Identifying Cardiovascular Risk Profiles Clusters among Mediterranean Adolescents across Seven Countries
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Research Design
2.3. Data Collection and Survey Instrument
2.4. Measures and Insatruments
2.4.1. Overweight and Obesity
2.4.2. Physical Activity Habits: Moderate Physical Activity
2.4.3. Physical Activity Habits: Vigorous Physical Activity
2.4.4. Smoking Habits
2.4.5. Alcohol Consumption Habits
2.5. Data Analysis
3. Results
3.1. Survey Findings: Sociodemographic Characteristics of the Total Sample
3.2. Modifiable Lifestyle Characteristics of the Total Sample
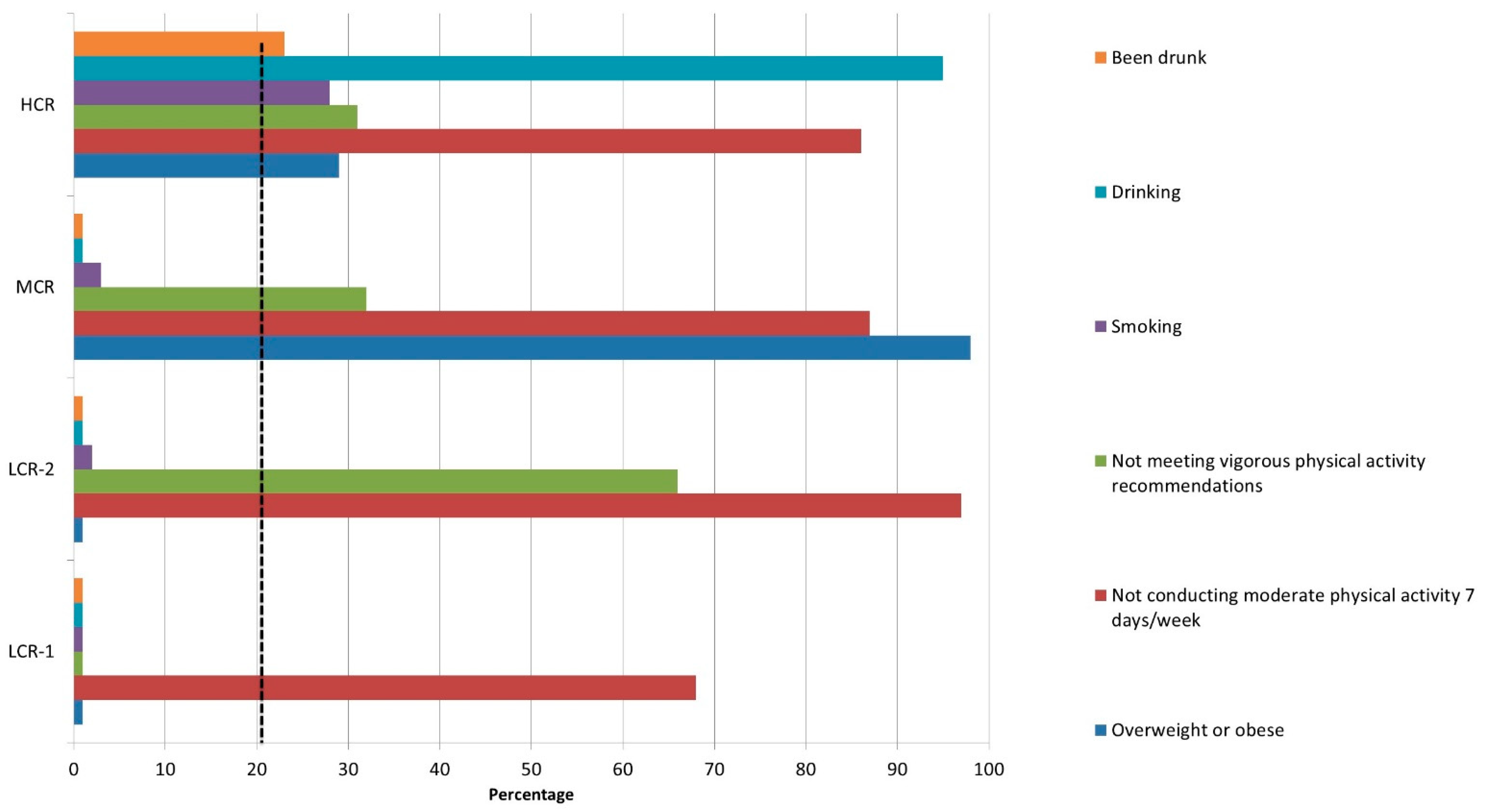
3.3. Cluster Analysis
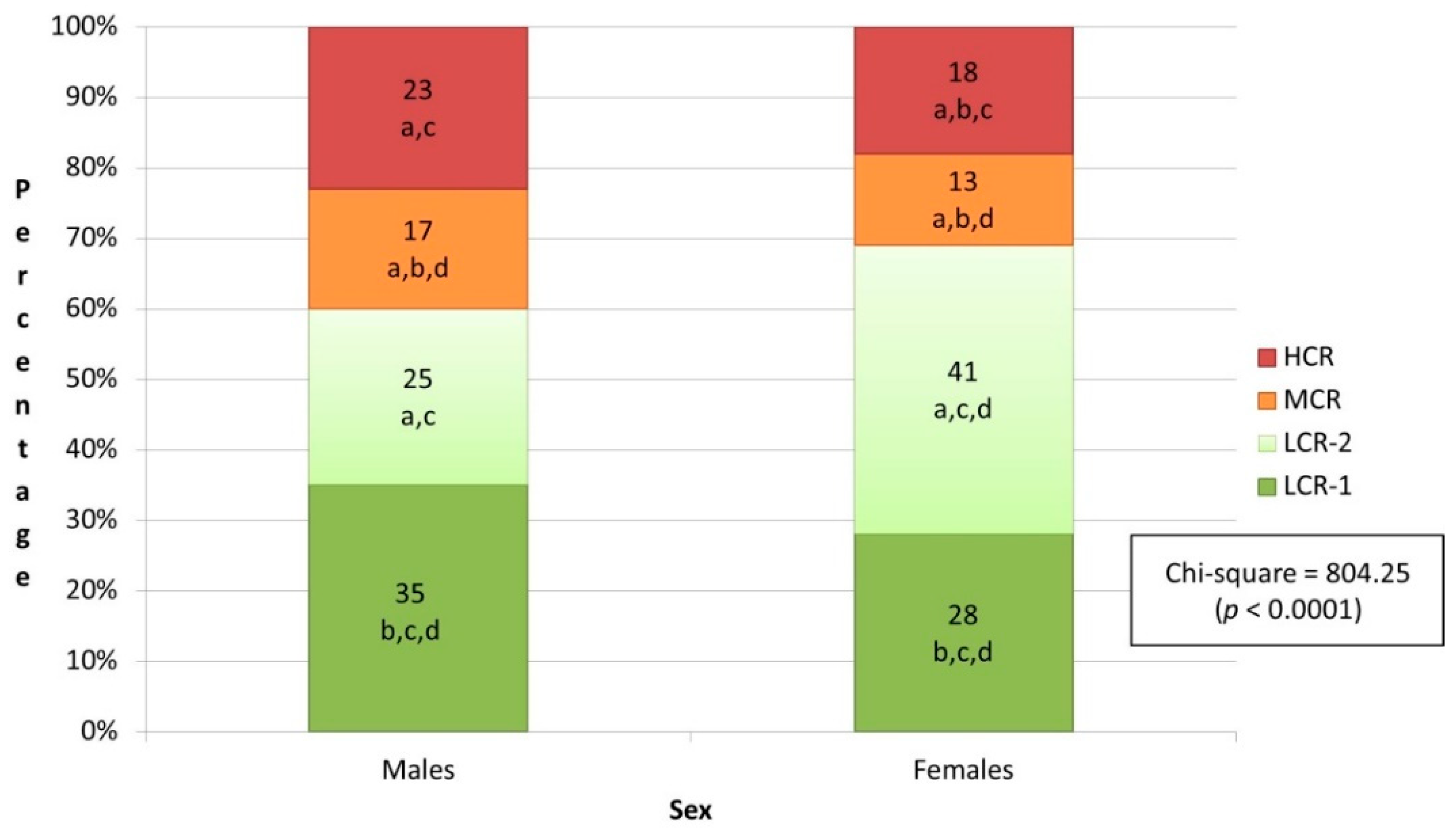
