How Did the Pandemic Affect Communication in Clinical Settings? A Qualitative Study with Critical and Emergency Care Nurses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Study Setting and Participants
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
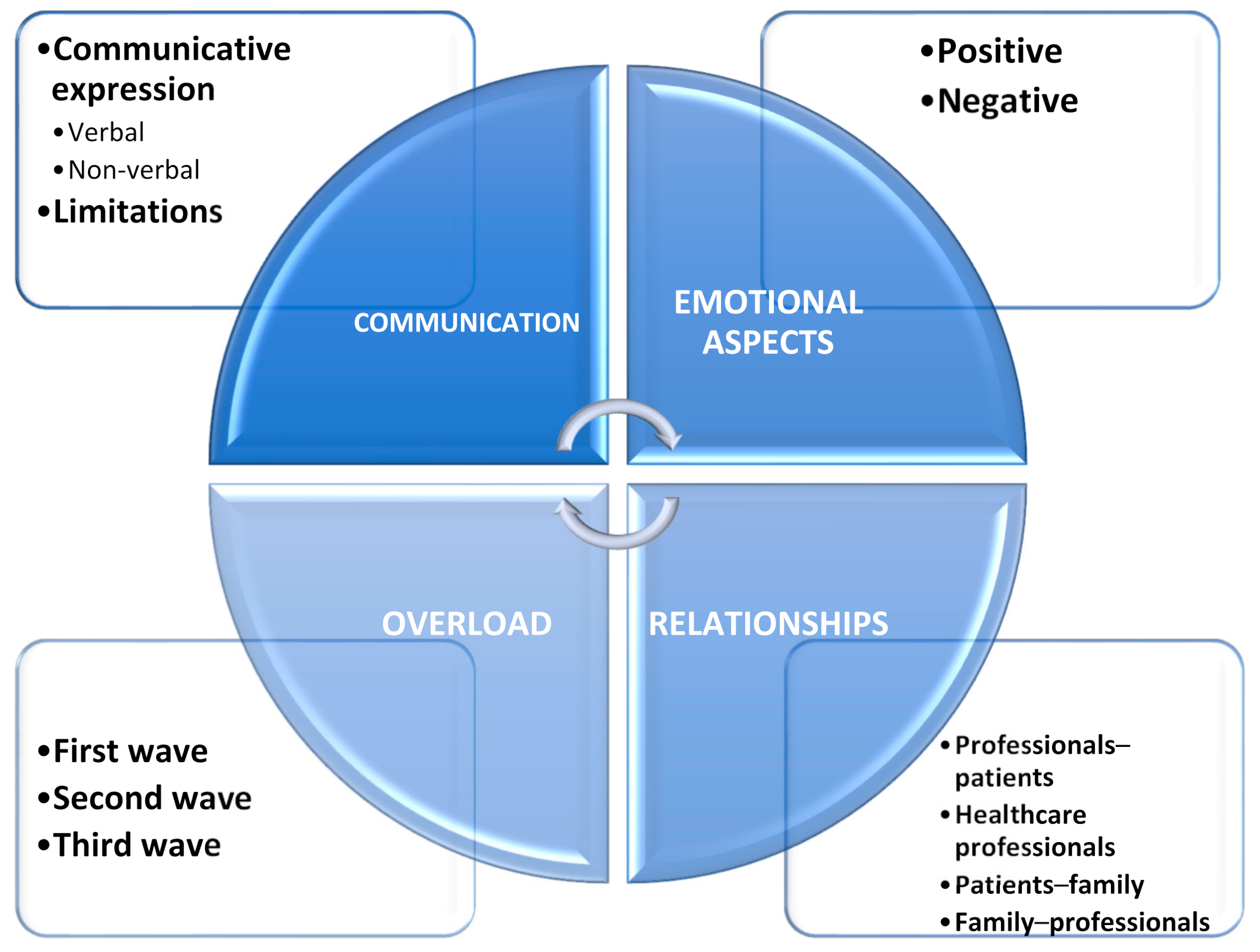
3. Results
3.1. Dimension 1. Communication
3.1.1. Communicative Expression: Verbal
“(...) communication was easier between colleagues if you had previously met them before wearing the PPE. It is clear to me that verbal communication has suffered; especially at the beginning, it was more limited.”(N1)
“I think it is difficult for the professional to give information and for the patient to receive it because of the PPE. However, I saw better communication between colleagues than, for example, with the family, which was the big problem at the beginning of the pandemic.”(N12)
“Young people communicated better with their relatives than older people. Of course, I am referring to communication via telephone because communication in person has been lost.”(N6)
“(…) the work dynamic in emergency situations was good, because in the end, once the team does what needs to be done, it will always be backed by the team that is outside (…)”(N7)
“(…) in situations of emergency, all of us wear our armor, and we have to take risks to save a life; in that situation, communication is adequate for the situation you are facing (…)”(N3)
“(…) communication was increased to its highest degree (…)”(N5)
3.1.2. Communicative Expression: Non-Verbal
“You don’t see the facial expression; with PPE, you can hardly perform non-verbal communication. I think you get more information with the eyes when you wear PPE.”(N1)
“(…) I notice it in the eyes, by looking at my colleagues’ eyes, I can tell if they are OK or not…by the gestures, in the manner in which they sit or walk, in the way they say hi…in my case, I have learned how to look at my colleagues’ eyes, and tell if he is tired or angry…I have learned how to observe all the gestures and behaviors, the manner in which they talk, and especially the way they look, to know how they are feeling…it’s complicated, and I supposed that it depends on how observant you become (…)”(N3)
“(...) now it’s all eyes and voice (...) communication is something basic, you have to work on it every day, whether it’s with your eyes, gestures or whatever (...)”(N2)
3.1.3. Limitations in Communication
“(…) what happened to me is that deaf-mute people came, and it was a real problem, because obviously a mute-deaf person will look at your lips, but since you are wearing a mask, they can’t.”(N3)
“(…) it’s more difficult, and you also don’t have skills to tend to these patients, I’m not sure if what I transmitted got to them correctly.”(N5)
“I noticed it was more difficult to communicate with people with disabilities, but we used slates or signs... you survive to understand the patient.”(N7)
3.2. Dimension 2. Emotional Aspects
3.2.1. Positive Aspects
