Use of the Ultrasound Technique as Compared to the Standard Technique for the Improvement of Venous Cannulation in Patients with Difficult Access
Abstract
1. Introduction
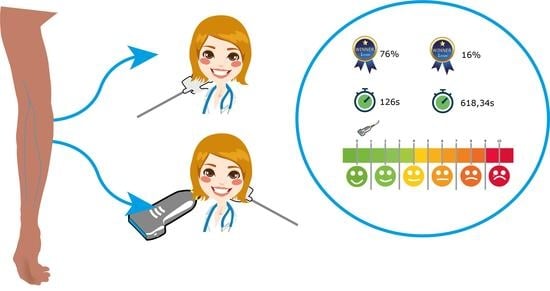
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Variables
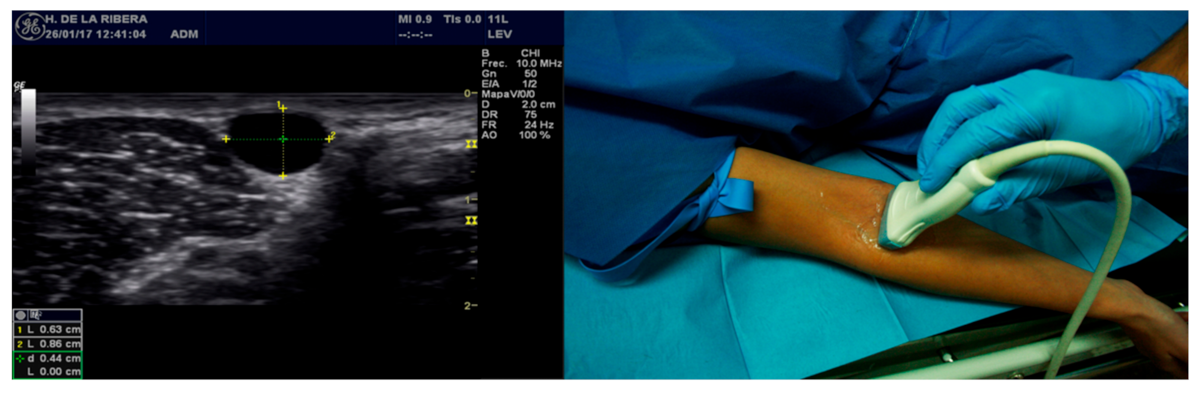
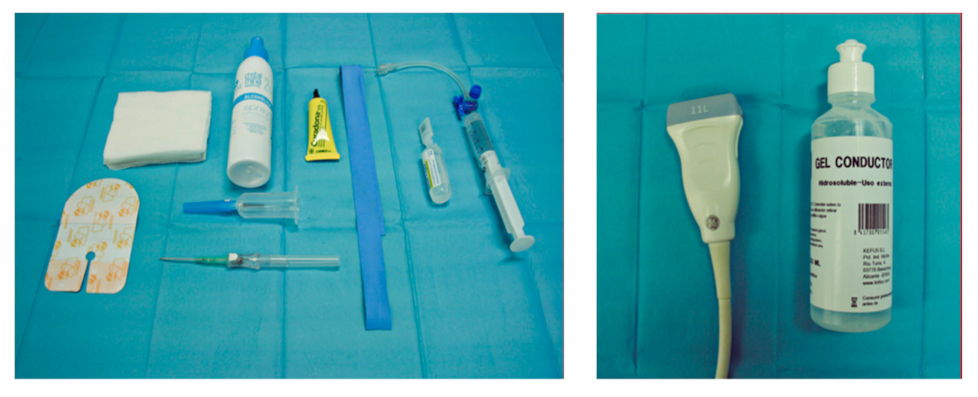
2.3. Equipment
2.4. Sample Calculation and Type of Sampling
2.5. Target Population and Study Population
2.6. Analysis Strategy
2.7. Ethical Aspects
3. Results
3.1. Sociodemographic and Clinical Characteristics
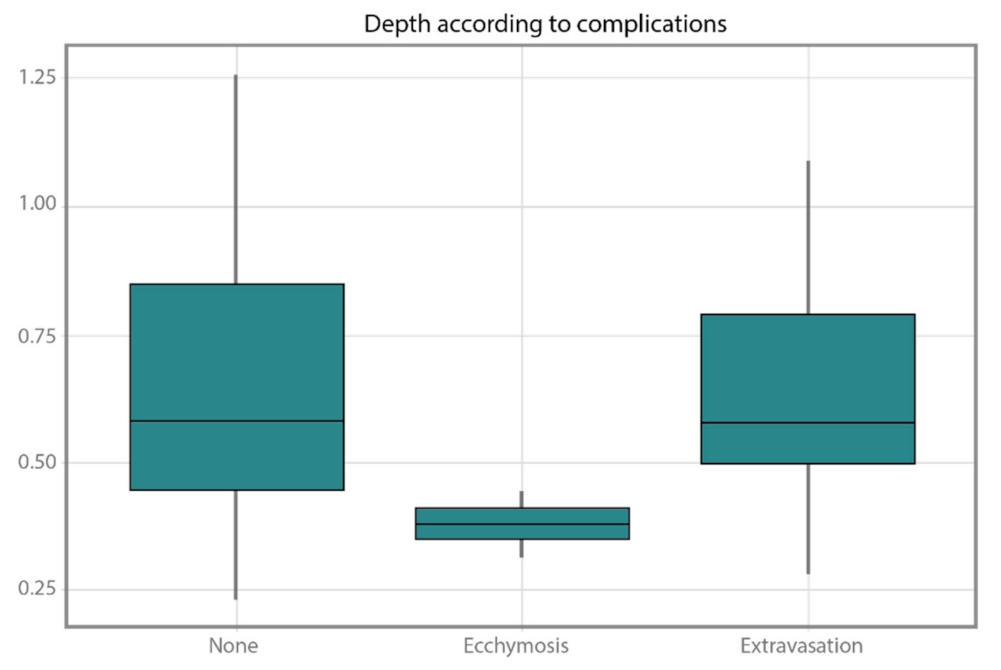
3.2. Variables of Interest
3.3. Ultrasound Technique Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Alexandrou, E.; Ray-Barruel, G.; Carr, P.J.; Frost, S.A.; Inwood, S.; Higgins, N.; Lin, F.; Alberto, L.; Mermel, L.; Rickard, C.; et al. Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes Worldwide. J. Hosp. Med. 2018, 13, E1–E7. Available online: https://pubmed.ncbi.nlm.nih.gov/29813140/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Fields, J.M.; Piela, N.E.; Au, A.K.; Ku, B.S. Risk factors associated with difficult venous access in adult ED patients. Am. J. Emerg. Med. 2014, 32, 1179–1182. Available online: https://pubmed.ncbi.nlm.nih.gov/25171796/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Jacobson, A.F.; Winslow, E.H. Variables influencing intravenous catheter insertion difficulty and failure: An analysis of 339 intravenous catheter insertions. Heart Lung J. Crit. Care 2005, 34, 345–359. Available online: https://pubmed.ncbi.nlm.nih.gov/16157191/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Presley, B.; Isenberg, J.D. Ultrasound Guided Intravenous Access; StatPearls: Treasure Island, FL, USA, 2021; Available online: https://pubmed.ncbi.nlm.nih.gov/30252244/ (accessed on 3 December 2021).
