Prevalence of Anxiety and Depression among Psychiatric Healthcare Workers during the COVID-19 Pandemic: A Malaysian Perspective
Abstract
:1. Introduction
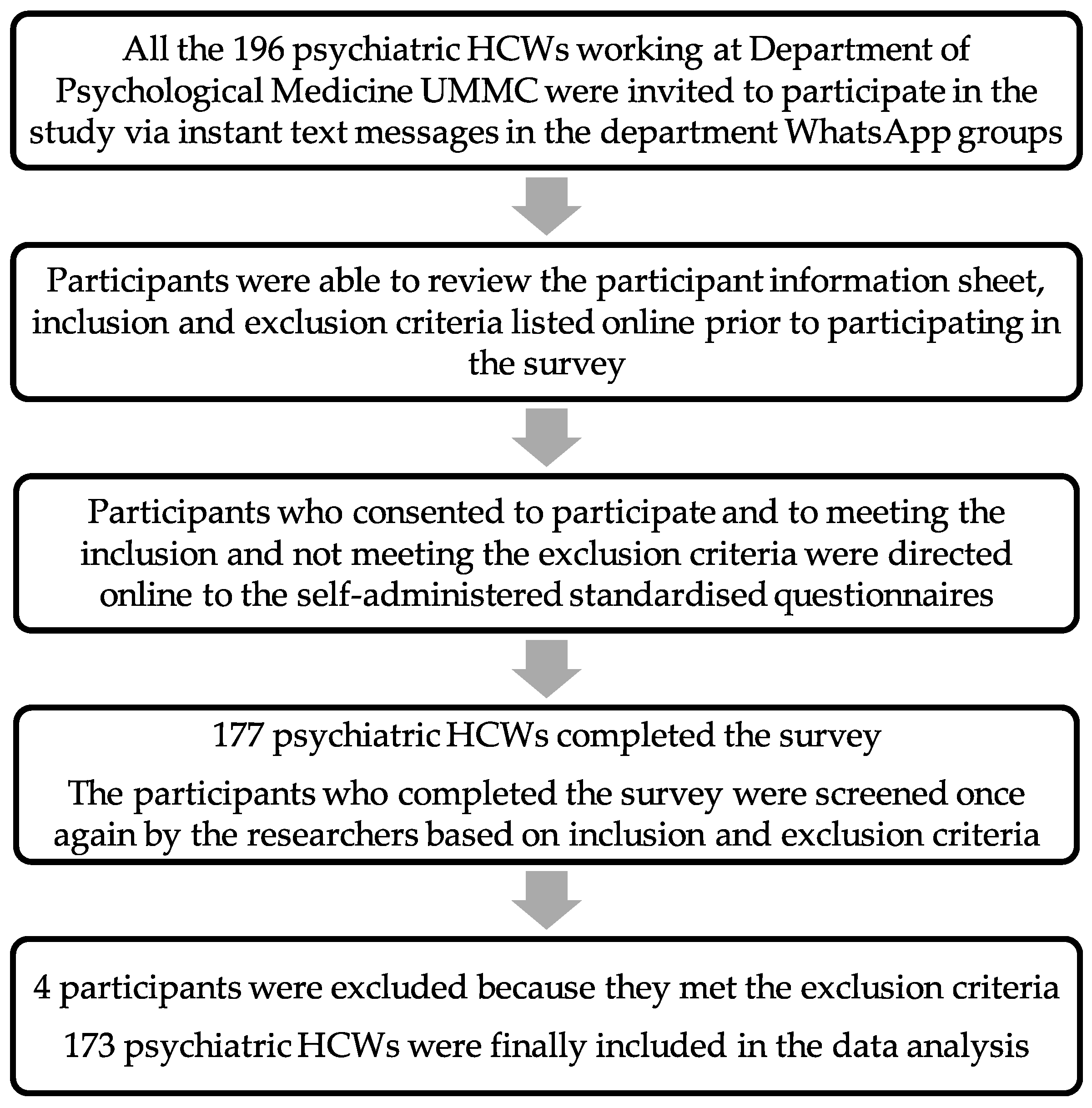
2. Materials and Methods
2.1. Inclusion Criteria
- Psychiatric HCWs who were working at the Department of Psychological Medicine UMMC during the study period from 1 May 2021 till 31 August 2021;
- Available to be contacted via instant text message;
- Able to understand English or Malay language;
- Able to give consent.
2.2. Exclusion Criteria
- Under the age of 18 years old;
- Psychiatric HCWs who had worked for less than two months at the Department of Psychological Medicine UMMC before participating in the study;
- Medical and nursing students who were completing a placement at the Department of Psychological Medicine UMMC during the COVID-19 pandemic;
- Declined to participate in the study.
