Abstract
(1) Background and objective: Tooth movements described as unexplained, aberrant, unexpected, unwanted, or undesirable can occur in the presence of an intact orthodontic retention wire, without detachment or fracture. This iatrogenic phenomenon, known little or not by many practitioners, responsible for significant dental and periodontal complications, both functional and aesthetic, is called “Wire Syndrome” (WS). It is therefore considered an undesirable event of bonded orthodontic retainers, which must be differentiated from an orthodontic relapse. The objective was to perform, for the first time, a systematic review of the literature in order to define the prevalence of WS and to study its associated clinical characteristics. (2) Methods: A systematic review of the literature was performed following the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and recommendations using an electronic search strategy on four databases complemented by a manual search. All the prospective and retrospective clinical studies, including case reports and series, written in English or French, clearly mentioning the description, detection, or management of WS were included. Three independent blinding review authors were involved in study selection, data extraction, and bias assessment using the Mixed Methods Appraisal Tool (MMAT). (3) Results: Of 1891 results, 20 articles published between 2007 and 2021 fulfilled the inclusion criteria, with a globally high risk of bias since 16 articles were case report/series. The analysis of each article allowed the highlighting of WS through 13 categories, as follows: prevalence, apparition delay, patient characteristics, arch and tooth involved, families of movements, dental and periodontal consequences, type of wire, risk factors, etiologies, treatment, and preventive approach. (4) Conclusion: This systematic review of the literature elaborated a synthesis on WS, allowing general practitioners, periodontists, and orthodontists to understand this adverse event, to facilitate the diagnostic approach, and to underline preventive measures against WS. This review was registered in the International Prospective Register of Systematic Reviews (PROSPERO; number CRD42021269297).
1. Introduction
The long-term follow-up of orthodontic bonded retainers remains a challenge for orthodontists, but also for periodontists, as well as general practitioners. Whereas fixed retainer placement is a common procedure after orthodontic treatment, complications, which can be severe, can happen. Indeed, in 2007, Katsaros et al. [1] were the first to describe this problem, which occurs when the orthodontic retainer is always bonded to the anterior teeth, inducing serious complications on these teeth under the name “unexpected complications of bonded mandibular lingual retainers”. This phenomenon was thereafter described by some authors under different names, such as “severe complication of a bonded mandibular lingual retainer” [2] in 2012, “Syndrome du Fil” [3] in 2015, “inadvertent tooth movement with fixed lingual retainers” [4] in 2016, or “extreme complication of a fixed lingual mandibular lingual retainer” [5] in 2021.
The synthesis of clinical experience evoked by the authors cited above allows us to define and characterize Wire Syndrome (WS) as follows: Fixed orthodontic retainers can provoke aberrant, unexpected, unwanted, or unexplained tooth movement on teeth still bonded by a fixed retainer placed after orthodontic treatment, which could induce progressively iatrogenic dental and periodontal complications, functional and/or aesthetic, ranging from minor teeth displacement to teeth expulsion from the bone with loss of vitality. In the presence of severe WS, the retainer may become detached or fractured. WS is not a classic orthodontic relapse, and the position of the teeth does not correspond to any previous situation.
However, neither general practitioners nor dental specialists, such as orthodontists and periodontists, are aware of the Wire Syndrome phenomenon. Concerning general practitioners, a lack of knowledge has been detected. A survey in eastern France showed that only 18.6% of general dentists were aware of the risks of adverse tooth movement associated with unintentionally active fixed retainers [6]; these results are globally in agreement with a Swiss survey by Habegger et al. [7]. However, general practitioners are seeing an increasing number of patients with a bonded retainer, estimated at 2–10 patients per week [7]. Concerning orthodontists, in a survey conducted by Padmos et al. [8] in New Zealand, one in eight was not familiar with this problem, and one in five had never seen any such cases. Padmos et al. [8] therefore concluded that it is necessary for all dental professionals worldwide to become more knowledgeable about this phenomenon, to be able to recognize associated cases, and also to prevent the worsening of complications.
Therefore, the aim of this study was to perform the first systematic review of the literature on Wire Syndrome (WS) in order to define the prevalence, to study its associated clinical characteristics, and, specifically, to facilitate the diagnostic approach of practitioners and to underline preventive and curative measures against WS.
2. Methods
2.1. Protocol Registration
A systematic review of the literature (SRL) was performed, following as closely as possible the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and recommendations (reference). The protocol was registered in the International Prospective Register of Systematic Review (PROSPERO) (CRD42021269297).