- Costantino, T.G.; Kirtz, J.F.; Satz, W.A. Ultrasound-Guided Peripheral Venous Access vs. the External Jugular Vein as the Initial Approach to the Patient with Difficult Vascular Access. J. Emerg. Med. 2010, 39, 462–467. Available online: https://pubmed.ncbi.nlm.nih.gov/19303238/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Van Loon, F.H.J.; Puijn, L.A.P.M.; Houterman, S.; Bouwman, A.R.A. Development of the A-DIVA Scale: A Clinical Predictive Scale to Identify Difficult Intravenous Access in Adult Patients Based on Clinical Observations. Medicine 2016, 95, e3428. [Google Scholar]
- Rodriguez-Calero, M.A.; De Pedro-Gomez, J.E.; Molero-Ballester, L.J.; Fernandez-Fernandez, I.; Matamalas-Massanet, C.; Moreno-Mejias, L.; Blanco-Mavillard, I.; Moya-Suarez, A.B.; Personat-Labrador, C.; Morales-Asencio, J.M. Risk Factors for Difficult Peripheral Intravenous Cannulation. The PIVV2 Multicentre Case-Control Study. J. Clin. Med. 2020, 9, 799. Available online: https://pubmed.ncbi.nlm.nih.gov/32183475/ (accessed on 3 December 2021). [CrossRef]
- Hodzic, S.; Golic, D.; Smajic, J.; Sijercic, S.; Umihanic, S.; Umihanic, S. Complications Related to Insertion and Use of Central Venous Catheters (CVC). Med. Arch. 2014, 68, 300–303. Available online: https://pubmed.ncbi.nlm.nih.gov/25568558/ (accessed on 3 December 2021).
- Nayeemuddin, M.; Pherwani, A.D.; Asquith, J.R. Imaging and management of complications of central venous catheters. Clin. Radiol. 2013, 68, 529–544. Available online: https://pubmed.ncbi.nlm.nih.gov/23415017/ (accessed on 3 December 2021). [CrossRef]
- Duran-Gehring, P.; Bryant, L.; Reynolds, J.A.; Aldridge, P.; Kalynych, C.J.; Guirgis, F.W. Ultrasound-Guided Peripheral Intravenous Catheter Training Results in Physician-Level Success for Emergency Department Technicians. J. Ultrasound Med. 2016, 35, 2343–2352. Available online: https://pubmed.ncbi.nlm.nih.gov/27629755/ (accessed on 3 December 2021). [CrossRef]
- McCarthy, M.L.; Shokoohi, H.; Boniface, K.S.; Eggelton, R.; Lowey, A.; Lim, K.; Shesser, R.; Li, X.; Zeger, S.L. Ultrasonography Versus Landmark for Peripheral Intravenous Cannulation: A Randomized Controlled Trial. Ann. Emerg. Med. 2015, 68, 10–18. Available online: https://pubmed.ncbi.nlm.nih.gov/26475248/ (accessed on 3 December 2021). [CrossRef]
- AIUM. AIUM Practice Parameter for the Use of Ultrasound to Guide Vascular Access Procedures. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2019, 38, E4–E18. Available online: https://pubmed.ncbi.nlm.nih.gov/30758889/ (accessed on 3 December 2021).
- Millington, S.J.; Hendin, A.; Shiloh, A.L.; Koenig, S. Better with Ultrasound: Peripheral Intravenous Catheter Insertion. Chest 2020, 157, 369–375. Available online: https://pubmed.ncbi.nlm.nih.gov/31654617/ (accessed on 30 November 2021). [CrossRef] [PubMed]
- Franco-Sadud, R.; Schnobrich, D.; Matthews, B.K.; Candotti, C.; Abdel-Ghani, S.; Perez, M.G.; Rodgers, S.C.; Mader, M.J.; Haro, E.K.; Dancel, R.; et al. Recommendations on the Use of Ultrasound Guidance for Central and Peripheral Vascular Access in Adults: A Position Statement of the Society of Hospital Medicine. J. Hosp. Med. 2019, 14, E1–E22. Available online: https://pubmed.ncbi.nlm.nih.gov/31561287/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Alexandrou, E. Right Assessment and Vein Selection. In Vessel Health and Preservation: The Right Approach for Vascular Access; Springer: Cham, Switzerland, 2019; pp. 9–22. Available online: https://link.springer.com/chapter/10.1007/978-3-030-03149-7_2 (accessed on 19 January 2022).
- Walters, S.J. Sample size and power estimation for studies with health related quality of life outcomes: A comparison of four methods using the SF-36. Health Qual. Life Outcomes 2004, 2, 26. [Google Scholar] [CrossRef] [PubMed][Green Version]
- The R Project for Statistical Computing. Available online: https://www.r-project.org (accessed on 14 June 2017).
