Validity Analysis of Neck Circumference as a Screening Test for Hypoxia Occurrence in Patients Undergoing Sedative Endoscopy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Research Environment and Participants
2.3. Research Tools
2.3.1. STOP-BANG Sleep Questionnaire
2.3.2. Berlin Sleep Questionnaire
2.3.3. Neck Circumference in a Sitting Position and a Lateral Decubitus Position
2.4. Ethical Considerations
2.5. Data Analysis
3. Results
3.1. Hypoxia Occurrence According to Subject Characteristics, Sleep Questionnaire, and Neck Circumference
3.2. Comparison of Performance as a Screening Test for Hypoxia
3.3. Sensitivity, Specificity, and Cutoff Values for the Decrease in Oxygen Saturation for Each Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kiriyama, S.; Naitoh, H.; Kuwano, H. Propofol sedation during endoscopic treatment for early gastric cancer compared to midazolam. World J. Gastroenterol. WJG 2014, 20, 11985. [Google Scholar] [CrossRef] [PubMed]
- McQuaid, K.R.; Laine, L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest. Endosc. 2008, 67, 910–923. [Google Scholar] [CrossRef]
- Ristikankare, M.; Julkunen, R.; Heikkinen, M.; Mattila, M.; Laitinen, T.; Wang, S.; Hartikainen, J. Sedation, topical pharyngeal anesthesia and cardiorespiratory safety during gastroscopy. J. Clin. Gastroenterol. 2006, 40, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, M.; Fanti, L.; Gemma, M.; Pasculli, N.; Beretta, L.; Testoni, P.A. Adverse events during monitored anesthesia care for GI endoscopy: An 8-year experience. Gastrointest. Endosc. 2011, 74, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Lee, K.-Y. Safe sedation in a private clinic. J. Korean Med. Assoc. 2011, 54, 1179–1188. [Google Scholar] [CrossRef]
- Gross, J.B.; Bailey, P.L.; Connis, R.T.; Coté, C.J.; Davis, F.G.; Epstein, B.S.; Gilbertson, L.; Nickinovich, D.G.; Zerwas, J.M.; Zuccaro, G., Jr. Practice Guidelines for Sedation and Analgesia by Non-Anesthesiologists. Anesthesiology 2002, 96, 1004–1017. [Google Scholar] [CrossRef]
- Dumonceau, J.-M.; Riphaus, A.; Schreiber, F.; Vilmann, P.; Beilenhoff, U.; Aparicio, J.R.; Vargo, J.J.; Manolaraki, M.; Wientjes, C.; Rácz, I.; et al. Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates Guideline-Updated June 2015. Endoscopy 2015, 47, 1175–1189. [Google Scholar] [CrossRef] [PubMed]
