Health and Mindfulness during the Syndemic of SARS-CoV-2: An Ethnographic Study
Abstract
:1. Introduction
The Syndemic in Spain
2. Related Work
2.1. Mindfulness: Holistic Vision of Health, Body and Mind-Body
2.2. Scientific Evidence and Configuration of the Imaginary
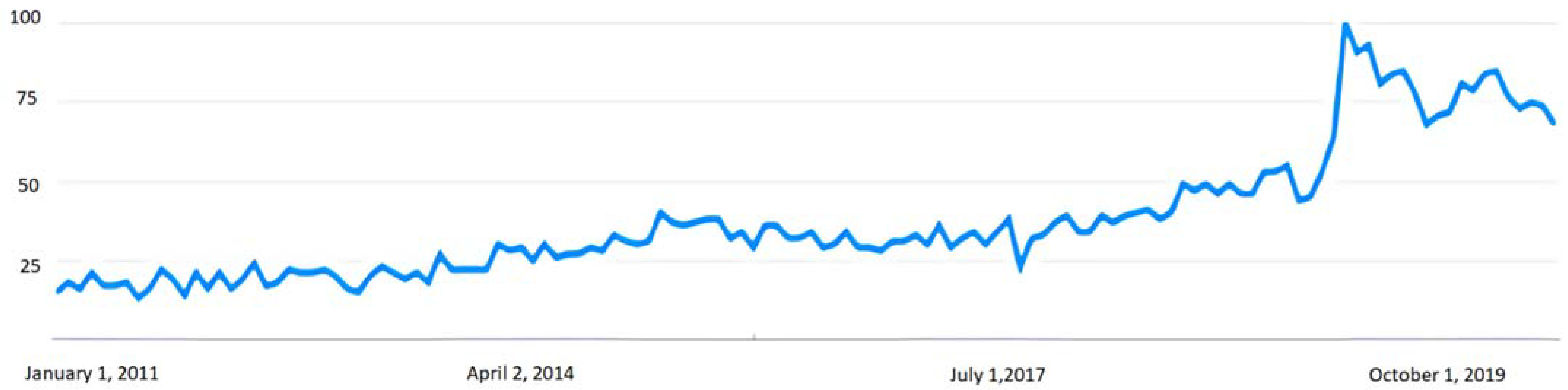
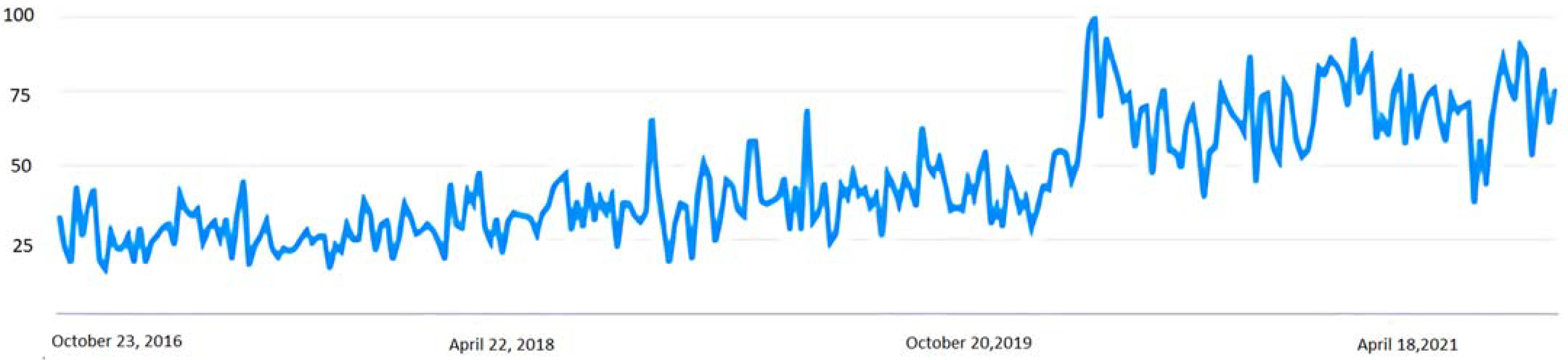
2.3. The Rise of Mindfulness during the Syndemic
3. Purpose of the Work
4. Materials and Methods
4.1. Participants and Procedures
4.2. Sociodemographic Characteristics of the Informants
5. Results
5.1. Health Impairment Due to Syndemic
“My social relationships have diminished, it has negatively affected my state of mind, my fears and insecurities have increased, it has removed me emotionally, and it has made me worse and better”.(male student, 40 years old, six years of experience)
“Well, I ended up with my self-esteem on the ground and with a lot of fear of what surrounds me”.(female student, 46 years old, one year of experience)
“I could say that this time of introspection and being alone with myself has been good for me”.(female student, 44 years old, five years of experience)
“It has provoked in me greater introspection, more interest in investigating myself and my relationship with my environment”.(female student, 50 years old, two years of experience)
“My case was different because when we saw that they were going to confine us, we moved to a house that we have in the mountains. So, it can be said that I spent it mostly outside where there was more or less normality, so it affected me little”.(female student, 43 years old, three years of experience)
