A Survey on Treatment Status of Korean Medicine Doctors for the Behavioral and Psychological Symptoms of Dementia: Preliminary Data for Guidance of Integrative Care
Abstract
:1. Introduction
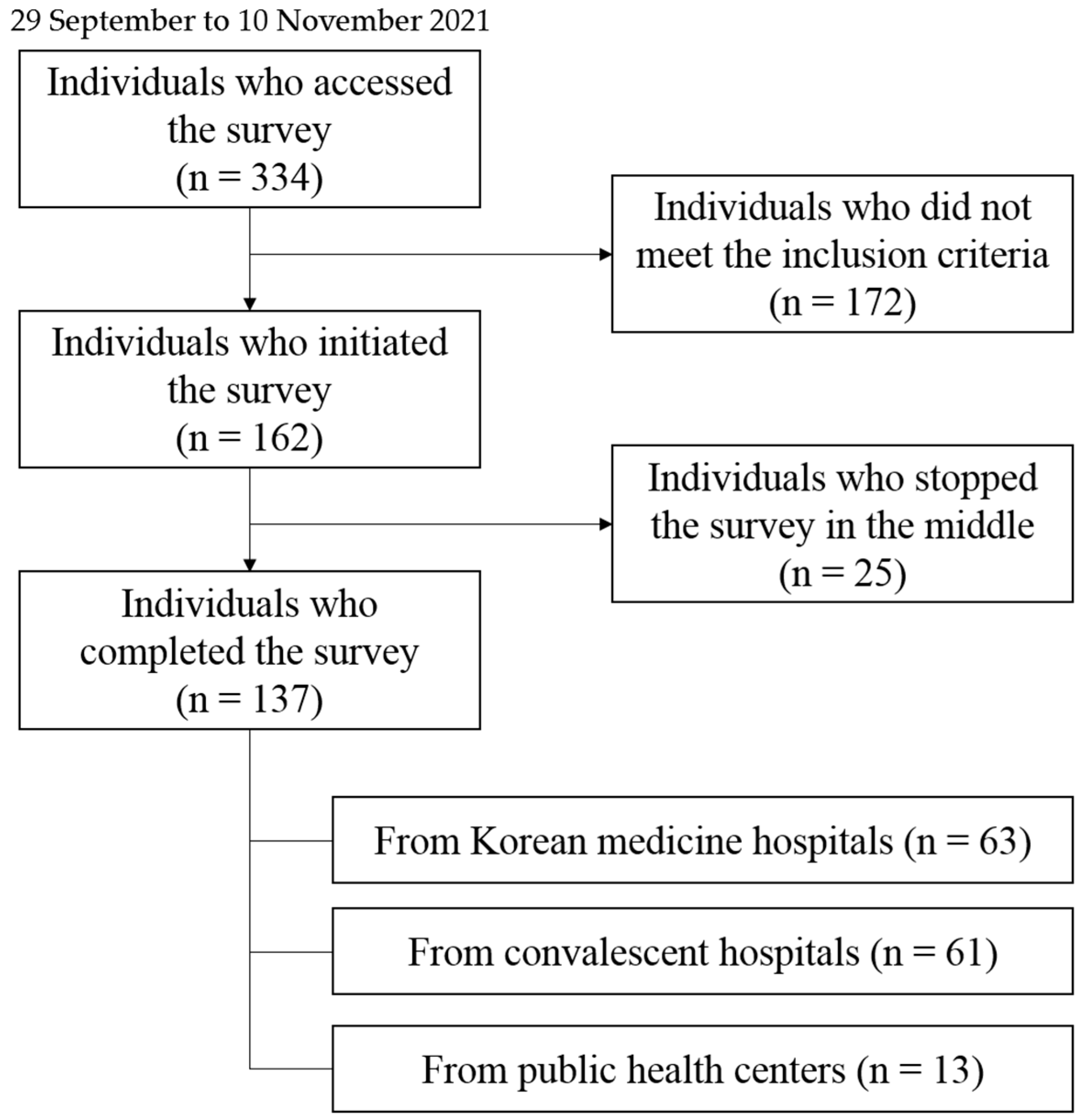
2. Materials and Methods
2.1. Participants
2.2. Questionnaire Construction
2.3. Distribution and Collection of Questionnaires
2.4. Data Entry
2.5. Statistical Analysis
2.6. Ethical Consideration
3. Results
3.1. Participants’ Characteristics
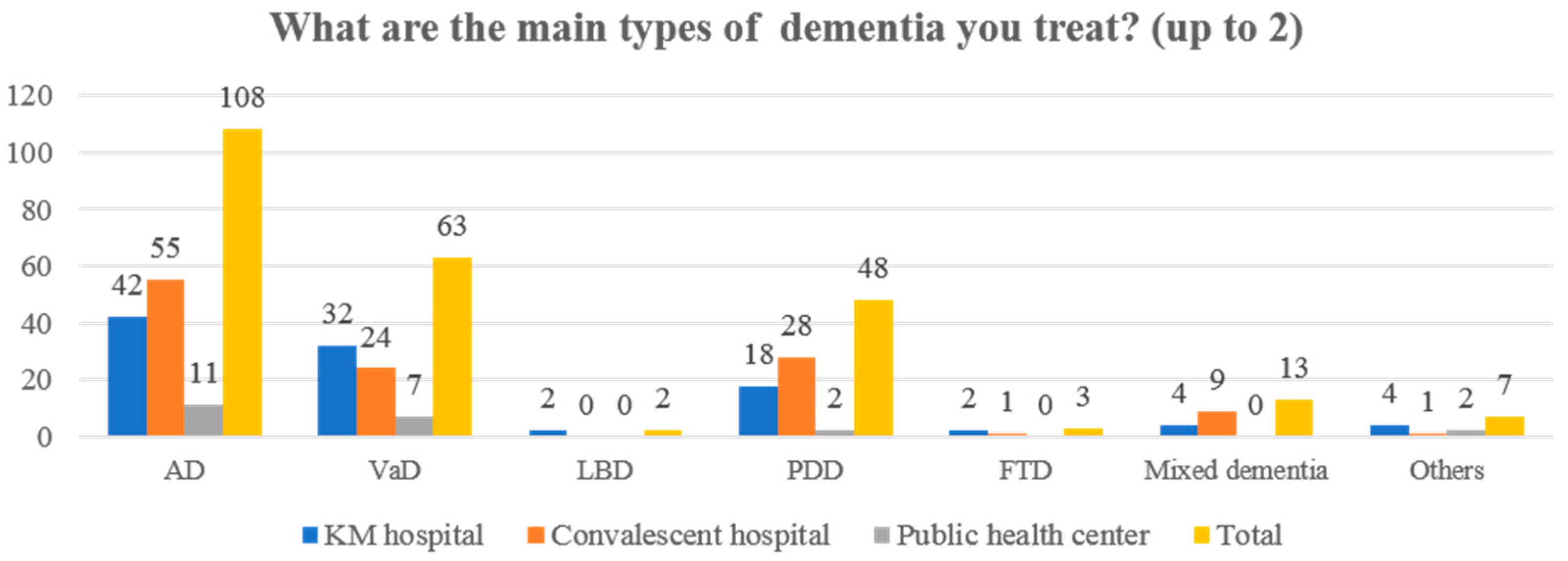
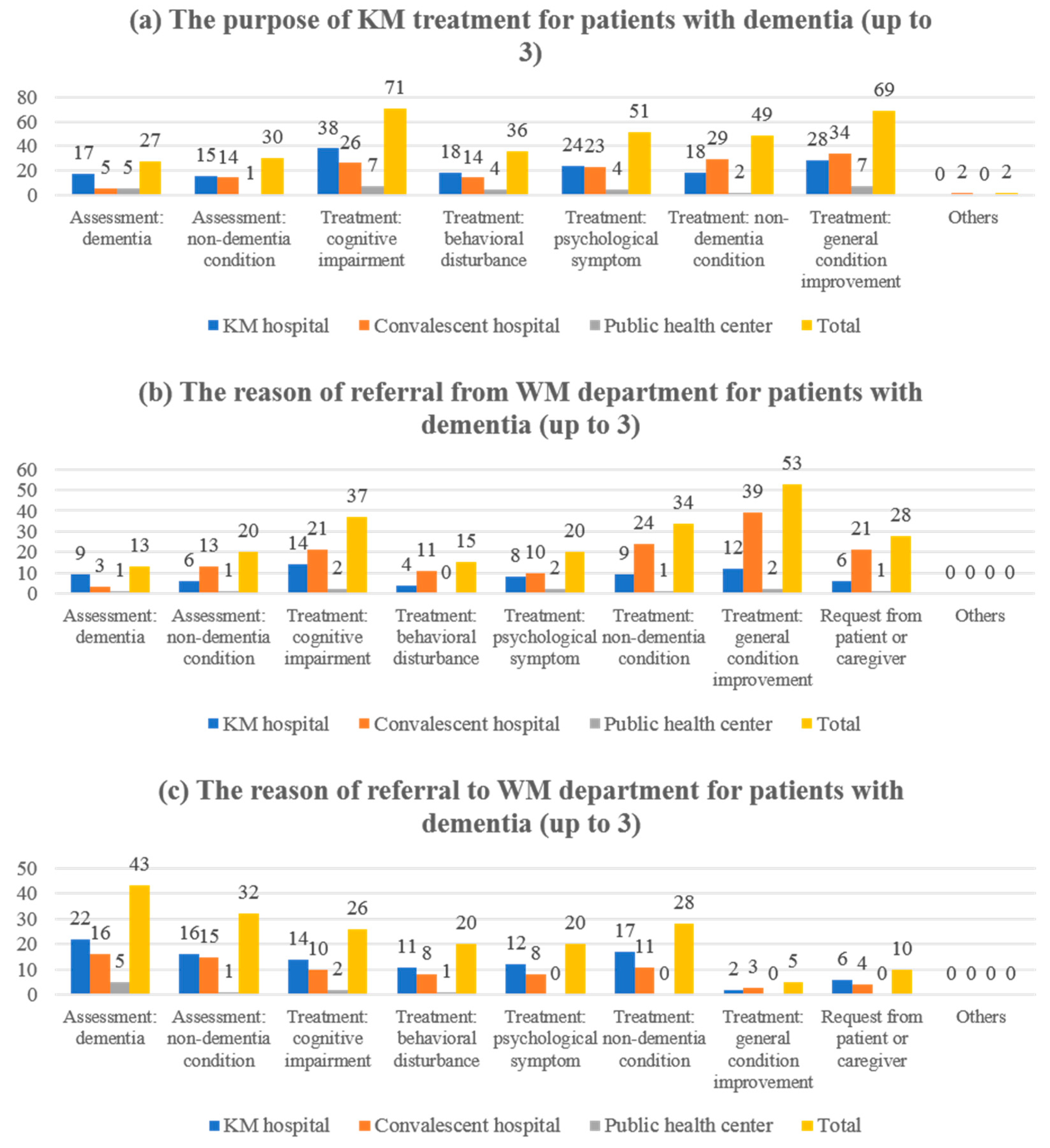
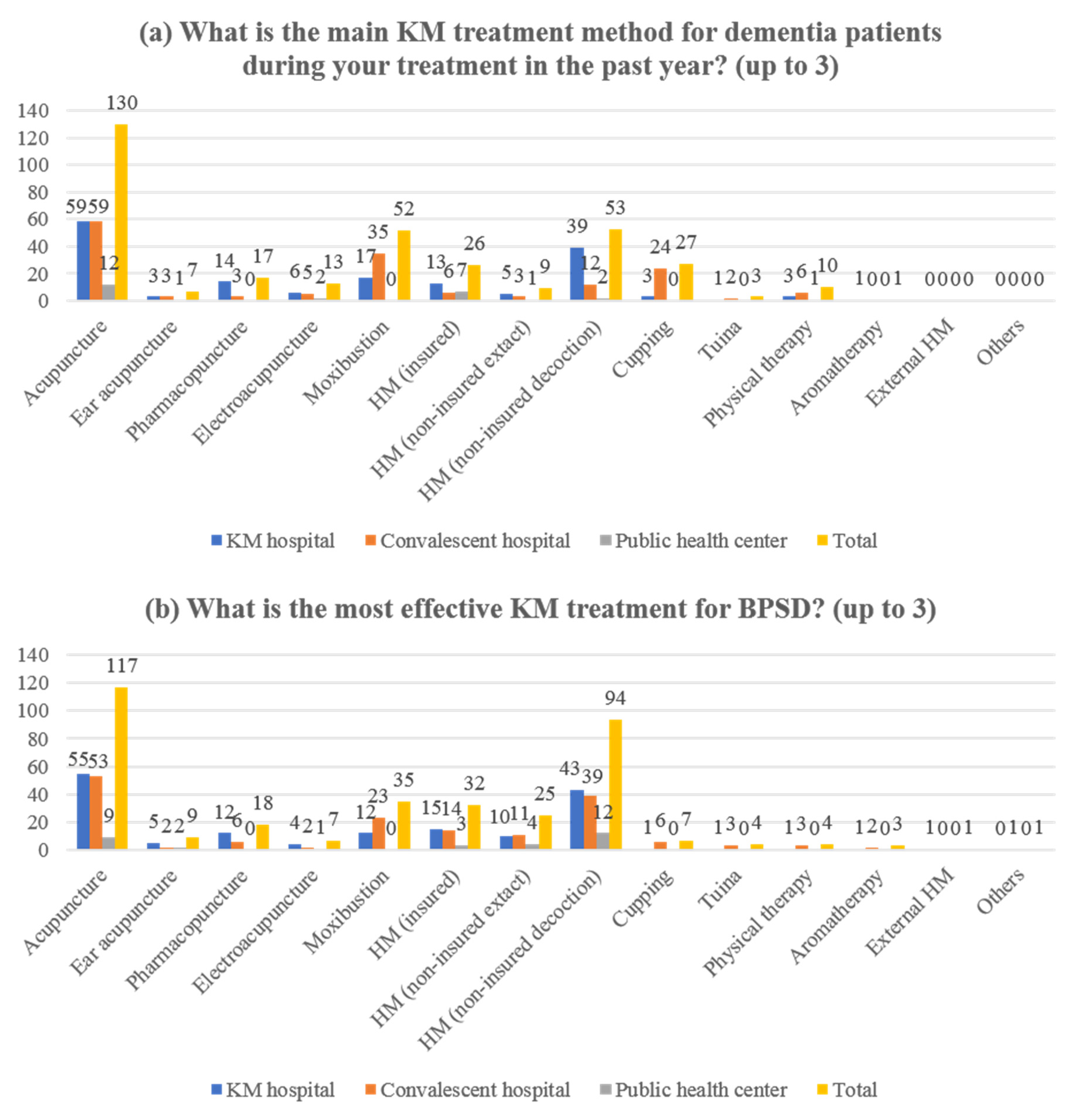
3.2. The Current Status and Experience of Integrative Treatment for Dementia Patients
3.3. The Perception of BPSD Management
3.4. The Knowledge of BPSD Management
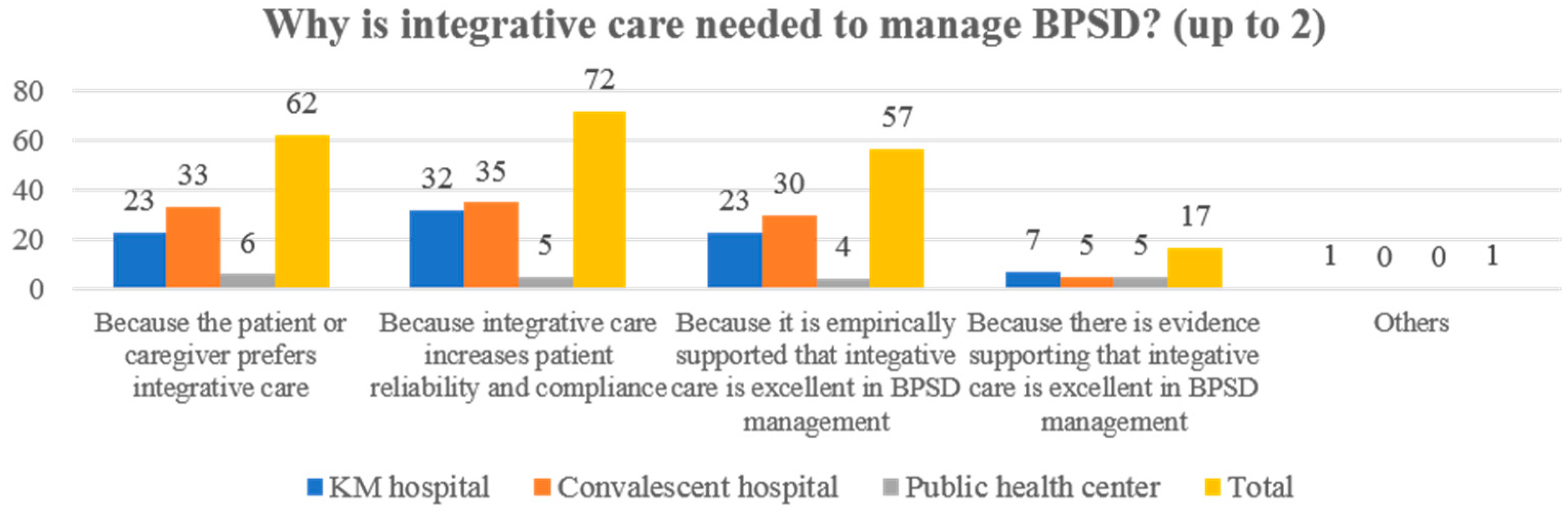
3.5. Perceptions and Needs of Manuals to Promote Integrative Care on BPSD
4. Discussion
4.1. Main Findings of the Survey
4.2. Clinical Interpretation
4.3. Results of Previous Studies
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patterson, C. World Alzheimer Report 2018; Alzheimer’s Disease International Location: London, UK, 2018. [Google Scholar]
- Schaller, S.; Mauskopf, J.; Kriza, C.; Wahlster, P.; Kolominsky-Rabas, P.L. The main cost drivers in dementia: A systematic review. Int. J. Geriatr. Psychiatry 2015, 30, 111–129. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Zucchella, C.; Sinforiani, E.; Tamburin, S.; Federico, A.; Mantovani, E.; Bernini, S.; Casale, R.; Bartolo, M. The multidisciplinary approach to Alzheimer’s disease and dementia. A narrative review of non-pharmacological treatment. Front. Neurol. 2018, 9, 1058. [Google Scholar] [CrossRef] [PubMed]