- Do, S.Y.; Kim, S.; Kim, K.T.; Cho, Y.W. Clinical Risk Factors for Sleep Apnea in a Korean Sleep Clinic. J. Korean Neurol. Assoc. 2019, 37, 352–360. [Google Scholar] [CrossRef]
- Chung, F.; Abdullah, H.R.; Liao, P. STOP-Bang Questionnaire A Practical Approach to Screen for Obstructive Sleep Apnea. Chest 2016, 149, 631–638. [Google Scholar] [CrossRef]
- Chung, F.; Yegneswaran, B.; Liao, P.; Chung, S.A.; Vairavanathan, S.; Islam, S.; Khajehdehi, A.; Shapiro, C.M. STOP Questionnaire: A Tool to Screen Patients for Obstructive Sleep Apnea. Anesthesiology 2008, 108, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Chung, F.; Yegneswaran, B.; Liao, P.; Chung, S.A.; Vairavanathan, S.; Islam, S.; Khajehdehi, A.; Shapiro, C.M. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med. Rev. 2017, 36, 116–124. [Google Scholar] [CrossRef]
- Patel, V.A.; Romain, P.S.; Sanchez, J.; Fisher, D.A.; Schulteis, R.D. Obstructive Sleep Apnea Increases the Risk of Cardiopulmonary Adverse Events Associated with Ambulatory Colonoscopy Independent of Body Mass Index. Dig. Dis. Sci. 2017, 62, 2834–2839. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, N.A.A.; Dilektasli, A.G.; Cetinoglu, E.D.; Ursavas, A.; Karadag, M. Diagnostic Accuracy of a Modified STOP-BANG Questionnaire with National Anthropometric Obesity Indexes. Turk. Thorac. J. 2019, 20, 103. [Google Scholar] [CrossRef]
- Simpson, L.; Mukherjee, S.; Cooper, M.; Ward, K.L.; Lee, J.D.; Fedson, A.C.; Potter, J.; Hillman, D.; Eastwood, P.; Palmer, L.; et al. Sex Differences in the Association of Regional Fat Distribution with the Severity of Obstructive Sleep Apnea. Sleep 2010, 33, 467. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-W.; Lee, S.-Y.; Ye, M.-K.; Kang, S.-G.; Kim, S.-T.; Park, K.-H.; Kim, J.-E.; Shin, S.-H. Correlation Analysis between Anthropometric Measurement and the Results of Seep Questionnaires in Patients with Obstructive Sleep Apnea. J. Rhinol. 2015, 22, 96–102. [Google Scholar] [CrossRef][Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Silva, G.E.; Vana, K.D.; Goodwin, J.L.; Sherrill, D.L.; Quan, S.F. Identifi cation of Patients with Sleep Disordered Breathing: Comparing the four-Variable Screening Tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J. Clin. Sleep Med. 2011, 7, 467–472. [Google Scholar] [CrossRef]
