The Optimization of HIV Testing in Eastern Indonesia: Findings from the 2017 Indonesian Demographic and Health Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
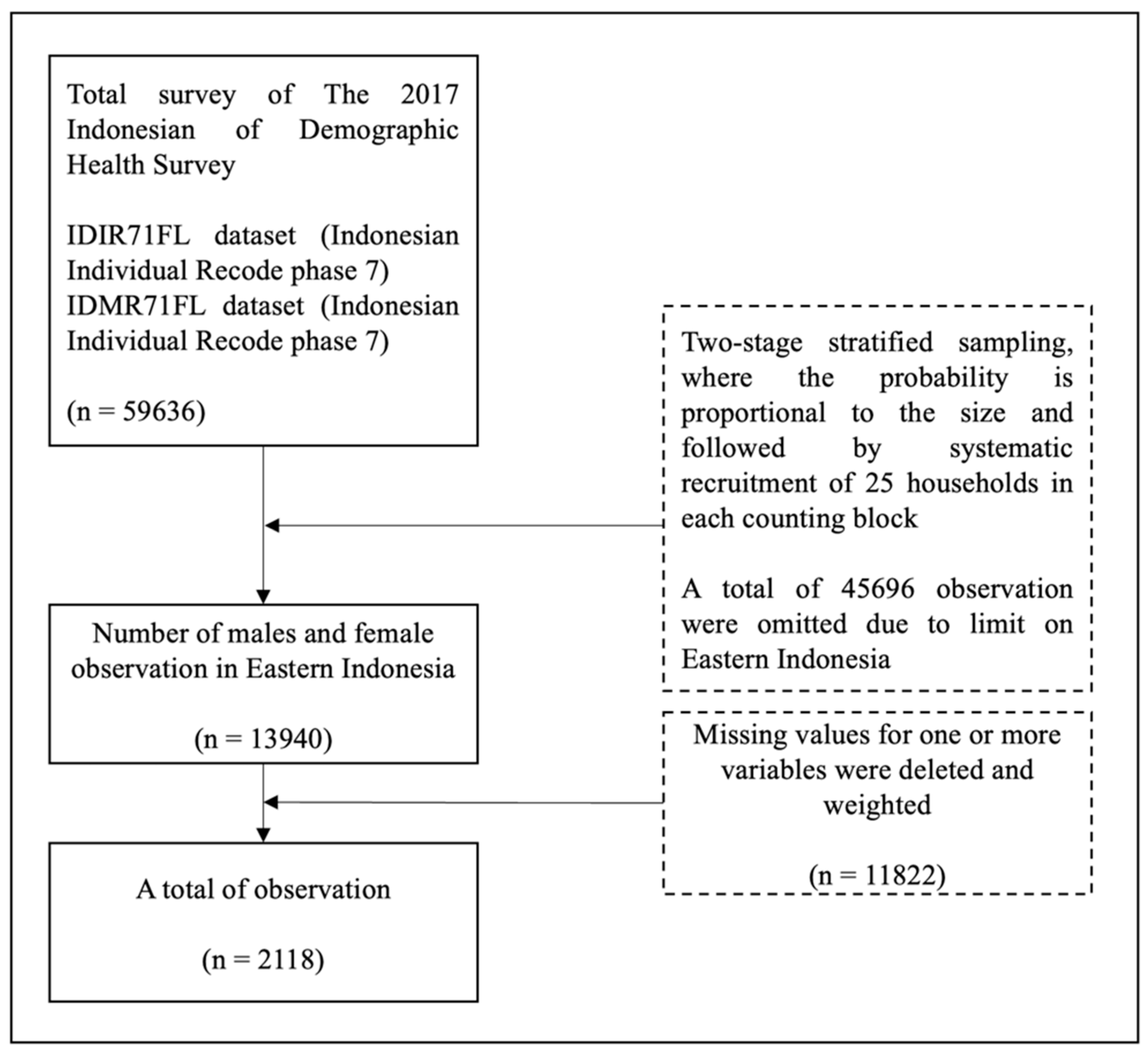
2.2. Data Sources and Sample
2.3. Variables
2.4. Data Analysis
2.5. Ethical Consideration
3. Results
4. Discussion
4.1. Limitations
4.2. Recommendation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roberts, J.; Soehoed, R.; Au, M.; Nguyen, N.T.M.; Andriansyah, R. Midterm Evaluation of Usaid/Indonesia Linkages Program; United States Agency: Washington, DC, USA, 2017; pp. 7–12.