2.2. Article Identification
2.2.1. PICOs Question and Eligibility Criteria
According to the question formulated using the “Population, Intervention, Comparison, Outcome and Study Designs (PICOs) model”:
- –
- Participants (P): Patients with “Wire Syndrome” (WS), i.e., dental movements described as aberrant, unexpected, unexplained, unwanted, or excessive;
- –
- Interventions (I): Fixed orthodontic retainer bonded at the maxilla and/or mandible after orthodontic treatment;
- –
- Comparisons (C): Patients not affected by “Wire Syndrome” (only for studies including a control group);
- –
- Outcomes (O): Define the prevalence of “Wire Syndrome” and the characteristics associated with it.
- –
- Study designs (S): All prospective and retrospective clinical studies, including case reports or series, written in English or French, clearly reporting the description, detection, or management of “Wire Syndrome” or tooth movement described as aberrant, unexpected, unwanted, or unexplained in the presence of a bonded fixed retainer placed after orthodontic treatment were included, regardless of the length of the follow-up. In vitro studies, narrative reviews, author opinions, editorials, or commentaries were excluded.
2.2.2. Search Strategy
- ❖
- Electronic search
A search strategy, tailored to each database, combining keywords, Medical Subject Headings (MeSH) terms, and Boolean operators was performed without date restriction.
The electronic search was conducted on four different databases on 1 September 2021 (Table 1).

Table 1.
Search strategy, according to each database.
- ❖
- Manual search
To complement the electronic searches, a manual search was conducted:
- –
- From the bibliography of articles selected by the electronic search;
- –
- From the search engine of a selection of orthodontic and dental journals:
- ○
- American Journal of Orthodontics and Dentofacial Orthopedics;
- ○
- European Journal of Orthodontics;
- ○
- Journal of Orthodontics;
- ○
- Journal of Clinical Orthodontics;
- ○
- Orthodontic & Craniofacial Research;
- ○
- The Angle Orthodontist;
- ○
- Revue d’Orthopédie Dento-Faciale;
- ○
- L’information Dentaire.
2.3. Article Selection
2.3.1. Electronic Search
This research was conducted using the reference management software Zotero version 5.0.96.2 (https://www.zotero.org accessed on 1 September 2021). Two authors carried out the entire procedure independently. In the case of disagreement, a third author was interviewed, and a mutual discussion was conducted to reach a consensus.
After avoiding duplicates, the inclusion of articles was carried out in three steps:
- –
- Reading of titles;
- –
- Reading of abstracts;
- –
- Reading of the full text.
For articles with no available abstracts, full-text articles were read for eligibility assessment.
2.3.2. Manual Search
The same selection procedure applied to the electronic research was carried out.
2.4. Data Extraction
For the articles selected in this SRL, tables were made to synthesize the important data of the articles by the same two operators independently, as follows: author names, year of publication and journal, aim, study design, population, and results summary.
Because the included studies had heterogeneous methods, methodological analyses, and results, it was not possible to perform a meta-analysis. Therefore, the analysis of the articles was qualitative and descriptive.
2.5. Risk of Bias Analysis
Given the heterogeneity of the studies selected for this SRL, a tool that can evaluate the methodological quality of different types of studies within the same SRL was employed: The “Mixed Methods Appraisal Tool” (MMAT) [9] (http://mixedmethodsappraisaltoolpublic.pbworks.com accessed on 1 September 2021).
3. Results
3.1. Article Selection
3.1.1. Electronic Search
The electronic search conducted on 1 September 2021 identified 1891 references. After eliminating duplicates, 1270 references were analyzed. Based on the reading of the title, 211 titles were retained. Then, a reading of the abstract was conducted, retaining 50 articles for a full reading of the text. After a complete reading of these 50 articles, 15 articles were finally retained.
3.1.2. Manual Search
The manual search identified 13 additional articles. After applying the selection procedure on these 13 articles, five articles were retained in the present study.
In total, the applied search strategy resulted in the selection of 20 articles in this SRL (Figure 1).
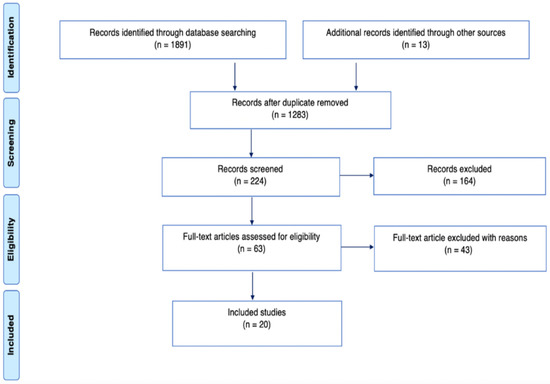
Figure 1.
Systematic search and selection strategy. PRISMA flow diagram.
3.2. Studies’ Characteristics
Out of the 20 articles selected in our SRL, the study designs were heterogeneous, with one randomized controlled study [10] and a large majority of case series and case reports.