“(…) I felt completely committed to the cause, with solidarity. It has been very intense. The comradeship came to the surface, and I had the satisfaction of taking the work forward day by day (...) My conscience is clear. I have to say that I have learned a lot, and I have acquired new knowledge and incorporated it. I have also become aware of the responsibility we have.”(N5)
“(…) I saw a high degree of camaraderie (…)”(N10)
3.2.2. Negative Aspects
“(…) it was like a war, but without knowing the enemy, you knew you had an enemy who could give you a deadly disease, then you would say: ‘well, what means do I have to face this’ (…) I was overcome with emotions, at first I cried a lot (…) The feeling was fear, always a lot of fear when thinking if I had become infected (…)”(N5)
“(…) it’s hard for people to understand what we health workers went through; it would change a lot of behaviors in society in general.”(N11)
3.3. Dimension 3. Overload
3.3.1. First Wave
“(…) we were afraid of not knowing if we were doing things right (…)”(N10)
“It was all speculation because nothing was known. There was a lack of information, we didn’t even know how to use a PPE. The health centers were closed, and we only attended emergencies, acute care, or wound cleaning. We were finding out new things every day. There was more information in primary care than in specialized care at the beginning. We did things like in other ICUs but without really knowing why... they didn’t train us...”(N9)
3.3.2. Second Wave
“Conditions improved over the following months. I learned to deal with stress, uncertainty, and chaos. New protocols were introduced (...) to this day.”(N8)
“(…) dealing with the shifts was better with time and with the experience we gained, also gaining confidence little by little (…)”(N2)
3.3.3. Third Wave
“(…) although it was very, very hard, and perhaps the hardest from what was experienced in the entire region (…), but you face it differently.”(N6)
“It was the hardest working period of all, but we had the situation under control.”(N8)
“The key point was when we got vaccinated, it was a bit of a liberation.”(N10)
3.4. Dimension 4. Relationships
3.4.1. Health Professionals–Patient
“You try to convey affection, but with PPE, it is more difficult. You spend less time in the rooms with the patient. You are left ‘affected’ after experiencing this, the suffering during the shift and the feeling of sorrow for not being able to save many patients.”(N5)
“(...) Fear and caution when approaching the patient (...) you thought of all of them as suspects of being infected or being infected yourself and infecting others. At the beginning, the relationship was more distant; now, a little less. In general, there was less communication with the patients, less face-to-face care, and more telephone care. With the patients who had BIPAP, it was more difficult to communicate.”(N12)
“(…) at first, you did what you had to do, and you left the room, and now, thanks to the vaccination, we have lost some of the fear, you feel safer, and we have more information (…)”(N2)
“(…) at first, you couldn’t make great efforts in patient care because you had to leave the room quickly, and now we know more (…)”(N6)