- Yang, H.; Park, H. Usefulness of the Berlin, STOP, and STOP-Bang Questionnaires in the Diagnosis of Obstructive Sleep Apnea. J. Sleep Med. 2019, 16, 11–20. [Google Scholar] [CrossRef]
- Kang, J.H.; Ryu, B.Y.; Suh, H.S.; Shim, K.W. Neck Circumference as a Simple Obesity Index. Korean J. Obes. 2002, 11, 142–149. [Google Scholar]
- Enestvedt, B.K.; Eisen, G.M.; Holub, J.; Lieberman, D.A. Is the American Society of Anesthesiologists classification useful in risk stratification for endoscopic procedures? Gastrointest. Endosc. 2013, 77, 464–471. [Google Scholar] [CrossRef]
- Alfonso, E.; Piñeros, F. Deep Sedation for Endoscopy Not Administered by Anesthesiologists: The Position of an Endoscopist in 2011. Rev. Colomb. De Gastroenterol. 2011, 26, 107–116. [Google Scholar]
- Wolk, R.; Somers, V.K. Sleep and the metabolic syndrome. Authors J. Compil. C 2007, 92, 67–78. [Google Scholar] [CrossRef] [PubMed]
- Namysłowski, G.; Scierski, W.; Mrówka-Kata, K.; Kawecka, I.; Kawecki, D.; Czecior, E. Sleep Study in Patients with Overweight and Obesity. J. Physiol. Pharmacol. 2005, 56, 59–65. [Google Scholar] [PubMed]
- Lee, S.K.; Hong, S.-N.; Jung, J.H.; Choi, J.H. A Case of Bariatric Surgery for an OSAS Patient with Severe Obesity. Sleep Med. Psychophysiol. 2016, 23, 93–96. [Google Scholar] [CrossRef][Green Version]
- Triantafillidis, J.K.; Merikas, E.; Nikolakis, D.; Papalois, A.E.; Niko-lakis, D. Sedation in gastrointestinal endoscopy: Current issues. World J. Gastroenterol. 2013, 19, 463–481. [Google Scholar] [CrossRef]
- Waring, J.P.; Baron, T.H.; Hirota, W.K.; Goldstein, J.L.; Jacobson, B.C.; Leighton, J.A.; Faigel, D.O. Guidelines for Conscious Sedation and Monitoring During Gastrointestinal Endoscopy. Gastrointest. Endosc. 2003, 58, 317–322. [Google Scholar] [CrossRef]
- Liou, S.-C.; Hsu, C.-M.; Chen, C.; Su, M.-Y.; Chiu, C.-T. Assessment of the Berlin Questionnaire for evaluation of hypoxemia risk in subjects undergoing deep sedation for screening gastrointestinal endoscopy. Ther. Clin. Risk Manag. 2018, 14, 1331. [Google Scholar] [CrossRef]