- Fisher, T.J.; Schwartz, A.C.; Greenspan, H.N.; Heinrich, T.W. Dementia: A complex disease with multiple etiologies and multiple treatments. Int. J. Psychiatry Med. 2016, 51, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Feast, A.; Orrell, M.; Charlesworth, G.; Melunsky, N.; Poland, F.; Moniz-Cook, E. Behavioural and psychological symptoms in dementia and the challenges for family carers: Systematic review. Br. J. Psychiatry J. Ment. Sci. 2016, 208, 429–434. [Google Scholar] [CrossRef] [Green Version]
- Kwon, C.Y.; Lee, B. Prevalence of behavioral and psychological symptoms of dementia in community-dwelling dementia patients: A systematic review. Front. Psychiatry 2021, 12, 741059. [Google Scholar] [CrossRef]
- Tible, O.P.; Riese, F.; Savaskan, E.; von Gunten, A. Best practice in the management of behavioural and psychological symptoms of dementia. Ther. Adv. Neurol. Disord. 2017, 10, 297–309. [Google Scholar] [CrossRef]
- Cotta Ramusino, M.; Perini, G.; Vaghi, G.; dal Fabbro, B.; Capelli, M.; Picascia, M.; Franciotta, D.; Farina, L.; Ballante, E.; Costa, A. Correlation of frontal atrophy and CSF tau levels with neuropsychiatric symptoms in patients with cognitive impairment: A Memory clinic experience. Front. Aging Neurosci. 2021, 13, 595758. [Google Scholar] [CrossRef]
- Azermai, M.; Petrovic, M.; Elseviers, M.M.; Bourgeois, J.; van Bortel, L.M.; vander Stichele, R.H. Systematic appraisal of dementia guidelines for the management of behavioural and psychological symptoms. Ageing Res. Rev. 2012, 11, 78–86. [Google Scholar] [CrossRef]
- Sorbi, S.; Hort, J.; Erkinjuntti, T.; Fladby, T.; Gainotti, G.; Gurvit, H.; Nacmias, B.; Pasquier, F.; Popescu, B.O.; Rektorova, I.; et al. EFNS-ENS Guidelines on the diagnosis and management of disorders associated with dementia. Eur. J. Neurol. 2012, 19, 1159–1179. [Google Scholar] [CrossRef]