Additionally, the included studies were conducted worldwide, and the year of publication varied from 2007 to 2021.
Several different names were attributed to “Wire Syndrome” (Table 2). More specifically, the first article describing “unexpected movements” was by Katsaros et al. [1] in 2007. The French term “Syndrome du Fil” was introduced thereafter by Roussarie et al. [3] in 2015.
The terms “X effect” and “Twist effect” were first used by Kucera et al. [11] in 2016.
Finally, no conflict of interest in any studies were declared.

Table 2.
History of the different definitions/descriptions of Wire Syndrome (WS).
Table 2.
History of the different definitions/descriptions of Wire Syndrome (WS).
| Authors | Publication Date | Wire Syndrome Definition |
|---|---|---|
| Katsaros et al. [1] | 2007 | Unexpected complications of bonded mandibular lingual retainers |
| Abudiak et al. [12] | 2011 | A complication with orthodontic fixed retainers |
| Renkema et al. [13] | 2011 | Unexpected posttreatment complications |
| Alessandri Bonetti et al. [14] | 2012 | Isolated-type recession defects with an abnormal buccolingual inclination |
| Pazera et al. [2] | 2012 | Severe complication of a bonded mandibular lingual retainer |
| Farret et al. [15] | 2015 | Extreme labial movement of the root |
| Roussarie et al. [3] | 2015 | Syndrome du fil |
| Kučera et al. [11,16] | 2016 | Unexpected complications/X effect, Twist effect, and non-specific complications |
| Laursen et al. [17] | 2016 | Complications after unintentional tooth displacement by active bonded retainers |
| Shaughnessy et al. [4] | 2016 | Inadvertent tooth movement with fixed lingual retainers |
| Wolf et al. [18] | 2016 | Undesired tooth movement |
| Egli et al. [10] | 2017 | Unexpected posttreatment changes |
| Jacobs et al. [19] | 2017 | Single tooth torque problems |
| Beitlitum et al. [20] | 2020 | Unwanted effects such as inadvertent tooth movement and torque changes |
| Kim et al. [21] | 2020 | Unexpected tooth movements |
| Klaus et al. [22] | 2020 | Unwanted tooth movements |
| Knaup et al. [23] | 2021 | Side effects of twistflex retainers |
| Singh et al. [5] | 2021 | Extreme complication of a fixed mandibular lingual retainer |
3.3. Bias Results
The MMAT score was relatively high for each included study, with a mean of 73 ± 18.2%.
3.4. Studies’ Results
A description of each included study is provided in Table 3.

Table 3.
Summary description of each included study. AJODO: American Journal of Orthodontics and Dentofacial Orthopedics. * If the article had several aims, only the one related to Wire Syndrome is mentioned.
Analysis of the results allowed the synthesis of said results around 13 categories. Note that not all articles presented information in all categories.
Prevalence: The prevalence varied from 1.1% to 43.0%. The lowest prevalence estimate of 1.1% was found in a retrospective study by Kučera et al. [11], which had the largest sample size, with 3500 patients included. The highest prevalence was found in the study of Wolf et al. [18], which included only 30 patients, with a prevalence of 13% and 30% in severe and moderate WS, respectively.
Apparition delay: Kucera et al. [11] showed that WS appeared in a mean interval of 4 ± 2.8 years. The apparition delay found in the included case reports and series was mostly (80%) within this range, except for five publications that were above this range [3,4,15,17]. The shortest apparition delay reported was one year in the study of Katsaros et al. [1], and the longest time reported was 21 years after placement of a bonded retainer in the case report of Farret et al. [15].
Patient characteristics: Gender: The overall publications included 40 men and 81 women. Age: The youngest WS patient identified in this SRL was 13.5 years old [1], and the oldest was 56 years old [20]. The study by Kucera et al. [11] calculated the average age of its 38 WS patients and found it to be 20.7 ± 8.9 years. The ages of the patients included in the case reports and series mostly corresponded to this range, except for three [15,17,20], who were above this range. Parafunction: Only Alessandri Bonetti et al. [14] mentioned parafunctions, where, for two patients with WS, onychophagia was demonstrated by questioning and exobuccal examination (nail deformation).
Arch and tooth involved: WS was found in 72 cases in the maxilla versus 179 cases described in the mandible. Additionally, WS involved 39 maxillary incisors, 6 maxillary canines, 64 mandibular incisors, and 100 mandibular canines.
Families of movements: Although WS shows significant interindividual variation, the movements can be categorized into four groups (Table 4).

Table 4.
Wire Syndrome (WS) movement families. N.B.: The terms “X effect©” and “twist effect©” were introduced by Kucera et al. [11,16].
