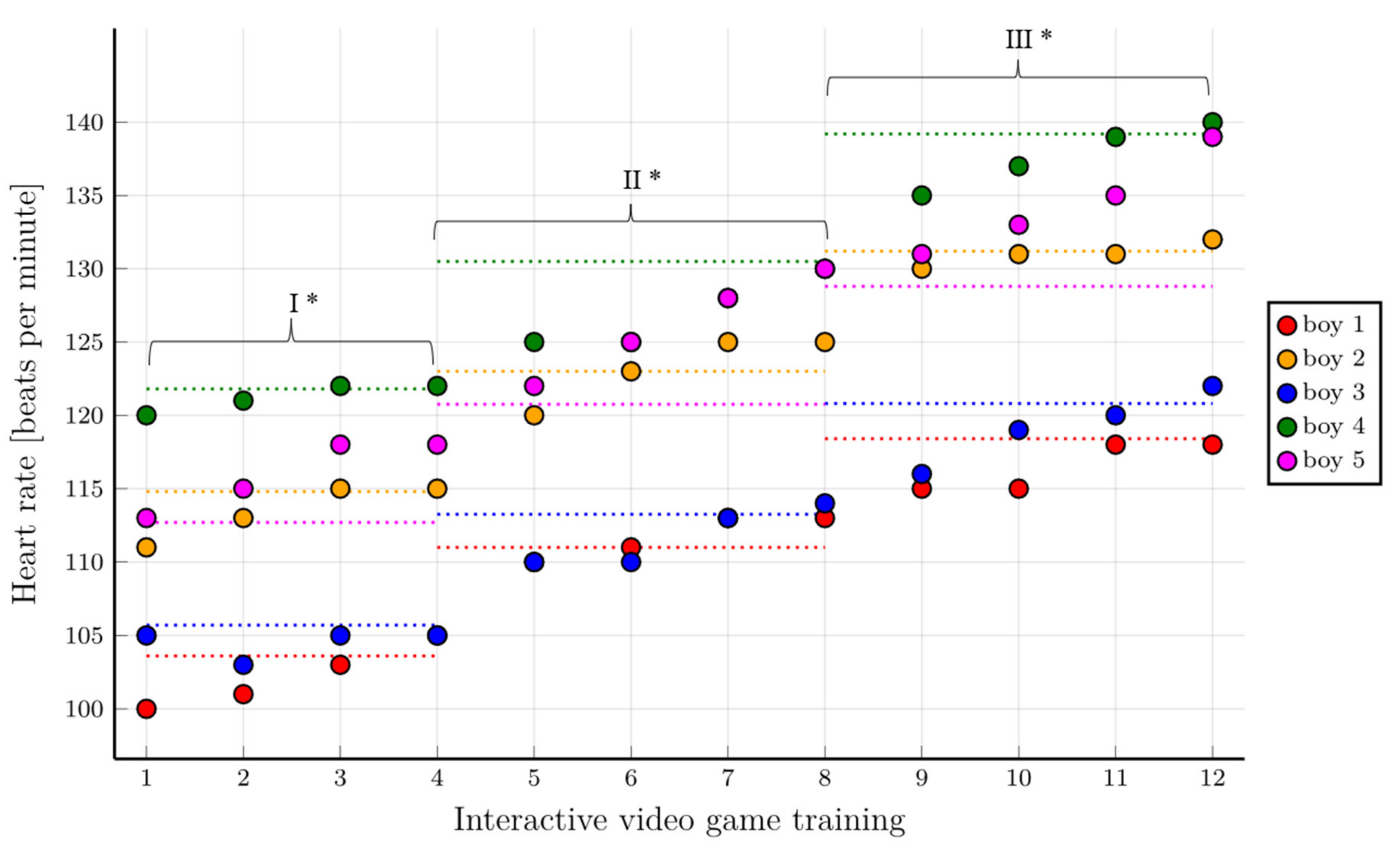
7.2. Assessment of the Feasibility of Training with IVGs in the Intervention Group
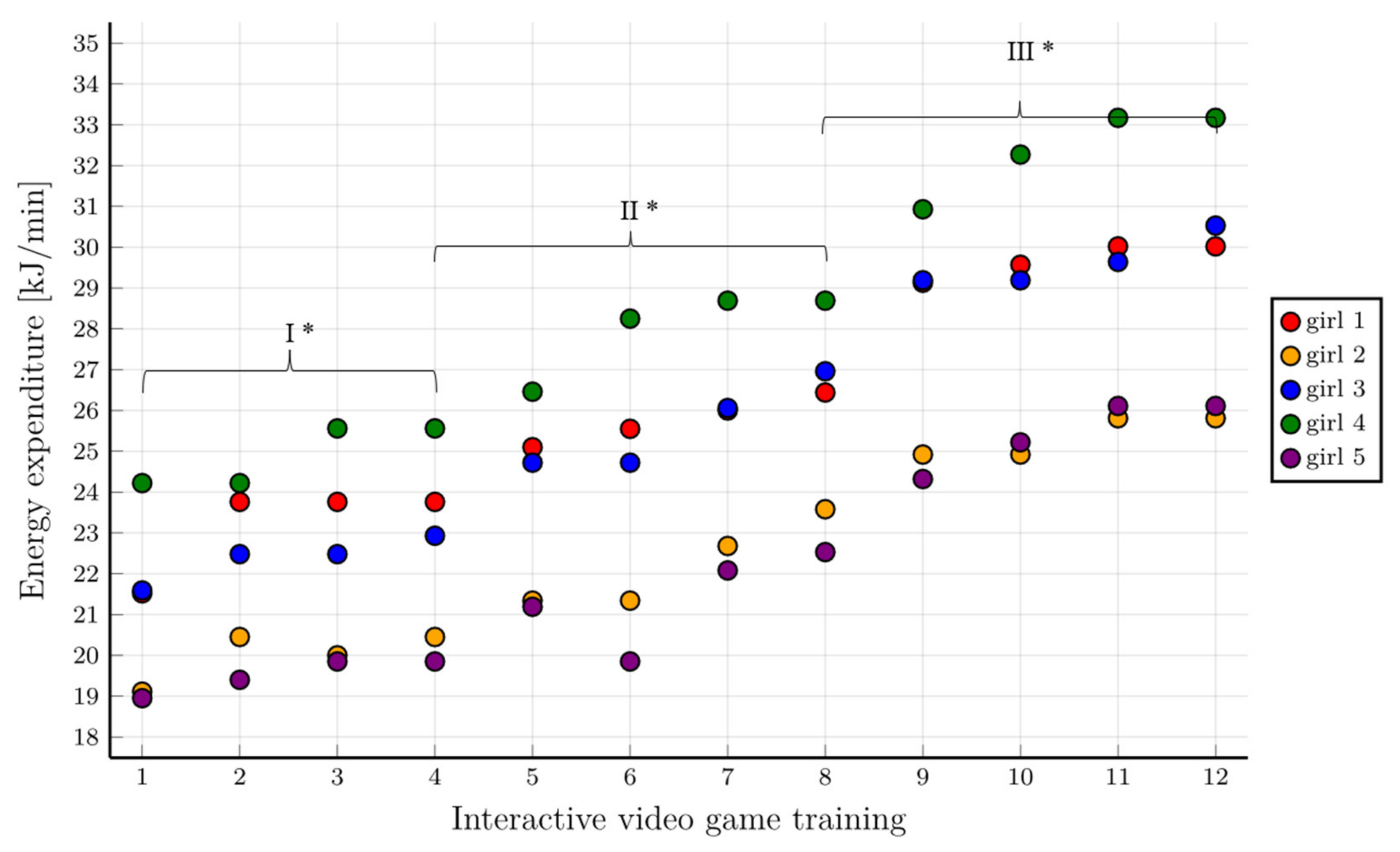
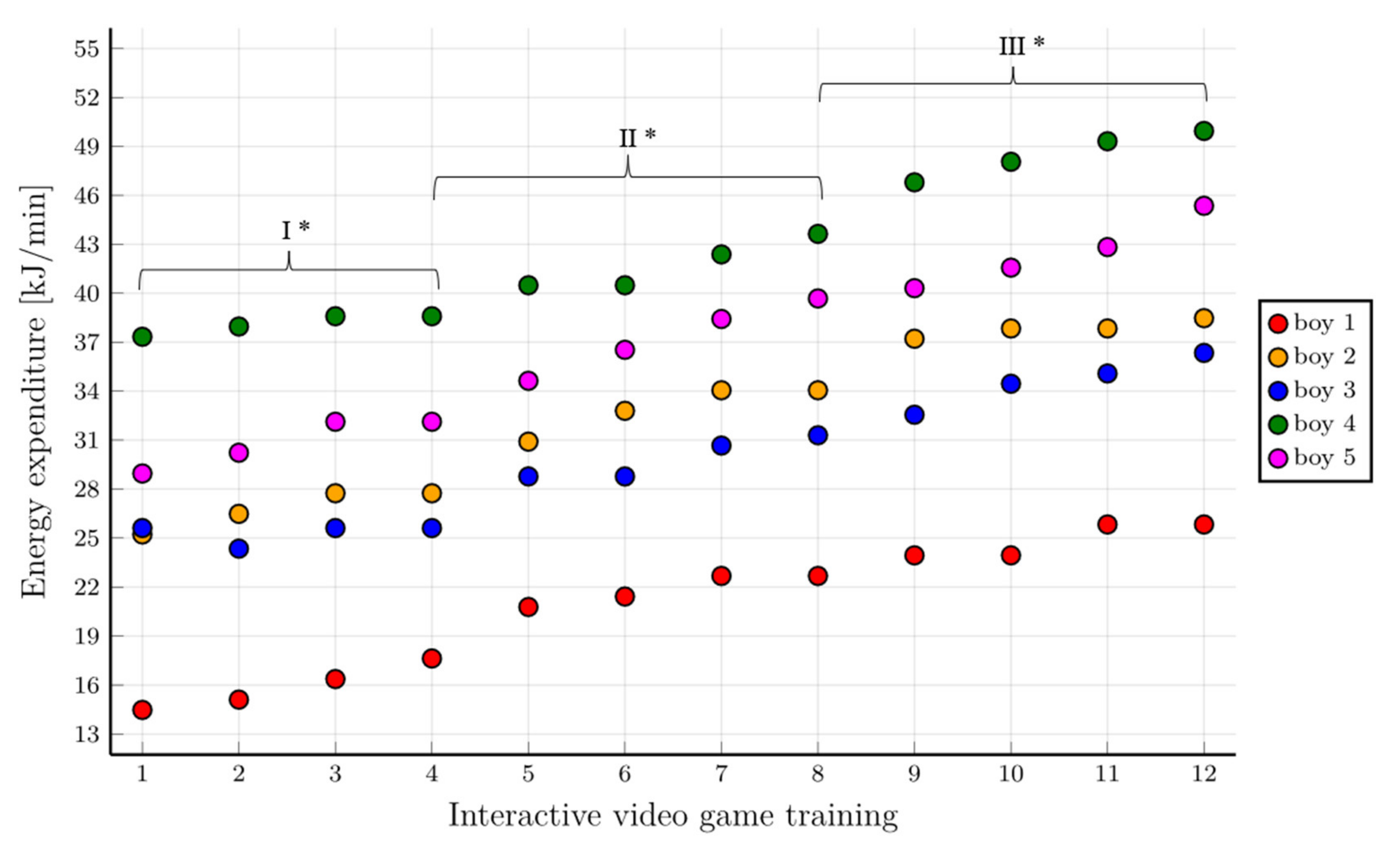
7.3. Assessment of Energy Expenditure during Training with the Use of IVGs
7.4. Cardiorespiratory Fitness after 14 Months following the IVGs Intervention—CPET Results
7.5. Level of Physical Activity Immediately after the IVGs Intervention and in the Follow-Up Study
8. Discussion
9. Strengths and Limitations of This Study
10. Future Research Directions
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Noone, A.M.; Howlader, N.; Krapcho, M.; Miller, D.; Brest, A.; Yu, M.; Ruhl, J.; Tatalovich, Z.; Mariotto, A.; Lewis, D.R.; et al. SEER Cancer Statistics Review, 1975–2015; National Cancer Institute: Bethesda, MD, USA, 2018. Available online: https://seer.cancer.gov/csr/1975_2015/ (accessed on 21 March 2022).