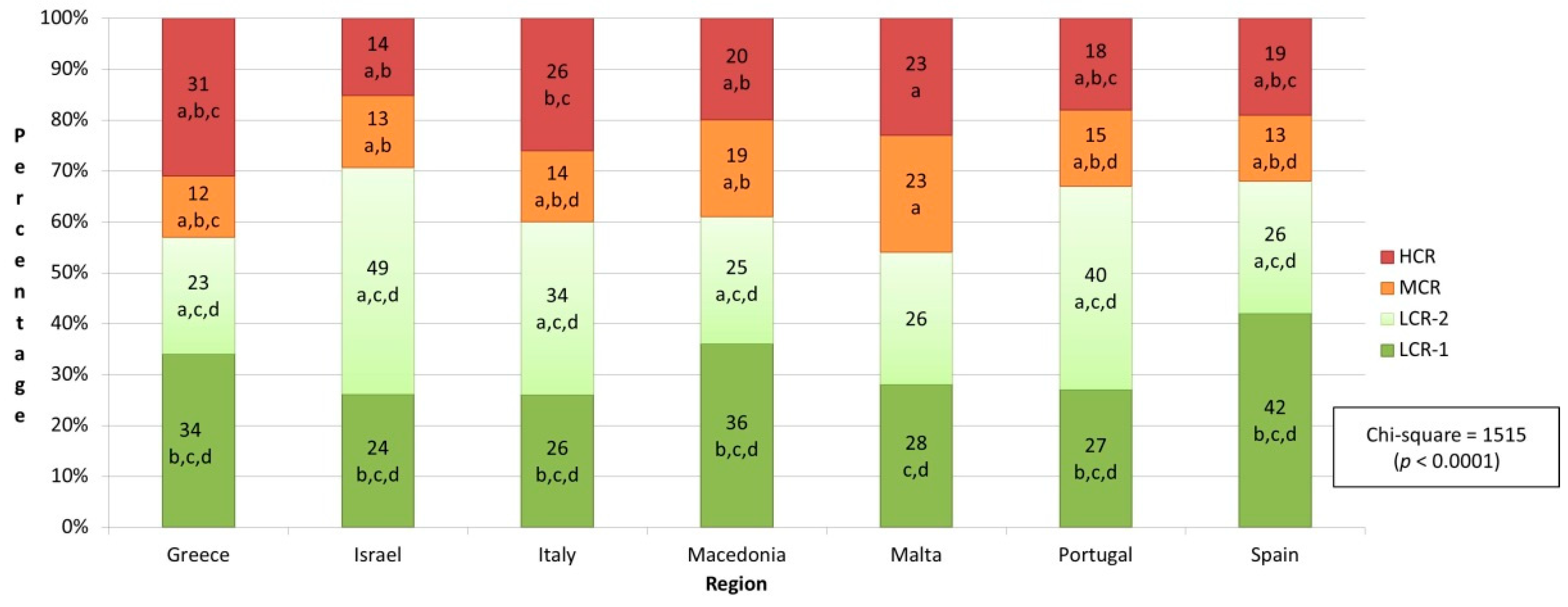
3.4. Sociodemographic Characteristics of the Four Clusters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Olvera Lopez, E.; Ballard, B.D.; Jan, A. Cardiovascular Disease; StatPearls Publishing: Treasure Island, FL, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK535419/ (accessed on 20 December 2021).