Dental consequences: WS is responsible for displacement of the affected teeth in all spatial dimensions with a large range of variations. These displacements can be slight, according to the study by Klaus et al. [22], which mentioned a median magnitude of unwanted movement from 0 to 0.66 mm. However, extreme movement of the tooth can cause rupture of the vascular–nervous bundle and loss of vitality of the tooth [14,15] associated with the exposure of the root until the apex [5].
Periodontal consequences: Tooth WS displacements can contribute to vestibular or lingual gingival recessions, dehiscences, or fenestrations apparition, responsible for aesthetic repercussions and/or exposure of the root, leading to discomfort or pain, particularly due to hypersensitivity [20]. In severe cases, displacement of the root out of its socket may result in resorption of the entire vestibular or lingual wall, depending on the direction of tooth movement [15]. The root (and its apex) may be projected out of the bone [2].
Type of retention wire: Several different types of wires are involved in the occurrence and development of WS, as follows:
- ❖
- Flat, braided chains (Ortho FlexTech).
- ❖
- Single-stranded, round wire bonded on the canines only; diameter: 0.036 inch.
- ❖
- Round, twisted, stainless steel wire:
- Unknows strands with diameter: 0.0175 inch; 0.0215 inch; 0.0195 inch;
- Three strands with a diameter of 0.0155, 0.0195, or 0.0195 inches (heat treatment);
- Five strands with a diameter of 0.0215 inched (gold-plated);
- Six strands with a diameter of 0.0175 inches.
- ❖
- Round, coaxial, stainless steel wire:
- Six strands with a diameter of 0.018 inches.
Most cases of WS are seen in the presence of round, twisted, stainless steel wires [1,2,3,4,5,10,11,12,13,14,16,17,18,21,23], although flat, braided chains are also concerned [3], as well as single-stranded, round wires bonded only on the canines [5] and round, coaxial, stainless steel wires [22].
Risk Factors: Predisposing factors of WS were investigated in three studies [11,18,22]:
- ❖
- Patient-related factors: Different parameters were found to be significant in WS patients, such as lower facial level increase (p < 0.0001) [11], vestibulo-position of mandibular incisors before orthodontic treatment (p = 0.029) [11], and presence of dysfunctions/parafunctions (p = 0.049) [22]. However, Klaus et al. [22] did not find any significant difference in WS patients regarding mandibular plane angle or initial vestibulo-version of the incisors.
- ❖
- Orthodontic treatment-related factors: Different parameters were found to be significant in WS patients, such as debonded at a young age (p = 0.03) [11], canine expansion and overjet reduction during treatment [18], and absence of inter-incisal contact at the end of treatment (p < 0.01) [22]. In contrast, Klaus et al. [22] found no significant difference in WS patients regarding expansion of the inter-canine distance and reduction in overjet. Kucera et al. [11] showed no significant difference regarding treatment duration (p = 0.270), inter-canine distance (p = 0.065), or change in incisor inclination (p = 0.151).
- ❖
- Wire-related factors: No significant differences were found in patients with WS regarding debonded wire (p ≤ 0.05) [22], (p = 0.562) [11] and type of wire (p = 1.000) [11].
Etiologies: Different etiological hypotheses were mentioned in the included studies, which can be grouped into three categories, as follows (Table 5): practitioner-, wire-, and patient-related etiologies.

Table 5.
Etiological hypotheses of Wire Syndrome (WS).
Treatment: Treatment depends on the severity of WS. It should be noted that in the three cases where treatment was not performed [14,21], clinical aggravation occurred.
- ❖
- Mild severity: The most common treatment was retainer removal. Some authors [10,23] observed significant improvement up to spontaneous repositioning. Stripping was recommended by Roussarie et al. [3] to facilitate teeth repositioning and avoid relapse. The correction of parafunctions was also recommended [14]. For two research teams [3,5], an observation period of six months to one year was performed after wire removal.
- ❖
- Moderate severity: The wire is also removed, but orthodontic retreatment is required to correct malposition and to properly reposition the root in the alveolar bone, in order to improve surgical conditions [2,3,12,14,15,19,20].
- ❖
- Significant severity: Orthodontic retreatment combined with endodontic and/or periodontal treatment is indicated. Endodontic treatment is performed when the displacement of the tooth is so important that it has caused a rupture of the vascular–nervous bundle. Endodontic surgery may be associated if necessary [14,15]. In cases where periodontal surgery is indicated, the removal of retainers is beneficial [20]. In cases of extreme WS, dental avulsion is sometimes the only solution [5].
Recommendations: The authors of the included studies described some recommendations to avoid the development of WS (Table 6).

Table 6.