- Dyer, S.M.; Harrison, S.L.; Laver, K.; Whitehead, C.; Crotty, M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int. Psychogeriatr. 2018, 30, 295–309. [Google Scholar] [CrossRef] [PubMed]
- Tampi, R.R.; Tampi, D.J.; Balachandran, S.; Srinivasan, S. Antipsychotic use in dementia: A systematic review of benefits and risks from meta-analyses. Ther. Adv. Chronic Dis. 2016, 7, 229–245. [Google Scholar] [CrossRef] [PubMed]
- Gallini, A.; Andrieu, S.; Donohue, J.M.; Oumouhou, N.; Lapeyre-Mestre, M.; Gardette, V. Trends in use of antipsychotics in elderly patients with dementia: Impact of national safety warnings. Eur. Neuropsychopharmacol. 2014, 24, 95–104. [Google Scholar] [CrossRef] [Green Version]
- Rees, L.; Weil, A. Integrated medicine. BMJ 2001, 322, 119–120. [Google Scholar] [CrossRef] [PubMed]
- Sierpina, V.S.; Sierpina, M.; Loera, J.A.; Grumbles, L. Complementary and integrative approaches to dementia. South. Med. J. 2005, 98, 636–645. [Google Scholar] [CrossRef]
- Teut, M.; Bloedt, S.; Baur, R.; Betsch, F.; Elies, M.; Fruehwald, M.; Fuesgen, I.; Kerckhoff, A.; Krüger, E.; Schimpf, D.; et al. Dementia: Treating patients and caregivers with complementary and alternative medicine—Results of a clinical expert conference using the World Café method. Forsch. Komplement. 2013, 20, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Wells, R.E.; Baute, V.; Wahbeh, H. Complementary and integrative medicine for neurologic conditions. Med. Clin. 2017, 101, 881–893. [Google Scholar] [CrossRef]
- Kim, D.; Shih, C.C.; Cheng, H.C.; Kwon, S.H.; Kim, H.; Lim, B. A comparative study of the traditional medicine systems of South Korea and Taiwan: Focus on administration, education and license. Integr. Med. Res. 2021, 10, 100685. [Google Scholar] [CrossRef]