- McPhee, P.G.; Singh, S.; Morrison, K.M. Childhood obesity and cardiovascular disease risk: Working towards solutions. Can. J. Cardiol. 2020, 36, 1352–1361. [Google Scholar] [CrossRef] [PubMed]
- Francula-Zaninovic, S.; Nola, I.A. Management of measurable variable cardiovascular disease’ risk factors. Curr. Cardiol. Rev. 2018, 14, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.; Lawes, C.M.; Bennett, D.A.; Milne, R.J.; Rodgers, A. Treatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular risk. Lancet 2005, 365, 434–441. [Google Scholar] [CrossRef]
- World Health Organization. Global Atlas on Cardiovascular Disease Prevention and Control; WHO: Geneva, Switzerland, 2011; Available online: https://www.researchgate.net/publication/272488023_Global_Atlas_on_Cardiovascular_Disease_Prevention_and_Control (accessed on 19 January 2022).
- World Health Organization. Cardiovascular Diseases (CVDs): Key Facts; WHO: Geneva, Switzerland, 2021; Available online: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 19 January 2022).
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef]
- Jagannathan, R.; Patel, S.A.; Ali, M.K.; Narayan, K.V. Global updates on cardiovascular disease mortality trends and attribution of traditional risk factors. Curr. Diabetes Rep. 2019, 19, 44. [Google Scholar] [CrossRef]
- Abidov, A.; Chehab, O. Cardiovascular risk assessment models: Have we found the perfect solution yet? J. Nucl. Cardiol. 2020, 27, 2375–2385. [Google Scholar] [CrossRef]
- Abrignani, M.G.; Luca, F.; Favilli, S.; Benvenuto, M.; Rao, C.M.; di Fusco, S.A.; Gabrielli, D.; Gulizia, M.M.; on behalf Cardiovascular Prevention Area, Young Cardiologists Area, and Paediatric Cardiology Task Force of the Associazione Nazionale Medici Cardiologi Ospedalieri (ANMCO), and Heart Care Foundation. Lifestyles and cardiovascular prevention in childhood and adolescence. Pediatr. Cardiol. 2019, 40, 1113–1125. [Google Scholar] [CrossRef]
- Gourgari, E.; Dabelea, D.; Rother, K. Modifiable risk factors for cardiovascular disease in children with type 1 diabetes: Can early intervention prevent future cardiovascular events? Curr. Diabetes Rep. 2017, 17, 134. [Google Scholar] [CrossRef]
- Brand, C.; Martins, C.M.; Lemes, V.B.; Pessoa, M.L.; Dias, A.F.; Cadore, E.L.; Mota, J.; Gaya, A.C.A.; Gaya, A.R. Effects and prevalence of responders after a multicomponent intervention on cardiometabolic risk factors in children and adolescents with overweight/obesity: Action for health study. J Sports Sci. 2020, 38, 682–691. [Google Scholar] [CrossRef]
- Rodriguez-Artalej, F.; Banegas, B. Cardiovascular epidemiology and prevention. J. Epidemiol. Community Health 2004, 58, 116. [Google Scholar] [CrossRef][Green Version]
- Rippe, J.M. Lifestyle strategies for risk factor reduction, prevention, and treatment of cardiovascular disease. Am. J. Lifestyle Med. 2019, 13, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Guardamagna, O.; Abello, F.; Cagliero, P.; Lughetti, L. Impact of nutrition since early life on cardiovascular prevention. Ital. J. Pediatr. 2012, 38, 73. [Google Scholar] [CrossRef] [PubMed]
- Marques, A.; Demetriou, Y.; Tesler, R.; Gouveia, É.R.; Peralta, M.; de Matos, M.G. Healthy lifestyle in children and adolescents and its association with subjective health complaints: Findings from 37 countries and regions from the HBSC study. Int. J. Environ. Res. 2019, 16, 3292. [Google Scholar] [CrossRef] [PubMed]