“Communication has worsened because of the barriers. Patients were inside the box, and you had to talk to them from the other side of the door. We didn’t have the means to improve communication at the beginning (tablets or telephones inside the box), but when we went in to do something to the patient, we would explain or let them know that we were there to help them. Depending on what the patient asked you for, you gave them more or less information... but we never withheld information from the patients.”(N9)
3.4.2. Healthcare Professionals
“More bonding between colleagues, to a greater extent in the ICU because we were all new and without knowledge. We had great support from the referring nurses. We helped each other a lot in any way we could. It has been very intense and an exceptional experience with an incredible connection, very intense work shifts, and you saw your colleague who was the same as you. New knowledge at a rapid pace. Colleagues from another hospital came to help us.”(N4)
“(…) it’s hard to forget, it was everything, 12-h shifts ‘to the death,’ but you had your colleague there, and with just one look, you knew that she was feeling the same way, but we supported each other, the camaraderie was spectacular and hard to forget, for me, these will remain in my heart for the rest of my life (…)”(N5)
3.4.3. Patients–Family
“We try to get them to communicate every day, especially those with limitations, by providing them with a tablet. Those who took a sudden turn for the worse did not have time to talk to anyone. Visits were not allowed to avoid the spread of infections, but in special situations, they were allowed, but the family member had to wear a PPE (to say goodbye, for example).”(N2)
“(…) for the patients who were conscious, we made sure they had a telephone or table to speak to their families (…)”(N8)
“(…) it was very hard, because it’s not the same thing to see them on the screen than in person, because you cannot touch, it’s been a big problem (…)”(N5)
3.4.4. Family–Health Professionals
“(…) communication was promoted, with a greater number of telephone calls to the family to provide information although I think it worsened, as they could not be there in person (…)”(N9)
“(…) the family members were a lot more understanding; after observing our working conditions, they waited patiently because we were doing everything possible (…)”(M1)
“The relatives have been much more understanding when they see how and in what conditions we were working. They made the task much easier; they waited patiently because they knew we are doing our best. People were afraid and understood the situation. They were informed at all times, but people waited patiently and didn’t resent our work so much.”(N8)
4. Discussion
4.1. Key Practice/Policy Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pallarés Carratalá, V.; Górriz-Zambrano, C.; Llisterri Caro, J.L.; Gorriz, J.L. The COVID-19 pandemic: An opportunity to change the way we care for our patients. Semergen 2020, 46 (Suppl. 1), 3–5. [Google Scholar] [CrossRef] [PubMed]
- Johns Hopkins University. Covid-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. Available online: https://coronavirus.jhu.edu/map.html (accessed on 10 May 2020).