- Gatta, G.; Botta, L.; Rossi, S.; Aareleid, T.; Bielska-Lasota, M.; Clavel, J.; Dimitrova, N.; Jakab, Z.; Kaatsch, P.; Lacour, B.; et al. Childhood cancer survival in Europe 1999–2007: Results of EUROCARE-5—a population-based study. Lancet Oncol. 2014, 15, 35–47. [Google Scholar] [CrossRef]
- Enskär, K.; von Essen, L. Physical problems and psychosocial function in children with cancer. Nurs Child. Young People 2008, 20, 37–41. [Google Scholar] [CrossRef]
- Thorsteinsson, T.; Larsen, H.B.; Schmiegelow, K.; Thing, L.F.; Krustrup, P.; Pedersen, M.T.; Christensen, K.B.; Mogensen, P.R.; Helms, A.S.; Andersen, L.B. Cardiorespiratory fitness and physical function in children with cancer from diagnosis throughout treatment. BMJ Open Sport Exerc. Med. 2017, 3, e000179. [Google Scholar] [CrossRef]
- Miller, E.; Jacob, E.; Hockenberry, M.J. Nausea, Pain, Fatigue, and Multiple Symptoms in Hospitalized Children with Cancer. Oncol. Nurs. Forum 2011, 38, E382–E393. [Google Scholar] [CrossRef] [PubMed]
- Nunes, M.D.R.; Jacob, E.; Bomfim, E.O.; Lopes-Junior, L.C.; de Lima, R.A.G.; Floria-Santos, M.; Nascimento, L.C. Fatigue and health related quality of life in children and adolescents with cancer. Eur. J. Oncol. Nurs. 2017, 29, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Kabak, V.Y.; Calders, P.; Duger, T.; Mohammed, J.; Van Breda, E. Short and long-term impairments of cardiopulmonary fitness level in previous childhood cancer cases: A systematic review. Support. Care Cancer 2018, 27, 69–86. [Google Scholar] [CrossRef] [PubMed]
- Berkman, A.; Lakoski, S.G. A Review of Cardiorespiratory Fitness in Adolescent and Young Adult Survivors of Childhood Cancer: Factors that Affect its Decline and Opportunities for Intervention. J. Adolesc. Young Adult Oncol. 2016, 5, 8–15. [Google Scholar] [CrossRef]
- Perdikaris, P.; Merkouris, A.; Patiraki, E.; Tsoumakas, K.; Vasilatou-Kosmidis, E.; Matziou, V. Evaluating cancer related fatigue during treatment according to children’s, adolescents’ and parents’ perspectives in a sample of Greek young patients. Eur. J. Oncol. Nurs. 2009, 13, 399–408. [Google Scholar] [CrossRef]
- Morales, J.S.; Valenzuela, P.L.; Rincon, C.; Takken, T.; Fiuza-Luces, C.; Santos-Lozano, A.; Lucia, A. Exercise training in childhood cancer: A systematic review and meta-analysis of randomized controlled trials. Cancer Treat. Rev. 2018, 70, 154–167. [Google Scholar] [CrossRef]
- Braam, K.I.; van der Torre, P.; Takken, T.; Veening, M.A.; van Dulmen-den Broeder, E.; Kaspers, G.J.L. Physical exercise training interventions for children and young adults during and after treatment for childhood cancer. Cochrane Database Syst. Rev. 2016, 3, CD008796. [Google Scholar] [CrossRef]
- Fiuza-Luces, C.; Padilla, J.R.; Soares-Miranda, L.; Santana-Sosa, E.; Quiroga, J.V.; Santos-Lozano, A.; Pareja-Galeano, H.; Sanchis-Gomar, F.; Lorenzo-Gonzalez, R.; Verde, Z.; et al. Exercise Intervention in Pediatric Patients with Solid Tumors: The Physical Activity in Pediatric Cancer Trial. Med. Sci. Sports Exerc. 2017, 49, 223–230. [Google Scholar] [CrossRef]
- Doyle, C.; Kushi, L.H.; Byers, T.; Courneya, K.S.; Demark-Wahnefried, W.; Grant, B.; McTiernan, A.; Rock, C.L.; Thompson, C.; Gansler, T.; et al. Nutrition and Physical Activity During and After Cancer Treatment: An American Cancer Society Guide for Informed Choices. CA Cancer J. Clin. 2006, 56, 323–353. [Google Scholar] [CrossRef] [PubMed]
- Rehorst-Kleinlugtenbelt, L.B.; Bekkering, W.P.; van der Torre, P.; van der Net, J.; Takken, T. Physical activity level objectively measured by accelerometery in children undergoing cancer treatment at home and in a hospital setting: A pilot study. Pediatr. Hematol. Oncol. J. 2019, 4, 82–88. [Google Scholar] [CrossRef]