- Seo, Y.; You, D.; Kim, H.; Kim, S.; Lee, G.; Kim, S.; Kang, H.; Jung, I. A survey of the recognition on the practice pattern, diagnosis, and treatment of korean medicine of dementia and mild cognitive impairment—Focusing on the differences between neuropsychiatrists of korean medicine and general physicians. J. Orient. Neuropsychiatry 2017, 28, 263–274. [Google Scholar] [CrossRef]
- Kang, T.; Lee, S. A study on the position and role of Korean medicine doctors working at long-term care hospitals. J. Soc. Prev. Korean Med. 2015, 19, 77–90. [Google Scholar]
- Birch, S. Treating the patient not the symptoms: Acupuncture to improve overall health—Evidence, acceptance and strategies. Integr. Med. Res. 2019, 8, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Cheung, C.K.; Wyman, J.F.; Halcon, L.L. Use of complementary and alternative therapies in community-dwelling older adults. J. Altern. Complement. Med. 2007, 13, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, K.; Binting, S.; Witt, C.M.; Teut, M. Use of complementary and alternative medicine by older adults—A cross-sectional survey. BMC Geriatr. 2014, 14, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wells, R.E.; Phillips, R.S.; Schachter, S.C.; McCarthy, E.P. Complementary and alternative medicine use among US adults with common neurological conditions. J. Neurol. 2010, 257, 1822–1831. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steiner, G.Z.; George, E.S.; Metri, N.J.; MacMillan, F.; Dubois, S.; Moyle, W.; Hohenberg, M.I.; Singh, K.; Townsend, C.; Chang, D.; et al. Use of complementary medicines and lifestyle approaches by people living with dementia: Exploring experiences, motivations and attitudes. Int. J. Older People Nurs. 2021, 16, e12378. [Google Scholar] [CrossRef] [PubMed]