“Confinement has not caused me any problems. I am aware that many people have been affected. But I have really handled it well, with acceptance and calm”.(Female student, 50 years old, five years of experience)
5.2. Motivation for the Practice of Mindfulness
“I tried it [mindfulness] for the first time in a meditation and transpersonal development workshop, and I continue to practice it until now. It all started with the search to alleviate that discomfort and negativity that consumed me in life at that time”.(male student, 40 years old, six years of experience)
“Mainly due to emotional discomfort derived from my work. On the other hand, as a way of acquiring tools and being able to apply them at work and with my family”.(female student, 39 years old, three years of experience)
“What was my main motivation for mindfulness? Well, in my case I resorted to mindfulness because of the need to know who I am”.(female student, 37 years old, two years of experience)
“I wanted to find my inner peace, because I was a roller coaster. I was absolutely afraid of everything, from the time I got up until I went to bed… I still have, there are times when I get up and say: “oh! I’m like a fear of something and I have to stop!”… Meditation has served me at a brutal level”(female student, 54 years old, seven years of experience)
5.3. Mindfulness and Health Improvement
“Greater knowledge of myself and my emotions, knowing and being aware of how I respond to stimuli, the reason for my behaviors in certain cases, tools to better respond to situations, and above all to be able to identify my state. It has also given me more coherence in my day-to-day life”.(female student, 39 years old, two years of experience)
“I have gone from crying without knowing why, to being sad, to being stressed, to not being able to sleep, to taking pills, I was taking I don’t know how many pills, the doctor told me: ‘You will never be able to get rid of this treatment’. … And I no longer take depression or sleeping pills, I sleep like a dormouse, I play sports, I feel good…”(female student, 54 years old, seven years of experience)
“Begin to live in a different way, with awareness of my life experience. A very large rupture of conceptual schemes linked to entrenched emotions, which have been the basis of my life until now. With a new vision, I take responsibility by breaking schemes and creating new ones, thereby beginning to create a new life experience. Begin to feel like owner, responsible and creator of my life”.(female student, 56 years old, one year of experience)
“Very radical changes can occur. My experience with people who have had oncological processes confirms that the mental change in their relationship with the disease is absolutely crucial for following treatment and managing suffering. […] In the case of people with chronic depression who have been taking medication for a long time, I have also seen improvements when they face what happens to them and meditate, I remember a student who, after taking Prozac for five years, was able to stop medication”.(female instructor, 50 years, 25 years of experience)