- Kauhanen, L.; Järvelä, L.; Lähteenmäki, P.M.; Arola, M.; Heinonen, O.J.; Axelin, A.; Lilius, J.; Vahlberg, T.; Salanterä, S. Active video games to promote physical activity in children with cancer: A randomized clinical trial with follow-up. BMC Pediatr. 2014, 14, 1–10. [Google Scholar] [CrossRef]
- Liang, Y.; Lau, P. Effects of Active Videogames on Physical Activity and Related Outcomes Among Healthy Children: A Systematic Review. Games Health J. 2014, 3, 122–144. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.; Irwin, J. Active video games to promote physical activity in children and youth: A systematic review. Arch. Pediatr. Adolesc. Med. 2010, 164, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Guy, S.; Ratzki-Leewing, A.; Gwadry-Sridhar, F. Moving Beyond the Stigma: Systematic Review of Video Games and Their Potential to Combat Obesity. Int. J. Hypertens. 2011, 2011, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lu, A.S.; Kharrazi, H.; Gharghabi, F.; Thompson, D. A Systematic Review of Health Videogames on Childhood Obesity Prevention and Intervention. Games Health J. 2013, 2, 131–141. [Google Scholar] [CrossRef]
- Oliveira, C.B.; Pinto, R.Z.; Saraiva, B.T.C.; Tebar, W.R.; Delfino, L.D.; Franco, M.R.; Silva, C.C.M.; Christofaro, D.G.D. Effects of active video games on children and adolescents: A systematic review with meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 4–12. [Google Scholar] [CrossRef]
- Vázquez, F.L.; Otero, P.; García-Casal, J.A.; Blanco, V.; Torres, J.; Arrojo, M. Efficacy of video game-based interventions for active aging. A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208192. [Google Scholar] [CrossRef]
- Page, Z.E.; Barrington, S.; Edwards, J.; Barnett, L.M. Do active video games benefit the motor skill development of non-typically developing children and adolescents: A systematic review. J. Sci. Med. Sport 2017, 20, 1087–1100. [Google Scholar] [CrossRef] [PubMed]
- Howcroft, J.; Klejman, S.; Fehlings, D.; Wright, F.V.; Zabjek, K.; Andrysek, J.; Biddiss, E. Active Video Game Play in Children with Cerebral Palsy: Potential for Physical Activity Promotion and Rehabilitation Therapies. Arch. Phys. Med. Rehabil. 2012, 93, 1448–1456. [Google Scholar] [CrossRef]
- Hsiao, L.; Huang, W.; Hsu, T.; Lin, S.; Chen, H.; Wang, T. Development of a Kinect-based bilateral rehabilitation game for children with cerebral palsy. J. Neurol. Sci. 2017, 381, 191–192. [Google Scholar] [CrossRef]
- Andrysek, J.; Klejman, S.; Steinnagel, B.; Torres-Moreno, R.; Zabjek, K.F.; Salbach, N.M.; Moody, K. Preliminary Evaluation of a Commercially Available Videogame System as an Adjunct Therapeutic Intervention for Improving Balance Among Children and Adolescents WITH Lower Limb Amputations. Arch. Phys. Med. Rehabil. 2012, 93, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Hamari, L.; Järvelä, L.S.; Lähteenmäki, P.M.; Arola, M.; Axelin, A.; Vahlberg, T.; Salanterä, S. The effect of an active video game intervention on physical activity, motor performance, and fatigue in children with cancer: A randomized controlled trial. BMC Res. Notes 2019, 12, 1–7. [Google Scholar] [CrossRef] [PubMed]
- International Collaborative Treatment Protocol for Children and Adolescents with Acute Lymphoblastic Leukemia. Available online: https://www.gpoh.de/kinderkrebsinfo/content/health_professionals/clinical_trials/pohkinderkrebsinfotherapiestudien/aieop_bfm_all_2017/index_eng.html (accessed on 21 March 2022).
