White Spots Prevalence and Tooth Brush Habits during Orthodontic Treatment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients’ Selection
2.2. The Examination of Teeth Surfaces
2.3. Statistical Analysis
3. Results
3.1. Prevalence of WS Lesion
3.2. Distribution of WS Lesion on the Affected Teeth
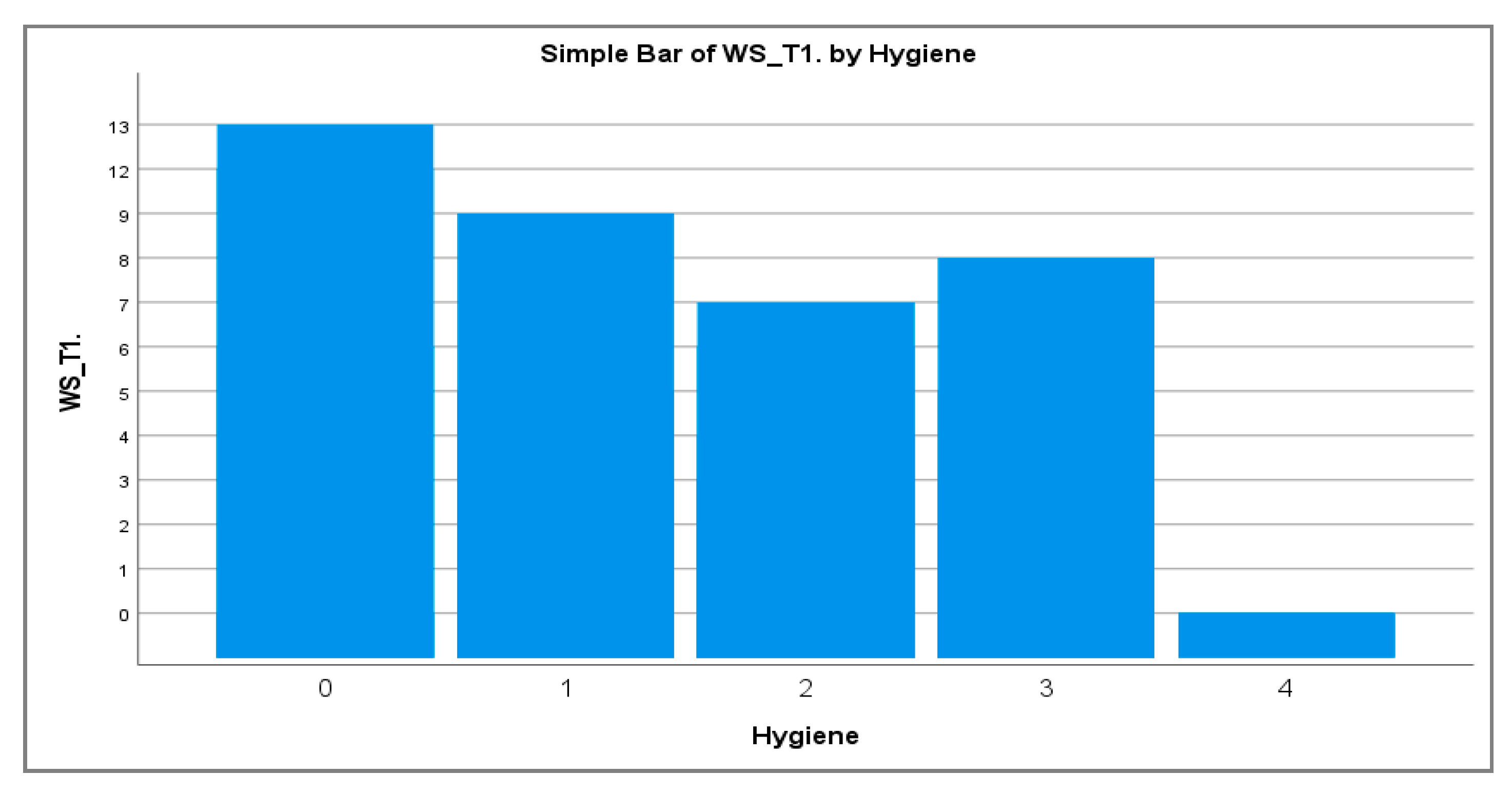
3.3. Correlation of Tooth Brushing Habits Related to WS Lesion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tavares, M.I.; Saraiva, J.; do Vale, F.; Coelho, A.S.; Amaro, I.F.; Marto, C.M.; Francisco, I.; Ferreira, M.M.; Paula, A.B.; Carrilho, E.V. Resin infiltration in white spot lesions caused by orthodontic hypomineralisation: A minimally invasive therapy. Br. Dent. J. 2021, 231, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Sundararaj, D.; Venkatachalapathy, S.; Tandon, A.; Pereira, A. Critical evaluation of incidence and prevalence of white spot lesions during fixed orthodontic appliance treatment: A meta-analysis. J. Int. Soc. Prev. Community Dent. 2015, 5, 433–439. [Google Scholar] [PubMed] [Green Version]
- Sudjalim, T.R.; Woods, M.G.; Manton, D.J. Prevention of white spot lesions in orthodontic practice: A contemporary review. Aust. Dent. J. 2006, 51, 284–289. [Google Scholar] [CrossRef]
- Puleio, F.; Fiorillo, L.; Gorassini, F.; Iandolo, A.; Meto, A.; D’Amico, C.; Cervino, G.; Pinizzotto, M.; Bruno, G.; Portelli, M.; et al. Systematic Review on White Spot Lesions Treatments. Eur. J. Dent. 2021. [Google Scholar] [CrossRef] [PubMed]
- Gorelick, L.; Geiger, A.M.; Gwinnett, A.J. Incidence of white spot formation after bonding and banding. Am. J. Orthod. 1982, 81, 93–98. [Google Scholar] [CrossRef]
- Lucchese, A.; Gherlone, E. Prevalence of white-spot lesions before and during orthodontic treatment with fixed appliances. Eur. J. Orthod. 2013, 35, 664–668. [Google Scholar] [CrossRef] [Green Version]
- Rosenbloom, R.G.; Tinanoff, N. Salivary Streptococcus mutans levels in patients before, during, and after orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1991, 100, 35–37. [Google Scholar] [CrossRef]
- Selwitz, R.H.; Ismail, A.I.; Pitts, N.B. Dental caries. Lancet 2007, 369, 51–59. [Google Scholar] [CrossRef]
- Maxfield, B.J.; Hamdan, A.M.; Tüfekçi, E.; Shroff, B.; Best, A.M.; Lindauer, S.J. Development of white spot lesions during orthodontic treatment: Perceptions of patients, parents, orthodontists, and general dentists. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 337–344. [Google Scholar] [CrossRef]
- Tufekci, E.; Dixon, J.S.; Gunsolley, J.C.; Lindauer, S.J. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011, 81, 206–210. [Google Scholar] [CrossRef] [Green Version]