“[Mindfulness] It is aimed at people who may be going through a crisis, but they still have the resources and ability to help themselves, the ability to learn and enough motivation to be constant in the practice. You have to be motivated, because if you find yourself in a deep depression and you don’t find the motivation, it won’t work, it won’t do you any good”.(female instructor, 50 years old, 25 years of experience)
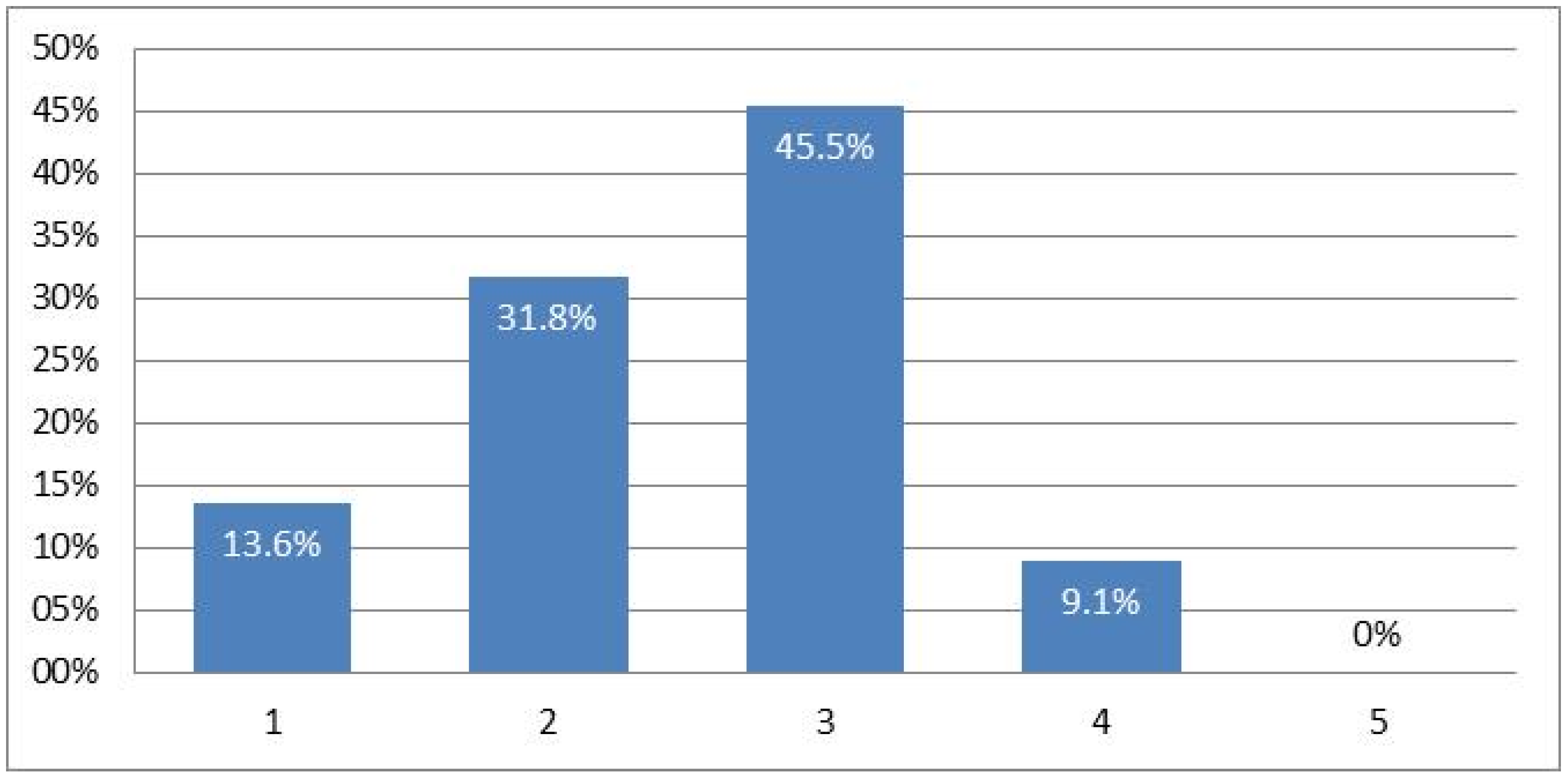
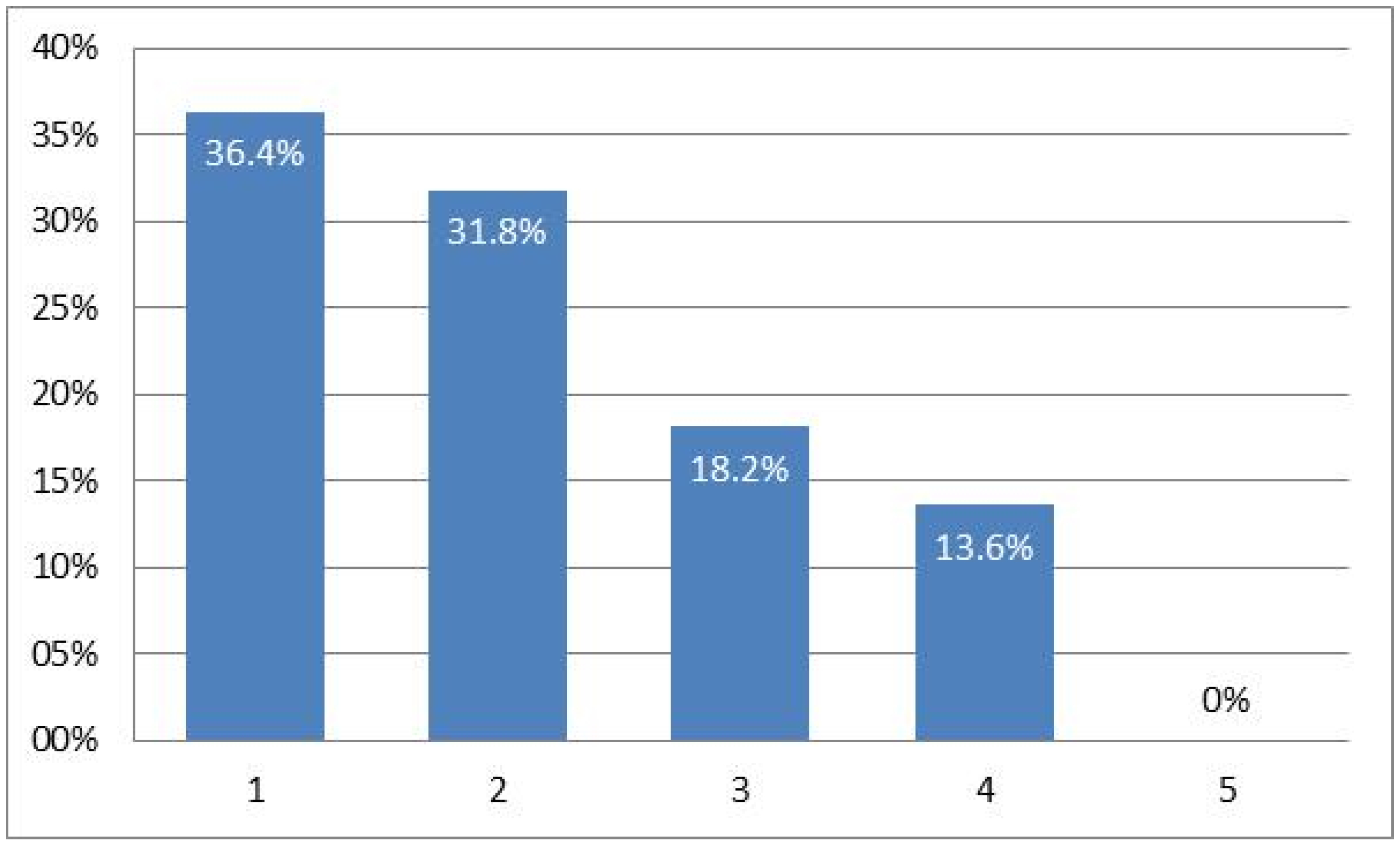
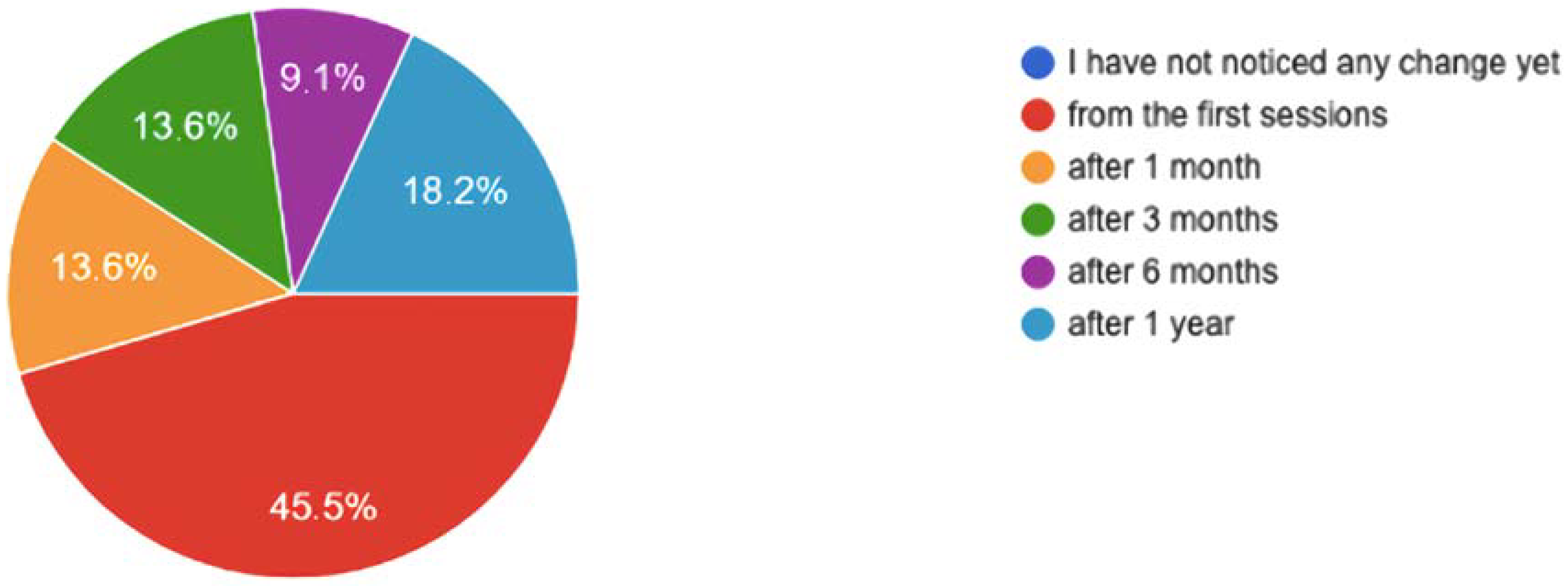
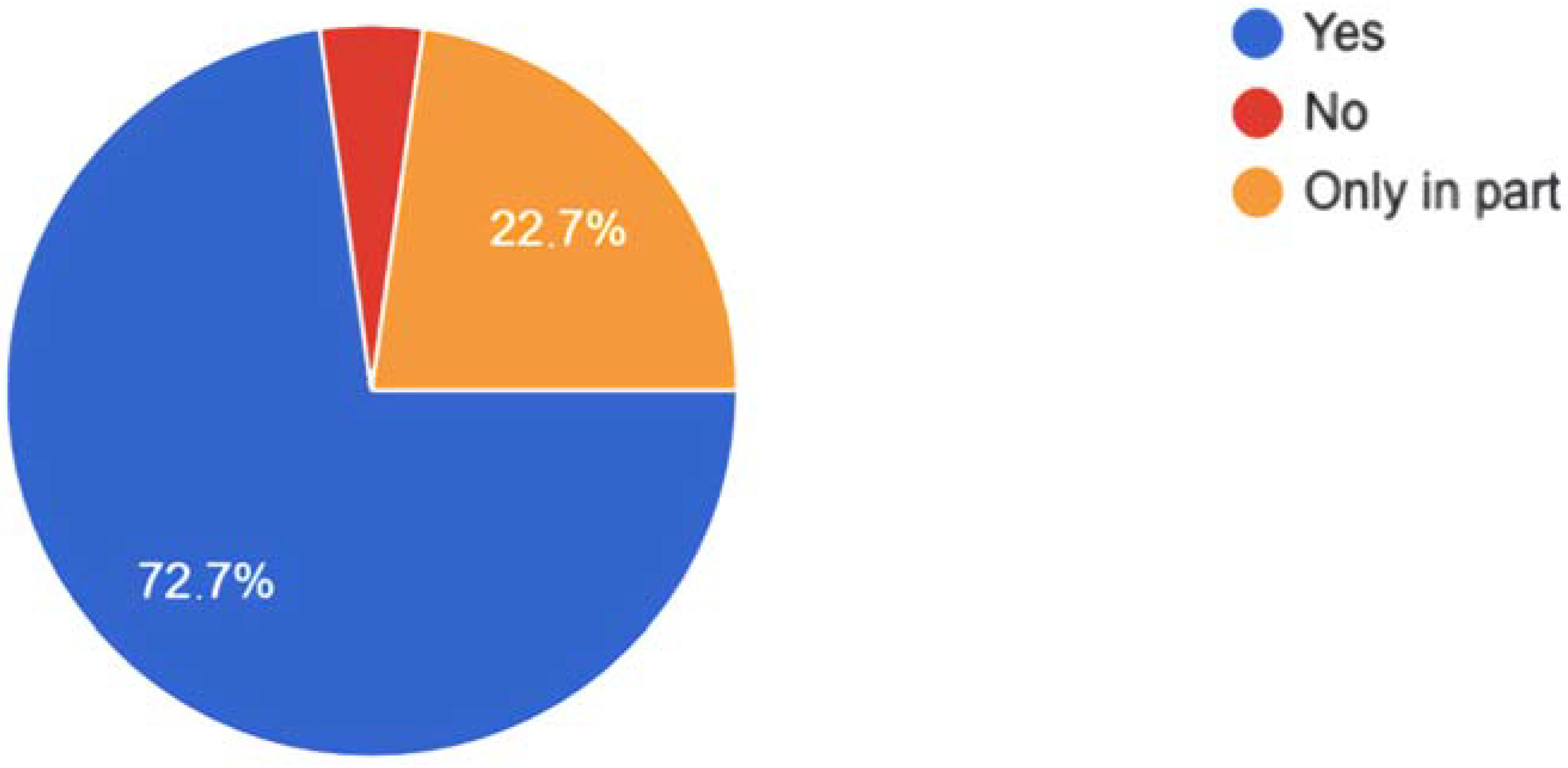
5.4. Mindfulness and the Effectiveness of Techniques
5.5. Mindfulness and Syndemic
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Singer, M. Introduction to Syndemics: A Critical Systems Approach to Public and Community Health; Jossey-Bass: San Francisco, CA, USA, 2009. [Google Scholar]
- Antón-Hurtado, F. Paternidades Judicializadas. In Hombres, Género Y Patriarcado: Reflexiones, Cuerpos Y Representaciones; Téllez, A., Martínez-Guirao, J.E., Sanfélix, J., Eds.; Dykinson: Madrid, Spain, 2020; pp. 75–96. [Google Scholar]
- Krishnamurti, J. El Libro de la Vida. Meditaciones Diarias; GaiaMSBCS: Madrid, Spain, 2013. [Google Scholar]
- Lévi-Strauss, C. L’Anthropologie Face Aux Problèmes Du Monde Modern; Seuil: París, France, 2011. [Google Scholar]
- Ministerio de Sanidad, Consumo y Bienestar Social. Gobierno de España. 2021. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/situacionActual.htm (accessed on 21 January 2022).