- Schweitzer, J.; Zimmermann, M.; Rasche, M.; Von Neuhoff, C.; Creutzig, U.; Dworzak, M.; Reinhardt, D.; Klusmann, J.-H. Improved outcome of pediatric patients with acute megakaryoblastic leukemia in the AML-BFM 04 trial. Ann. Hematol. 2015, 94, 1327–1336. [Google Scholar] [CrossRef]
- Van Brussel, M.; Bongers, B.C.; Hulzebos, E.H.J.; Burghard, M.; Takken, T. A Systematic Approach to Interpreting the Cardio-pulmonary Exercise Test in Pediatrics. Pediatr. Exerc. Sci. 2019, 31, 194–203. [Google Scholar] [CrossRef]
- American Thoracic Society. American College of Chest Physicians ATS/ACCP Statement on Cardiopulmonary Exercise Testing. Am. J. Respir. Crit. Care Med. 2003, 167, 211–277. [Google Scholar] [CrossRef]
- Godfrey, S. Methods of measuring the response to exercise in children. In Applications in Health and Disease; Godfrey, S., Ed.; Exercise Testing in Children; W.B. Saunders Company Ltd.: London, UK, 1974; pp. 12–41. [Google Scholar]
- Kowaluk, A.; Woźniewski, M. Peak Oxygen Uptake and Exercise Capacity of Children Undergoing Leukemia Treatment. Int. J. Environ. Res. Public Health 2020, 17, 8732. [Google Scholar] [CrossRef]
- Bongers, B.C.; van Brussel, M.; Hulzebos, H.J.; Takken, T. Paediatric exercise testing in clinics and classrooms: A comparative review of different assessments. OA Epidemiol. 2013, 1, 1–12. [Google Scholar] [CrossRef][Green Version]
- Zaqout, M.; Vyncke, K.; Moreno, L.A.; De Miguel-Etayo, P.; Lauria, F.; Molnar, D.; Lissner, L.; Hunsberger, M.; Veidebaum, T.; Tornaritis, M.; et al. Determinant factors of physical fitness in European children. Int. J. Public Health 2016, 61, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Marinov, B.; Mandadjieva, S.; Kostianev, S. Pictorial and verbal category-ratio scales for effort estimation in children. Child. Care Health Dev. 2008, 34, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Chung, P.K.; Leung, R.Y.H.; Liu, J.D.; Quach, B.; Zhao, Y. Exercise regulation during cycle ergometry using Cantonese version of the CERT and Borg’s RPE. J. Phys. Educ. Sport 2013, 13, 170–176. [Google Scholar]
- Keytel, L.R.; Goedecke, J.; Noakes, T.D.; Hiiloskorpi, H.; Laukkanen, R.; van der Merwe, L.; Lambert, E. Prediction of energy expenditure from heart rate monitoring during submaximal exercise. J. Sports Sci. 2005, 23, 289–297. [Google Scholar] [CrossRef]
- Hui, S.S.C.; Chan, J.W.S. The relationship between heart rate reserve and oxygen uptake reserve in children and adolescents. Res. Q. Exerc. Sport 2006, 77, 41–49. [Google Scholar] [CrossRef]
- Ross, W.L.; Le, A.; Zheng, D.J.; Mitchell, H.-R.; Rotatori, J.; Li, F.; Fahey, J.T.; Ness, K.K.; Kadan-Lottick, N.S. Physical activity barriers, preferences, and beliefs in childhood cancer patients. Support. Care Cancer 2018, 26, 2177–2184. [Google Scholar] [CrossRef]
- Mossé, Y.P.; Lim, M.; Voss, S.D.; Wilner, K.; Ruffner, K.; Laliberte, J.; Rolland, D.; Balis, F.; Maris, J.M.; Weigel, B.J.; et al. Safety and activity of crizotinib for paediatric patients with refractory solid tumours or anaplastic large-cell lymphoma: A Children’s Oncology Group phase 1 consortium study. Lancet Oncol. 2013, 14, 472–480. [Google Scholar] [CrossRef]
- Gavotto, A.; Huguet, H.; Picot, M.-C.; Guillaumont, S.; Matecki, S.; Amedro, P. The V̇e/V̇co2 slope: A useful tool to evaluate the physiological status of children with congenital heart disease. J. Appl. Physiol. 2020, 129, 1102–1110. [Google Scholar] [CrossRef]
- Bansal, N.; Amdani, S.; Lipshultz, E.R.; Lipshultz, S.E. Chemotherapy-induced cardiotoxicity in children. Expert Opin. Drug Metab. Toxicol. 2017, 13, 817–832. [Google Scholar] [CrossRef]
- Huang, T.-T.; Ness, K.K. Exercise Interventions in Children with Cancer: A Review. Int. J. Pediatr. 2011, 2011, 1–11. [Google Scholar] [CrossRef]