- Steinberger, J.; Daniels, S.R.; Hagberg, N. AHA scientific statement. Cardiovascular health promotion in children: Challenges and opportunities for 2020 and beyond. Circulation 2016, 134, e236–e255. [Google Scholar] [CrossRef] [PubMed]
- Celermajer, D.S.; Ayer, J.G.J. Childhood risk factors for adult cardiovascular disease and primary prevention in childhood. Heart 2006, 92, 1701–1706. [Google Scholar] [CrossRef]
- Furtado, J.A.M.; Almeida, S.M.; Mascarenhas, P. Anthropometric features as predictors of atherogenic dyslipidemia and cardiovascular risk in a large population of school-aged children. PLoS ONE 2018, 13, e0197922. [Google Scholar] [CrossRef]
- Jardim, T.V.; Sousa, A.L.; Povoa, T.I.; Barroso, W.K.; Chinem, B.; Jardim, L.; Bernardes, R.; Coca, A.; Jardim, P.C.B.V. The natural history of cardiovascular risk factors in health professionals: 20-year follow-up. BMC Public Health 2015, 15, 1111. [Google Scholar] [CrossRef][Green Version]
- Zaborskis, A.; Grincaitė, M.; Kavaliauskienė, A.; Tesler, R. Family structure and affluence in adolescent eating behaviour: A cross-national study in forty-one countries. Public Health Nutr. 2020, 24, 2521–2532. [Google Scholar] [CrossRef]
- Tur-Sinai, A.; Kolobov, T.; Tesler, R.; Baron-Epel, O.; Dvir, K.; Harel-Fisch, Y. Direct and the indirect determinants of weight-control behaviours among adolescents. Eur. J. Public Health 2019, 29 (Suppl. 4), ckz186-134. [Google Scholar] [CrossRef]
- Ben Yaish, S.; Tesler, R.; Boaz, M.; Harel Fisch, Y.; Kaufman-Shriqui, V. Overestimation of body weight and its association with parental, teacher, and peer support: Evidence from the Israeli Health behaviours in schools survey. Public Health Nutr. 2021, 24, 4035–4042. [Google Scholar] [CrossRef]
- Nadeau, K.J.; Maahs, D.M.; Daniels, S.R.; Eckel, R.H. Childhood obesity and cardiovascular disease: Links and prevention strategies. Nat. Rev. Cardiol. 2011, 8, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Winkleby, M.A.; Kraemer, H.C.; Ahn, D.K.; Varady, A.N. Ethnic and socioeconomic differences in cardiovascular disease risk factors: Findings for women from the Third National Health and Nutrition Examination Survey, 1988–1994. JAMA 1998, 280, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Roger, V.L.; Sidney, S.; Fairchild, A.L.; Howard, V.J.; Labarthe, D.R.; Shay, C.M.; Tiner, C.; Whitsel, L.P.; Rosamund, W.D.; on behalf of the American Heart Association Advocacy Coordinating Committee. Recommendations for cardiovascular health and disease surveillance for 2030 and beyond: A policy statement from the American Heart Association. Circulation 2020, 141, e104–e119. [Google Scholar] [CrossRef] [PubMed]
- Hutchins-Wiese, H.L.; Bales, C.W.; Starr, K.N. Mediterranean diet scoring systems: Understanding the evolution and applications for Mediterranean and non-Mediterranean countries. Br. J. Nutr. 2021, 22. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Reports. Health Behaviour in School-Aged Children: World Health Organization Collaborative Cross-National Survey. Available online: http://www.hbsc.org/publications/international/ (accessed on 30 December 2021).