- Castilla, J.; Moreno-Iribas, C.; Ibero Esparza, C.; Martínez-Baz, I.; Trobajo-Sanmartín, C.; Ezpeleta, C.; Guevara, M.; Grupo para el Estudio de COVID-19 en Navarra. Primera onda pandémica de COVID-19 en Navarra, febrero-junio 2020. An. Sist. Sanit. Navar. 2021, 1–12. [Google Scholar] [CrossRef]
- De Nicolás Jiménez, J.M.; Blázquez Recio, L.M.; Fabregat Domínguez, M.T.; Palomo Cobos, L. COVID-19 y esfuerzo asistencial en atención primaria. Aten. Primaria 2020, 52, 588–590. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Villegas, A.; Bautista-Mesa, R.J.; Baena-Lopez, M.A.; Garzon-Miralles, A.; Castellano-Ortega, M.A.; Leal-Costa, C.; Peiro, S. Impact of the COVID-19 Pandemic on Healthcare Activity in the Regional Hospitals of Andalusia (Spain). J. Clin. Med. 2022, 11, 363. [Google Scholar] [CrossRef]
- Soriano, J.B.; Gerli, A.G.; Centanni, S.; Ancochea, J. Forecasting COVID-19 Infection Trends and New Hospital Admissions in Spain Due to SARS-CoV-2 Variant of Concern Omicron. Arch. Bronconeumol. 2022; in press. [Google Scholar] [CrossRef]
- Red Nacional de Vigilancia Epidemiológica. Analysis of COVID-19 Cases in Health Personnel in Spain; Instituto Carlos III: Madrid, Spain, 2020. [Google Scholar]
- Rodriguez-Menéndez, G.; Rubio-García, A.; Conde-Alvarez, P.; Armesto-Luque, L.; Garrido-Torres, N.; Capitan, L.Á.; Luque, A.; Ruiz-Veguilla, M.; Crespo-Facorro, B. Short-Term Emotional Impact of COVID-19 Pandemic on Spaniard Health Workers. J. Affect. Disord. 2021, 278, 390–394. [Google Scholar] [CrossRef]
- Pulido-Fuentes, M.; Flores-Martos, J.A.; Abad-González, L.; Navarta-Sánchez, M.V.; Valera-Oviedo, L.; Cipriano-Crespo, C. Emotions in the Time of COVID-19: Affections and Impacts among the Spanish Primary Care Workforce. Healthcare 2021, 9, 1723. [Google Scholar] [CrossRef]
- Consejería de Salud Región de Murcia Murciasalud. The Health Portal of the Region of Murcia. Hospital Catalog. Available online: http://www.murciasalud.es/seccion.php?idsec=45 (accessed on 29 December 2021).
- Back, A.; Tulsky, J.A.; Arnold, R.M. Communication Skills in the Age of COVID-19. Ann. Intern. Med. 2020, 172, 759–760. [Google Scholar] [CrossRef] [Green Version]
- Rubinelli, S.; Myers, K.; Rosenbaum, M.; Davis, D. Implications of the Current COVID-19 Pandemic for Communication in Healthcare. Patient Educ. Couns. 2020, 103, 1067–1069. [Google Scholar] [CrossRef]
- Werder, O. Toward a Humanistic Model in Health Communication. Glob. Health Promot. 2019, 26, 33–40. [Google Scholar] [CrossRef]
- Leal-Costa, C.; Tirado-González, S.; van-der Hofstadt Román, C.J.; Rodríguez-Marín, J. Creation of the Communication Skills Scale in Health Professionals, CSS-HP. An. Psicol. 2016, 32, 49–59. [Google Scholar] [CrossRef]
- Martín Padilla, E.; Sarmiento Medina, P.; Ramírez Jaramillo, A. Professional communication in long term health care quality. Rev. Calid. Asist. Organo Soc. Espanola Calid. Asist. 2014, 29, 135–142. [Google Scholar] [CrossRef]
- Smith, G.D.; Ng, F.; Ho Cheung Li, W. COVID-19: Emerging Compassion, Courage and Resilience in the Face of Misinformation and Adversity. J. Clin. Nurs. 2020, 29, 1425–1428. [Google Scholar] [CrossRef] [Green Version]
- Leal-Costa, C.; Díaz-Agea, J.L.; Tirado-González, S.; Rodríguez-Marín, J.; van-der Hofstadt, C.J. Communication skills: A preventive factor in Burnout syndrome in health professionals. An. Sist. Sanit. Navar. 2015, 38, 213–223. [Google Scholar] [CrossRef]
- Fuertes Goñi, C.; Aranda Auserón, G.; Arroyo Anies, M.P. Communication and mindfulness to prevent burnout. An. Sist. Sanit. Navar. 2016, 39, 331–333. [Google Scholar] [CrossRef]