2.3. Measurement Tools
2.3.1. Hospital Anxiety and Depressive Scale (HADS) English and Malay Version
2.3.2. Brief-COPE English and Malay Version
2.4. Statistical Analyses
2.5. Ethical Considerations
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Elengoe, A. COVID-19 Outbreak in Malaysia. Osong Public Health Res. Perspect. 2020, 11, 93–100. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 4 October 2021).
- Ministry of Health Malaysia. Covid-19 (Maklumat Terkini). Available online: http://www.moh.gov.my/index.php/pages/view/2019-ncov-wuhan (accessed on 4 October 2021).
- Abdullah, J.M.; Wan Ismail, W.F.N.; Mohamad, I.; Ab Razak, A.; Harun, A.; Musa, K.I.; Lee, Y.Y. A Critical Appraisal of COVID-19 in Malaysia and Beyond. Malays. J. Med. Sci. MJMS 2020, 27, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fancourt, D.; Steptoe, A.; Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. Lancet Psychiatry 2021, 8, 141–149. [Google Scholar] [CrossRef]
- Center for Disease Control, C. Morbidity and Mortality Weekly Report (MMWR). 2021. Available online: https://www.cdc.gov/mmwr/index.html (accessed on 10 October 2021).
- Azuddin, A.; Razak, Z.; Omar, N. A Year Of Living Under COVID-19. Part 1: How the Year-Long Pandemic Impacted Malaysians’ Overall Mental and Physical Well-Being. 2021. Available online: https://www.centre.my/post/covid-19-physical-mental-health (accessed on 10 October 2021).
- Holingue, C.; Badillo-Goicoechea, E.; Riehm, K.E.; Veldhuis, C.B.; Thrul, J.; Johnson, R.M.; Fallin, M.D.; Kreuter, F.; Stuart, E.A.; Kalb, L.G. Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: Findings from American trend panel survey. Prev. Med. 2020, 139, 106231. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, R.; Sikhosana, N.; Green, H.; Halcomb, E.J.; Middleton, R.; Alananzeh, I.; Trakis, S.; Moxham, L. Anxiety and depression among healthcare workers during the COVID-19 pandemic: A systematic umbrella review of the global evidence. BMJ Open 2021, 11, e054528. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Sahebi, A.; Nejati-Zarnaqi, B.; Moayedi, S.; Yousefi, K.; Torres, M.; Golitaleb, M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 107, 110247. [Google Scholar] [CrossRef]
- Alnazly, E.; Khraisat, O.M.; Al-Bashaireh, A.M.; Bryant, C.L. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS ONE 2021, 16, e0247679. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.R.; Wang, K.; Yin, L.; Zhao, W.F.; Xue, Q.; Peng, M.; Min, B.Q.; Tian, Q.; Leng, H.X.; Du, J.L.; et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020, 89, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Ilhan, B.; Kupeli, I. Secondary traumatic stress, anxiety, and depression among emergency healthcare workers in the middle of the COVID-19 outbreak: A cross-sectional study. Am. J. Emerg. Med. 2021, 52, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, S.; Hossain, S.; Muyeed, A.; Islam, M.M.; Mohsin, M. The global prevalence of depression, anxiety, stress, and, insomnia and its changes among health professionals during COVID-19 pandemic: A rapid systematic review and meta-analysis. Heliyon 2021, 7, e07393. [Google Scholar] [CrossRef] [PubMed]
- Alshekaili, M.; Hassan, W.; Al Said, N.; Al Sulaimani, F.; Jayapal, S.K.; Al-Mawali, A.; Chan, M.F.; Mahadevan, S.; Al-Adawi, S. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: Frontline versus non-frontline healthcare workers. BMJ Open 2020, 10, e042030. [Google Scholar] [CrossRef] [PubMed]
- Mokhtari, R.; Moayedi, S.; Golitaleb, M. COVID-19 pandemic and health anxiety among nurses of intensive care units. Int. J. Ment. Health Nurs. 2020, 29, 1275–1277. [Google Scholar] [CrossRef] [PubMed]
- Karagol, A.; Kaya, Z.T. Healthcare Workers’ Burn-out, Hopelessness, Fear of COVID-19 and Perceived Social Support Levels. Eur. J. Psychiatry 2022. [Google Scholar] [CrossRef]