- Al-Khateeb, S.; Cate, J.T.; Angmar-Månsson, B.; Jong, E.D.J.D.; Sundström, G.; Exterkate, R.; Oliveby, A. Quantification of formation and remineralization of artificial enamel lesions with a new portable fluorescence device. Adv. Dent. Res. 1997, 11, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Guzmán-Armstrong, S.; Chalmers, J.; Warren, J.J. White spot lesions: Prevention and treatment. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Lopatiene, K.; Borisovaite, M.; Lapenaite, E. Prevention and Treatment of White Spot Lesions During and After Treatment with Fixed Orthodontic Appliances: A Systematic Literature Review. J. Oral Maxillofac. Res. 2016, 7, e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mizrahi, E. Enamel demineralization following orthodontic treatment. Am. J. Orthod. 1982, 82, 62–67. [Google Scholar] [CrossRef]
- Julien, K.C.; Buschang, P.H.; Campbell, P.M. Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod. 2013, 83, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Hadler-Olsen, S.; Sandvik, K.; El-Agroudi, M.A.; Øgaard, B. The incidence of caries and white spot lesions in orthodontically treated adolescents with a comprehensive caries prophylactic regimen-a prospective study. Eur. J. Orthod. 2012, 34, 633–639. [Google Scholar] [CrossRef] [Green Version]
- Hysi, D.; Kuscu, O.O.; Droboniku, E.; Toti, C.; Xhemnica, L.; Caglar, E. Prevalence and aetiology of Molar-Incisor Hypomineralisation among children aged 8-10 years in Tirana, Albania. Eur. J. Paediatr. Dent. 2016, 17, 75–79. [Google Scholar]
- Lygidakis, N.A.; Wong, F.; Jälevik, B.; Vierrou, A.M.; Alaluusua, S.; Espelid, I. Best Clinical Practice Guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): An EAPD Policy Document. Eur. Arch. Paediatr. Dent. 2010, 11, 75–81. [Google Scholar] [CrossRef]
- Boersma, J.G.; van der Veen, M.H.; Lagerweij, M.D.; Bokhout, B.; Prahl-Andersen, B. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: Influencing factors. Caries Res. 2005, 39, 41–47. [Google Scholar] [CrossRef]
- Geiger, A.M.; Gorelick, L.; Gwinnett, A.J.; Griswold, P.G. The effect of a fluoride program on white spot formation during orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1988, 93, 29–37. [Google Scholar] [CrossRef]
- Khalaf, K. Factors Affecting the Formation, Severity and Location of White Spot Lesions during Orthodontic Treatment with Fixed Appliances. J. Oral Maxillofac. Res. 2014, 5, e4. [Google Scholar] [CrossRef] [Green Version]
- Kozak, U.; Sękowska, A.; Chałas, R. The Effect of Regime Oral-Hygiene Intervention on the Incidence of New White Spot Lesions in Teenagers Treated with Fixed Orthodontic Appliances. Int. J. Environ. Res. Public Health 2020, 17, 9460. [Google Scholar] [CrossRef] [PubMed]
- Kühnisch, J.; Ekstrand, K.; Pretty, I.A.; Twetman, S.; Van Loveren, C.; Gizani, S.; Loizidou, M.S. Best clinical practice guidance for management of early caries lesions in children and young adults: An EAPD policy document. Eur. Arch. Paediatr. Dent. 2016, 17, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Meto, A.; Colombari, B.; Odorici, A.; Giva, L.B.; Pericolini, E.; La Regina, A.; Blasi, E. Antibacterial Effects of MicroRepair®BIOMA-Based Toothpaste and Chewing Gum on Orthodontic Elastics Contaminated In Vitro with Saliva from Healthy Donors: A Pilot Study. Appl. Sci. 2020, 10, 6721. [Google Scholar] [CrossRef]