- Bahl, A.; Pandurangadu, A.V.; Tucker, J.; Bagan, M. A randomized controlled trial assessing the use of ultrasound for nurse-performed IV placement in difficult access ED patients. Am. J. Emerg. Med. 2016, 34, 1950–1954. Available online: https://pubmed.ncbi.nlm.nih.gov/27422220/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Villén Villegas, T.; Trueba Vicente, Á. Evaluación de dos métodos de canalización vascular con ayuda ecográfica en operadores sin experiencia previa. Emerg. Rev. Soc. Española Med. Urgenc. Emerg. 2015, 27, 43–45. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=5411752&info=resumen&idioma=ENG (accessed on 3 December 2021).
- Salleras-Duran, L.; Fuentes-Pumarola, C.; Bosch-Borràs, N.; Punset-Font, X.; Sampol-Granes, F.-X. Ultrasound-Guided Peripheral Venous Catheterization in Emergency Services. J. Emerg. Nurs. 2016, 42, 338–343. Available online: https://pubmed.ncbi.nlm.nih.gov/26953509/ (accessed on 3 December 2021). [CrossRef]
- Salleras-Duran, L.; Fuentes-Pumarola, C. Revisión bibliográfica sobre efectividad, complicaciones, satisfacción de los usuarios y profesionales en la cateterización periférica ecoguiada en relación con la técnica tradicional. Enferm. Clín. 2015, 26, 298–306. [Google Scholar]
- Van Loon, F.H.J.; Buise, M.P.; Claassen, J.J.F.; Dierick-van Daele, A.T.M.; Bouwman, A.R.A. Comparison of ultrasound guidance with palpation and direct visualisation for peripheral vein cannulation in adult patients: A systematic review and meta-analysis. Br. J. Anaesth. 2018, 121, 358–366. Available online: https://pubmed.ncbi.nlm.nih.gov/30032874/ (accessed on 3 December 2021). [CrossRef]
- Danski, M.T.R.; Oliveira AM de Meier, M.J.; Pedrolo, E. Efectividad de la ultrasonografía en la punción venosa periférica: Revisión integradora. Enferm. Glob. 2016, 15, 354–367. [Google Scholar] [CrossRef]
- Stolz, L.A.; Stolz, U.; Howe, C.; Farrell, I.J.; Adhikari, S. Ultrasound-Guided Peripheral Venous Access: A Meta-Analysis and Systematic Review. J. Vasc. Access 2015, 16, 321–326. Available online: https://pubmed.ncbi.nlm.nih.gov/25656255/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Egan, G.; Healy, D.; O’Neill, H.; Clarke-Moloney, M.; Grace, P.A.; Walsh, S. Ultrasound guidance for difficult peripheral venous access: Systematic review and meta-analysis. Emerg. Med. J. 2013, 30, 521–526. Available online: https://pubmed.ncbi.nlm.nih.gov/22886890/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Panebianco, N.L.; Fredette, J.M.; Szyld, D.; Sagalyn, E.B.; Pines, J.M.; Dean, A.J. What You See (Sonographically) Is What You Get: Vein and Patient Characteristics Associated with Successful Ultrasound-guided Peripheral Intravenous Placement in Patients with Difficult Access. Acad. Emerg. Med. 2009, 16, 1298–1303. Available online: https://pubmed.ncbi.nlm.nih.gov/19912132/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- González-Peredo, R.; Prieto-Salceda, M.D.; Campos-Caubet, L.; Fernández-Díaz, F.; García-Lago-Sierra Incera-Alvear, I.M. Characteristics of hospital emergency departments users. Frequent users. Semergen 2018, 44, 537–548. [Google Scholar] [CrossRef] [PubMed]
- Erickson, C.S.; Liao, M.M.; Haukoos, J.S.; Douglass, E.; DiGeronimo, M.; Christensen, E.; Hopkins, E.; Bender, B.; Kendall, J.L. Ultrasound-guided small vessel cannulation: Long-axis approach is equivalent to short-axis in novice sonographers experienced with landmark-based cannulation. West. J. Emerg. Med. 2014, 15, 824–830. Available online: https://pubmed.ncbi.nlm.nih.gov/25493126/ (accessed on 3 December 2021). [CrossRef]
- Revert Cogollos, A.; Cuenca Torres, M.; Caballero González, D.; Esquer Peris, M.J.; García Bermejo, P.; Garmilla Ezquerra, P. Calidad y adecuación de las vías periféricas en el servicio de urgencias. Enfermería Integral Rev. Científica Col. Of. Enfermería Valencia 2016, 26–30, ISSN 0214-0128. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=6123573&info=resumen&idioma=SPA (accessed on 3 December 2021).