- Palgi, Y.; Bergman, Y.S.; Ben-David, B.; Bodner, E. No psychological vaccination: Vaccine hesitancy is associated with negative psychiatric outcomes among Israelis who received COVID-19 vaccination. J. Affect. Disord. 2021, 287, 352–353. [Google Scholar] [CrossRef] [PubMed]
- Shaukat, N.; Ali, D.M.; Razzak, J. Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. Int. J. Emerg. Med. 2020, 13, 40. [Google Scholar] [CrossRef]
- Pang, N.T.P.; Nold Imon, G.; Johoniki, E.; Mohd Kassim, M.A.; Omar, A.; Syed Abdul Rahim, S.S.; Hayati, F.; Jeffree, M.S.; Ng, J.R. Fear of COVID-19 and COVID-19 Stress and Association with Sociodemographic and Psychological Process Factors in Cases under Surveillance in a Frontline Worker Population in Borneo. Int. J. Environ. Res. Public Health 2021, 18, 7210. [Google Scholar] [CrossRef]
- Marvaldi, M.; Mallet, J.; Dubertret, C.; Moro, M.R.; Guessoum, S.B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 126, 252–264. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.E.; Stanton, A.L. Coping resources, coping processes, and mental health. Annu. Rev. Clin. Psychol. 2007, 3, 377–401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roth, S.; Cohen, L.J. Approach, avoidance, and coping with stress. Am. Psychol. 1986, 41, 813–819. [Google Scholar] [CrossRef] [PubMed]
- DeRossett, T.; LaVoie, D.J.; Brooks, D. Religious Coping Amidst a Pandemic: Impact on COVID-19-Related Anxiety. J. Relig. Health 2021, 60, 3161–3176. [Google Scholar] [CrossRef] [PubMed]
- Yusoff, N.; Low, W.Y.; Yip, C.H. Reliability and validity of the Brief COPE Scale (English version) among women with breast cancer undergoing treatment of adjuvant chemotherapy: A Malaysian study. Med. J. Malays. 2010, 65, 41–44. [Google Scholar]
- Lin, J.; Ren, Y.H.; Gan, H.J.; Chen, Y.; Huang, Y.F.; You, X.M. Factors associated with resilience among non-local medical workers sent to Wuhan, China during the COVID-19 outbreak. BMC Psychiatry 2020, 20, 417. [Google Scholar] [CrossRef]
- Francis, B.; Gill, J.S.; Yit Han, N.; Petrus, C.F.; Azhar, F.L.; Ahmad Sabki, Z.; Said, M.A.; Ong Hui, K.; Chong Guan, N.; Sulaiman, A.H. Religious Coping, Religiosity, Depression and Anxiety among Medical Students in a Multi-Religious Setting. Int. J. Environ. Res. Public Health 2019, 16, 259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, G.C.; Mohamed, S.; Sulaiman, A.H.; Zainal, N.Z. Anxiety and Depression in Cancer Patients: The Association with Religiosity and Religious Coping. J. Relig. Health 2017, 56, 575–590. [Google Scholar] [CrossRef] [PubMed]
- Abel, M.H. Interaction of humor and gender in moderating relationships between stress and outcomes. J. Psychol. 1998, 132, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Institute for Public Health, Ministry of Health, Malaysia. National Health and Morbidity Survey 2015 (NHMS 2015). Vol. II: Non-Communicable Diseases, Risk Factors & Other Health Problems. 2015. Available online: https://www.moh.gov.my/moh/resources/nhmsreport2015vol2.pdf (accessed on 8 October 2021).
- Midin, M.D.; Zainal, N.Z.; Lee, T.C.; Ibrahim, N. Mental Health Services in Malaysia. Taiwan. J. Psychiatry 2018, 32, 281–293. Available online: http://www.sop.org.tw/sop_journal/Upload_files/32_4/01.pdf (accessed on 10 October 2021).
- Shields, G.; Ng, R.; Ventriglio, A.; Castaldelli-Maia, J.; Torales, J.; Bhugra, D. WPA Position Statement on Recruitment in Psychiatry. World Psychiatry Off. J. World Psychiatr. Assoc. 2017, 16, 113–114. [Google Scholar] [CrossRef] [PubMed]
- Suarn, S.; Toh, C.L.; Lim, C.H.; Sivasampu, S.; Mazni, M.J.; Azizul, A.; Aizah, S.N.A.; Fatihah, M. National Healthcare Establishment and Workforce Statistics 2011: Psychiatric Services in Malaysian Hospitals; Clinical Research Centre, Ministry of Health: Putrajaya, Malaysia, 2012; pp. 113–127. Available online: https://www.crc.gov.my/wp-content/uploads/documents/report/NHEWS_Hospitals_2010_FullReport.pdf (accessed on 12 October 2021).