Recommendations to avoid Wire Syndrome (WS).
4. Discussion
To the best of our knowledge, the present publication is the first systematic review of the literature on the subject of Wire Syndrome (WS). After identifying 1891 articles, 20 articles were selected and analyzed, with a globally high risk of bias. Given the limited number of existing publications on WS and the relevant information found in the case reports and case series, these types of study designs were included.
The description of WS is recent; the first publication on WS appeared in 2007 [1], followed by an increase in publications, and the distinction between classic relapse and WS is also a very new concept. Since the introduction of fixed bonded retainers in the 1970s by Zachrisson, fixed retainers have been progressively preferred to removable thermoplastic application by patients and practitioners [22,25], and, parallelly, there has been an increasing number of orthodontic treatments. The prevalence of WS is therefore likely to rise and also to attract more research interest. Concerning specifically the prevalence of WS, six studies estimated the prevalence of adverse movements associated with bonded retainers, in which the prevalence varied from 1% (3500 patients studied [11]) to 43% (30 patients studied [18]). This wide range can be explained by the differences in sample size between these two monocentric studies. Moreover, the protocols (patient selection, practitioners, type of wire, bonded protocol, etc.) were very different between the studies.
Regarding the delay in apparition, WS appeared between 1 and 21 years after the placement of a retainer in the included studies. The majority of cases of WS appeared within the first five years after the placement of the retainer. This time interval should be considered with caution for several reasons. First of all, it is difficult to date the apparition of WS with precision, as retainer visits are intermittent. Moreover, it is difficult to detect early WS, and the patient often consults when complications are already severe [20]. Concerning the characteristics of the patients, all ages, particularly young people under 30 years of age, are affected by WS. Twice as many women as men seem to be affected. Orthodontic treatment is usually performed in adolescence, and WS occurs also a few years after the end of orthodontic treatment. In addition, one study showed the presence of onychophagia in both patients with WS [14]. This parafunction could therefore increase the risk of developing WS in our patients. Additionally, concerning the arch and tooth concerned, WS was first described in the mandible in 2007 by Katsaros et al. [1], although the first case described in the maxillary arch was in 2011 [12]. Moreover, although in the study by Klaus et al. [22] maxillary teeth are more affected by WS than mandibular teeth (20.9% versus 14%), most WS cases occur in the mandible. Indeed, more fixed retainers are placed in the mandible than in the maxilla, where thermoplastic retainers are preferred [8,26]. Placement of a maxillary bonded retainer requires composite plots that can create interference/occlusal trauma with the mandibular arch, resulting in more failures [27]. In addition, when a maxillary bonded retainer is indicated, wires are most often placed from lateral incisor to the lateral incisor than from canine to canine to avoid the previously mentioned difficulties [28], so WS on maxillary canines is rare. However, it should also be noted that WS in the maxilla is more quickly detected than WS in the mandible because it affects the patient’s smile, which leads to early consultation [3]. Finally, the teeth most often affected by WS are the mandibular canines. It would seem that WS preferentially affects the “terminal” teeth that are always contained by the fixed bonded retainer.
In the presence of WS, the bonded retainer is intact in most cases but, in severe cases, the wire may become partially debonded or fractured due to important dental movement. In any situation, various and different clinical dental and periodontal signs can be found. The detection of one sign related to WS must immediately alert the practitioner to the possible presence of WS in order to stop the iatrogenic evolutive process and to start adapted therapy. Indeed, this syndrome is progressive and starts with minor dental and periodontal consequences until the loss of vitality and/or tooth expulsion. In addition, when treatment is not carried out [14,21], clinical worsening can occur [2,24]. Movements due to WS do not correspond to a relapse or a physiological process: The situation of the teeth does not correspond to their position before orthodontic treatment, nor to their position at the time of debonding, as underlined by Kastaros et al. [1]. WS can therefore be qualified as a new malposition observed after placement of a fixed bonded retainer following orthodontic treatment [18,22], although no value or threshold has been scientifically determined [22]. Thus, a severe WS is easily identified because the clinical signs are more marked, contrary to an early WS, whose clinical signs are mild; the identification of complex cases is easy, while early detection remains difficult. In the case of mild movements, differentiation of movements related to a classic relapse from WS also remains arduous. Therefore, the challenge for orthodontists during follow-up visits is to detect incipient WS. Additionally, general practitioners, as well as periodontists, also have an important role to play in the early detection of WS. Finally, the patient must also be actively involved in monitoring [1,13]. Patients should be alerted to the need for maintenance and the plausible occurrence of adverse effects related to the presence of the retainer wire.