- Yuguero, O.; Forné, C.; Esquerda, M.; Pifarré, J.; Abadías, M.J.; Viñas, J. Empathy and Burnout of Emergency Professionals of a Health Region: A Cross-Sectional Study. Medicine 2017, 96, e8030. [Google Scholar] [CrossRef]
- Llor Lozano, J.; Seva Llor, A.M.; Díaz Agea, J.L.; Llor Gutiérrez, L.; Leal Costa, C. Burnout, Habilidades de Comunicación y Autoeficacia En Los Profesionales de Urgencias y Cuidados Críticos. Enferm. Glob. 2020, 19, 68–92. [Google Scholar] [CrossRef]
- Leonard, M.; Graham, S.; Bonacum, D. The Human Factor: The Critical Importance of Effective Teamwork and Communication in Providing Safe Care. BMJ Qual. Saf. 2004, 13, i85–i90. [Google Scholar] [CrossRef] [Green Version]
- Alvarez Aparicio, A.I. Communication of bad news in the health field in times of COVID-19. Telephone. Rev. Comun. Salud 2020, 10, 211–248. [Google Scholar]
- Handberg, C.; Voss, A.K. Implementing Augmentative and Alternative Communication in Critical Care Settings: Perspectives of Healthcare Professionals. J. Clin. Nurs. 2018, 27, 102–114. [Google Scholar] [CrossRef]
- Calle, G.H.L.; Martin, M.C.; Nin, N. Seeking to Humanize Intensive Care. Rev. Bras. Ter. Intensiva 2017, 29, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Slatore, C.G.; Hansen, L.; Ganzini, L.; Press, N.; Osborne, M.L.; Chesnutt, M.S.; Mularski, R.A. Communication by Nurses in the Intensive Care Unit: Qualitative Analysis of Domains of Patient-Centered Care. Am. J. Crit. Care Off. Publ. Am. Assoc. Crit.-Care Nurses 2012, 21, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Castro-Martinez, A.; Diaz-Morilla, P. Management of internal and external communication in private hospitals in Spain during the COVID-19 crisis. Rev. Comun. Salud 2020, 10, 525–547. [Google Scholar]
- Mast, M.S. On the Importance of Nonverbal Communication in the Physician-Patient Interaction. Patient Educ. Couns. 2007, 67, 315–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mheidly, N.; Fares, M.Y.; Zalzale, H.; Fares, J. Effect of Face Masks on Interpersonal Communication during the COVID-19 Pandemic. Front. Public Health 2020, 8, 898. [Google Scholar] [CrossRef] [PubMed]
- Baron, R.A.; Byrne, D.; Branscombe, N.R. Social Psychology; Pearson: Boston, MA, USA, 2006. [Google Scholar]
- Shurlock, J.; Rudd, J.; Jeanes, A.; Iacovidou, A.; Creta, A.; Kanthasamy, V.; Schilling, R.; Sullivan, E.; Cooke, J.; Laws-Chapman, C.; et al. Communication in the Intensive Care Unit during COVID-19: Early Experience with the Nightingale Communication Method. Int. J. Qual. Health Care J. Int. Soc. Qual. Health Care 2021, 33, mzaa162. [Google Scholar] [CrossRef] [PubMed]
- Morse, J.M. The Significance of Saturation. Qual. Health Res. 1995, 5, 147–149. [Google Scholar] [CrossRef]
- Bianchi, M.; Prandi, C.; Bonetti, L. Experience of Middle Management Nurses during the COVID-19 Pandemic in Switzerland: A Qualitative Study. J. Nurs. Manag. 2021, 29, 1956–1964. [Google Scholar] [CrossRef]
- Kwaghe, A.V.; Ilesanmi, O.S.; Amede, P.O.; Okediran, J.O.; Utulu, R.; Balogun, M.S. Stigmatization, Psychological and Emotional Trauma among Frontline Health Care Workers Treated for COVID-19 in Lagos State, Nigeria: A Qualitative Study. BMC Health Serv. Res. 2021, 21, 855. [Google Scholar] [CrossRef]
- Leever, A.M.; Hulst, M.V.D.; Berendsen, A.J.; Boendemaker, P.M.; Roodenburg, J.L.N.; Pols, J. Conflicts and Conflict Management in the Collaboration between Nurses and Physicians—A Qualitative Study. J. Interprof. Care 2010, 24, 612–624. [Google Scholar] [CrossRef]
- Angland, S.; Dowling, M.; Casey, D. Nurses’ Perceptions of the Factors Which Cause Violence and Aggression in the Emergency Department: A Qualitative Study. Int. Emerg. Nurs. 2014, 22, 134–139. [Google Scholar] [CrossRef]