- Thompson, M. The first 90: The gateway to prevention and care: Opening slowly, but not for all. Curr. Opin. HIV AIDS 2019, 14, 486–493. [Google Scholar] [CrossRef] [PubMed]
- Unaids. Understanding Fast-Tract Accelerating Action to End the AIDS Epidemic by 2030; UNAIDS: Geneva, Switzerland, 2015. [Google Scholar]
- Unaids. AIDS and The Sustainable Development Goals. Available online: https://www.unaids.org/en/AIDS_SDGs (accessed on 3 March 2022).
- Riskesdas. Hasil Utama Riset Kesehatan Dasar Tahun 2018; Kementrian Kesehatan Republik Indonesia: Jakarta, Indonesia, 2018; pp. 1–100.
- WHO. HIV AIDS (Auckl) 2020; WHO: Macclesfield, UK, 2020. [Google Scholar]
- Munro, J.; Butt, L. Compelling Evidence: Research Methods, HIV/AIDS, and Politics in Papua, Indonesia. Asia Pac. J. Anthropol. 2012, 13, 334–351. [Google Scholar] [CrossRef]
- Deussom, R. Optimizing Indonesia’s Health Workforce to Advance the “Test and Treat” Policy for Sustained Epidemic Control. Available online: https://hrh2030program.org/optimizing-indonesias-health-workforce-to-advance-the-test-and-treat-policy-for-sustained-epidemic-control/ (accessed on 11 July 2021).
- Pradnyani, P.; Januraga, P.; Mahmudah, M.; Wibowo, A. Peer support and access to information as predictors of HIV testing among indirect female sex workers in Bali, Indonesia. HIV AIDS Rev. 2020, 19, 206–211. [Google Scholar] [CrossRef]
- Napirah, M.R.; Rahman, A.; Tony, A. Faktor-faktor yang berhubungan dengan pemanfaatan pelayanan kesehatan di wilayah kerja Puskesmas Tambarana Kecamatan Poso Pesisir Utara Kabupaten Poso. J. Pengemb. Kota 2016, 4, 29–39. [Google Scholar] [CrossRef]
- Apers, H.; Nöstlinger, C.; Van Beckhoven, D.; Deblonde, J.; Apers, L.; Verheyen, K.; Loos, J. Identifying key elements to inform HIV-testing interventions for primary care in Belgium. Health Promot. Int. 2020, 35, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Bulman, J.; Goode, D.; Evans, A. P203 HIV-Testing African Service Users within a Newly Integrated Sexual Health Service-Our Experience. BMJ J. 2016, 92, A87. [Google Scholar] [CrossRef][Green Version]
- Hensen, B.; Taoka, S.; Lewis, J.J.; Weiss, H.A.; Hargreaves, J. Systematic review of strategies to increase men’s HIV-testing in sub-Saharan Africa. AIDS 2014, 28, 2133–2145. [Google Scholar] [CrossRef]
- Traynor, S.M.; Rosen-Metsch, L.; Feaster, D.J. Missed Opportunities for HIV Testing Among STD Clinic Patients. J. Community Health 2018, 43, 1128–1136. [Google Scholar] [CrossRef]
- Olii, N.; Arifin, H.; Kurniawati, Y.; Rasyid, P.S.; Badjuka, B.Y.M.; Lee, B.O. The utilization profile of place for HIV testing in Indonesia: A nationwide study. J. HIV/AIDS Soc. Serv. 2021, 20, 319–329. [Google Scholar] [CrossRef]
- Ministry of Health Republic Indonesia. HIV Epidemiologi Review Indonesia 2016; Kemenkes: Jakarta, Indonesia, 2017; pp. 26–29. [Google Scholar]
- Riono, P.; Challacombe, S.J. HIV in Indonesia and in neighbouring countries and its social impact. Oral Dis. 2020, 26, 28–33. [Google Scholar] [CrossRef]
- Sianturi, E.I.; Perwitasari, D.A.; Islam, M.A.; Taxis, K. The association between ethnicity, stigma, beliefs about medicines and adherence in people living with HIV in a rural area in Indonesia. BMC Public Health 2019, 19, 55. [Google Scholar] [CrossRef]
- Arinaitwe, I.; Amutuhaire, H.; Atwongyeire, D.; Tusingwire, E.; Kawungezi, P.C.; Rukundo, G.Z.; Ashaba, S. Social Support, Food Insecurity, and HIV Stigma Among Men Living with HIV in Rural Southwestern Uganda: A Cross-Sectional Analysis. HIV AIDS 2021, 13, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Sianturi, E.I.; Perwitasari, D.A.; Soltief, S.N.; Atiqul Islam, M.; Geboers, B.; Taxis, K. Health literacy of people living with HIV in a rural area in Indonesia: A cross-sectional study. Health Soc. Care Community 2021, 29, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Deussom, R.H.; Rottach, E.; Prabawanti, C.; Rahmat, E.; Rachmawati, T.; Sirajulmunir, N. Health Workforce Assessment in Jakarta for Effective HIV Policy Implementation: Challenges and Opportunities toward Epidemic Control. J. Ekon. Kesehat. Indones. 2019, 3, 84–93. [Google Scholar] [CrossRef]
- The World Bank. The World Bank in Indonesia: Having Maintained Political Stability, Indonesia is One of East Asia Pacific’s Most Vibrant Democracies, Emerging as a Confident Middle-Income Country. Available online: https://www.worldbank.org/en/country/indonesia/overview#1 (accessed on 12 August 2021).