With regard to WS prevention, the most important preventive measure is the use of a bonded passive retainer. The use of a dental model to perfectly fit the retainer to the teeth before placement is recommended, as well as an indirect bonding protocol. Furthermore, special care should also be taken when the fixed retainer needs to be repaired. When a composite comes loose, small tooth movements may have already occurred and the wire is no longer a perfect fit. In this case, using an instrument to “push” the wire to better fit the teeth results in an active wire that could potentially be responsible for subsequent WS. Therefore, a new passive wire should be bonded rather than repaired. Another strategy for preventing WS is double retention, which combines a fixed bonded retainer with a removable thermoplastic retainer [4,5,8,18]. Finally, the number of WS cases increases during the first five years according to Kucera et al. [11], suggesting that monitoring in the orthodontic office should be preferred, at least during this interval. Treatment depends on the severity of the case, from non-invasive treatment, through a multidisciplinary endodontic/periodontal approach, to extraction of the involved tooth in extreme cases. In the case of early WS, the most important reflex is to remove the fixed retainer to immediately stop the iatrogenic WS process; spontaneous correction of tooth malposition may occur [10,23].
Although there are explanatory hypotheses that could justify the risk factors mentioned by the authors, not all studies agreed. Indeed, WS seems to be due to a combination of different and multifactorial etiologies. In addition, it appears that the delay in apparition varies with etiology [29]. Early WS could probably be explained by an error in wire adaptation (lack of passivity) or bonding [29]. When WS appears several years after orthodontic placement, wire-related etiologies are preferred. Regarding dysfunction, some authors hypothesized that oro-vestibular forces exerted by the tongue could cause undesirable movement [2,22,29], although Shaugnessy et al. excluded the role of the tongue because its pressure would be less than that required to deform the wire [4]. In addition, the risk of wire deformation also increases with time due to the progressive wear of the composite, which results in a larger section of the wire being exposed to deformation [29]. Additionally, a change or instability in the mechanical properties of the wires, whether inborn or acquired, could be involved in WS. A fixed retainer could become unintentionally active. Moreover, a break in adhesion at the wire–composite interface can cause a “pivot effect”, resulting in torsion of the teeth around the wire, which then acts as a center of rotation [8,15,29]. The tooth pivots around the wire, which could explain the unwanted torque of the teeth involved in WS. After observing the rotational movements of the six anterior teeth, Wolf et al. [18] hypothesized that the fixed wire causes forces that rotate the entire block of interconnected anterior teeth stiffened by the wire in the vestibular direction on one side and lingual on the other due to physiological transverse constriction.
The type of wire seems to have an influence on the occurrence of WS. In the study of Padmos et al. [25], the mechanical properties of round multistrand wires were incriminated. Indeed, most of the included studies in this systematic review described WS as being associated with round, multistrand twisted wires [1,2,3,4,5,10,11,12,13,14,16,17,18,21,23]. Engeler et al. [30] assured that all documented adverse movements are present only with multistrand wires, whereas Roussarie et al. [24] showed that no wire is immune to WS. While some authors expressed a preference for the type of wire to be used to avoid the development of WS, no consensus on wire selection could be advanced. In addition, the diversity of materials and bonding protocols make it difficult to draw any conclusions. Recently, Gelin et al. [31] investigated the effect of rectangular, 0.014 × 0.014 inch, memory shape-customized CAD/CAM nitinol retainers (Memotain TM; CA Digital GmbH, Mettmann, Germany) versus round, 0.0175 inch (in), six-stranded, twisted, stainless steel wire retainers (Supra-FlexTM; RMO Europe, Illkirch-Graffenstaden, France) and showed no significant difference between these two types of retainer after one year of placement. To reach a consensus on the preferred type of wire to use, randomized controlled studies must be conducted on a large sample size and over long observation periods.
Finally, some additional points should be made regarding this systematic review of the literature. First, only one study designed as a randomized controlled trial was included for analysis, and the risk of bias was considered high, as the majority of included studies were designed as case series/reports. Second, there was a lack of information in the included studies. For example, few data were provided on patient characteristics prior to orthodontic treatment (e.g., baseline crowding and cephalometric measurement), orthodontic biomechanics employed to treat the patient (e.g., elastics employed and brackets prescribed), bonding and retainer placement protocol, history of retainer failures (e.g., number of breakages, detachment, or re-bonding), etc. Furthermore, the periodontal conditions, such as type of phenotype [32], traction of labial frenum, or oral hygiene quality, were not investigated in each study. However, these parameters may have an influence on the development of WS, probably from a multifactorial origin. Moreover, the selected studies have extreme heterogeneity in terms of the variables compared and the outcomes measured. Concomitantly, the enormous heterogeneity of the included studies made it impossible to perform a meta-analysis. All of this represents a limitation that is important to consider.
