Patients’ and Nurses’ Perceptions of Importance of Caring Nurse–Patient Interactions: Do They Differ?
Abstract
1. Introduction
Theoretical Framework
2. Materials and Methods
2.1. Study Design
2.2. Respondents
2.3. Instrument
2.4. Data Collection
2.5. Data Analysis
2.6. Ethical Considerations
3. Results
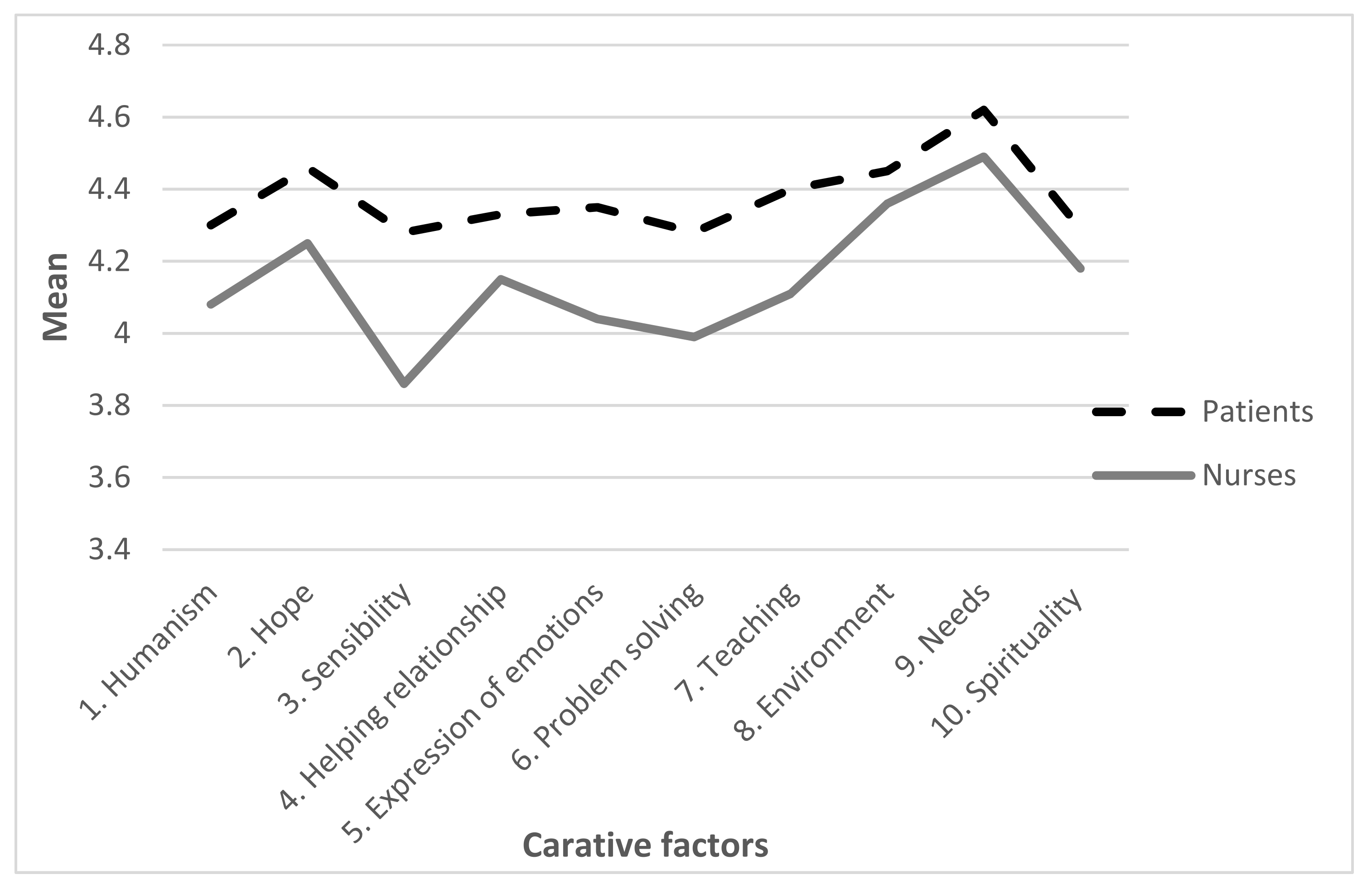
3.1. Patients’ and Nurses’ Perception of Caring Nurse–Patient Interaction
3.2. Differences in Patients’ and Nurses’ Perception of the Importance of Caring Nurse–Patient Interactions
3.3. Contribution of Independent Variables to Explanation of Nurses’ and Patients’ Perception of Caring Interaction
4. Discussion
4.1. Patients’ Perception of the Importance of Caring Nurse–Patient Interactions
4.2. Nurses’ Perception of Importance of Caring Nurse–Patient Interactions
4.3. Differences in Patients’ and Nurses’ Perceptions Related to the Importance of Caring Nurse–Patient Interactions
4.4. Further Research and Practice
4.5. Limitations of the Study
4.6. Implications for Nursing
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bridges, J.; Nicholson, C.; Maben, J.; Pope, C.; Flatley, M.; Wilkinson, C.; Meyer, J.; Tziggili, M. Capacity for care: Meta-ethnography of acute care nurses’ experiences of the nurse-patient relationship. Adv. Nurs. 2013, 69, 760–772. [Google Scholar] [CrossRef] [PubMed]
- Alligood, M.R. Nursing Theorists and Their Work, 9th ed.; Mosby Elsevier: Maryland Heights, MO, USA, 2017; ISBN 9780323402248. [Google Scholar]
- Létourneau, D.; Chantal, C.; Goudreau, J. Humanizing Nursing Care: An Analysis of Caring Theories Through the Lens of Humanism. Int. J. Hum. Caring 2017, 21, 32–40. [Google Scholar] [CrossRef]
- Kitson, A.; Muntlin Athlin, A.; Conroy, T. Anything but basic: Nursing’s challenge in meeting patients’ fundamental care needs. J. Nurs. Scholarsh. 2014, 46, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Wiechula, R.; Conroy, T.; Kitson, A.; Marshall, R.J.; Whitaker, N.; Rasmussen, P. Umbrella review of the evidence: What factors influence the caring relationship between a nurse and patient? J. Adv. Nurs. 2015, 72, 723–734. [Google Scholar] [CrossRef]
- Fortuno, A.F.; Oco, D.B.; Clores, M.A. Influential Components of Caring Nurse-Patient Interaction (CNPI) in a Tertiary Hospital in the Philippines: Towards Improving Health Outcomes of Patients. Int. J. Nurs. Sci. 2017, 7, 84–90. [Google Scholar] [CrossRef]
- Chung, H.-C.; Chen, Y.-C.; Chang, S.-C.; Hsu, W.-L.; Hsieh, T.-C. Development and Validation of Nurses’ Well-Being and Caring Nurse–Patient Interaction Model: A Psychometric Study. Int. J. Environ. Res. Public Health 2021, 18, 7750. [Google Scholar] [CrossRef]
- Feo, R.; Donnelly, F.; Athlin, Å.M.; Jangland, E. Providing high-quality fundamental care for patients with acute abdominal pain. J. Health Organ. Manag. 2019, 33, 110–123. [Google Scholar] [CrossRef]