- Munárriz, L.A. Tercer milenio: Tiempo de utopía. An. De La Fund. Joaquín Costa 1997, 14, 255–277. [Google Scholar]
- Tolosana, C.L. Rito, funciones y significado. Música Oral Del Sur Música Hisp. Y Ritual. 2012, 9, 22–28. [Google Scholar]
- Bauman, Z. Miedo Líquido. La Sociedad Contemporánea Y Sus Temores; Paidós: Barcelona, Spain, 2007. [Google Scholar]
- Beck, U. La Sociedad Del Riesgo: Hacia Una Nueva Modernidad; Paidós: Barcelona, Spain, 2010. [Google Scholar]
- Santomauro, D.F.; Herrera, A.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Tang, Y.Y.; Hölzel, B.K.; Posner, M.I. The neuroscience of mindfulness. Nat. Rev. Neurosci. 2015, 16, 213–225. [Google Scholar] [CrossRef]
- Harari, Y.N. 21 Lecciones Para El Siglo XXI; Debate: Barcelona, Spain, 2020. [Google Scholar]
- García-Campayo, J.; Demarzo, M. Qué Sabemos Del Mindfulness? Kairós: Barcelona, Spain, 2018. [Google Scholar]
- Kabat-Zinn, J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life; Hyperion: New York, NY, USA, 1994. [Google Scholar]
- García-Campayo, J.; Demarzo, M. Mindfulness, Curiosidad Y Aceptación; Siglantana: Barcelona, Spain, 2015. [Google Scholar]
- Kabat-Zinn, J. Mindfulness-based stress reduction (MBSR). Constr. Hum. Sci. 2003, 8, 73. [Google Scholar]
- Segal, Z.V.; Teasdale, J.D.; Williams, J.M.; Gemar, M.C. The mindfulness-based cognitive therapy adherence scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clin. Psychol. Psychother. 2002, 9, 131–138. [Google Scholar] [CrossRef]
- Bowen, S.; Chawla, N.; Grow, J.; Marlatt, G.A. Mindfulness-Based Relapse Prevention for Addictive Behaviors; Guilford Publications: New York, NY, USA, 2021. [Google Scholar]
- McBee, L. Mindfulness-Based Elder Care: A CAM Model for Frail Elders and Their Caregivers; Springer Publishing Co.: New York, NY, USA, 2008. [Google Scholar]
- Bardacke, N.; Duncan, L.G. Mindfulness-based childbirth and parenting: Cultivating inner resources for the transition to parenthood and beyond. In Mindfulness-Based Treatment Approaches; Academic Press: Cambridge, MA, USA, 2014; pp. 213–237. [Google Scholar]
- Kabat-Zinn, J. Mindfulness-Based Interventions in Context: Past, Present, and Future. Clin. Psychol. Sci. Pract. 2006, 10, 144–156. [Google Scholar] [CrossRef]
- García-Campayo, J. Mindfulness: Nuevo Manual Práctico: El Camino De La Atención Plena; Singlatana: Barcelona, Spain, 2019. [Google Scholar]
- Gibson, J. The Ecological Approach to Visual Perception; Lawrence Erlbaum Associates: London, UK, 1986. [Google Scholar]
- Hutchins, E. Cognition in the Wild; The MIT Press: Cambridge, MA, USA, 1995. [Google Scholar]
- Clark, A. Being There: Putting Brain and World Together Again; The MIT Press: Cambridge, MA, USA, 1997. [Google Scholar]
- Healy, S.; Braithwaite, V. Cognitive ecology: A field of substance? Trends Ecol. Evol. 2000, 15, 22–26. [Google Scholar] [CrossRef]
- Antón-Hurtado, F. Propuesta antropológica de un modelo analítico para abordar la Syndemia. Cult. De Los Cuid. (Edición Digit.) 2020, 24, 2–6. [Google Scholar] [CrossRef]
- World Health Organization & Candau, Marcolino Gomes. The Work of WHO, 1967: Annual Report of the Director-General to the World Health Assembly and to the United Nations. World Health Organization. 1968. Available online: https://apps.who.int/iris/handle/10665/85804 (accessed on 10 January 2022).