- Graves, L.; Ridgers, N.; Williams, K.; Stratton, G.; Atkinson, G.; Cable, N. The Physiological Cost and Enjoyment of Wii Fit in Adolescents, Young Adults, and Older Adults. J. Phys. Act. Health 2010, 7, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Fazelniya, Z.; Najafi, M.; Moafi, A.; Talakoub, S. The impact of an interactive computer game on the quality of life of children undergoing chemotherapy. Iran. J. Nurs. Midwifery Res. 2017, 22, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Winter, C.; Müller, C.; Hoffmann, C.; Boos, J.; Rosenbaum, D. Physical activity and childhood cancer. Pediatr. Blood Cancer 2009, 54, 501–510. [Google Scholar] [CrossRef]
- Ghazisaeidi, M.; Safdari, R.; Goodini, A.; Mirzaiee, M.; Farzi, J. Digital games as an effective approach for cancer management: Opportunities and challenges. J. Educ. Health Promot. 2017, 6, 30. [Google Scholar] [CrossRef]
- González-González, C.S.; Toledo-Delgado, P.A.; Muñoz-Cruz, V.; Torres-Carrion, P.V. Serious games for rehabilitation: Gestural interaction in personalized gamified exercises through a recommender system. J. Biomed. Inform. 2019, 97, 103266. [Google Scholar] [CrossRef] [PubMed]
- Barnett, A.; Cerin, E.; Baranowski, T. Active Video Games for Youth: A Systematic Review. J. Phys. Act. Health 2011, 8, 724–737. [Google Scholar] [CrossRef] [PubMed]
- White, J.; Flohr, J.A.; Winter, S.S.; Vener, J.; Feinauer, L.R.; Ransdell, L.B. Potential benefits of physical activity for children with acute lymphoblastic leukaemia. Pediatr. Rehabil. 2005, 8, 53–58. [Google Scholar] [CrossRef]
- Baranowski, T.; Abdelsamad, D.; Baranowski, J.; O’Connor, T.M.; Thompson, D.; Barnett, A.; Cerin, E.; Chen, T.-A. Impact of an Active Video Game on Healthy Children’s Physical Activity. Pediatrics 2012, 129, e636–e642. [Google Scholar] [CrossRef]
- Chung, J.O.K.; Li, W.H.C.; Cheung, A.T.; Ho, L.L.K.; Xia, W.; Chan, G.C.F.; Lopez, V. Relationships among resilience, depressive symptoms, self-esteem, and quality of life in children with cancer. Psychooncology 2021, 30, 194–201. [Google Scholar] [CrossRef]
- Liu, R.D.; Chinapaw, M.J.; Huijgens, P.C.; van Mechelen, W. Physical exercise interventions in haematological cancer patients, feasible to conduct but effectiveness to be established: A systematic literature review. Cancer Treat. Rev. 2009, 35, 185–192. [Google Scholar] [CrossRef]

| Intervention Group n = 10 | Control Group n = 11 | p-Values Intervention Group vs. Control Group | |||||
|---|---|---|---|---|---|---|---|
| Determinant Variables | Mean ± SD | Boys Mean ± SD n = 5 | Girls Mean ± SD n = 5 | Mean ± SD | Boys Mean ± SD n = 7 | Girls Mean ± SD n = 4 | |
| Age (years) | 11.3 ± 1.9 | 11.4 ± 2.2 | 11.2 ± 2.0 | 10.08 ± 1.9 | 10.15 ± 2.0 | 9.9 ± 2.2 | 0.38 |
| Height (cm) | 149.1 ± 13.76 | 154 ± 15.36 | 144.2 ± 11.39 | 140 ± 16.5 | 141.7 ± 18.42 | 137 ± 14.51 | 0.51 |
| Weight (kg) | 46.59 ± 16.01 | 49.6 ± 17.8 | 43.5 ± 15.4 | 36.45 ± 9.9 | 36.57 ± 10.86 | 36.25 ± 9.43 | 0.24 |
| Treatment Duration (months) | 6.4 ± 1.6 | 6.0 ± 2.0 | 6.8 ± 1.3 | 6.3 ± 1.7 | 6.4 ± 2.1 | 6.0 ± 1.15 | 0.87 |
| HGB (mg/dL) | 8.35 ± 0.2 | 8.44 ± 0.15 | 8.26 ± 0.18 | 8.33 ± 0.17 | 8.24 ± 0.15 | 8.47 ± 0.12 | 0.78 |
| PLT (G/L) | 173.9 ± 57.26 | 162.6 ± 60.97 | 185.2 ± 57.8 | 142.3 ± 72.6 | 116.7 ± 76.78 | 187 ± 40.11 | 0.28 |
| RBC (T/L) | 3.143 ± 0.36 | 3.0 ± 0.29 | 3.29 ± 0.4 | 3.52 ± 0.29 | 3.46 ± 0.3 | 3.62 ± 0.22 | 0.02 |
| WBC (G/L) | 1.91 ± 0.8 | 2.16 ± 0.9 | 1.67 ± 0.57 | 2.27 ± 1.1 | 2.39 ± 1.42 | 2.06 ± 0.31 | 0.92 |
| HR at rest | 86.5 ± 3.4 | 86.2 ± 4.2 | 86.8 ± 2.9 | 84.9 ± 4.16 | 85.1 ± 4.95 | 84.5 ± 2.89 | 0.35 |
| Level of Difficulty | IVG Session Number | Game Type | Game Duration/Break Duration in Each Session |
|---|---|---|---|
| First level—70% HRpeak | 1–4 | Beach volleyball | 5 min/1 min |
| Tennis | 5 min/1 min | ||
| River rush | 5 min/1 min | ||
| Reflex ridge | 5 min/end of the game | ||
| Second level—75% HRpeak | 5–8 | Beach volleyball | 5 min/1 min |
| Tennis | 5 min/1 min | ||
| River rush | 5 min/1 min | ||
| Reflex ridge | 5 min/end of the game | ||
| Third level—80% HRpeak | 9–12 | Beach volleyball | 5 min/1 min |
| Tennis | 5 min/1 min | ||
| River rush | 5 min/1 min | ||
| Reflex ridge | 5 min/end of the game |