- Stöckigt, B.; Teut, M.; Witt, C.M. CAM use and suggestions for medical care of senior citizens: A qualitative study using the World Café Method. Evid. Based Complement. Alternat. Med. 2013, 2013, 951245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korean Statistical Information Service. Statistical Database. 2011. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=354&tblId=DT_HIRA44&conn_path=I2 (accessed on 18 January 2022).
- Fugh-Berman, A. Herb-drug interactions. Lancet 2000, 355, 134–138. [Google Scholar] [CrossRef]
| Classification | KM Hospital (n = 63) (n (%)) | Convalescent Hospital (n = 61) (n (%)) | Public Health Center (n = 13) (n (%)) | Total (n = 137) (n (%)) |
|---|---|---|---|---|
| Sex | ||||
| Male | 40 (63.49%) | 42 (68.85%) | 12 (92.31%) | 94 (68.61%) |
| Female | 23 (36.51%) | 19 (31.15%) | 1 (7.69%) | 43 (31.39%) |
| Age (years) ¶ | ||||
| <30 | 9 (14.29%) | 2 (3.28%) | 6 (46.15%) | 17 (12.41%) |
| ≥30 to <40 | 30 (47.62%) | 22 (36.07%) | 7 (53.85%) | 59 (43.07%) |
| ≥40 to <49 | 14 (22.22%) | 24 (39.34%) | 0 (0%) | 38 (27.74%) |
| ≥50 to <59 | 10 (15.87%) | 11 (18.03%) | 0 (0%) | 21 (15.33%) |
| ≥60 | 0 (0%) | 2 (3.28%) | 0 (0%) | 2 (1.46%) |
| Clinical experience (years) ¶ | ||||
| <5 | 10 (15.87%) | 5 (8.20%) | 6 (46.15%) | 21 (15.33%) |
| ≥ 5 to <10 | 20 (31.75%) | 17 (27.87%) | 7 (53.85%) | 44 (32.12%) |
| ≥10 to <15 | 13 (20.63%) | 11 (18.03%) | 0 (0%) | 24 (17.52%) |
| ≥15 to <20 | 7 (11.11%) | 14 (22.95%) | 0 (0%) | 21 (15.33%) |
| ≥20 to <30 | 9 (14.29%) | 6 (9.84%) | 0 (0%) | 15 (10.95%) |
| ≥30 | 4 (6.35%) | 8 (13.11%) | 0 (0%) | 12 (8.76%) |
| Type of KM doctor license ¶ | ||||