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yahya, F.; Othman, Z. Validation of the Malay version of hospital anxiety and depression scale (HADS) in Hospital Universiti Sains Malaysia. Int. Med. J. 2015, 22, 80–82. Available online: http://eprints.usm.my/44323/1/IMJ%202015%3B22%282%2980-82%20Validation%20HADS.pdf (accessed on 12 October 2021).
- Hashim, Z. Reliability and Validatidity of Hospital Anxiety and Depression Scale (HADS) on breast cancer survivors: Malaysia case study. Asia Pac. Environ. Occup. Health J. 2016, 2, 19–24. [Google Scholar]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Rand, K.L.; Cohee, A.A.; Monahan, P.O.; Wagner, L.I.; Shanahan, M.L.; Champion, V.L. Coping Among Breast Cancer Survivors: A Confirmatory Factor Analysis of the Brief COPE. J. Nurs. Meas. 2019, 27, 259–276. [Google Scholar] [CrossRef]
- Eisenberg, S.A.; Shen, B.J.; Schwarz, E.R.; Mallon, S. Avoidant coping moderates the association between anxiety and patient-rated physical functioning in heart failure patients. J. Behav. Med. 2012, 35, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Papathanasiou, I.V.; Tsaras, K.; Kleisiaris, C.F.; Fradelos, E.C.; Tsaloglidou, A.; Damigos, D. Anxiety and Depression in Staff of Mental Units: The Role of Burnout. Adv. Exp. Med. Biol. 2017, 987, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Chow, S.K.; Francis, B.; Ng, Y.H.; Naim, N.; Beh, H.C.; Ariffin, M.A.A.; Yusuf, M.H.M.; Lee, J.W.; Sulaiman, A.H. Religious Coping, Depression and Anxiety among Healthcare Workers during the COVID-19 Pandemic: A Malaysian Perspective. Healthcare 2021, 9, 79. [Google Scholar] [CrossRef] [PubMed]
- Th’ng, F.; Rao, K.A.; Ge, L.; Mao, D.; Neo, H.N.; Molina, J.A.; Seow, E. A One-Year Longitudinal Study: Changes in Depression and Anxiety in Frontline Emergency Department Healthcare Workers in the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 1228. [Google Scholar] [CrossRef] [PubMed]
- Van Steenkiste, E.; Schoofs, J.; Gilis, S.; Messiaen, P. Mental health impact of COVID-19 in frontline healthcare workers in a Belgian Tertiary care hospital: A prospective longitudinal study. Acta Clin. Belg. 2021, 1–8. [Google Scholar] [CrossRef]
- Sahimi, H.M.S.; Mohd Daud, T.I.; Chan, L.F.; Shah, S.A.; Rahman, F.H.A.; Nik Jaafar, N.R. Depression and Suicidal Ideation in a Sample of Malaysian Healthcare Workers: A Preliminary Study During the COVID-19 Pandemic. Front. Psychiatry 2021, 12, 658174. [Google Scholar] [CrossRef]
- Dagan, N.; Barda, N.; Kepten, E.; Miron, O.; Perchik, S.; Katz, M.A.; Hernan, M.A.; Lipsitch, M.; Reis, B.; Balicer, R.D. BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. N. Engl. J. Med. 2021, 384, 1412–1423. [Google Scholar] [CrossRef]
- Tarcan, M.; Hikmet, N.; Schooley, B.; Top, M.; Tarcan, G.Y. An analysis of the relationship between burnout, socio-demographic and workplace factors and job satisfaction among emergency department health professionals. Appl. Nurs. Res. 2017, 34, 40–47. [Google Scholar] [CrossRef]
- Yee, A.; Hodori, N.A.M.; Tung, Y.Z.; Ooi, P.L.; Latif, S.A.B.A.; Isa, H.M.; Ng, D.L.C.; Chai, C.S.; Tan, S.B. Depression level and coping responses toward the movement control order and its impact on quality of life in the Malaysian community during the COVID-19 pandemic: A web-based cross-sectional study. Ann. Gen. Psychiatry 2021, 20, 31. [Google Scholar] [CrossRef] [PubMed]