- Lovrov, S.; Hertrich, K.; Hirschfelder, U. Enamel Demineralization during Fixed Orthodontic Treatment—Incidence and Correlation to Various Oral-hygiene Parameters. J. Orofac. Orthop. 2007, 68, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L. Oral Health: The First Step to Well-Being. Medicina 2019, 55, 676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cosma, L.L.; Şuhani, R.D.; Mesaroş, A.; Badea, M.E. Current treatment modalities of orthodontically induced white spot lesions and their outcome—a literature review. Med. Pharm. Rep. 2019, 92, 25–30. [Google Scholar] [CrossRef]
- Nascimento, P.L.; Fernandes, M.T.; Figueiredo, F.E.; Faria-E-Silva, A.L. Fluoride-Releasing Materials to Prevent White Spot Lesions around Orthodontic Brackets: A Systematic Review. Braz. Dent. J. 2016, 27, 101–107. [Google Scholar] [CrossRef]
- Gu, X.; Yang, L.; Yang, D.; Gao, Y.; Duan, X.; Zhu, X.; Yuan, H.; Li, J. Esthetic improvements of postorthodontic white-spot lesions treated with resin infiltration and microabrasion: A split-mouth, randomized clinical trial. Angle Orthod. 2019, 89, 372–377. [Google Scholar] [CrossRef] [Green Version]
- Shan, D.; He, Y.; Gao, M.; Liu, H.; Zhu, Y.; Liao, L.; Hadaegh, F.; Long, H.; Lai, W. A comparison of resin infiltration and microabrasion for postorthodontic white spot lesion. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 516–522. [Google Scholar] [CrossRef]
- Müller, L.K.; Jungbauer, G.; Jungbauer, R.; Wolf, M.; Deschner, J. Biofilm and Orthodontic Therapy. Monogr. Oral Sci. 2021, 29, 201–213. [Google Scholar] [PubMed]
- Contaldo, M.; Lucchese, A.; Lajolo, C.; Rupe, C.; Di Stasio, D.; Romano, A.; Petruzzi, M.; Serpico, R. The Oral Microbiota Changes in Orthodontic Patients and Effects on Oral Health: An Overview. J. Clin. Med. 2021, 10, 780. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.; Jongsma, M.A.; Mei, L.; van der Mei, H.C.; Busscher, H.J. Orthodontic treatment with fixed appliances and biofilm formation--a potential public health threat? Clin. Oral Investig. 2014, 18, 1711–1718. [Google Scholar] [CrossRef]
- Tušek, I.; O’Rourke, B.; Lekić, C.; Tušek, J.; Tušek, B. Early childhood caries in multilingual community. Cent. Eur. J. Public Health 2020, 28, 286–291. [Google Scholar] [CrossRef]
| Score | Examination Criteria |
|---|---|
| 0 | Sound tooth surface when probing: no evidence of caries after 5 s air drying |
| 1 | First visual change in enamel: opacity or discoloration (white or brown) is visible at the entrance to the pit or fissure after prolonged air drying |
| 2 | Distinct visual change is enamel visible when wet: lesion must still be visible when dry |
| WS | T1 | T2 | p-Value | ||
|---|---|---|---|---|---|
| Frequency | Percent (%) | Frequency | Percent (%) | ||
| 0 | 30 | 40.5 | 29 | 39.2 | p = 0.386 |
| 1 | 10 | 13.5 | 9 | 12.2 | |
| 2 | 9 | 12.2 | 10 | 13.5 | |
| 3 | 10 | 13.5 | 6 | 8.1 | |
| 4 | 3 | 4.1 | 6 | 8.1 | |
| 5 | 3 | 4.1 | 3 | 4.1 | |
| 6 | 3 | 4.1 | 2 | 2.7 | |
| 7 | 2 | 2.7 | 3 | 4.1 | |
| 8 | 1 | 1.4 | 1 | 1.4 | |
| 9 | 1 | 1.4 | 3 | 4.1 | |
| 10 | 0 | 0 | 1 | 1.4 | |
| 12 | 1 | 1.4 | 0 | 0 | |
| 13 | 1 | 1.4 | 1 | 1.4 | |
| Total | 74 | 100.0 | 74 | 100 | |