| Specialist | 35 (55.56%) | 12 (19.67%) | 4 (30.77%) | 51 (37.23%) |
| General practitioner | 28 (44.44%) | 49 (80.33%) | 9 (69.23%) | 86 (62.77%) |
| Classification | KM Hospital (n = 63) (n (%)) | Convalescent Hospital (n = 61) (n (%)) | Public Health Center (n = 13) (n (%)) | Total (n = 137) (n (%)) |
|---|---|---|---|---|
| Average treatment cost (out-of-pocket) per treatment (KRW) ¶ | ||||
| <5000 | 5 (7.94%) | 27 (44.26%) | 7 (53.85%) | 39 (28.47%) |
| ≥5000 to <10,000 | 12 (19.05%) | 10 (16.39%) | 5 (38.46%) | 27 (19.71%) |
| ≥10,000 to <20,000 | 27 (42.86%) | 16 (26.23%) | 1 (7.69%) | 44 (32.12%) |
| ≥20,000 to <50,000 | 15 (23.81%) | 8 (13.11%) | 0 (0%) | 23 (16.79%) |
| ≥50,000 to <100,000 | 3 (4.76%) | 0 (0%) | 0 (0%) | 3 (2.19%) |
| ≥100,000 | 1 (1.59%) | 0 (0%) | 0 (0%) | 1 (0.73%) |
| Classification Likert Scale (1 (Strongly Disagree (or Very Little) to 5 Strongly Agree (or Very Much)) | KM Hospital (n = 63) (Mean ± SD) | Convalescent Hospital (n = 61) (Mean ± SD) | Public Health Center (n = 13) (Mean ± SD) | Total (n = 137) (Mean ± SD) |
|---|---|---|---|---|
| Perceptions (advocacy) of effectiveness | ||||
| WM treatments for BPSD | 3.51 ± 0.77 | 3.54 ± 0.64 | 3.54 ± 1.08 | 3.53 ± 0.76 |
| KM treatments for BPSD | 3.78 ± 0.68 | 3.70 ± 0.66 | 4.31 ± 0.61 | 3.80 ± 0.68 |
| Integrative care for BPSD | 3.92 ± 0.72 | 3.95 ± 0.73 | 4.38 ± 0.62 | 3.98 ± 0.73 |
| Perceptions (advocacy) of safety | ||||
| WM treatments for BPSD | 3.41 ± 0.85 | 3.26 ± 0.74 | 3 ± 1.11 | 3.31 ± 0.84 |
| KM treatments for BPSD | 4.05 ± 0.79 | 4.08 ± 0.63 | 4.46 ± 0.63 | 4.10 ± 0.72 |
| Integrative care for BPSD ¶ | 3.94 ± 0.66 | 3.97 ± 0.68 | 4.08 ± 0.92 | 3.96 ± 0.70 |
| Knowledge of BPSD | ||||
| Definition of BPSD | 3.33 ± 0.93 | 3.08 ± 0.66 | 3.69 ± 0.72 | 3.26 ± 0.82 |