- Soriano, G.P. Psychometric Evaluation of the Filipino Version of Caring Nurse-Patient Interaction Scale-Patient. Int. J. Hum. Caring 2019, 23, 329–333. [Google Scholar] [CrossRef]
- Haryani, A. Predictors of Nurse’s Caring Behavior towards Patients with Critical Illness. KnE Life Sci. 2019, 12–22. [Google Scholar] [CrossRef]
- Morrison, K.B.; Korol, S. Nurses’ perceived and actual caregiving roles: Identifying factors that can contribute to job satisfaction. J. Clin. Nurs. 2014, 23, 3468–3477. [Google Scholar] [CrossRef]
- Zeleníkova, R.; Gurková, E.; Friganovic, A.; Uchmanowicz, I.; Jarošová, D.; Žiaková, K.; Plevová, I.; Papastavrou, E. Unfinished nursing care in four central European countries. J. Nurs. Manag. 2019, 28, 1888–1900. [Google Scholar] [CrossRef] [PubMed]
- Bachnik, S.; Ausserhofer, D.; Baernholdt, M.; Simon, M. Patient-centred care, nurse work environment and implicit rationing of nursing care in Swiss acute care hospitals: A crosssectional multi-center study. Int. J. Nurs. Stud. 2018, 81, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Felgen, J.A. Caring: Core value, currency, and commodity…is it time to get tough about “soft”? Nurs. Adm. Q. 2003, 27, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Cara, C.; Gauvin-Lepage, J.; Lefebvre, H.; Létourneau, D.; Alderson, M.; Larue, C.; Beauchamp, J.; Gagnon, L.; Casimir, M.; Girard, F.; et al. Le Modèle humaniste des soins infirmiers—UdeM: Perspective novatrice et pragmatique. Rech. En Soins Infirm. 2016, 125, 20–31. [Google Scholar] [CrossRef]
- Watson, J. Caring science and human caring theory: Transforming personal and professional practices of nursing and health care. J. Health Hum. Serv. Adm. 2009, 31, 466–482. [Google Scholar] [CrossRef]
- Delmas, P.; Antonini, M.; Berthoud, L.; O’Reilly, L.; Cara, C.; Brousseau, S.; Bellier-Teichmann, T.; Weidmann, J.; Roulet-Schwab, D.; Ledoux, I.; et al. A comparative descriptive analysis of perceived quality of caring attitudes and behaviours between haemodialysis patients and their nurses. Nurs. Open 2019, 7, 563–570. [Google Scholar] [CrossRef]
- Roulin, M.J.; Jonniaux, S.; Guisado, H.; Séchaud, L. Perceptions of inpatients and nurses towards the importance of nurses’ caring behaviours in rehabilitation: A comparative study. Int. J. Nurs. Pract. 2020, 23, e128135. [Google Scholar] [CrossRef]
- Brewer, B.B.; Watson, J. Evaluation of authentic human caring professional practices. J. Nurs. Adm. 2015, 45, 622–627. [Google Scholar] [CrossRef]
- Settecase-Wu, C.A.; Whetsell, M.V. Caring in the Nurse-Patient Relationship through the Caritas Lens: An Integrative Review. Rev. Cult. Del Cuid. 2018, 15, 34–66. [Google Scholar] [CrossRef]
- Watson, J. Human Caring Science: A Theory of Nursing, 2nd ed.; Jones and Bartlett Learning LLC: Sudbury, MA, USA, 2012; pp. 17–30. ISBN 9781449628109 1449628109. [Google Scholar]
- Watson, J. Watson’s theory of human carıng and subjectıve lıvıng experıences: Caratıve factors/carıtas processes as a dıscıplınary guıde to the professıonal nursıng practıce. Texto Contexto Enferm. 2007, 16, 129–135. [Google Scholar] [CrossRef]