| WS | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 12 | 13 | Total | p Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | M | 13 | 5 | 3 | 3 | 0 | 1 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 29 | p = 0.043 |
| F | 17 | 5 | 6 | 7 | 3 | 2 | 1 | 2 | 0 | 1 | 0 | 1 | 1 | 45 | ||
| T2 | M | 11 | 6 | 4 | 2 | 1 | 1 | 2 | 0 | 0 | 1 | 0 | 0 | 1 | 29 | p = 0.060 |
| F | 18 | 3 | 6 | 4 | 5 | 2 | 0 | 3 | 1 | 2 | 1 | 0 | 0 | 45 |
| upper right (UR) central incisor | 11 | 7% |
| upper right (UR) lateral incisor | 8 | 5% |
| upper right (UR) canine (cuspid) | 9 | 6% |
| upper right (UR) first premolar (first bicuspid) | 4 | 3% |
| upper right (UR) second premolar (second bicuspid) | 2 | 1% |
| upper right (UR) first molar | 17 | 11% |
| upper left (UL) central incisor | 13 | 8% |
| upper left (UL) lateral incisor | 11 | 7% |
| upper left (UL) canine (cuspid) | 4 | 3% |
| upper left (UL) first premolar (first bicuspid) | 9 | 6% |
| upper left (UL) second premolar (second bicuspid) | 7 | 4% |
| upper left (UL) first molar | 23 | 15% |
| lower left (UL) central incisor | 2 | 1% |
| lower left (UL) first premolar (first bicuspid) | 2 | 1% |
| lower left (UL) second premolar (second bicuspid) | 1 | 1% |
| lower left (LL) first molar | 16 | 10% |
| lower right (LR) central incisor | 1 | 1% |
| lower right (LR) lateral incisor | 1 | 1% |
| lower right (LR) canine (cuspid) | 2 | 1% |
| lower right (LR) first premolar (first bicuspid) | 2 | 1% |
| lower right (LR) second premolar (second bicuspid) | 2 | 1% |
| lower right (LR) first molar | 9 | 6% |
| Tooth Brushing Frequency | Patients | Percent (%) |
|---|---|---|
| 0 | 6 | 8.1 |
| 1 | 13 | 18.9 |
| 2 | 41 | 58.1 |
| 3 | 8 | 12.2 |
| 4 | 1 | 2.7 |
| Total | 74 | 100.0 |
| Gender | Tooth Brushing Frequency | Total | p Value | ||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |||
| M | 2 | 9 | 16 | 1 | 1 | 29 | |
| F | 4 | 5 | 27 | 8 | 1 | 45 | p = 0.139 |
| Total | 6 | 14 | 43 | 9 | 2 | 74 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toti, Ç.; Meto, A.; Kaçani, G.; Droboniku, E.; Hysi, D.; Tepedino, M.; Zaja, E.; Fiorillo, L.; Meto, A.; Buci, D.; et al. White Spots Prevalence and Tooth Brush Habits during Orthodontic Treatment. Healthcare 2022, 10, 320. https://doi.org/10.3390/healthcare10020320
Toti Ç, Meto A, Kaçani G, Droboniku E, Hysi D, Tepedino M, Zaja E, Fiorillo L, Meto A, Buci D, et al. White Spots Prevalence and Tooth Brush Habits during Orthodontic Treatment. Healthcare. 2022; 10(2):320. https://doi.org/10.3390/healthcare10020320
Chicago/Turabian StyleToti, Çeljana, Agron Meto, Gerta Kaçani, Etleva Droboniku, Dorjan Hysi, Michele Tepedino, Edlira Zaja, Luca Fiorillo, Aida Meto, Denada Buci, and et al. 2022. "White Spots Prevalence and Tooth Brush Habits during Orthodontic Treatment" Healthcare 10, no. 2: 320. https://doi.org/10.3390/healthcare10020320
APA StyleToti, Ç., Meto, A., Kaçani, G., Droboniku, E., Hysi, D., Tepedino, M., Zaja, E., Fiorillo, L., Meto, A., Buci, D., & Tanellari, O. (2022). White Spots Prevalence and Tooth Brush Habits during Orthodontic Treatment. Healthcare, 10(2), 320. https://doi.org/10.3390/healthcare10020320