- Flores-Guerrero, R. Salud, Enfermedad y Muerte: Lecturas desde la Antropología Sociocultural. Rev. Mad 2004, 10, 21–29. [Google Scholar] [CrossRef] [Green Version]
- Ulcuango, R. Manual de medicina de los pueblos Kichwas del Ecuador. In Codenpeecuarunary; Ecuarunari: Quito, Ecuador, 1998. [Google Scholar]
- Fernández Juárez, G. Médicos y Yatiris: Salud e Interculturalidad en el Altiplano Aymara; Organización Panamericana de la Salud: La Paz, Bolivia, 1999. [Google Scholar]
- Loza Balsa, G. Esbozo de Medicina Aymara; UMSA: La Paz, Bolivia, 1995. [Google Scholar]
- Guevara Torres, G. Salud y Antropología; Ministerio de Salud Ucayali-Pucallpa: Lima, Peru, 1999. [Google Scholar]
- Vergés de López, C. Mujer Ngöbe: Salud y Enfermedad; Instituto de la Mujer de la Universidad de Panamá: Panama City, Panama, 1998. [Google Scholar]
- Li, P. El Gran Libro De La Medicina China; Martínez Roca: Barcelona, Spain, 2001. [Google Scholar]
- Kit, W.K. El Gran Libro De La Medicina China; Un Enfoque de la Salud Física, Emocional, Mental y Espiritual; Urano: Barcelona, Spain, 2003. [Google Scholar]
- Maciocia, G. Los Fundamentos De La Medicina China; Aneid Press: Cascais, Portugal, 2001. [Google Scholar]
- Prevosti, A. Taoísmo. Filosofía y Religión del dao, in Prevosti (Coord.) Pensamiento y Religión en Asia Oriental; UOC: Barcelona, Spain, 2011. [Google Scholar]
- Lao, Z.; Suarez-Girard, A.H. Tao Te King; Siruela: Madrid, Spain, 2011. [Google Scholar]
- Román, M.T. Sabidurías Orientales De La Antigüedad; Alianza Editorial: Madrid, Spain, 2004. [Google Scholar]
- Watts, A. El Camino Del Tao; Kairós: Madrid, Spain, 1996. [Google Scholar]
- Hofmann, S.G.; Sawyer, A.T.; Witt, A.A.; Oh, D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J. Consult. Clin. Psychol. 2010, 78, 169–183. [Google Scholar] [CrossRef]
- Kil, H.; O’Neill, D.; Grusec, J.E. Prosocial motivation as a mediator between dispositional mindfulness and prosocial behavior. Personal. Individ. Differ. 2021, 177, 110806. [Google Scholar] [CrossRef]
- Blanck, P.; Perleth, S.; Heidenreich, T.; Kröger, P.; Ditzen, B.; Bents, H.; Mander, J. Effects of mindfulness exercises as stand-alone intervention on symptoms of anxiety and depression: Systematic review and meta-analysis. Behav. Res. Ther. 2018, 102, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Donald, J.N.; Sahdra, B.K.; Van Zanden, B.; Duineveld, J.J.; Atkins, P.W.; Marshall, S.L.; Ciarrochi, J. Does your mindfulness benefit others? A systematic review and meta-analysis of the link between mindfulness and prosocial behaviour. Br. J. Psychol. 2019, 110, 101–125. [Google Scholar]
- Juul, L.; Pallesen, K.J.; Bjerggaard, M.; Nielsen, C.; Fjorback, L.O. A pilot randomised trial comparing a mindfulness-based stress reduction course, a locally-developed stress reduction intervention and a waiting list control group in a real-life municipal health care setting. BMC Public Health 2020, 20, 409. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Thompson, D.R.; Jenkins, Z.M.; Ski, C.F. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J. Psychiatr. Res. 2017, 95, 156–178. [Google Scholar] [CrossRef] [PubMed]
- Bowen, S.; Witkiewitz, K.; Clifasefi, S.L.; Grow, J.; Chawla, N.; Hsu, S.H.; Carroll, H.A.; Harrop, E.; Collins, S.E.; Lustyk, M.K.; et al. Relative Efficacy of Mindfulness-Based Relapse Prevention, Standard Relapse Prevention, and Treatment as Usual for Substance Use Disorders: A Randomized Clinical Trial. JAMA Psychiatry 2014, 71, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Poissant, H.; Moreno, A.; Potvin, S.; Mendrek, A. A Meta-analysis of Mindfulness-Based Interventions in Adults with Attention-Deficit Hyperactivity Disorder: Impact on ADHD Symptoms, Depression, and Executive Functioning. Mindfulness 2020, 11, 2669–2681. [Google Scholar] [CrossRef]
- Cairncross, M.; Miller, C.J. The Effectiveness of Mindfulness-Based Therapies for ADHD: A Meta-Analytic Review. J. Atten. Disord. 2020, 5, 627–643. [Google Scholar] [CrossRef]
- Pandey, A.; Hale, D.; Das, S.; Goddings, A.L.; Blakemore, S.J.; Viner, R.M. Effectiveness of Universal Self-regulation-Based Interventions in Children and Adolescents: A Systematic Review and Meta-analysis. JAMA Pediatr. 2018, 172, 566–575. [Google Scholar] [CrossRef] [Green Version]
- Bronson, M.B. Self-Regulation in Early Childhood; The Guilford Press: New York, NY, USA, 2000. [Google Scholar]