- Zahavi, D.; Martiny, K.M.M. Phenomenology in Nursing Studies: New Perspectives. Int. J. Nurs. Stud. 2019, 93, 155–162. [Google Scholar] [CrossRef]
- Edward, K.-L.; Welch, T. The Extension of Colaizzi’s Method of Phenomenological Enquiry. Contemp. Nurse 2011, 39, 163–171. [Google Scholar] [CrossRef]
- Van Rijnsoever, F.J. (I Can’t Get No) Saturation: A Simulation and Guidelines for Sample Sizes in Qualitative Research. PLoS ONE 2017, 12, e0181689. [Google Scholar] [CrossRef] [Green Version]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care J. Int. Soc. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [Green Version]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, N.R.; Steinberg, A.; Arnold, R.M.; Doshi, A.A.; White, D.B.; DeLair, W.; Nigra, K.; Elmer, J. Perspectives on Telephone and Video Communication in the Intensive Care Unit during COVID-19. Ann. Am. Thorac. Soc. 2021, 18, 838–847. [Google Scholar] [CrossRef]
- Monin, J.K.; Ali, T.; Syed, S.; Piechota, A.; Lepore, M.; Mourgues, C.; Gaugler, J.E.; Marottoli, R.; David, D. Family Communication in Long-Term Care During a Pandemic: Lessons for Enhancing Emotional Experiences. Am. J. Geriatr. Psychiatry Off. J. Am. Assoc. Geriatr. Psychiatry 2020, 28, 1299–1307. [Google Scholar] [CrossRef]
- Finset, A.; Bosworth, H.; Butow, P.; Gulbrandsen, P.; Hulsman, R.L.; Pieterse, A.H.; Street, R.; Tschoetschel, R.; van Weert, J. Effective Health Communication—A Key Factor in Fighting the COVID-19 Pandemic. Patient Educ. Couns. 2020, 103, 873–876. [Google Scholar] [CrossRef]
- Lord, H.; Loveday, C.; Moxham, L.; Fernandez, R. Effective Communication Is Key to Intensive Care Nurses’ Willingness to Provide Nursing Care amidst the COVID-19 Pandemic. Intensive Crit. Care Nurs. 2021, 62, 102946. [Google Scholar] [CrossRef]
- Bowman, B.A.; Back, A.L.; Esch, A.E.; Marshall, N. Crisis Symptom Management and Patient Communication Protocols Are Important Tools for All Clinicians Responding to COVID-19. J. Pain Symptom Manage. 2020, 60, e98–e100. [Google Scholar] [CrossRef]
- Xu, H.; Stjernswärd, S.; Glasdam, S. Psychosocial Experiences of Frontline Nurses Working in Hospital-Based Settings during the COVID-19 Pandemic—A Qualitative Systematic Review. Int. J. Nurs. Stud. Adv. 2021, 3, 100037. [Google Scholar] [CrossRef] [PubMed]
- Leal-Costa, C.; Díaz-Agea, J.L.; Ruzafa-Martínez, M.; Ramos-Morcillo, A.J. Work-related stress amongst health professionals in a pandemic. An. Sist. Sanit. Navar. 2021, 44, 123–124. [Google Scholar] [CrossRef] [PubMed]
- Orcajada Muñoz, I.; Amo Setien, F.J.; Díaz Agea, J.L.; Hernández Ruipérez, T.; de Adánez Martínez, M.G.; Leal Costa, C. The Communication Skills and Quality Perceived in an Emergency Department: The Patient’s Perspective. Int. J. Nurs. Pract. 2020, 26, e12831. [Google Scholar] [CrossRef] [PubMed]
- Leal-Costa, C.; Tirado González, S.; Ramos-Morcillo, A.J.; Ruzafa-Martínez, M.; Díaz Agea, J.L.; van-der Hofstadt Román, C.J. Communication Skills and Professional Practice: Does It Increase Self-Efficacy in Nurses? Front. Psychol. 2020, 11, 1169. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.J.; Lim, O.B.; Shim, J.L. Critical Care Nurses’ Communication Experiences with Patients and Families in an Intensive Care Unit: A Qualitative Study. PLoS ONE 2020, 15, e0235694. [Google Scholar] [CrossRef]
- Hampton, T.; Crunkhorn, R.; Lowe, N.; Bhat, J.; Hogg, E.; Afifi, W.; De, S.; Street, I.; Sharma, R.; Krishnan, M.; et al. The Negative Impact of Wearing Personal Protective Equipment on Communication during Coronavirus Disease 2019. J. Laryngol. Otol. 2020, 134, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Muzzi, E.; Chermaz, C.; Castro, V.; Zaninoni, M.; Saksida, A.; Orzan, E. Short Report on the Effects of SARS-CoV-2 Face Protective Equipment on Verbal Communication. Eur. Arch. Oto-Rhino-Laryngol. 2021, 278, 3565–3570. [Google Scholar] [CrossRef]