- Sitzman, K.; Watson, J. Assessing and Measuring Caring in Nursing and Health Sciences: Watson’s Caring Science Guide, 3rd ed.; Springer Publishing Company: New York, NY, USA, 2019; pp. 251–270. ISBN 978-0-8261-9542-5. [Google Scholar]
- Lechleitner, R.A. Study to Assess Home Health Nurses from a Carative Perspective. Hosp. Top. 2019, 97, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.; Fazzone, P.A.; Sitzman, K.; Hardin, S.R. The Current Intervention Studies Based on Watson’s Theory of Human Caring: A Systematic Review. Int. J. Hum. Caring 2019, 23, 4–22. [Google Scholar] [CrossRef]
- Rodrigues, M.G.D.R.; Séchaud, L. Caring Models in Geriatric Rehabilitation. Holist. Nurs. Pract. 2019, 33, 237–253. [Google Scholar] [CrossRef]
- Feo, R.; Conroy, T.; Wiechula, R.; Rasmussen, P.; Kitson, A. Instruments measuring behavioural aspects of the nurse-patient relationship: A scoping review. J. Clin. Nurs. 2020, 29, 1808–1821. [Google Scholar] [CrossRef] [PubMed]
- Cossette, S.; Cara, C.; Ricard, N.; Pepin, J. Assessing nurse–patient interactions from a caring perspective: Report of the development and preliminary psychometric testing of the Caring Nurse–Patient Interactions Scale. Int. J. Nurs. Stud. 2005, 42, 673–686. [Google Scholar] [CrossRef]
- Aupia, A.; Lee, T.-T.; Liu, C.-Y.; Wu, S.-F.V.; Mills, M.A. Caring behavior perceived by nurses, patients and nursing students in Indonesia. J. Prof. Nurs. 2018, 34, 314–319. [Google Scholar] [CrossRef]
- Vujanić, J.; Prlić, N.; Lovrić, R. Nurses’ Self-Assessment of Caring Behaviors in Nurse-Patient Interactions: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 5255. [Google Scholar] [CrossRef]
- Lovrić, R.; Prlić, N.; Milutinović, D.; Marjanac, I.; Žvanut, B. Changes in nursing students’ expectations of nursing clinical faculties’ competences: A longitudinal, mixed methods study. Nurse Educ. Today 2017, 59, 38–44. [Google Scholar] [CrossRef]
- Creative Research Systems. Sample Size Calculator. Available online: https://www.surveysystem.com/ (accessed on 25 February 2021).
- Suliman, W.A.; Welmann, E.; Omer, T.; Thomas, L. Applying Watson’s Nursing Theory to Assess Patient Perceptions of Being Cared for in a Multicultural Environment. J. Nurs. Res. 2009, 17, 293–300. [Google Scholar] [CrossRef]
- Calong, K.A.; Soriano, G.P. Construct Validity and Reliability of Caring Nurse Patient Interaction Scale-Nurse among Filipino Nurses. Int. J. Caring Sci. 2019, 12, 1017–1022. [Google Scholar]
- Papastavrou, E.; Efstathiou, G.; Tsangari, H.; Suhonen, R.; Leino-Kilpi, H.; Patiraki, E.; Karlou, C.; Balogh, Z.; Palese, A.; Tomietto, M.; et al. A cross-cultural study of the concept of caring through behaviours patients’ and nurses’ perspectives in six different EU countries. J. Adv. Nurs. 2012, 68, 1026–1037. [Google Scholar] [CrossRef]