- Costantino, T.G.; Parikh, A.K.; Satz, W.A.; Fojtik, J.P. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann. Emerg. Med. 2005, 46, 456–461. Available online: https://pubmed.ncbi.nlm.nih.gov/16271677/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Aponte, H.; Acosta, S.; Rigamonti, D.; Sylvia, B.; Austin, P.; Samolitis, T. The use of ultrasound for placement of intravenous catheters. AANA J. 2007, 75, 212–216. [Google Scholar]
- Weiner, S.G.; Sarff, A.R.; Esener, D.E.; Shroff, S.D.; Budhram, G.R.; Switkowski, K.M.; Mostofi, M.B.; Barus, R.W.; Coute, R.A.; Darvish, A.H. Single-operator ultrasound-guided intravenous line placement by emergency nurses reduces the need for physician intervention in patients with difficult-to-establish intravenous access. J. Emerg. Med. 2013, 44, 653–660. Available online: https://pubmed.ncbi.nlm.nih.gov/23103067/ (accessed on 3 December 2021). [CrossRef]
- Mahler, S.A.; Wang, H.; Lester, C.; Skinner, J.; Arnold, T.C.; Conrad, S.A. Short- vs long-axis approach to ultrasound-guided peripheral intravenous access: A prospective randomized study. Am. J. Emerg. Med. 2011, 29, 1194–1197. Available online: https://pubmed.ncbi.nlm.nih.gov/20951527/ (accessed on 3 December 2021). [CrossRef]
- Blanco, P. Ultrasound-guided peripheral venous cannulation in critically ill patients: A practical guideline. Ultrasound J. 2019, 11, 1–7. Available online: https://pubmed.ncbi.nlm.nih.gov/31624927/ (accessed on 3 December 2021). [CrossRef]
- Miles, G.; Salcedo, A.; Spear, D. Implementation of a successful registered nurse peripheral ultrasound-guided intravenous catheter program in an emergency department. J. Emerg. Nurs. 2012, 38, 353–356. Available online: https://pubmed.ncbi.nlm.nih.gov/21514651/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Fields, J.M.; Dean, A.J.; Todman, R.W.; Au, A.K.; Anderson, K.L.; Ku, B.S.; Pines, J.M.; Panebianco, N.L. The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity. Am. J. Emerg. Med. 2012, 30, 1134–1140. Available online: https://pubmed.ncbi.nlm.nih.gov/22078967/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Elia, F.; Ferrari, G.; Molino, P.; Converso, M.; De Filippi, G.; Milan, A.; Aprà, F. Standard-length catheters vs long catheters in ultrasound-guided peripheral vein cannulation. Am. J. Emerg. Med. 2012, 30, 712–716. Available online: https://pubmed.ncbi.nlm.nih.gov/21703801/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Bahl, A.; Hang, B.; Brackney, A.; Joseph, S.; Karabon, P.; Mohammad, A.; Nnanabu, I.; Shotkin, P. Standard long IV catheters versus extended dwell catheters: A randomized comparison of ultrasound-guided catheter survival. Am. J. Emerg. Med. 2019, 37, 715–721. Available online: https://pubmed.ncbi.nlm.nih.gov/30037560/ (accessed on 3 December 2021). [CrossRef]