- Inchley, J.; Currie, D.; Cosma, A.; Samdal, O. Health Behaviour in Schoolaged Children (HBSC) Study Protocol: Background, Methodology and MANDATORY Items for the 2017/18 Survey; HBSC International Coordinating Centre: St. Andrews, UK, 2018. [Google Scholar]
- Roberts, C.; Currie, C.; Samdal, O.; Currie, D.; Smith, R.; Maes, L. Measuring the health and health behaviours of adolescents through cross-national survey research: Recent developments in the health behaviour in school-aged children (HBSC) study. J. Public Health 2007, 15, 179–186. [Google Scholar] [CrossRef]
- Currie, C.; Molcho, M.; Boyce, W.; Holstein, B.; Torsheim, T.; Richter, M. Researching health inequalities in adolescents: The development of the health behaviour in school-aged children (HBSC) family affluence scale. Soc. Sci. Med. 2008, 66, 1429–1436. [Google Scholar] [CrossRef] [PubMed]
- Elgar, F.J.; Gariépy, G.; Torsheim, T.; Currie, C. Early-life income inequality and adolescent health and well-being. Soc. Sci. Med. 2017, 174, 197–208. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2010, 7, 284–294. [Google Scholar] [CrossRef]
- Hutzler, Y.; Tesler, R.; Ng, K.; Barak, S.; Kazula, H.; Harel-Fisch, Y. Physical activity, sedentary screen time and bullying behaviors: Exploring differences between adolescents with and without disabilities. Int. J. Adolesc. Youth 2021, 26, 110–126. [Google Scholar] [CrossRef]
- Walker, M.; Nixon, S.; Haines, J.; McPherson, A.C. Examining risk factors for overweight and obesity in children with disabilities: A commentary on Bronfenbrenner’s ecological systems framework. Dev. Neurorehabil. 2019, 22, 359–364. [Google Scholar] [CrossRef]
- World Health Organization. Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 30 December 2021).
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behavior. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Charrier, L.; Berchialla, P.; Dalmasso, P.; Borraccino, A.; Lemma, P.; Cavallo, F. Cigarette smoking and multiple health risk behaviors: A latent class regression model to identify a profile of young adolescents. Risk Anal. 2019, 39, 1771–1782. [Google Scholar] [CrossRef] [PubMed]
- Pedroni, C.; Dujeu, M.; Lebacq, T.; Desnouck, V.; Holmberg, E.; Castetbon, K. Alcohol consumption in early adolescence: Associations with sociodemographic and psychosocial factors according to gender. PLoS ONE 2021, 16, e0245597. [Google Scholar] [CrossRef] [PubMed]
- Kent, P.; Jensen, R.K.; Kongsted, A. A comparison of three clustering methods for finding subgroups in MRI, SMS or clinical data: SPSS twostep cluster analysis, latent Gold and SNOB. BMC Med. Res. Methodol. 2014, 14, 113. [Google Scholar] [CrossRef]
- Mooi, E.; Sarstedt, M. A Concise Guide to Market Research; Springer: Berlin, Germany, 2011. [Google Scholar]
- Benassi, M.; Garofalo, S.; Ambrosini, F.; Sant’Angelo, R.P.; Raggini, R.; de Paoli, G.; Ravani, C.; Giovagnoli, S.; Orsoni, M.; Piraccini, G. Using two-step cluster analysis and latent class cluster analysis to classify the cognitive heterogeneity of cross-diagnostic psychiatric inpatients. Front. Psychol. 2020, 11, 1085. [Google Scholar] [CrossRef]
- Armstrong, S.; Wong, C.A.; Perrin, E.; Page, S.; Sibley, L.; Skinner, A. Association of physical activity with income, race/ethnicity, and sex among adolescents and young adults in the United States: Findings from the National Health and Nutrition Examination Survey, 2007–2016. JAMA Pediatr. 2018, 172, 732–740. [Google Scholar] [CrossRef]