- Sossong, A.; Poirier, P. Patient and nurse perceptions of caring in rural United States. Int. J. Hum. Caring 2013, 17, 79–85. [Google Scholar] [CrossRef]
- Merrill, A.S.; Hayes, J.S.; Clukey, L.; Curtis, D. Do they really care? How trauma patients perceive nurses’ caring behaviors. J. Trauma Nurs. 2012, 19, 3–37. [Google Scholar] [CrossRef] [PubMed]
- Lynn, M.L. Understanding and measuring patients’ assessment of the quality of nursing care. Nurs. Res. 2007, 56, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Norman, V.; Rossillo, K.; Skelton, K. Creating healing environments through the theory of caring. AORN J. 2016, 104, 400–409. [Google Scholar] [CrossRef]
- Lotfi, M.; Zamanzadeh, V.; Valizadeh, L.; Khajehgoodari, M. Assessment of nurse–patient communication and patient satisfaction from nursing care. Nurs. Open 2019, 6, 1189–1196. [Google Scholar] [CrossRef]
- Chan, E.A.; Wong, F.; Cheung, M.Y.; Lam, W. Patients’ perceptions of their experiences with nurse-patient communication in oncology settings: A focused ethnographic study. PLoS ONE 2018, 13, e0199183. [Google Scholar] [CrossRef]
- Tay, L.H.; Hegney, D.; Ang, E. Factors affecting effective communication between registered nurses and adult cancer patients in an inpatient setting: A systematic review. Int. J. Evid.-Based Healthc. 2011, 9, 151–164. [Google Scholar] [CrossRef]
- Song, Y.; Lv, X.; Liu, J.; Huang, D.; Hong, J.; Wang, W.; Wang, W. Experience of nursing support from the perspective of patients with cancer in mainland China. Nurs. Health Sci. 2016, 18, 510–518. [Google Scholar] [CrossRef]
- Jiang, L.L.; Ruan, H.; Xiang, X.J.; Jia, Q. Investigation and analysis of the caring attitude and behaviour of nurses in Shanghai, China. Int. J. Nurs. Pract. 2014, 21, 426–432. [Google Scholar] [CrossRef]
- Youssef, H.A.M.; Mansour, M.A.M.; Ayasreh, I.R.A.; Al-Mawajdeh, N.A.A. A Medical-Surgical Nurse’s Perceptions of Caring Behaviors among Hospitals in Taif City. Life Sci. 2013, 10, 720–730. [Google Scholar]
- Locsin, R.C. The Co-Existence of Technology and Caring in the Theory of Technological Competency as Caring in Nursing. J. Med. Investig. 2017, 64, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; Davidson, C.L.; Panik, A.; Buckenmyer, C.; Delpais, P.; Ortiz, M. An examination of ESI triage scoring accuracy in relationship of ED nursing attitudes and experience. J. Emerg. Nurs. 2014, 40, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Adams, L.Y.; Maykut, C.A. Bullying: The antithesis of caring, acknowledging the dark side of the nursing profession. Int. J. Caring Sci. 2015, 8, 765–773. [Google Scholar]
- Berquist, R.; St-Pierre, I.; Holmes, D. Uncaring nurses: Mobilizing power, knowledge, difference and resistance to explain workplace violence in academia. Res. Theory Nurs. Pract. 2018, 32, 199–215. [Google Scholar] [CrossRef]
- Romyn, A.; Rush, K.L.; Hole, R. Vascular access transition: Experiences of patients on hemodialysis. Nephrol. Nurs. J. 2015, 42, 445–453. [Google Scholar]