- Hughes, C. Changes and challenges in 20 years of research into the development of executive functions. Infant Child Dev. 2011, 20, 251–271. [Google Scholar] [CrossRef] [Green Version]
- Duckworth, A.L.; Tsukayama, E.; May, H. Establishing causality using longitudinal hierarchical linear modeling: An illustration predicting achievement from self-control. Soc. Psychol. Personal. Sci. 2010, 1, 311–317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogg, T.; Roberts, B.W. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychol. Bull. 2004, 6, 887–919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daly, M.; Egan, M.; Quigley, J.; Delaney, L.; Baumeister, R.F. Childhood self-control predicts smoking throughout life: Evidence from 21,000 cohort study participants. Health Psychol. 2016, 35, 1254–1263. [Google Scholar] [CrossRef]
- Basso, J.C.; McHale, A.; Ende, V.; Oberlin, D.J.; Suzuki, W.A. Brief, daily meditation enhances attention, memory, mood, and emotional regulation in non-experienced meditators. Behav. Brain Res. 2019, 356, 208–220. [Google Scholar] [CrossRef]
- Montero-Marin, J.; Garcia-Campayo, J.; Pérez-Yus, M.C.; Zabaleta-Del-Olmo, E.; Cuijpers, P. Meditation techniques v. relaxation therapies when treating anxiety: A meta-analytic review. Psychol. Med. 2019, 49, 2118–2133. [Google Scholar] [CrossRef]
- Lutz, A.; Slagter, H.A.; Dunne, J.D.; Davidson, R. Attention regulation and monitoring in meditation. Trends Cogn. Sci. 2008, 4, 163–169. [Google Scholar] [CrossRef] [Green Version]
- Randal, C.; Pratt, D.; Bucci, S. Mindfulness and Self-esteem: A Systematic Review. Mindfulness 2015, 6, 1366–1378. [Google Scholar] [CrossRef]
- Thompson, B.; Waltz, J. Mindfulness, Self-Esteem, and Unconditional Self-Acceptance. J. Ration.-Emot. Cogn.-Behav. Ther. 2008, 6, 119–126. [Google Scholar] [CrossRef]
- Afonso, R.F.; Kraft, I.; Aratanha, M.A.; Kozasa, E.H. Neural correlates of meditation: A review of structural and functional MRI studies. Front. Biosci. (Sch. Ed.) 2020, 12, 92–115. [Google Scholar] [CrossRef]
- Gotink, R.A.; Meijboom, R.; Vernooij, M.W.; Smits, M.; Hunink, M.G. 8-week Mindfulness Based Stress Reduction induces brain changes similar to traditional long-term meditation practice—A systematic review. Brain Cogn. 2016, 108, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Behan, C. The benefits of meditation and mindfulness practices during times of crisis such as COVID-19. Ir. J. Psychol. Med. 2020, 37, 256–258. [Google Scholar] [CrossRef] [PubMed]
- Lomas, T.; Medina, J.C.; Ivtzan, I.; Rupprecht, S.; Eiroa-Orosa, F.J. A systematic review of the impact of mindfulness on the well-being of healthcare professionals. J. Clin. Psychol. 2018, 74, 319–355. [Google Scholar] [CrossRef] [Green Version]
- Paniagua, P.S.; Reyes, M.T.A.; Couso, M.P.P.; Majuelo, R.S.; Villalba, R.S.; Martínez, B.G. COVID-19 y mindfulness en profesionales sanitarios: Una revisión sistemática. Rev. Ocronos. 2021, 4, 139–144. Available online: https://revistamedica.com/covid-mindfulness-sanitarios/ (accessed on 10 January 2022).
- Deguma, M.C.; Lumayag, C.G.; Villaganas, M.; Delos Reyes, N.; Deguma, J.J. From anxious loneliness to meditation: A mental health self-care strategy to cope with the COVID-19 pandemic. Advance online publication. J. Public Health 2021, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Tellez, A. La Investigación Antropológica; Editorial Club Universitario: San Vicente del Raspeig, Spain, 2007. [Google Scholar]
- Tellez, A.; Martínez-Guirao, J.E. Métodos y Técnicas de Investigación en Antropología Social. Guía Didáctica y Práctica. Universidad Miguel Hernández de Elche. 2008. Available online: https://grados.ugr.es/ramas/ciencias-sociales-juridicas/grado-antropologia-social-y-cultural/metodos-y-tecnicas-investigacion-antropologia/guia-docente (accessed on 10 January 2022).
- Waddington, C.H. Evolutionary systems—Animal and human. Nature 1956, 183, 1634–1638. [Google Scholar] [CrossRef]
- Bianco, G. Aspectos Psicofisiológicos del Embarazo, Parto y Puerperio VIII Jornada de Salud Perinatal. Santiago de Compostela, 25 November 2014. Available online: https://www.sergas.es/docs/muller/VIIIPerinatal/Documentacion/3_aspectos_psicofisioloxicos_Gabriella.pdf (accessed on 10 January 2022).
- Instituto de la Mujer La Perspectiva de Género. Esencial en la Respuesta a la COVID-19; Ministerio de Igualdad, Gobierno de España: Madrid, Spain, 2020; Available online: https://www.inmujeres.gob.es/diseno/novedades/IMPACTO_DE_GENERO_DEL_COVID_19_(uv).pdf (accessed on 10 January 2022).