- Francis, B.; Petrus, C.; Ng, Y.; Sulaiman, A.H.; Gill, J.; Said, M.; Beh, H.C.; Azizah Ariffin, M.; Yusuf, H.; Lee, J. Religious Coping During the COVID-19 Pandemic: Gender, Occupational and Socio-economic Perspectives Among Malaysian Frontline Healthcare Workers. Alpha Psychiatry 2021, 22, 194–199. [Google Scholar] [CrossRef]
- Coiro, M.J.; Watson, K.H.; Ciriegio, A.; Jones, M.; Wolfson, A.R.; Reisman, J.; Compas, B.E. Coping with COVID-19 stress: Associations with depression and anxiety in a diverse sample of U.S. adults. Curr. Psychol. 2021, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Torjesen, I. Covid-19: Mental health services must be boosted to deal with “tsunami” of cases after lockdown. Br. Med. J. 2020, 369, m1994. [Google Scholar] [CrossRef] [PubMed]
- Mikkola, L.; Suutala, E.; Parviainen, H. Social support in the workplace for physicians in specialization training. Med. Educ. Online 2018, 23, 1435114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, B.Y.Q.; Chew, N.W.S.; Lee, G.K.H.; Jing, M.; Goh, Y.; Yeo, L.L.L.; Zhang, K.; Chin, H.K.; Ahmad, A.; Khan, F.A.; et al. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. Ann. Intern. Med. 2020, 173, 317–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norhayati, M.N.; Che Yusof, R.; Azman, M.Y. Depressive symptoms among frontline and non-frontline healthcare providers in response to the COVID-19 pandemic in Kelantan, Malaysia: A cross sectional study. PLoS ONE 2021, 16, e0256932. [Google Scholar] [CrossRef] [PubMed]
- Muller, A.E.; Hafstad, E.V.; Himmels, J.P.W.; Smedslund, G.; Flottorp, S.; Stensland, S.O.; Stroobants, S.; Van de Velde, S.; Vist, G.E. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res. 2020, 293, 113441. [Google Scholar] [CrossRef] [PubMed]
| Variables | n (%) | |
|---|---|---|
| Age (years) a | 36.46 (8.05) | |
| Duration of service (months) a | 147.53 (90.36) | |
| Duration of service in psychiatric department (months) a | 103.57 (86.55) | |
| Ethnicity | ||
| Malay | 126 (72.8) | |
| Non-Malay | 47 (27.2) | |
| Gender | ||
| Female | 118 (68.2) | |
| Male | 55 (31.8) | |
| Education attainment | ||
| Degree and higher | 87 (50.3%) | |
| Diploma and lower | 86 (49.7%) | |
| Medical comorbidity | ||
| No | 148 (85.5) | |
| Yes | 25 (14.5) | |
| Psychiatric history | ||
| No | 126 (72.8) | |
| Yes | 47 (27.2) | |
| Marital status | ||
| Single | 44 (25.4) | |
| Married | 123 (71.1) | |
| Divorce | 6 (3.5 | |
| Number of children | ||
| At least one child | 108 (62.4) | |
| No children | 65 (37.6) | |
| Living arrangements | ||
| Alone | 13 (7.5) | |
| Family | 143 (82.7) | |
| Friend(s) | 17 (9.8) | |
| Living with elderly | ||
| No | 131 (75.7) | |
| Yes | 42 (24.3) | |
| Family member tested positive for COVID-19 | ||
| No | 138 (79.8) | |
| Yes | 35 (20.2) | |
| Household income | ||
| (n = 171) | ||
| Less than RM 4850 (B40 income tier) | 43 (25.1) | |
| RM 4850–RM 10,959 (M40 income tier) | 98 (57.3) | |
| More than RM 10,959 (T20 income tier) | 30 (17.5) | |
| Financial hardship during COVID-19 | ||
| No | 126 (72.8) | |