- Thomas, D.; Newcomb, P.; Fusco, P. Perception of Caring Among Patients and Nurses. J. Patient Exp. 2019, 6, 194–200. [Google Scholar] [CrossRef]
- Kullberg, A.; Sharp, L.; Johansson, H.; Bergenmar, M. Information exchange in oncological inpatient care—Patient satisfaction, participation, and safety. Eur. J. Oncol. Nurs. 2015, 19, 142–147. [Google Scholar] [CrossRef]
- Ghafouri Fard, M.; Haririan, H.; Aghajanloo, A.; Akbari, M.; Shirvani, Y. Obstacles of Nursing Process Application from Perspective of the Nursing Instructor and Nursing Students in Zanjan Faculty of Nursing and Midwifery. J. Med. Educ. Dev. 2012, 5, 69–77. [Google Scholar]
- Miskir, Y.; Emishaw, S. Determinants of Nursing Process Implementation in North East Ethiopia: Cross-Sectional Study. Nurs. Res. Pract. 2018, 2018, 7940854. [Google Scholar] [CrossRef]
- Thorup, C.B.; Rundqvist, E.; Roberts, C.; Delmar, C. Care as a matter of courage: Vulnerability, suffering and ethical formation in nursing care. Scand. J. Caring Sci. 2011, 26, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Dobrowolska, B.; Palese, A. The caring concept, its behaviours and obstacles: Perceptions from a qualitative study of undergraduate nursing students. Nurs. Inq. 2016, 23, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, D.; Çinar, H.G. Hemşirelik bölümü son sınıf öğrencilerinin bakım odaklı hemşire-hasta etkileşimine yönelik tutmlarının incelenmesi. J. Hum. Sci. 2017, 14, 3300–3309. [Google Scholar] [CrossRef][Green Version]
- Cervantes, L.; Zoucha, J.; Jones, J.; Fischer, S. Experiences and values of Latinos with end stage renal disease: A systematic review of qualitative studies. Nephrol. Nurs. J. 2016, 43, 479–493. [Google Scholar]
- Nasim, A.; Chrysoula, D. Investigating the perceptions of nurses and patients for the nursing care provided and received in a hospital setting. J. Nurs. Healthc. Res. 2020, 9, 8–15. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 369, 1328–1329. [Google Scholar] [CrossRef]
- Vandenhouten, C.; Kubsch, S.; Peterson, M.; Murdock, J.; Lehrer, L. Watson’s theory of transpersonal caring: Factors impacting nurses professional caring. Holist. Nurs. Pract. 2012, 26, 326–334. [Google Scholar] [CrossRef]
- Li, Y.S.; Yu, W.P.; Yang, B.H.; Liu, C.F. A comparison of the caring behaviours of nursing students and registered nurses: Implications for nursing education. J. Clin. Nurs. 2016, 25, 3317–3325. [Google Scholar] [CrossRef]
| Carative Factors (F1–F10) | Description |
|---|---|
| F1—Humanism | Formation of a humanistic-altruistic system of values. Humanistic-altruistic feelings and acts provide the basis of human caring and promote the best professional care, and as such, constitute the first and most basic factor for science and ethic of caring. |
| F2—Hope | Instillation of faith-hope. In this carative factor (CF), patients’ beliefs are encouraged, honored, and respected as significant influences in promoting and maintaining health. |