| Age Range | Number of People | Sex |
|---|---|---|
| 35–45 | 22 | 4 |
| 46–55 | 14 | 2 |
| 56–67 | 8 | 0 |
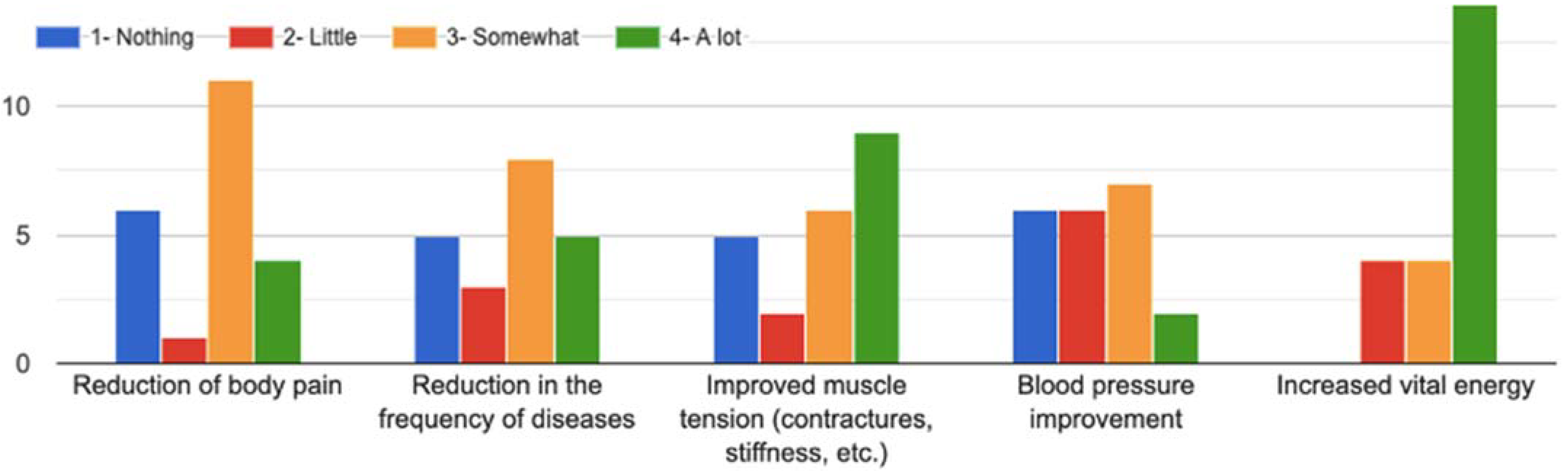
| Nothing | Little | Somewhat | A Lot | |
|---|---|---|---|---|
| Reduction of body pain | 27.3% | 4.5% | 50% | 18.2% |
| Reduction in the frequency of diseases | 22.7% | 13.6% | 36.4% | 22.7% |
| Improved muscle tension (contractures, stiffness, etc.) | 22.7% | 9.1% | 27.3% | 40.9% |
| Blood pressure improvement | 27.3% | 27.3% | 31.8% | 9.1% |
| Increased vital energy | 0% | 18.2% | 18.2% | 63.6% |
| Nothing | Little | Somewhat | A Lot | |
|---|---|---|---|---|
| Anxiety reduction | 0.0% | 0.0% | 22.7% | 72.7% |
| Feeling of peace and tranquility | 0.0% | 4.5% | 9.1% | 86.4% |
| Improved self-control | 0.0% | 4.5% | 18.2% | 77.3% |
| Improved social relationships | 0.0% | 4.5% | 31.8% | 63.6% |
| Decrease in negative emotions (fear, anger) | 4.5% | 0.0% | 36.4% | 59.1% |
| Decrease in negative thoughts | 4.5% | 0.0% | 27.3% | 68.2% |
| Increased empathy | 0.0% | 0.0% | 36.4% | 63.6% |
| Greater tolerance | 0.0% | 0.0% | 31.8% | 68.2% |
| Greater compassion | 0.0% | 0.0% | 36.4% | 59.1% |
| Improved self-compassion and self-care | 0.0% | 9.1% | 27.3% | 63.6% |
| Stress reduction | 0.0% | 4.5% | 45.5% | 50.0% |
| Reduction of depressive states | 0.0% | 13.6% | 36.4% | 45.5% |
| I Don’t Use It | Not Efficient at All | Not Very Efficient | Efficient | Very Efficient | |
|---|---|---|---|---|---|
| Mindfulness of breathing | 0.0% | 0.0% | 4.5% | 27.3% | 68.2% |
| Attention to sounds | 36.4% | 0.0% | 9.1% | 31.8% | 22.7% |
| Attention in images | 50.0% | 0.0% | 9.1% | 27.3% | 9.1% |
| Use of mantras | 22.7% | 9.1% | 9.1% | 45.5% | 13.6% |
| Visualizations | 22.7% | 0.0% | 9.1% | 40.9% | 27.3% |
| Attention to the body (body scan) | 4.5% | 0.0% | 9.1% | 45.5% | 40.9% |
| Attention to emotion | 4.5% | 4.5% | 9.1% | 40.9% | 40.9% |
| Years of Practice | Mental | Physical |
|---|---|---|
| 1 or less | 3 | 2.25 |
| between 1 and 3 | 3 | 2.2 |
| 3 or more | 1.9 | 1.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez Guirao, J.E.; Antón Hurtado, F.; Sánchez Vera, F.; Tellez Infantes, A. Health and Mindfulness during the Syndemic of SARS-CoV-2: An Ethnographic Study. Healthcare 2022, 10, 686. https://doi.org/10.3390/healthcare10040686
Martínez Guirao JE, Antón Hurtado F, Sánchez Vera F, Tellez Infantes A. Health and Mindfulness during the Syndemic of SARS-CoV-2: An Ethnographic Study. Healthcare. 2022; 10(4):686. https://doi.org/10.3390/healthcare10040686
Chicago/Turabian StyleMartínez Guirao, Javier Eloy, Fina Antón Hurtado, Fulgencio Sánchez Vera, and Anastasia Tellez Infantes. 2022. "Health and Mindfulness during the Syndemic of SARS-CoV-2: An Ethnographic Study" Healthcare 10, no. 4: 686. https://doi.org/10.3390/healthcare10040686
APA StyleMartínez Guirao, J. E., Antón Hurtado, F., Sánchez Vera, F., & Tellez Infantes, A. (2022). Health and Mindfulness during the Syndemic of SARS-CoV-2: An Ethnographic Study. Healthcare, 10(4), 686. https://doi.org/10.3390/healthcare10040686