- Mayorga-Vega, D.; Casado-Robles, C.; López-Fernández, I.; Viciana, J. A comparison of the utility of different step-indices to translate the physical activity recommendation in adolescents. J. Sports Sci. 2021, 39, 469–479. [Google Scholar] [CrossRef]
- Somerset, S.; Hoare, D.J. Barriers to voluntary participation in sport for children: A systematic review. BMC Pediatr. 2018, 18, 47. [Google Scholar] [CrossRef]
- Weatherson, K.A.; McKay, R.; Gainforth, H.L.; Jung, M.E. Barriers and facilitators to the implementation of a school-based physical activity policy in Canada: Application of the theoretical domains framework. BMC Public Health 2017, 17, 835. [Google Scholar] [CrossRef]
- Sallis, J.F.; Bull, F.; Guthold, R.; Heath, G.W.; Inoue, S.; Kelly, P.; Oyeyemi, A.L.; Perez, L.G.; Richards, J.; Hallal, P.C. Lancet physical activity series 2 executive committee. Progress in physical activity over the Olympic quadrennium. Lancet 2016, 388, 1325–1336. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, M.; Tynjälä, J.; Villberg, J.; Lv, Y.; Kannas, L. Socioeconomic differences in adolescents’ smoking: A comparison between Finland and Beijing, China. BMC Public Health 2016, 16, 805. [Google Scholar] [CrossRef] [PubMed]
- Peralta, M.; Henriques-Neto, D.; Gouveia, É.R.; Sardinha, L.B.; Marques, A. Promoting health-related cardiorespiratory fitness in physical education: A systematic review. PLoS ONE 2020, 15, e0237019. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Xi, B.; Li, Z.; Wu, H.; Zhao, M.; Liang, Y.; Bovet, P. Prevalence and trends in tobacco use among adolescents aged 13–15 years in 143 countries, 1999–2018: Findings from the Global Youth Tobacco Surveys. Lancet Child Adolesc. Health 2021, 5, 245–255. [Google Scholar] [CrossRef]
| Variables | Mean (SD) (Range) OR N (%) | |
|---|---|---|
| Age, years: mean (SD) | 13.57 (1.61) (10.5–16.5) | |
| Sex: n (%) | Male | 12,454 (47.69) |
| Female | 13,656 (52.30) | |
| Socioeconomic status (Family Affluence Scale): mean (SD) (range) | 7.96 (2.49) (0.00–17.00) | |
| Country: n (%) | Spain | 3368 (12.89) |
| Greece | 3028 (11.59) | |
| Israel | 6031 (23.09) | |
| Italy | 3237 (12.39) | |
| Macedonia | 3629 (13.89) | |
| Malta | 2010 (7.69) | |
| Portugal | 4807 (18.41) | |
| Variable | Mean (SD) (Range) OR N (%) | ||
|---|---|---|---|
| Weight | Overweight and obese: n (%) | Yes | 5004 (19.16) |
| No | 21,106 (80.83) | ||
| Physical activity habits | 60 min of moderate physical activity/day: mean (SD) (range) | 3.72 (2.13) (0.00–7.00) | |
| Vigorous physical activity 3x week: n (%) | Not meeting recommendations | 7968 (30.51) | |
| Meeting recommendations | 18,142 (69.48) | ||
| Smoking habits | Days smoking in the past 30 days: n (%) | Every day | 432 (1.65) |
| At least once a week but not every day | 430 (1.64) | ||
| Less than once a week | 852 (3.26) | ||
| No smoking | 24,396 (93.43) | ||
| Drinking habits | Drinking alcohol status: n (%) | Regular users | 1907 (7.30) |
| Irregular users | 3186 (12.20) | ||
| Not users | 21,017 (80.49) | ||
| Days drunk in the past 30 days: n (%) | Twice or more | 378 (1.44) | |
| Once | 835 (3.19) | ||
| Never | 24,897 (95.35) | ||