| Intervention Group n = 10 | Control Group n = 11 | p-Values Intervention Group vs. Control Group | |||||
|---|---|---|---|---|---|---|---|
| Outcome Variables | Mean ± SD | Boys Mean ± SD n = 5 | Girls Mean ± SD n = 5 | Mean ± SD | Boys Mean ± SD n = 7 | Girls Mean ± SD n = 4 | |
| VO2peak (mL kg−1 min−1) | 22.5 ± 2.6 | 23.3 ± 2.7 | 21.69 ± 2.5 | 21.86 ± 2.44 | 22.22 ± 2.8 | 21.24 ± 1.9 | 0.57 |
| HRpeak | 154.7 ± 12 | 159.6 ± 10.45 | 149.8 ± 12.4 | 149.5 ± 10.0 | 143.1 ± 5.8 | 160.8 ± 1.7 | 0.30 |
| VO2 (mL/min) | 1068 ± 395.6 | 1247 ± 329.3 | 888. 4 ± 404.1 | 1228 ± 251.9 | 1241 ± 292.1 | 1205 ± 199.6 | 0.29 |
| VCO2 (mL/min) | 1069 ± 517.8 | 1269 ± 495.6 | 868.2 ± 507.3 | 1179 ± 403.9 | 1284 ± 479.1 | 995.8 ± 119.9 | 0.59 |
| VE (L/min) | 28.33 ± 9.4 | 31.22 ± 6.5 | 25.44 ± 11.7 | 29.47 ± 6.0 | 30.13 ± 6.8 | 28.33 ± 4.9 | 0.75 |
| VE/VCO2 | 28.74 ± 6.02 | 26.18 ± 5.1 | 31.31 ± 6.3 | 26.8 ± 3.9 | 25.91 ± 4.5 | 28.35 ± 2.2 | 0.4 |
| RQ = VCO2exhaled /VO2uptake | 0.97 ± 0.14 | 0.99 ± 0.16 | 0.94 ± 0.15 | 0.95 ± 0.2 | 1.0 ± 0.2 | 0.8 ± 0.06 | 0.93 |
| MET | 6.38 ± 0.7 | 6.62 ± 0.8 | 6.14 ± 0.7 | 6.2 ± 0.7 | 6.3 ± 0.8 | 6.0 ± 0.5 | 0.53 |
| Test Duration (s) | 481.1 ± 35.5 | 474.4 ± 41.1 | 487.8 ± 32.3 | 461.2 ± 32.7 | 469.4 ± 37.7 | 446.8 ± 17.2 | 0.95 |
| EEtest I | EEtest II | EE1 | EE2 | EE3 | EE4 | EE5 | EE6 | EE7 | EE8 | EE9 | EE10 | EE11 | EE12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention group | ||||||||||||||
| Mean (kJ/min) | 49.83 | 54.59 | 23.7 | 24.44 | 25.21 | 25.42 | 27.44 | 27.97 | 29.37 | 29.95 | 31.93 | 32.7 | 33.57 | 34.16 |
| Std. Deviation (kJ/min) | 10.85 | 12.26 | 6.30 | 6.26 | 6.47 | 6.23 | 6.41 | 6.86 | 6.99 | 7.24 | 7.50 | 7.88 | 7.88 | 8.39 |
| Girls | ||||||||||||||
| Mean (kJ/min) | 41.92 | 45.22 | 21.08 | 22.06 | 22.33 | 22.51 | 23.76 | 23.94 | 25.1 | 25.64 | 27.7 | 28.23 | 28.95 | 29.13 |
| Std. Deviation (kJ/min) | 4.04 | 3.97 | 2.16 | 2.09 | 2.45 | 2.36 | 2.37 | 3.36 | 2.72 | 2.53 | 2.91 | 3.12 | 3.06 | 3.13 |
| Boys | ||||||||||||||
| Mean (kJ/min) | 57.74 | 63.96 | 26.32 | 26.82 | 28.09 | 28.34 | 31.11 | 32.0 | 33.64 | 34.27 | 36.16 | 37.17 | 38.18 | 39.19 |
| Std. Deviation (kJ/min) | 9.59 | 10.16 | 8.22 | 8.35 | 8.22 | 7.78 | 7.29 | 7.34 | 7.56 | 8.07 | 8.57 | 8.96 | 8.77 | 9.23 |
| p-Values boys vs. girls | 0.02 * | 0.01 * | 0.23 | 0.28 | 0.2 | 0.17 | 0.09 | 0.07 | 0.06 | 0.07 | 0.09 | 0.09 | 0.08 | 0.07 |
| Intervention Group n = 10 | Control Group n = 11 | p-Values Intervention Group vs. Control Group | |||||
|---|---|---|---|---|---|---|---|
| Outcome Variables | Mean ± SD | Boys Mean ± SD n = 5 | Girls Mean ± SD n = 5 | Mean ± SD | Boys Mean ± SD n = 7 | Girls Mean ± SD n = 4 | |
| VO2peak (mL kg−1 min−1) | 25.35 ± 2.3 | 25.59 ± 3.12 | 25.11 ± 1.4 | 22.84 ± 2.26 | 23.45 ± 2.24 | 21.78 ± 2.1 | 0.16 |
| HRpeak | 163.3 ± 13.2 | 168.8 ± 12.3 | 157.8 ± 12.8 | 147.5 ± 16.05 | 139.3 ± 11.04 | 162 ± 13.3 | 0.17 |
| VO2 (mL/min) | 797.3 ± 250.2 | 830.6 ± 354.3 | 764 ± 111.9 | 1101 ± 384.1 | 1196 ± 441.2 | 936 ± 212.4 | 0.81 |
| VCO2 (mL/min) | 739.3 ± 324.6 | 789 ± 454.1 | 689.6 ± 157.2 | 1025 ± 295.5 | 1088 ± 316.8 | 914.8 ± 254.7 | 0.77 |
| VE (L/min) | 32.86 ± 7.2 | 32.24 ± 10.0 | 33.48 ± 3.8 | 29.05 ± 7.12 | 27.74 ± 5.94 | 31.33 ± 9.3 | 0.88 |
| VE/VCO2 | 48.15 ± 14.17 | 45.16 ± 14.55 | 51.14 ± 14.8 | 29.16 ± 6.85 | 26.04 ± 2.4 | 34.63 ± 9.1 | 0.61 |
|
RQ = VCO2exhaled/ VO2uptake | 0.9 ± 0.08 | 0.92 ± 0.1 | 0.89 ± 0.07 | 0.95 ± 0.099 | 0.94 ± 0.10 | 0.97 ± 0.1 | 0.90 |
| MET | 7.2 ± 0.65 | 7.26 ± 0.9 | 7.14 ± 0.4 | 6.58 ± 0.78 | 6.82 ± 0.81 | 6.2 ± 0.6 | 0.41 |
| Test Duration (s) | 591.6 ± 97.8 | 608.4 ± 112.9 | 574.8 ± 90 | 432.9 ± 71.7 | 439.14 ± 78.12 | 421.98 ± 84 | 0.62 |
| VO2peak b (mL kg−1 min−1) | VO2 a (mL/min) | VCO2 a (mL/min) | VE b (L/min) | VE/VCO2 a | RQ = VCO2exhaled /VO2 uptake a | HRpeak b | MET b | Test Duration b (s) | |
|---|---|---|---|---|---|---|---|---|---|
| Mean Difference Between Pre- and Post-Intervention Results | 2.86 | −4.6 | −8.8 | 4.53 | 7.6 | −5.3 | 8.6 | 0.82 | 65.2 |