| Yes, getting worse | 47 (27.2) | |
| Adequate social support | ||
| No | 5 (2.9) | |
| Yes | 168 (97.1) | |
| Occupation | ||
| Doctor | 71 (41.0) | |
| Nurse | 62 (35.8) | |
| Allied Health Professional | 31 (17.9) | |
| Administrative Staff | 9 (5.2) | |
| Work in shift rotation | ||
| No | 106 (61.3) | |
| Yes | 67 (38.7) | |
| Working hours per week | ||
| 45 h or less | 123 (71.1) | |
| 46 h or more | 50 (28.9) | |
| Providing direct care to COVID-19 patients | ||
| No | 132 (76.3) | |
| Yes | 41 (23.7) | |
| Adequate support at workplace | ||
| No | 16 (9.2) | |
| Yes | 157 (90.8) | |
| Increased work burden due to COVID-19 pandemic | ||
| No | 65 (37.6) | |
| Yes | 108 (62.4) | |
| Investigated as close contact for COVID-19 | ||
| No | 117 (67.6) | |
| Yes | 56 (32.4) | |
| Tested for COVID-19 | ||
| No | 106 (61.3) | |
| Yes | 67 (38.7) | |
| Tested positive with COVID-19 | ||
| No | 169 (97.7) | |
| Yes | 4 (2.3) | |
| Perceived at risk group for COVID-19 | ||
| No | 31 (17.9) | |
| Yes | 142 (82.1) | |
| Received COVID-19 vaccination | ||
| No | 20 (11.6) | |
| Yes | 153 (88.4) | |
| Coping | Approach a | 33.63 (9.03) |
| Avoidant a | 21.44 (5.48) | |
| Religion b | 7 (3) | |
| Humour a | 4.57 (1.70) | |
| Scale | Prevalence (n) | Lower 95% CI | Higher 95% CI |
|---|---|---|---|
| HADS-Anxiety | |||
| Minimal/No (<8) | 78.0% (135) | 71.3% | 83.6% |
| Mild (8–10) | 16.8% (29) | 11.9% | 23.0% |
| Moderate (11–14) | 4.0% (7) | 2.0% | 8.1% |
| Severe (15–21) | 1.2% (2) | 0.3% | 4.1% |
| HADS-Depression | |||
| Minimal/No (<8) | 83.2% (144) | 77.0% | 88.1% |
| Mild (8–10) | 12.7% (22) | 8.6% | 18.5% |
| Moderate (11–14) | 4.0% (7) | 2.0% | 8.1% |
| Severe (15–21) | 0.0% (0) | ||
| HADS-Anxiety and Depression | |||
| Neither anxiety nor depression | 72.3% (125) | 65.2% | 78.4% |
| Either anxiety or depression | 16.8% (29) | 11.9% | 23.0% |
| Both anxiety and depression | 11.0% (19) | 7.1% | 16.5% |
| Variables | Bivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|
| Anxiety | Depression | ||||||
| HADS-A (Score > 8) n (%) | HADS-A (Score < 8) n (%) | p-Value | HADS-D (Score > 8) n (%) | HADS-D (Score < 8) n (%) | p-Value | ||
| Age (years) a | 34.3 (7.1) | 37.0 (8.2) | 0.047 * | 34.3 (6.2) | 36.9 (8.3) | 0.057 * | |
| Duration of service (months) a | 120.6 (86.1) | 155.1 (90.4) | 0.037 * | 119.1 (74.8) | 153.3 (92.3) | 0.063 * | |
| Duration of service in psychiatric department (months) a | 64.4 (69.0) | 114.6 (88.0) | <0.001 * | 60.8 (59.1) | 112.2 (88.8) | <0.001 * | |
| Ethnicity c | 0.337 | 0.188 * | |||||
| Malay | 30 (78.9) | 96 (71.1) | 24 (82.8) | 102 (70.8) | |||
| Non-Malay | 8 (21.1) | 39 (28.9) | 5 (17.2) | 42 (29.2) | |||
| Gender c | 0.020 * | 0.733 | |||||
| Female | 20 (52.6) | 98 (72.6) | 19 (65.5) | 99 (68.8) | |||
| Male | 18 (47.4) | 37 (27.4) | 10 (34.5) | 45 (31.3) | |||
| Education attainment c | 0.153 * | 0.519 | |||||
| Degree and higher | 23 (60.5) | 64 (47.4) | 13 (44.8) | 74 (51.4) | |||
| Diploma and lower | 15 (39.5) | 71 (52.6) | 16 (55.2) | 70 (48.6) | |||
| Medical comorbidity c | 0.193 * | 0.259 | |||||
| No | 35 (92.1) | 113 (83.7) | 27 (93.1) | 121 (84.0) | |||
| Yes | 3 (7.9) | 22 (16.3) | 2 (6.9) | 23 (16.0) | |||