- Vasu, T.S.; Doghramji, K.; Cavallazzi, R.; Grewal, R.; Hirani, A.; Leiby, B.; Markov, D.; Reiter, D.; Kraft, W.K.; Witkowski, T. Obstructive Sleep Apnea Syndrome and Postoperative Complications: Clinical Use of the STOP-BANG Questionnaire. Arch. Otolaryngol.-Head Neck Surg. 2010, 136, 1020–1024. [Google Scholar] [CrossRef]
- Park, J.-H.; Lee, S.J.; Gwak, J.I.; Shim, J.-Y.; Lee, J.K. Sleep quality of breast cancer patients receiving chemotherapy in the outpatients setting. Korean J. Fam. Med. 2010, 31, 778–785. [Google Scholar] [CrossRef]
- Katz, I.; Stradling, J.; Sljutsky, A.S.; Zamel, N.; Hoffstein, V. Do Patients with Obstructive Sleep Apnea Have Thick Necks? Am. Rev. Respir. Dis. 1990, 141, 1228–1231. [Google Scholar] [CrossRef]
- Kim, S.E.; Park, B.S.; Park, S.; Shin, K.J.; Ha, S.Y.; Park, J.S.; Park, K.M. Has Snoring Significance for Predicting Obstructive Sleep Apnea Severity? Korean J. Clin. Neurophysiol. 2015, 17, 61. [Google Scholar] [CrossRef][Green Version]
| Variable | Category | No Hypoxia (n = 145) Mean (SD) | Hypoxia (n = 23) Mean (SD) | t/χ2 | p |
|---|---|---|---|---|---|
| Age (year) | 49.70 ± 12.45 | 53.39 ± 12.31 | −1.325 | 0.187 | |
| Sex | Man | 71 (49.0) | 14 (60.9) | 1.125 | 0.289 |
| Woman | 74 (51.0) | 9 (39.1) | |||
| Height (cm) | 164.70 ± 8.16 | 166.39 ± 7.65 | −0.933 | 0.352 | |
| Weight (kg) | 65.76 ± 14.10 | 78.38 ± 14.88 | −3.806 | 0.001 | |
| BMI (kg/m2) | 24.10 ± 3.91 | 28.29 ± 4.92 | −3.900 | 0.001 | |
| Propofol amount (mg) | 3.10 ± 1.17 | 2.88 ± 1.26 | 0.732 | 0.465 | |
| ASA class | Status I | 80 (47.3) | 6 (3.6) | 6.403 | 0.011 |
| Status II | 66 (39.1) | 17 (10.1) | |||
| Examination | Gastroscopy only | 86 (59.3) | 13 (56.5) | 0.064 | 0.801 |
| Gastroscopy and Colonoscopy | 59 (40.7) | 10 (43.5) | |||
| History | No | 79 (54.5) | 7 (30.4) | 4.595 | 0.032 |
| Yes | 66 (45.5) | 16 (69.6) | |||
| STOP-BANG | 2.48 ± 1.603 | 4.74 ± 1.514 | 6.330 | <0.001 | |
| Berlin | 1 ± 0.847 | 1.74 ± 0.964 | 3.817 | <0.001 | |
| Neck-sit (cm) | 35.71 ± 4.00 | 40.35 ± 4.06 | 5.158 | <0.001 | |
| Neck-lying (cm) | 36.43 ± 4.10 | 41.20 ± 4.22 | −5.154 | <0.001 |
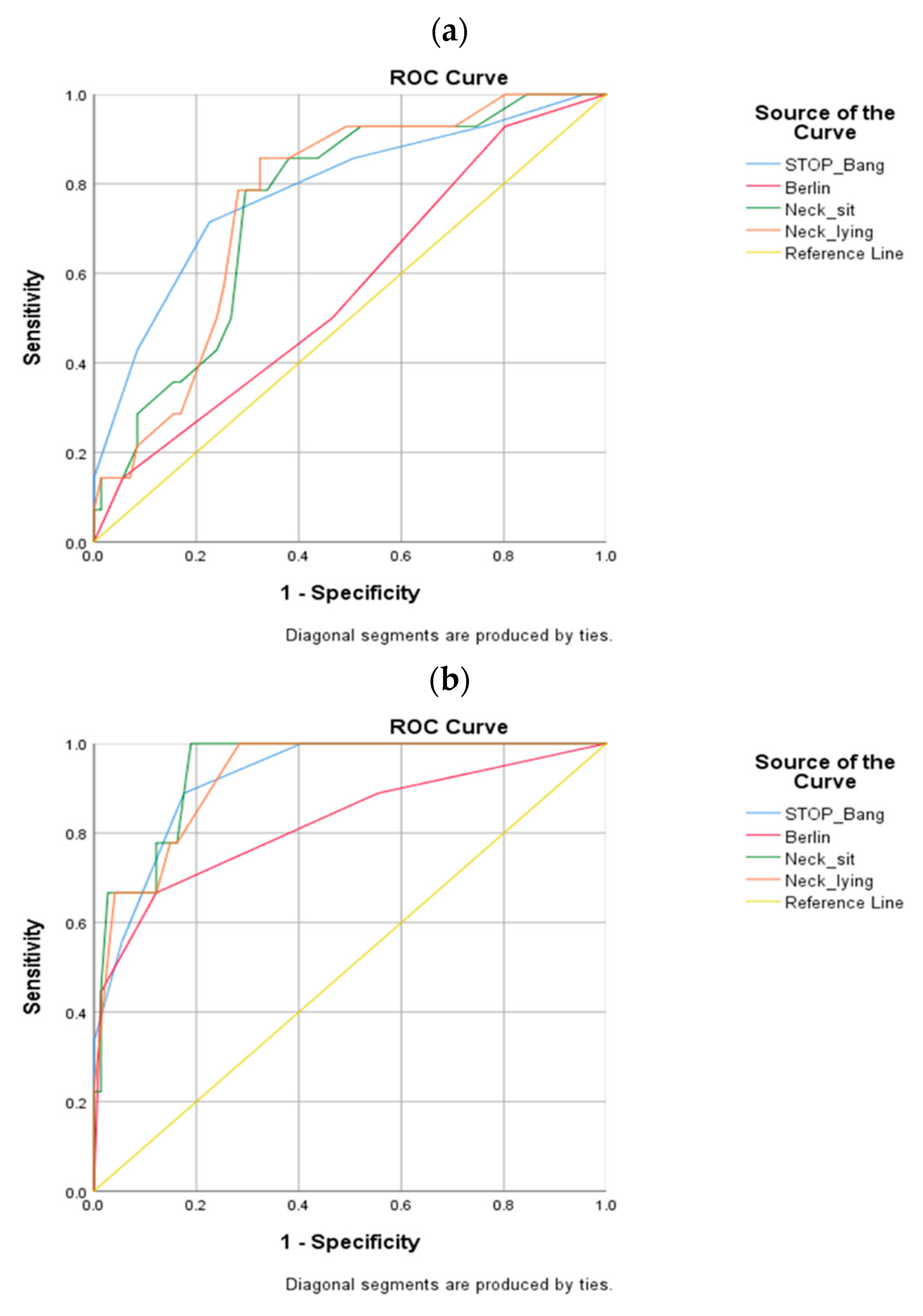
| Variable | AUC † | Standard Error | 95% Confidence Interval | |
|---|---|---|---|---|
| Men | STOP-BANG | 0.785 | 0.072 | 0.643–0.926 |
| Berlin | 0.567 | 0.082 | 0.406–0.728 | |
| Neck-sit | 0.749 | 0.064 | 0.624–0.875 | |