| p-Value | 0.02 * | 0.72 | 0.5 | 0.24 | 0.56 | 0.68 | 0.14 | 0.02 * | 0.03 * |
| HGB b | PLT b | RBC b | WBC b | ||||||
| Mean Difference Between Pre- and Post-Intervention Results | 4.66 | 87,1 | 1.30 | 10.42 | |||||
| p-Value | <0.0001 * | 0.0013 * | <0.0001 * | <0.0001 * |
| VO2peak b (mL kg−1 min−1) | VO2 b (mL/min) | VCO2 b (mL/min) | VE b (L/min) | VE/VCO2 a | RQ = VCO2exhaled/VO2uptake a | HRpeak b | MET b | Test Duration a (s) | |
|---|---|---|---|---|---|---|---|---|---|
| Mean Difference Between Pre- and Post-Intervention Results | 0.98 | −126.9 | −153.7 | 0.43 | 4.41 | 3.09 | −2 | 0.40 | 124.4 |
| p-Value | 0.34 | 0.37 | 0.32 | 0.88 | 0.91 | 0.94 | 0.73 | 0.21 | 0.005 * |
| HGB b | PLT b | RBC b | WBC a | ||||||
| Mean Difference Between Pre- and Post-Intervention Results | 4.34 | 161 | 0.68 | 80.09 | |||||
| p-Value | <0.0001 * | <0.0001 * | 0.0012 * | 0.049 * |
| Kruskal-Wallis Test | Physical Activity Level Immediately after the IVGs Intervention in Intervention Group vs. Control Group | |||||||
|---|---|---|---|---|---|---|---|---|
| HBSC 1 * | HBSC 2 * | HBSC 4.1 * | HBSC 4.2 * | HBSC 5.1 * | HBSC 5.2 * | HBSC 6.1 * | HBSC 6.2 * | |
| Difference Between Ranks | 281 | 361.5 | 123 | 87.53 | 127 | 159.9 | 83.27 | 146.3 |
| p-Value of Dunn’s Test | 0.0048 ** | 0.0003 ** | 0.22 | 0.38 | 0.20 | 0.11 | 0.40 | 0.14 |
| Physical Activity Level in Follow-Up Examination in Intervention Group vs. Control Group | ||||||||
| Difference Between Ranks | 194.4 | 130 | −63.49 | −142.7 | 1.50 | −72.93 | 65.4 | −10.97 |
| p-Value of Dunn’s Test | 0.12 | 0.28 | 0.6 | 0.24 | 0.99 | 0.54 | 0.59 | 0.93 |
| Wilcoxon’s Test | Physical Activity Level before IVGs Intervention vs. Immediately after the IVGs Intervention | |||||||
|---|---|---|---|---|---|---|---|---|
| HBSC 1 * | HBSC 2 * | HBSC 4.1 * | HBSC 4.2 * | HBSC 5.1 * | HBSC 5.2 * | HBSC 6.1 * | HBSC 6.2 * | |
| Median of Differences | 3 | 4 | 1.5 | 1 | 1 | 1.5 | 0.5 | 1.5 |
| p-Value Two Side Test | 0.002 ** | 0.002 ** | 0.0039 ** | 0.0469 ** | 0.0156 ** | 0.0078 ** | 0.0625 | 0.002 ** |
| Physical Activity Level Immediately after the IVGs Intervention vs. in Follow-Up Study after 14 Months | ||||||||
| Median of Differences | 0 | 0 | 2 | 3 | 2 | 2 | 1 | 1 |
| p-Value Two Side Test | >0.9999 | >0.9999 | 0.002 ** | 0.002 ** | 0.002 ** | 0.0039 ** | 0.0313 ** | 0.0156 ** |
| Wilcoxon’s Test | Physical Activity Level before Examination vs. after 1 Month in the Re-Examination Study | |||||||
|---|---|---|---|---|---|---|---|---|
| HBSC 1 * | HBSC 2 * | HBSC 4.1 * | HBSC 4.2 * | HBSC 5.1 * | HBSC 5.2 * | HBSC 6.1 * | HBSC 6.2 | |
| Median of Differences | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| p-Value Two Side Test | >0.9999 | >0.9999 | >0.9999 | >0.9999 | >0.9999 | 0.5 | >0.9999 | >0.9999 |
| Physical Activity Level Immediately after the IVGs Intervention vs. in Follow-Up Study after 14 Months | ||||||||
| Median of Differences | 1 | 3 | 3 | 3 | 4 | 3 | 2 | 2 |
| p-Value Two Side Test | 0.0039 ** | 0.001 ** | 0.001 ** | 0.001 ** | 0.001 ** | 0.001 ** | 0.002 ** | 0.001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowaluk, A.; Woźniewski, M. Interactive Video Games as a Method to Increase Physical Activity Levels in Children Treated for Leukemia. Healthcare 2022, 10, 692. https://doi.org/10.3390/healthcare10040692
Kowaluk A, Woźniewski M. Interactive Video Games as a Method to Increase Physical Activity Levels in Children Treated for Leukemia. Healthcare. 2022; 10(4):692. https://doi.org/10.3390/healthcare10040692
Chicago/Turabian StyleKowaluk, Aleksandra, and Marek Woźniewski. 2022. "Interactive Video Games as a Method to Increase Physical Activity Levels in Children Treated for Leukemia" Healthcare 10, no. 4: 692. https://doi.org/10.3390/healthcare10040692
APA StyleKowaluk, A., & Woźniewski, M. (2022). Interactive Video Games as a Method to Increase Physical Activity Levels in Children Treated for Leukemia. Healthcare, 10(4), 692. https://doi.org/10.3390/healthcare10040692