| Psychiatric history d | 0.122 * | 0.425 | |||||
| No | 36 (94.7) | 134 (99.3) | 28 (96.6) | 142 (98.6) | |||
| Yes | 2 (5.3) | 1 (0.7) | 1 (3.4) | 2 (1.4) | |||
| Marital status c | 0.004 * | 1.000 | |||||
| Single (Ref) | 16 (42.1) | 28 (20.7) | 7 (24.1) | 37 (25.7) | |||
| Married | 19 (50.0) | 104 (77.0) | 21 (72.4) | 102 (70.8) | |||
| Divorce | 3 (7.9) | 3 (2.2) | 1 (3.4) | 5 (3.5) | |||
| Number of children c | 0.073 * | 0.707 | |||||
| At least one child | 19 (50.0) | 89 (65.9) | 19 (65.5) | 89 (61.8) | |||
| No children | 19 (50.0) | 46 (34.1) | 10 (34.5) | 55 (38.2) | |||
| Living arrangements c | 0.023 * | 0.023 * | |||||
| Alone | 6 (15.8) | 7 (5.2) | 5 (17.2) | 8 (5.6) | |||
| Family | 26 (68.4) | 117 (86.7) | 24 (82.8) | 119 (82.6) | |||
| Friend(s) | 6 (15.8) | 11 (8.1) | 0 (0) | 17 (11.8) | |||
| Living with elderly c | 0.600 | 0.649 | |||||
| No | 30 (78.9) | 101 (74.8) | 21 (72.4) | 110 (76.4) | |||
| Yes | 8 (21.1) | 34 (25.2) | 8 (27.6) | 34 (23.6) | |||
| Family member tested positive for COVID-19 c | 0.549 | 0.660 | |||||
| No | 29 (76.3) | 109 (80.7) | 24 (82.8) | 114 (79.2) | |||
| Yes | 9 (23.7) | 26 (19.3) | 5 (17.2) | 30 (20.8) | |||
| Household income c (n = 171) | 0.175 * | <0.022 * | |||||
| Less than RM 4850 | 12 (31.6) | 31 (23.3) | 8 (27.6) | 35 (24.6) | |||
| RM 4850–RM 10,959 | 23 (60.5) | 75 (56.4) | 21 (72.4) | 77 (54.2) | |||
| More than RM 10,959 | 3 (7.9) | 27 (20.3) | 0 (0.0) | 30 (21.1) | |||
| Financial hardship c | 0.209 * | 0.110 * | |||||
| No | 34 (89.5) | 109 (80.7) | 21 (72.4) | 122 (84.7) | |||
| Yes, getting worst | 4 (10.5) | 26 (19.3) | 8 (27.6) | 22 (15.3) | |||
| Adequate social support d | 0.303 | 0.591 | |||||
| No | 2 (5.3) | 3 (2.2) | 0 (0.0) | 5 (3.5) | |||
| Yes | 36 (94.7) | 132 (97.8) | 29 (100.0) | 139 (96.5) | |||
| Occupation c | 0.052 * | 0.919 | |||||
| Doctor | 22 (57.9) | 49 (36.3) | 13 (44.8) | 58 (40.3) | |||
| Nurse | 8 (21.1) | 54 (40.0) | 9 (31.0) | 53 (36.8) | |||
| Allied Health Professional | 5 (13.2) | 26 (19.3) | 5 (17.2) | 26 (18.1) | |||
| Administrative Staff | 3 (7.9) | 6 (4.4) | 2 (6.9) | 7 (4.9) | |||
| Work in shift rotation c | 0.306 | 0.460 | |||||
| No | 26 (68.4) | 80 (59.3) | 16 (55.2) | 90 (62.5) | |||
| Yes | 12 (31.6) | 55 (40.7) | 13 (44.8) | 54 (37.5) | |||
| Working hours per week c | 0.042 * | 0.038 * | |||||
| 45 h or less | 22 (57.9) | 101 (74.8) | 16 (55.2) | 107 (74.3) | |||
| 46 h or more | 16 (42.1) | 34 (25.2) | 13 (44.8) | 37 (25.7) | |||
| Providing direct care to COVID-19 patients c | 0.998 | 0.590 | |||||
| No | 29 (76.3) | 103 (76.3) | 21 (72.4) | 111 (77.1) | |||
| Yes | 9 (23.7) | 32 (23.7) | 8 (27.6) | 33 (22.9) | |||
| Adequate support at workplace d | 0.303 | 0.031 * | |||||
| No | 7 (18.4) | 9 (6.7) | 6 (20.7) | 10 (6.9) | |||
| Yes | 31 (81.6) | 126 (93.3) | 23 (79.3) | 134 (93.1) | |||
| Increased work burden due to COVID-19 pandemic c | 0.214 * | 0.224 * | |||||
| No | 11 (28.9) | 54 (40.0) | 8 (27.6) | 57 (39.6) | |||
| Yes | 27 (71.1) | 81 (60.0) | 21 (72.4) | 87 (60.4) | |||
| Investigated as close contact for COVID-19 c | 0.147 * | 0.116 * | |||||
| No | 22 (57.9) | 95 (70.4) | 16 (55.2) | 101 (70.1) | |||
| Yes | 16 (42.1) | 40 (29.6) | 13 (44.8) | 43 (29.9) | |||