- Sulistyono, R.E.; Susanto, T.; Tristiana, R.D. Patients Experience and Perception in Preventing Tuberculosis Transmission in Rural Areas: A Qualitative Research. J. Keperawatan Padjadjaran 2020, 8, 21–30. [Google Scholar] [CrossRef]
- ICF. Indonesia Demographic and Health Survey 2017; BKKBN, BPS, Kemenkes, and ICF: Jakarta, Indonesia, 2018. [Google Scholar]
- Lavrakas, P.J. Weighting—Encyclopedia of Survey Research Methods; Sage Publications: Thousand Oaks, CA, USA, 2008; Volume 1. [Google Scholar]
- Croft, T.N.; Marshall, A.M.J.; Allen, C.K. Guide to DHS Statistics; ICF International: Rockville, MD, USA, 2018; pp. 22–51. [Google Scholar]
- Macro International. Trends in Demographic and Reproductive Health Indicators in Ethiopia: Further Analysis of the 2000 and 2005 Demographic and Health Surveys Data; Macro International: Calverton, MD, USA, 2007. [Google Scholar]
- Kemenkes, Peraturan Menteri Kesehatan Republic Indonesia tentang Penanggulangan HIV AIDS; Kemenkes: Jakarta, Indonesia, 2013.
- Health Ministry of Republic Indonesia. Age Classification Based on Category; Ditjen Yankes: Jakarta, Indonesia, 2009. [Google Scholar]
- Croft, N.T.; Marshall, A.M.J.; Allen, C.K. Guide to DHS Statistics (Version 2); ICF International: Rockville, MD, USA, 2018; pp. 32–37. [Google Scholar]
- Demographic and Health Survey. Wealth Quintiles. Available online: https://dhsprogram.com/data/Guide-to-DHS-Statistics/Wealth_Quintiles.htm (accessed on 19 July 2021).
- Vyas, S.; Kumaranayake, L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006, 21, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Kementerian Pendidikan dan Kebudayaan. UU No. 20; Tahun 2003 Tentang Sistem Pendidikan Nasional; Kemendikbud: Jakarta, Indonesia, 2003; pp. 1–38. [Google Scholar]
- Badan Pusat Statistik. Peraturan Kepala Badan Pusat Statistik Nomor 37 Tahun 2010 Tentang Klasifikasi Perkotaan dan Perdesaan di Indonesia; BPS: Jakarta, Indonesia, 2010; pp. 1–4. [Google Scholar]
- DHS. Demographic Health Survey—Guide to DHS Statistics DHS-7. Available online: https://dhsprogram.com/data/Guide-to-DHS-Statistics/Guide_to_DHS_Statistics_DHS-7.htm (accessed on 19 July 2021).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS medicine 2007, 4, e296. [Google Scholar] [CrossRef]
- Gray, C.; Crawford, G.; Lobo, R.; Maycock, B. Co-Designing an Intervention to Increase HIV Testing Uptake with Women from Indonesia At-Risk of HIV: Protocol for a Participatory Action Research Study. Methods Protoc. 2019, 2, 41. [Google Scholar] [CrossRef]
- Koirala, S.; Deuba, K.; Nampaisan, O.; Marrone, G.; Ekström, A.M.; CAT-S group. Facilitators and barriers for retention in HIV care between testing and treatment in Asia—A study in Bangladesh, Indonesia, Lao, Nepal, Pakistan, Philippines and Vietnam. PLoS ONE 2017, 12, e0176914. [Google Scholar] [CrossRef]