5. Conclusions
This first review of the literature on Wire Syndrome (WS) included 20 articles published between 2007 and 2021, with a majority of case report/series leading to a globally high risk of bias. However, the analysis of the overall article provided an understanding of this adverse event associated with fixed orthodontic retainers, emphasized the importance of an early diagnosis, and highlighted preventive measures against WS for dental professionals worldwide, including general practitioners (GP), periodontists, and orthodontists. Indeed, the WS problem must involve all the dental health professions, including the general practitioners who will be able to refer, if necessary, the patient to a specialist practitioner; the continuity of the collaboration and the “ortho–paro–gp” link will then be prolonged during the therapeutic time, thus guaranteeing optimal patient care. Further studies are needed to improve the knowledge about fixed orthodontic retainers, based on a large, well-documented sample and conducted over a very long observation period.
Author Contributions
Conceptualization, C.C., F.V. and S.-M.D.; methodology, C.C., F.V. and S.-M.D.; software, C.C. and F.V.; validation, C.C., F.V., S.A. and S.-M.D.; formal analysis, C.C., F.V., S.A. and S.-M.D.; investigation, C.C., F.V., S.A. and S.-M.D.; resources, C.C., F.V., S.A. and S.-M.D.; data curation, C.C., F.V., S.A. and S.-M.D.; writing—original draft preparation, C.C.; writing—review and editing, C.C., F.V., S.A. and S.-M.D.; visualization, C.C., F.V., S.A. and S.-M.D.; supervision, C.C., S.A. and S.-M.D.; project administration, C.C. and S.-M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data underlying this article are available in the article.
Acknowledgments
The authors warmly thank Léa Graveline for proofreading the English version.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Katsaros, C.; Livas, C.; Renkema, A.M. Unexpected complications of bonded mandibular lingual retainers. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 838–841. [Google Scholar] [CrossRef] [PubMed]
- Pazera, P.; Fudalej, P.; Katsaros, C. Severe complication of a bonded mandibular lingual retainer. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 406–409. [Google Scholar] [CrossRef] [PubMed]
- Roussarie, F.; Douady, G. Effet indésirable des fils de contention collés: Le « syndrome du fil »: 1ère partie. Unwanted tooth movement produced by the bonded retention wires: The “wire syndrom”: First part. Rev. Orthop. Dento Faciale 2015, 49, 411–426. [Google Scholar] [CrossRef]
- Shaughnessy, T.G.; Proffit, W.R.; Samara, S.A. Inadvertent tooth movement with fixed lingual retainers. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 277–286. [Google Scholar] [CrossRef] [Green Version]
- Singh, P. Canine avulsion: An extreme complication of a fixed mandibular lingual retainer. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Rafflenbeul, F.; Hanriat, C.; Lefebvre, F.; Renkema, A.M.; Bolender, Y. How do general dental practitioners perceive and deal with orthodontic bonded retainers? Am. J. Orthod. Dentofac. Orthop. 2021, 160, e1–e8. [Google Scholar] [CrossRef]
- Habegger, M.; Renkema, A.M.; Bronkhorst, E.; Fudalej, P.S.; Katsaros, C. A survey of general dentists regarding orthodontic retention procedures. Eur. J. Orthod. 2017, 39, 69–75. [Google Scholar] [CrossRef] [Green Version]
- Padmos, J.; Mei, L.; Wouters, C.; Renkema, A.M. Orthodontic retention procedures in New Zealand: A survey to benefit clinical practice guideline development. J. World Fed. Orthod. 2019, 8, 24–30. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; et al. Improving the content validity of the mixed methods appraisal tool: A modified e-Delphi study. J. Clin. Epidemiol. 2019, 111, 49–59.e41. [Google Scholar] [CrossRef] [Green Version]
- Egli, F.; Bovali, E.; Kiliaridis, S.; Cornelis, M.A. Indirect vs direct bonding of mandibular fixed retainers in orthodontic patients: Comparison of retainer failures and posttreatment stability. A 2-year follow-up of a single-center randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 15–27. [Google Scholar] [CrossRef]
- Kučera, J.; Marek, I. Unexpected complications associated with mandibular fixed retainers: A retrospective study. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Abudiak, H.; Shelton, A.; Spencer, R.J.; Burns, L.; Littlewood, S.J. A complication with orthodontic fixed retainers: A case report. Orthod. Update 2011, 4, 112–117. [Google Scholar] [CrossRef]