- Neves, H.C.C.; Souza, A.C.S.e; Medeiros, M.; Munari, D.B.; Ribeiro, L.C.M.; Tipple, A.F.V. Safety of Nursing Staff and Determinants of Adherence to Personal Protective Equipment. Rev. Lat. Am. Enferm. 2011, 19, 354–361. [Google Scholar] [CrossRef] [Green Version]
- Alarfaj, M.A.; Foula, M.S.; Alshammary, S.; Nwesar, F.A.; Eldamati, A.M.; Alomar, A.; Abdulmomen, A.A.; Alarfaj, L.; Almulhim, A.; Alarfaj, O.; et al. Impact of Wearing Personal Protective Equipment on the Performance and Decision Making of Surgeons during the COVID-19 Pandemic: An Observational Cross-Sectional Study. Medicine 2021, 100, e27240. [Google Scholar] [CrossRef]
- Marler, H.; Ditton, A. “I’m Smiling Back at You”: Exploring the Impact of Mask Wearing on Communication in Healthcare. Int. J. Lang. Commun. Disord. 2021, 56, 205–214. [Google Scholar] [CrossRef]
- Goggin, G.; Ellis, K. Disability, Communication, and Life Itself in the COVID-19 Pandemic. Health Sociol. Rev. J. Health Sect. Aust. Sociol. Assoc. 2020, 29, 168–176. [Google Scholar] [CrossRef]
- Sabatello, M.; Burke, T.B.; McDonald, K.E.; Appelbaum, P.S. Disability, Ethics, and Health Care in the COVID-19 Pandemic. Am. J. Public Health 2020, 110, 1523–1527. [Google Scholar] [CrossRef]
- Rojo-Rojo, A.; Soto-Castellón, M.B.; García-Méndez, J.A.; Leal-Costa, C.; Adánez-Martínez, M.G.; Pujalte-Jesús, M.J.; Díaz-Agea, J.L. Training with High Fidelity Simulation in the Care of Patients with Coronavirus—A Learning Experience in Native Health Care Multi-Professional Teams. Healthcare 2021, 9, 1260. [Google Scholar] [CrossRef]
- Nogueira Rodrigues, M.E.; da Costa Belarmino, A.; Lopes Custódio, L.; Verde Gomes, I.L.; Rodrigues Ferreira, A. Communication in Health Work during the COVID-19 Pandemic. Investig. Educ. En Enfermeria 2020, 38, e9. [Google Scholar] [CrossRef]
- Bhavya, R.; Sambhav, S. Role of Mobile Communication with Emerging Technology in COVID-19. Int. J. Adv. Trends Comput. Sci. Eng. 2020, 9, 3338–3344. [Google Scholar] [CrossRef]
- Verhagen, L.M.; de Groot, R.; Lawrence, C.A.; Taljaard, J.; Cotton, M.F.; Rabie, H. COVID-19 Response in Low- and Middle-Income Countries: Don’t Overlook the Role of Mobile Phone Communication. Int. J. Infect. Dis. 2020, 99, 334–337. [Google Scholar] [CrossRef]
- Wu, A.W.; Connors, C.; Everly, G.S. COVID-19: Peer Support and Crisis Communication Strategies to Promote Institutional Resilience. Ann. Intern. Med. 2020, 172, 822–823. [Google Scholar] [CrossRef] [Green Version]
- Creese, J.; Byrne, J.-P.; Matthews, A.; McDermott, A.M.; Conway, E.; Humphries, N. “I Feel I Have No Voice”: Hospital Doctors’ Workplace Silence in Ireland. J. Health Organ. Manag. 2021, 35, 178–194. [Google Scholar] [CrossRef]
- Adkins, K. Exit Only: Harms from Silencing Employee Voice. J. Sci. Commun. 2020, 19, A03. [Google Scholar] [CrossRef]
| Number Code/Sex | Workplace | Age | Experience (Years) | Hospital |
|---|---|---|---|---|
| N1/Female | Emergencies | 28 | 3 | H1 |
| N2/Female | COVID Hospital Unit | 37 | 8 | H2 |
| N3/Female | Emergency Radiology Diagnosis | 30 | 5 | |
| N4/Male | Emergencies | 33 | 4 | |
| N5/Male | Emergencies | 27 | 6 | |
| N6/Female | ICU | 41 | 9 | H3 |
| N7/Female | ICU | 31 | 4 | |
| N8/Female | ICU | 53 | 18 | |
| N9/Female | ICU | 32 | 6 | |
| N10/Male | ICU | 34 | 8 | H4 |
| N11/Male | ICU | 33 | 5 | |
| N12/Male | Emergencies | 64 | 20 | H5 |