- Nursalam, N.; Sukartini, T.; Arifin, H.; Pradipta, R.O.; Mafula, D.; Ubudiyah, M. Determinants of the discriminatory behavior experienced by people living with HIV in Indonesia: A cross-sectional study of the demographic health survey. Open AIDS J. 2021, 15, 1–9. [Google Scholar] [CrossRef]
- Ante-Testard, P.A.; Benmarhnia, T.; Bekelynck, A.; Baggaley, R.; Ouattara, E.; Temime, L.; Jean, K. Temporal trends in socioeconomic inequalities in HIV testing: An analysis of cross-sectional surveys from 16 sub-Saharan African countries. Lancet Glob. Health 2020, 8, e808–e818. [Google Scholar] [CrossRef]
- Worku, M.G.; Teshale, A.B.; Tesema, G.A. Prevalence and Associated Factors of HIV Testing Among Pregnant Women: A Multilevel Analysis Using the Recent Demographic and Health Survey Data from 11 East African Countries. HIV/AIDS-Res. Palliat. Care 2021, 13, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, K.; Lindayani, L.; Emaliyawati, E.; Rahayu, U.; Nuraeni, A. Factors associated with adherence to antiretroviral therapy among people living with HIV infection in West Java Province, Indonesia. Malays. J. Med. Health Sci. 2020, 16, 209–214. [Google Scholar]
- Alfian, A.; Ibrahim, K.; Rafiyah, I. The Effect of the E-Patuh Application on HIV/Aids Patients’ Adherence in Consuming Antiretroviral. J. Keperawatan Padjadjaran 2019, 7, 49–57. [Google Scholar] [CrossRef]
- Sukartini, T.; Nursalam, N.; Arifin, H. The determinants of willingness to care for people living with HIV-AIDS: A cross-sectional study in Indonesia. Health Soc. Care Community 2021, 29, 809–817. [Google Scholar] [CrossRef]
- Handayani, S.; Andajani, S.; Djuari, L. Determinants of HIV provider-initiated testing and counseling screening service used by pregnant women in primary health centers in Surabaya. Med. J. Indones. 2018, 26, 293–301. [Google Scholar] [CrossRef]
- Perceptions of and barriers to HIV testing of women in Indonesia. Sex. Reprod. Health Matters 2020, 28, 1848003. [CrossRef]
- Thapa, S.; Hannes, K.; Cargo, M.; Buve, A.; Peters, S.; Dauphin, S.; Mathei, C. Stigma reduction in relation to HIV test uptake in low- and middle-income countries: A realist review. BMC Public Health 2018, 18, 1277. [Google Scholar] [CrossRef]


| Variable | n | % |
|---|---|---|
| HIV Test | ||
| No | 1519 | 71.72 |
| Yes | 599 | 28.28 |
| Region | ||
| Sulawesi | 1367 | 64.54 |
| Maluku | 437 | 20.63 |
| Papua | 314 | 14.83 |
| Age | ||
| 50–54 years | 41 | 1.94 |
| 35–49 years | 943 | 44.52 |
| 25–34 years | 752 | 35.51 |
| 15–24 years | 382 | 18.04 |
| Gender | ||
| Male | 425 | 20.07 |
| Female | 1693 | 79.93 |
| Wealth Index | ||
| Poorest | 382 | 18.04 |
| Poorer | 406 | 19.17 |
| Middle | 377 | 17.8 |
| Richer | 464 | 21.91 |
| Richest | 489 | 23.09 |
| Education | ||
| Higher education | 1046 | 49.39 |
| Secondary education | 930 | 43.91 |
| Primary education | 136 | 6.42 |
| No education | 6 | 0.28 |
| Residence | ||
| Urban | 1100 | 51.94 |
| Rural | 1018 | 48.06 |
| Respondents working | ||
| No | 162 | 7.65 |
| Yes | 1956 | 92.35 |
| Respondents earning | ||