| Neck-lying | 0.759 | 0.061 | 0.639–0.878 | |
| Women | STOP-BANG | 0.923 | 0.037 | 0.851–0.996 |
| Berlin | 0.821 | 0.088 | 0.647–0.994 | |
| Neck-sit | 0.940 | 0.030 | 0.872–0.998 | |
| Neck-lying | 0.926 | 0.035 | 0.857–0.996 |
| Sex | Variable | Cutoff | Sensitivity | Specificity | Sensitivity + Specificity |
|---|---|---|---|---|---|
| Men | STOP-BANG | 3.5 | 0.857 | 0.493 | 1.350 |
| 4.5 | 0.714 | 0.775 | 1.489 | ||
| 5.5 | 0.429 | 0.915 | 1.344 | ||
| Berlin | 0.5 | 0.929 | 0.197 | 1.126 | |
| 1.5 | 0.500 | 0.535 | 1.035 | ||
| 2.5 | 0.143 | 0.944 | 1.087 | ||
| Neck-sit | 39.8 | 0.786 | 0.662 | 1.448 | |
| 40.5 | 0.786 | 0.704 | 1.490 | ||
| 41.3 | 0.500 | 0.732 | 1.232 | ||
| Neck-lying | 39.8 | 0.857 | 0.634 | 1.491 | |
| 40.3 | 0.857 | 0.676 | 1.533 | ||
| 40.8 | 0.786 | 0.676 | 1.462 | ||
| Women | STOP-BANG | 1.5 | 1.000 | 0.595 | 1.595 |
| 2.5 | 0.889 | 0.824 | 1.713 | ||
| 3.5 | 0.556 | 0.946 | 1.502 | ||
| Berlin | 0.5 | 0.889 | 0.446 | 1.335 | |
| 1.5 | 0.667 | 0.878 | 1.545 | ||
| 2.5 | 0.444 | 0.986 | 1.431 | ||
| Neck-sit | 34.9 | 0.778 | 0.851 | 1.629 | |
| 35.3 | 0.778 | 0.878 | 1.656 | ||
| 35.8 | 0.667 | 0.878 | 1.545 | ||
| Neck-lying | 35.3 | 0.778 | 0.838 | 1.616 | |
| 35.8 | 0.778 | 0.851 | 1.629 | ||
| 36.3 | 0.667 | 0.878 | 1.545 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, H.-J.; Kim, J. Validity Analysis of Neck Circumference as a Screening Test for Hypoxia Occurrence in Patients Undergoing Sedative Endoscopy. Healthcare 2022, 10, 679. https://doi.org/10.3390/healthcare10040679
Song H-J, Kim J. Validity Analysis of Neck Circumference as a Screening Test for Hypoxia Occurrence in Patients Undergoing Sedative Endoscopy. Healthcare. 2022; 10(4):679. https://doi.org/10.3390/healthcare10040679
Chicago/Turabian StyleSong, Hyun-Ji, and Jiyun Kim. 2022. "Validity Analysis of Neck Circumference as a Screening Test for Hypoxia Occurrence in Patients Undergoing Sedative Endoscopy" Healthcare 10, no. 4: 679. https://doi.org/10.3390/healthcare10040679
APA StyleSong, H.-J., & Kim, J. (2022). Validity Analysis of Neck Circumference as a Screening Test for Hypoxia Occurrence in Patients Undergoing Sedative Endoscopy. Healthcare, 10(4), 679. https://doi.org/10.3390/healthcare10040679