| Variables | Cluster 1 (n = 8115): Mean (SD) (Range) OR N (%) | Cluster 2 (n = 8718): Mean (SD) (Range) OR N (%) | Cluster 3 (n = 3874): Mean (SD) (Range) OR N (%) | Cluster 4 (n = 5403): Mean (SD) (Range) OR N (%) | Chi-Square Test (p-Value) OR ANOVA Test (p-Value) | ||
|---|---|---|---|---|---|---|---|
| Low Cardiovascular Risk—Group 1 | Low Cardiovascular Risk—Group 2 | Moderate Cardiovascular Risk | High Cardiovascular Risk | ||||
| Weight | Overweight and obese: n (%) | Yes | 0 (0) c,d | 0 (0) c,d | 3874 (100) a,b,d | 1513 (28.00) a,b,c | 20,341 (<0.001) |
| No | 8115 (100) c,d | 8718 (100) c,d | 0 (0) a,b,d | 3890 (71.99) a,b,c | |||
| Physical activity | 60 min of moderate physical activity/day: mean (SD) (range) | 5.45 (1.18) b,c,d (4–7) | 2.38 (1.50) a,c,d (0–7) | 3.59 (2.04) a,b,d (0–7) | 3.69 (2.10) a,b,c (0–7) | 5183 (<0.001) | |
| Vigorous physical activity 3/week n (%) | Not meeting recommendations | 0 (0) b,c,d | 5080 (58.27) a,c,d | 1239 (31.98) a,b | 1649 (30.52) a,b | 12.24 (<0.001) | |
| Meeting recommendations | 8115 (100) b,c,d | 3638 (30.21) a,c,d | 2635 (68.01) a,b | 3754 (69.47) a,b | |||
| Smoking habits | Days smoking in the past 30 days: n (%) | Every day | 0 (0) d | 0 (0) d | 24 (0.61) d | 408 (7.55) a,b,c | 4715 (<0.001) |
| At least once a week but not every day | 22 (0.27) d | 29 (0.33) d | 25 (0.64) d | 354 (6.55) a,b,c | |||
| Less than once a week | 12 (0.14) d | 86 (0.98) d | 56 (1.44) d | 698 (12.91) a,b,c | |||
| No smoking | 8081 (99.58) d | 8603 (98.68) d | 3769 (97.28) d | 3943 (72.97) a,b,c | |||
| Drinking habits | Drinking alcohol status: n (%) | Regular users | 0 (0) d | (0) d | 0 (0) d | 1907 (35.29) a,b,c | 4841.29 (<0.001) |
| Irregular users | 0 (0) d | 0 (0) d | 3186 (58.9) a,b,c | ||||
| Not users | 8115 (100) d | 8718 (100) d | 0 (0) d | 310 (5.73) a,b,c | |||
| Days drunk in the past 30 days: n (%) | Twice or more | 0 (0) d | 0 (0) d | 0 (0) d | 378 (6.99) a,b,c | 1532.45 (<0.001) | |
| Once | 0 (0) d | 0 (0) d | 0 (0) d | 835 (15.45) a,b,c | |||
| Never | 8115 (100) d | 8718 (100) d | 3874 (100) d | 4190 (77.54) a,b,c | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tesler, R.; Barak, S.; Reges, O.; Moreno-Maldonado, C.; Maor, R.; Gaspar, T.; Ercan, O.; Sela, Y.; Green, G.; Zigdon, A.; et al. Identifying Cardiovascular Risk Profiles Clusters among Mediterranean Adolescents across Seven Countries. Healthcare 2022, 10, 268. https://doi.org/10.3390/healthcare10020268
Tesler R, Barak S, Reges O, Moreno-Maldonado C, Maor R, Gaspar T, Ercan O, Sela Y, Green G, Zigdon A, et al. Identifying Cardiovascular Risk Profiles Clusters among Mediterranean Adolescents across Seven Countries. Healthcare. 2022; 10(2):268. https://doi.org/10.3390/healthcare10020268
Chicago/Turabian StyleTesler, Riki, Sharon Barak, Orna Reges, Concepción Moreno-Maldonado, Rotem Maor, Tânia Gaspar, Oya Ercan, Yael Sela, Gizell Green, Avi Zigdon, and et al. 2022. "Identifying Cardiovascular Risk Profiles Clusters among Mediterranean Adolescents across Seven Countries" Healthcare 10, no. 2: 268. https://doi.org/10.3390/healthcare10020268
APA StyleTesler, R., Barak, S., Reges, O., Moreno-Maldonado, C., Maor, R., Gaspar, T., Ercan, O., Sela, Y., Green, G., Zigdon, A., Marques, A., Ng, K., & Harel-Fisch, Y. (2022). Identifying Cardiovascular Risk Profiles Clusters among Mediterranean Adolescents across Seven Countries. Healthcare, 10(2), 268. https://doi.org/10.3390/healthcare10020268