| No | 279 | 13.17 |
| Yes | 1839 | 86.83 |
| Stigma | ||
| No | 1435 | 67.75 |
| Yes | 683 | 32.25 |
| Knowledge | ||
| No | 66 | 3.12 |
| Some | 540 | 25.5 |
| More | 1512 | 71.39 |
| Information | ||
| No | 587 | 27.71 |
| Some | 890 | 42.02 |
| More | 641 | 30.26 |
| Variable | Eastern Indonesia | |||||
|---|---|---|---|---|---|---|
| Sulawesi | Maluku | Papua | ||||
| n | % | n | % | n | % | |
| HIV Test | ||||||
| No | 1001 | 73.23 | 314 | 71.85 | 204 | 64.97 |
| Yes | 366 | 26.77 | 123 | 28.15 | 110 | 35.03 |
| Age | ||||||
| 50–54 years | 32 | 2.34 | 3 | 0.69 | 6 | 1.91 |
| 35–49 years | 606 | 44.33 | 200 | 45.77 | 137 | 43.63 |
| 25–34 years | 468 | 34.24 | 160 | 36.61 | 124 | 39.49 |
| 15–24 years | 261 | 19.09 | 74 | 16.93 | 47 | 14.94 |
| Gender | ||||||
| Male | 268 | 19.60 | 75 | 17.16 | 82 | 26.11 |
| Female | 1099 | 80.40 | 362 | 82.84 | 232 | 73.89 |
| Wealth Index | ||||||
| Poorest | 180 | 13.17 | 117 | 26.77 | 85 | 27.07 |
| Poorer | 245 | 17.92 | 95 | 21.74 | 66 | 21.02 |
| Middle | 222 | 16.24 | 90 | 20.59 | 65 | 20.70 |
| Richer | 309 | 22.60 | 91 | 20.82 | 64 | 20.38 |
| Richest | 411 | 30.07 | 44 | 10.07 | 34 | 10.83 |
| Education | ||||||
| High education | 699 | 51.13 | 220 | 50.34 | 127 | 40.45 |
| Secondary education | 573 | 41.92 | 197 | 45.08 | 160 | 50.96 |
| Primary education | 93 | 6.80 | 19 | 4.35 | 24 | 7.64 |
| No education | 2 | 0.15 | 1 | 0.23 | 3 | 0.96 |
| Residence | ||||||
| Urban | 716 | 52.38 | 257 | 58.81 | 127 | 40.45 |
| Rural | 651 | 47.62 | 180 | 41.19 | 187 | 59.55 |
| Respondents working | ||||||
| No | 114 | 8.34 | 21 | 4.81 | 27 | 8.60 |
| Yes | 1253 | 91.66 | 416 | 95.19 | 287 | 91.40 |
| Respondents earning | ||||||
| No | 150 | 10.97 | 67 | 15.33 | 62 | 19.75 |
| Yes | 1217 | 89.03 | 370 | 84.67 | 252 | 80.25 |
| Stigma | ||||||
| No | 968 | 70.81 | 287 | 65.68 | 180 | 57.32 |
| Yes | 399 | 29.19 | 150 | 34.32 | 134 | 42.68 |
| Knowledge | ||||||
| No | 46 | 3.37 | 11 | 2.52 | 9 | 2.87 |
| Some | 338 | 24.73 | 108 | 24.71 | 94 | 29.94 |
| More | 983 | 71.91 | 318 | 72.77 | 211 | 67.20 |
| Information | ||||||
| No | 394 | 28.82 | 126 | 28.83 | 67 | 21.34 |
| Some | 544 | 39.80 | 193 | 44.16 | 153 | 48.73 |
| More | 429 | 31.38 | 118 | 27.00 | 94 | 29.94 |
| Variable | HIV Test | X2 | AOR | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|
| No | Yes | |||||||
| n | % | n | % | Lower | Upper | |||
| Region | ||||||||
| Sulawesi | 1001 | 47.26 | 366 | 17.28 | 8.58 ** | Ref. | ||
| Maluku | 314 | 14.83 | 123 | 5.81 | 1.004 | 0.77 | 1.29 | |
| Papua | 204 | 9.63 | 110 | 5.19 | 1.45 *** | 1.09 | 1.91 | |
| Age | ||||||||
| 50–54 years | 36 | 1.7 | 5 | 0.24 | 10.80 ** | Ref. | ||
| 35–49 years | 692 | 32.67 | 251 | 11.85 | 1.29 | 0.48 | 3.46 | |
| 25–34 years | 535 | 25.26 | 217 | 10.25 | 1.24 | 0.45 | 3.35 | |
| 15–24 years | 256 | 12.09 | 126 | 5.95 | 1.34 | 0.48 | 3.71 | |
| Gender | ||||||||
| Male | 357 | 16.86 | 68 | 3.21 | 39.53 *** | Ref. | ||