| F3—Sensibility | Cultivation of sensitivity to one’s self and to others. Nurses who recognize and use their sensitivity promote self-development and self-actualization and are able to encourage the same growth in others. Without this factor, nursing care would fall. |
| F4—Helping relationship | Development of a helping-trusting, human caring relationship. The human caring relationship is transpersonal. In that it connotes a special kind of relationship: a connection with the other person, a high regard for the whole person, and their being-in-the-world. |
| F5—Expression of emotions | Promotion and acceptance of the expression of positive and negative feelings. The caring relationship can move to a deeper, more honest, and authentic level if the nurse allows for this CF. |
| F6—Problem solving | Systematic use of a creative problem-solving caring process. This process involves full use of self and all of one’s faculties, knowledge, instincts, intuition, aesthetics, technology, skills, empirics, ethics, personal, and even spiritual knowing. |
| F7—Teaching | Promotion of transpersonal teaching–learning. This CF makes explicit that learning is more than just receiving information and data. It involves a caring relationship as context for any teaching learning. |
| F8—Environment | Provision for a supportive, protective and/or corrective mental, physical, societal, and spiritual environment. The areas that involve this factor are: comfort, privacy, safety, cleanliness, and aesthetic surroundings. |
| F9—Needs | Assistance with the gratification of human needs. All needs are equally important and must be valued and responded to for caring-healing. |
| F10—Spirituality | Allowance for existential–phenomenological–spiritual forces. This CF allows for spiritual filled meanings and unknowns to emerge open to infinite possibilities for miracles. |
| Respondents Characteristics | Number (%) | |
|---|---|---|
| Gender | male | 151 (51.9) |
| female | 140 (48.1) | |
| Age (years) | 18–40 | 38 (13.1) |
| 41–60 | 87 (29.9) | |
| 61–90 | 166 (57.0) | |
| Place of Residence | urban | 146 (50.2) |
| rural | 145 (49.8) | |
| Level of Education | elementary school | 70 (24.1) |
| high school | 189 (64.9) | |
| higher education | 32 (11.0) | |
| Department | Traumatology and Orthopedics | 56 (19.2) |
| Surgery | 22 (7.6) | |
| Gynecologic Oncology | 30 (10.3) | |
| Urology | 23 (7.9) | |
| Otorhinolaryngology | 18 (6.2) | |
| Oncology | 66 (22.7) | |
| Internal Clinic—Cardiology | 76 (26.1) | |
| Number of hospitalizations | 1–2 | 123 (42.3) |
| 3–5 | 128 (44.0) | |
| 6 and more | 40 (13.7) | |
| Respondents Characteristics | Number (%) | |
|---|---|---|
| Gender | Male | 25 (16.1) |
| Female | 130 (83.9) | |
| Age (years) | 18–25 | 28 (18.1) |
| 26–40 | 54 (34.8) | |
| >40 | 73 (47.1) | |
| Place of Residence | Urban | 96 (61.9) |
| Rural | 59 (38.1) | |