| Assessment method of BPSD ¶ | 3.21 ± 0.86 | 2.85 ± 0.72 | 3.85 ± 0.66 | 3.12 ± 0.83 |
| Differences in BPSD by type of dementia | 3.08 ± 0.88 | 2.72 ± 0.83 | 3.31 ± 0.72 | 2.94 ± 0.87 |
| Differences in BPSD by severity of dementia | 3.10 ± 0.79 | 2.87 ± 0.82 | 3.54 ± 0.93 | 3.04 ± 0.84 |
| Effectiveness of WM treatment on BPSD | 3.22 ± 0.86 | 2.98 ± 0.74 | 3.46 ± 0.75 | 3.14 ± 0.81 |
| Effectiveness of KM treatment on BPSD | 3.54 ± 0.83 | 3.33 ± 0.62 | 3.85 ± 0.86 | 3.47 ± 0.76 |
| Effectiveness of integrative care on BPSD | 3.37 ± 0.74 | 3.38 ± 0.68 | 3.69 ± 0.72 | 3.40 ± 0.72 |
| Safety of WM treatment on BPSD | 3.13 ± 0.83 | 2.87 ± 0.64 | 3.46 ± 0.84 | 3.04 ± 0.77 |
| Safety of KM treatment on BPSD | 3.63 ± 0.84 | 3.48 ± 0.64 | 3.92 ± 0.73 | 3.59 ± 0.76 |
| Safety of integrative care on BPSD | 3.38 ± 0.76 | 3.38 ± 0.68 | 3.62 ± 0.84 | 3.40 ± 0.74 |
| Knowledge of BPSD (non-KMD personnel) | ||||
| Effectiveness of KM treatment on BPSD | 2.81 ± 0.99 | 2.72 ± 0.94 | 3.15 ± 1.17 | 2.80 ± 1.00 |
| Effectiveness of integrative care on BPSD | 2.79 ± 0.99 | 2.75 ± 0.90 | 2.85 ± 1.23 | 2.78 ± 0.98 |
| Safety of KM treatment on BPSD | 2.92 ± 1.07 | 2.77 ± 0.95 | 3.15 ± 1.23 | 2.88 ± 1.04 |
| Safety of integrative care on BPSD | 2.84 ± 1.04 | 2.82 ± 0.97 | 2.85 ± 1.17 | 2.83 ± 1.02 |
| Classification Likert Scale 1 (Strongly Disagree to 5 Strongly Agree) | KM Hospital (n = 58) (Mean ± SD) | Convalescent Hospital (n = 59) (Mean ± SD) | Public Health Center (n = 11) (Mean ± SD) | Total (n = 128) (Mean ± SD) |
|---|---|---|---|---|
| Knowledge of BPSD (definition, types, and assessment) | 4.17 ± 0.56 | 4.02 ± 0.75 | 4 ± 0.60 | 4.09 ± 0.66 |
| Evidence of WM treatment on BPSD | 4.07 ± 0.72 | 3.83 ± 0.74 | 3.91 ± 0.51 | 3.95 ± 0.72 |