| Personal experience before the pandemic and initial experiences at the start of the pandemic |
| How would you describe your process of adaptation during the last few months until today? Please explain to me what the process entailed for you to go to work every day in an environment with COVID-positive patients |
| Feelings perceived during the different waves of the pandemic |
| How was the communication between the health professionals and the patients? What happened with the patients subjected to NIV *? |
| Please tell us about any experience about patients who had to be intubated quickly, without being able to say good-bye, if this occurred in your presence |
| Do you think the patient received the same amount of information about his/her disease as if the pandemic had not occurred? |
| Can you describe the communication between health professionals during the pandemic? Do you think communication has been negatively affected? |
| Before the pandemic, do you think you could have better interpreted the mood of a colleague at the hospital? |
| Do you think the relationships between colleagues have been affected by the pandemic? Explain your answer |
| What advice would you give to a colleague who is starting work at the same service you are at in order to effectively communicate with patients and the other health professionals? |
| After the workday, when you are at home, have you had to deal with some feelings? How would describe it/them? |
| As for the training for dealing with the pandemic, what aspects would you highlight? |
| Have you dealt with patients with a communication difficulty or with people who have some type of limitation or disability? Do you think the distancing protocols and personal protection equipment have had an influence on communication? |
| Have you noticed some alterations in communication with respect to the patient’s families and the health professionals during the pandemic? |
| Dimension | Category | Sub-Category |
|---|---|---|
| Communication | Communicative expression | Verbal:
|
Non-verbal:
| ||
| Limitations |
| |
| Emotional aspects | Positive |
|
| Negative |
| |
| Overload | First wave |
|
| Second wave |
| |
| Third wave |
| |
| Relationships | Professionals–patients |
|
| Healthcare professionals |
| |
| Patients–family |
| |
| Family–professionals |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz-Agea, J.L.; Orcajada-Muñoz, I.; Leal-Costa, C.; Adánez-Martínez, M.G.; De Souza Oliveira, A.C.; Rojo-Rojo, A. How Did the Pandemic Affect Communication in Clinical Settings? A Qualitative Study with Critical and Emergency Care Nurses. Healthcare 2022, 10, 373. https://doi.org/10.3390/healthcare10020373
Díaz-Agea JL, Orcajada-Muñoz I, Leal-Costa C, Adánez-Martínez MG, De Souza Oliveira AC, Rojo-Rojo A. How Did the Pandemic Affect Communication in Clinical Settings? A Qualitative Study with Critical and Emergency Care Nurses. Healthcare. 2022; 10(2):373. https://doi.org/10.3390/healthcare10020373
Chicago/Turabian StyleDíaz-Agea, José Luis, Irene Orcajada-Muñoz, César Leal-Costa, Maria Gracia Adánez-Martínez, Adriana Catarina De Souza Oliveira, and Andrés Rojo-Rojo. 2022. "How Did the Pandemic Affect Communication in Clinical Settings? A Qualitative Study with Critical and Emergency Care Nurses" Healthcare 10, no. 2: 373. https://doi.org/10.3390/healthcare10020373
APA StyleDíaz-Agea, J. L., Orcajada-Muñoz, I., Leal-Costa, C., Adánez-Martínez, M. G., De Souza Oliveira, A. C., & Rojo-Rojo, A. (2022). How Did the Pandemic Affect Communication in Clinical Settings? A Qualitative Study with Critical and Emergency Care Nurses. Healthcare, 10(2), 373. https://doi.org/10.3390/healthcare10020373