| Tested for COVID-19 | 0.629 | 0.923 | |||||
| No | 22 (57.9) | 84 (62.2) | 18 (62.1) | 88 (61.1) | |||
| Yes | 16 (42.1) | 51 (37.8) | 11 (37.9) | 56 (38.9) | |||
| Tested positive with COVID-19 d | 0.210 * | 0.523 | |||||
| No | 36 (94.7) | 133 (98.5) | 28 (96.6) | 141 (97.9) | |||
| Yes | 2 (5.3) | 2 (1.5) | 1 (3.4) | 3 (2.1) | |||
| Perceived at risk group for COVID c | 0.569 | 0.917 | |||||
| No | 8 (21.1) | 23 (17.0) | 5 (17.2) | 26 (18.1) | |||
| Yes | 30 (78.9) | 112 (83.0) | 24 (82.8) | 118 (82.0) | |||
| Received COVID-19 vaccination d | 0.391 | 0.111 * | |||||
| No | 6 (15.8) | 14 (10.4) | 6 (20.7) | 14 (9.7) | |||
| Yes | 32 (84.2) | 121 (89.6) | 23 (79.3) | 130 (90.3) | |||
| Coping | Approach a | 34.1 (6.8) | 33.5 (9.6) | 0.661 | 33.3 (7.9) | 33.7 (9.3) | 0.818 |
| Avoidant a | 24.8 (5.2) | 20.5 (5.2) | <0.001 * | 25.0 (5.7) | 20.7 (5.1) | <0.001 * | |
| Religion b | 6 (3.0) | 7 (2.0) | 0.002 * | 6 (3.0) | 7 (3.0) | 0.812 | |
| Humour a | 4.5 (1.5) | 4.6 (1.7) | 0.767 | 4.4 (1.6) | 4.6 (1.7) | 0.583 | |
| Variables | Anxiety | Depression | ||
|---|---|---|---|---|
| Adjusted B (95% CI) | p-Value | Adjusted B (95% CI) | p-Value | |
| Marital status | - | - | ||
| Married | 0.014 * | |||
| Divorce | 0.306 (0.114, 0.826) | 0.019 * | ||
| Single (Ref) | 3.030 (0.448, 20.499) | 0.256 | ||
| (Coping) Religion | 0.704 (0.543, 0.913) | 0.008 | - | - |
| (Coping) Avoidant | 1.254 (1.145, 1.373) | <0.001 ** | 1.199 (1.093, 1.315) | <0.001 ** |
| Financial hardship | - | - | 3.666 (1.193, 11.268) | 0.023 * |
| Yes | ||||
| No (Ref) | ||||
| Received COVID-19 vaccination | - | - | 0.312 (0.095, 1.03) | 0.056 |
| Yes | ||||
| No (Ref) | ||||
| Duration of service in psychiatric department (months) | - | - | 0.988 (0.981, 0.996) | 0.003 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Narendra Kumar, M.K.; Francis, B.; Hashim, A.H.; Zainal, N.Z.; Abdul Rashid, R.; Ng, C.G.; Danaee, M.; Hussain, N.; Sulaiman, A.H. Prevalence of Anxiety and Depression among Psychiatric Healthcare Workers during the COVID-19 Pandemic: A Malaysian Perspective. Healthcare 2022, 10, 532. https://doi.org/10.3390/healthcare10030532
Narendra Kumar MK, Francis B, Hashim AH, Zainal NZ, Abdul Rashid R, Ng CG, Danaee M, Hussain N, Sulaiman AH. Prevalence of Anxiety and Depression among Psychiatric Healthcare Workers during the COVID-19 Pandemic: A Malaysian Perspective. Healthcare. 2022; 10(3):532. https://doi.org/10.3390/healthcare10030532
Chicago/Turabian StyleNarendra Kumar, Mehul Kumar, Benedict Francis, Aili Hanim Hashim, Nor Zuraida Zainal, Rusdi Abdul Rashid, Chong Guan Ng, Mahmoud Danaee, Nurulwafa Hussain, and Ahmad Hatim Sulaiman. 2022. "Prevalence of Anxiety and Depression among Psychiatric Healthcare Workers during the COVID-19 Pandemic: A Malaysian Perspective" Healthcare 10, no. 3: 532. https://doi.org/10.3390/healthcare10030532
APA StyleNarendra Kumar, M. K., Francis, B., Hashim, A. H., Zainal, N. Z., Abdul Rashid, R., Ng, C. G., Danaee, M., Hussain, N., & Sulaiman, A. H. (2022). Prevalence of Anxiety and Depression among Psychiatric Healthcare Workers during the COVID-19 Pandemic: A Malaysian Perspective. Healthcare, 10(3), 532. https://doi.org/10.3390/healthcare10030532