| Female | 1162 | 54.86 | 531 | 25.07 | 2.37 *** | 1.75 | 3.12 | |
| Wealth Index | ||||||||
| Poorest | 266 | 12.56 | 116 | 5.48 | 10.11 ** | Ref. | ||
| Poorer | 289 | 13.64 | 117 | 5.52 | 0.92 | 0.67 | 1.28 | |
| Middle | 263 | 12.42 | 114 | 5.38 | 0.95 | 0.68 | 1.32 | |
| Richer | 323 | 15.25 | 141 | 6.66 | 0.93 | 0.66 | 1.3 | |
| Richest | 378 | 17.85 | 111 | 5.24 | 0.61 ** | 0.42 | 0.89 | |
| Education | ||||||||
| Higher education | 734 | 34.66 | 312 | 14.73 | 4.36 | Ref. | ||
| Secondary education | 685 | 32.34 | 245 | 11.57 | 0.98 | 0.78 | 1.23 | |
| Primary education | 97 | 4.58 | 39 | 1.84 | 1.17 | 0.75 | 1.82 | |
| No education | 3 | 0.14 | 3 | 0.14 | 2.71 | 0.51 | 14.38 | |
| Residence | ||||||||
| Urban | 806 | 38.05 | 294 | 13.88 | 2.72 * | Ref. | ||
| Rural | 713 | 33.66 | 305 | 14.4 | 1.09 | 0.88 | 1.35 | |
| Respondents working | ||||||||
| No | 113 | 5.34 | 49 | 2.31 | 0.33 | Ref. | ||
| Yes | 1406 | 66.38 | 550 | 25.97 | 1.15 | 0.79 | 1.67 | |
| Respondents earning | ||||||||
| No | 206 | 9.73 | 73 | 3.45 | 0.7 | Ref. | ||
| Yes | 1313 | 61.99 | 526 | 24.83 | 1.30 * | 0.96 | 1.78 | |
| Stigma | ||||||||
| No | 1023 | 48.3 | 412 | 19.45 | 4.44 ** | Ref. | ||
| Yes | 496 | 5.15 | 187 | 1.32 | 0.65 ** | 0.42 | 1.02 | |
| HIV-related Knowledge | ||||||||
| No | 47 | 23.42 | 19 | 8.83 | 5.14 * | Ref. | ||
| Some | 367 | 17.33 | 173 | 8.17 | 1.18 | 0.66 | 2.1 | |
| More | 1105 | 52.17 | 407 | 19.22 | 0.94 | 0.53 | 1.64 | |
| HIV-related Information | ||||||||
| No | 451 | 21.29 | 136 | 6.42 | 20.21 *** | Ref. | ||
| Some | 648 | 30.59 | 242 | 11.43 | 1.27 * | 0.98 | 1.64 | |
| More | 420 | 19.83 | 221 | 10.43 | 1.88 *** | 1.41 | 2.51 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibrahim, K.; Arifin, H.; Fitri, S.U.R.; Herliani, Y.K.; Harun, H.; Setiawan, A.; Lee, B.-O. The Optimization of HIV Testing in Eastern Indonesia: Findings from the 2017 Indonesian Demographic and Health Survey. Healthcare 2022, 10, 533. https://doi.org/10.3390/healthcare10030533
Ibrahim K, Arifin H, Fitri SUR, Herliani YK, Harun H, Setiawan A, Lee B-O. The Optimization of HIV Testing in Eastern Indonesia: Findings from the 2017 Indonesian Demographic and Health Survey. Healthcare. 2022; 10(3):533. https://doi.org/10.3390/healthcare10030533
Chicago/Turabian StyleIbrahim, Kusman, Hidayat Arifin, Siti Ulfah Rifa’atul Fitri, Yusshy Kurnia Herliani, Hasniatisari Harun, Agus Setiawan, and Bih-O Lee. 2022. "The Optimization of HIV Testing in Eastern Indonesia: Findings from the 2017 Indonesian Demographic and Health Survey" Healthcare 10, no. 3: 533. https://doi.org/10.3390/healthcare10030533
APA StyleIbrahim, K., Arifin, H., Fitri, S. U. R., Herliani, Y. K., Harun, H., Setiawan, A., & Lee, B.-O. (2022). The Optimization of HIV Testing in Eastern Indonesia: Findings from the 2017 Indonesian Demographic and Health Survey. Healthcare, 10(3), 533. https://doi.org/10.3390/healthcare10030533