| Level of Education | General Nurses (VET) | 112 (72.3) |
| BSc nurses | 43 (27.7) | |
| Length of Service (years) | ≤5 | 38 (24.5) |
| 6–20 | 45 (29.0) | |
| >21 | 72 (46.5) | |
| Workplace | Traumatology and Orthopedics | 40 (25.8) |
| Surgery | 34 (21.9) | |
| Gynecologic Oncology | 15 (9.7) | |
| Urology | 7 (4.5) | |
| Otorhinolaryngology | 11 (7.1) | |
| Oncology | 21 (13.5) | |
| Internal Clinic—Cardiology | 27 (17.4) | |
| Carative Factors (F1–F10) | Patient Perception | Nurses’ Perception | p * | ||
|---|---|---|---|---|---|
| Average | SD | Average | SD | ||
| F1—Humanism | 4.30 | 0.65 | 4.08 | 0.56 | <0.001 |
| F2—Hope | 4.46 | 0.59 | 4.25 | 0.51 | <0.001 |
| F3—Sensibility | 4.28 | 0.70 | 3.86 | 0.64 | <0.01 |
| F4—Helping relationship | 4.33 | 0.65 | 4.15 | 0.58 | <0.01 |
| F5—Expression of emotions | 4.35 | 0.66 | 4.04 | 0.62 | <0.001 |
| F6—Problem solving | 4.28 | 0.74 | 3.99 | 0.63 | <0.001 |
| F7—Teaching | 4.40 | 0.62 | 4.11 | 0.55 | <0.001 |
| F8—Environment | 4.45 | 0.61 | 4.36 | 0.55 | 0.132 |
| F9—Needs | 4.62 | 0.47 | 4.49 | 0.46 | <0.01 |
| F10—Spirituality | 4.29 | 0.57 | 4.18 | 0.57 | 0.109 |
| In total (CNPI-70) | 4.39 | 0.48 | 4.17 | 0.46 | <0.001 |
| Patients | Predictors | Criteria (Respondents’ Perceptions) | |
| * β | p | ||
| age | 0.046 | 0.446 | |
| gender | 0.000 | 0.994 | |
| level of education | −0.049 | 0.415 | |
| place of residence (urban/rural) | 0.109 | 0.067 | |
| department | 0.070 | 0.252 | |
| number of hospitalizations | −0.056 | 0.353 | |
| Regression model † R = 0.149, ‡ R2 = 0.022, § R2corr. = 0.002, ||F (5.289) = 1.07, p = 0.379 | |||
| Nurses | age | 0.128 | 0.759 |
| level of education | 0.084 | 0.308 | |
| place of residence (urban/rural) | −0.002 | 0.998 | |
| workplace (department) | −0.015 | 0.855 | |
| length of service | −0.101 | 0.807 | |
| Regression model † R = 0.135, ‡ R2 = 0.018, § R2kor = −0.015, ||F (4.154) = 0.55, p = 0.738 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vujanić, J.; Mikšić, Š.; Barać, I.; Včev, A.; Lovrić, R. Patients’ and Nurses’ Perceptions of Importance of Caring Nurse–Patient Interactions: Do They Differ? Healthcare 2022, 10, 554. https://doi.org/10.3390/healthcare10030554
Vujanić J, Mikšić Š, Barać I, Včev A, Lovrić R. Patients’ and Nurses’ Perceptions of Importance of Caring Nurse–Patient Interactions: Do They Differ? Healthcare. 2022; 10(3):554. https://doi.org/10.3390/healthcare10030554
Chicago/Turabian StyleVujanić, Jasenka, Štefica Mikšić, Ivana Barać, Aleksandar Včev, and Robert Lovrić. 2022. "Patients’ and Nurses’ Perceptions of Importance of Caring Nurse–Patient Interactions: Do They Differ?" Healthcare 10, no. 3: 554. https://doi.org/10.3390/healthcare10030554
APA StyleVujanić, J., Mikšić, Š., Barać, I., Včev, A., & Lovrić, R. (2022). Patients’ and Nurses’ Perceptions of Importance of Caring Nurse–Patient Interactions: Do They Differ? Healthcare, 10(3), 554. https://doi.org/10.3390/healthcare10030554