| Evidence of KM treatment on BPSD | 4.24 ± 0.62 | 4.10 ± 0.80 | 4.36 ± 0.88 | 4.19 ± 0.74 |
| Evidence of integrative care on BPSD | 4.12 ± 0.65 | 4.02 ± 0.70 | 4.27 ± 0.75 | 4.09 ± 0.68 |
| Criteria for KM treatment referral | 4.03 ± 0.81 | 3.92 ± 0.74 | 4.36 ± 0.77 | 4.01 ± 0.79 |
| Standardized referral form for KM treatment | 3.98 ± 0.71 | 3.85 ± 0.75 | 4.18 ± 0.83 | 3.94 ± 0.75 |
| Standardized reply form of KM treatment | 3.98 ± 0.67 | 3.98 ± 0.72 | 4.18 ± 0.83 | 4.01 ± 0.71 |
| Scenario of integrative medicine for BPSD | 4.10 ± 0.69 | 4.10 ± 0.72 | 3.73 ± 0.86 | 4.03 ± 0.73 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, C.-Y.; Lee, B. A Survey on Treatment Status of Korean Medicine Doctors for the Behavioral and Psychological Symptoms of Dementia: Preliminary Data for Guidance of Integrative Care. Healthcare 2022, 10, 269. https://doi.org/10.3390/healthcare10020269
Kwon C-Y, Lee B. A Survey on Treatment Status of Korean Medicine Doctors for the Behavioral and Psychological Symptoms of Dementia: Preliminary Data for Guidance of Integrative Care. Healthcare. 2022; 10(2):269. https://doi.org/10.3390/healthcare10020269
Chicago/Turabian StyleKwon, Chan-Young, and Boram Lee. 2022. "A Survey on Treatment Status of Korean Medicine Doctors for the Behavioral and Psychological Symptoms of Dementia: Preliminary Data for Guidance of Integrative Care" Healthcare 10, no. 2: 269. https://doi.org/10.3390/healthcare10020269
APA StyleKwon, C.-Y., & Lee, B. (2022). A Survey on Treatment Status of Korean Medicine Doctors for the Behavioral and Psychological Symptoms of Dementia: Preliminary Data for Guidance of Integrative Care. Healthcare, 10(2), 269. https://doi.org/10.3390/healthcare10020269