- Renkema, A.M.; Renkema, A.; Bronkhorst, E.; Katsaros, C. Long-term effectiveness of canine-to-canine bonded flexible spiral wire lingual retainers. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 614–621. [Google Scholar] [CrossRef]
- Alessandri Bonetti, G.; Incerti Parenti, S.; Zucchelli, G. Onychophagia and postorthodontic isolated gingival recession: Diagnosis and treatment. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 872–878. [Google Scholar] [CrossRef] [PubMed]
- Farret, M.M.; Farret, M.M.; da Luz Vieira, G.; Assaf, J.H.; de Lima, E.M. Orthodontic treatment of a mandibular incisor fenestration resulting from a broken retainer. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 332–337. [Google Scholar] [CrossRef] [Green Version]
- Kucera, J.; Streblov, J.; Marek, I.; Hanzelka, T. Treatment of Complications Associated with Lower Fixed Retainers. J. Clin. Orthod. 2016, 50, 54–59. [Google Scholar]
- Laursen, M.G.; Rylev, M.; Melsen, B. Treatment of Complications after Unintentional Tooth Displacement by Active Bonded Retainers. J. Clin. Orthod. 2016, 50, 290–297. [Google Scholar]
- Wolf, M.; Schulte, U.; Küpper, K.; Bourauel, C.; Keilig, L.; Papageorgiou, S.N.; Dirk, C.; Kirschneck, C.; Daratsianos, N.; Jäger, A. Post-treatment changes in permanent retention. J. Orofac. Orthop. 2016, 77, 446–453. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, C.; Katzorke, M.; Wiechmann, D.; Wehrbein, H.; Schwestka-Polly, R. Single tooth torque correction in the lower frontal area by a completely customized lingual appliance. Head Face Med. 2017, 13, 18. [Google Scholar] [CrossRef] [Green Version]
- Beitlitum, I.; Barzilay, V.; Rayyan, F.; Sebaoun, A.; Sarig, R. Post-Orthodontic Lower Incisors Recessions: Combined Periodontic and Orthodontic Approach. Int. J. Environ. Res. Public Health 2020, 17, 8060. [Google Scholar] [CrossRef]
- Kim, T.; Baek, S. Lingual bonded retainers: A case series of complications and resolutions. APOS Trends Orthod. 2020, 10, 3–11. [Google Scholar]
- Klaus, K.; Xirouchaki, F.; Ruf, S. 3D-analysis of unwanted tooth movements despite bonded orthodontic retainers: A pilot study. BMC Oral Health 2020, 20, 308. [Google Scholar] [CrossRef] [PubMed]
- Knaup, I.; Bartz, J.R.; Schulze-Späte, U.; Craveiro, R.B.; Kirschneck, C.; Wolf, M. Side effects of twistflex retainers-3D evaluation of tooth movement after retainer debonding. J. Orofac. Orthop. 2021, 82, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Roussarie, F.; Douady, G. Effet indésirable des fils de contention collés: Le « syndrome du fil »: Observations, théories, conséquences cliniques: 2e partie. Unwanted tooth movement produced by the bonded retention wire: The « wire syndrome », observations, theories, clinical consequences: Second part. Rev. Orthop. Dento Faciale 2018, 52, 327–341. [Google Scholar]
- Padmos, J.A.D.; Fudalej, P.S.; Renkema, A.M. Epidemiologic study of orthodontic retention procedures. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 496–504. [Google Scholar] [CrossRef]
- Andriekute, A.; Vasiliauskas, A.; Sidlauskas, A. A survey of protocols and trends in orthodontic retention. Prog. Orthod. 2017, 18, 31. [Google Scholar] [CrossRef] [Green Version]
- Schneider, E.; Ruf, S. Upper bonded retainers. Angle Orthod. 2011, 81, 1050–1056. [Google Scholar] [CrossRef]
- Zachrisson, B.U. Multistranded wire bonded retainers: From start to success. Am. J. Orthod Dentofac. Orthop. 2015, 148, 724–727. [Google Scholar] [CrossRef] [Green Version]
- Kučera, J.; Littlewood, S.J.; Marek, I. Fixed retention: Pitfalls and complications. Br. Dent. J. 2021, 230, 703–708. [Google Scholar] [CrossRef]
- Engeler, O.G.; Dalstra, M.; Arnold, D.T.; Steineck, M.; Verna, C. In vitro comparison of the torsional load transfer of various commercially available stainless-steel wires used for fixed retainers in orthodontics. J. Orthod. 2021, 48, 118–126. [Google Scholar] [CrossRef]
- Gelin, E.; Seidel, L.; Bruwier, A.; Albert, A.; Charavet, C. Innovative customized CAD/CAM nickel-titanium lingual retainer versus standard stainless-steel lingual retainer: A randomized controlled trial. Korean J. Orthod. 2020, 50, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, P.; Bissada, N.F. Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J. Periodontol. 2018, 89 (Suppl. 1), S204–S213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).