- Pandurangadu, A.V.; Tucker, J.; Brackney, A.R.; Bahl, A. Ultrasound-guided intravenous catheter survival impacted by amount of catheter residing in the vein. Emerg. Med. J. 2018, 35, 550–555. Available online: https://pubmed.ncbi.nlm.nih.gov/30021833/ (accessed on 3 December 2021). [CrossRef] [PubMed]
- Adhikari, S.; Blaivas, M.; Morrison, D.; Lander, L. Comparison of infection rates among ultrasound-guided versus traditionally placed peripheral intravenous lines. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2010, 29, 741–747. Available online: https://pubmed.ncbi.nlm.nih.gov/20427786/ (accessed on 3 December 2021). [CrossRef]
- Miles, G.; Newcomb, P.; Spear, D. Comparison of Dwell-Times of Two Commonly Placed Peripheral Intravenous Catheters: Traditional vs. Ultrasound-Guided. Open J. Nurs. 2015, 5, 1082–1088. [Google Scholar] [CrossRef]
- Witting, M.; Schenkel, S.M.; Lawner, B.J.; Euerle, B.D. Effects of Vein Width and Depth on Ultrasound-Guided Peripheral Intravenous Success Rates. J. Emerg. Med. 2010, 39, 70–75. Available online: https://pubmed.ncbi.nlm.nih.gov/19272730/ (accessed on 3 December 2021). [CrossRef]
- Van Loon, F.H.; van Hooff, L.W.; de Boer, H.D.; Koopman, S.S.; Buise, M.P.; Korsten, H.H.; Dierick-van Daele, A.; Bouwman, A.R. The Modified A-DIVA Scale as a Predictive Tool for Prospective Identification of Adult Patients at Risk of a Difficult Intravenous Access: A Multicenter Validation Study. J. Clin. Med. 2019, 8, 144. Available online: https://pubmed.ncbi.nlm.nih.gov/30691137/ (accessed on 19 January 2022). [CrossRef]

| Variable | Total (n = 72) | Controls (n = 38) | Cases (n = 34) | p-Value | |
|---|---|---|---|---|---|
| Sex * | Man | 28 (39) | 16 (47) | 12 (35) | 0.6318 |
| Woman | 44 (61) | 22 (53) | 22 (65) | ||
| Age + | 68.55 ± 17.56 | 68.89 ± 18.77 | 68.18 ± 16.67 | 0.5384 | |
| BMI + | 29.49 ± 6.18 | 27.51 ± 5.56 | 31.52 ± 6.22 | 0.0058 | |
| Temperature + | 36.45 ± 0.74 | 36.52 ± 0.79 | 36.38 ± 0.67 | 0.7995 | |
| BP + | Systolic | 122.19 ± 26.24 | 124.39 ± 24.37 | 119.74 ± 28.35 | 0.4598 |
| Diastolic | 68.71 ± 16.99 | 68.47 ± 13.75 | 68.97 ± 20.22 | 0.6557 | |
| Triage priority * | 2 | 13 (18) | 8 (21) | 5 (15) | 0.5782 |
| 3 | 28 (39) | 16 (42) | 12 (35) | ||
| 4 | 31 (43) | 14 (37) | 17 (50) | ||
| Obesity * | 31 (43) | 12 (32) | 19 (56) | 0.028 | |
| DM * | 26 (36) | 9 (24) | 15 (44) | 0.028 | |
| Cytostatic treatment * | Never | 52 (72) | 28 (74) | 24 (71) | |
| Not currently | 7 (10) | 5 (13) | 2 (6) | ||
| Yes currently | 13 (18) | 5 (13) | 9 (23) | 0.355 | |
| Anticoagulant treatment * | 36 (50) | 17 (45) | 19 (56) | 0.479 | |
| NLIV Drug user * | 6 (8) | 5 (13) | 1 (3) | 0.203 | |
| Inability Puncture * | None | 51 (71) | 27 (71) | 24 (71) | 0.965 |
| CVA | 8 (11) | 3 (8) | 5 (15) | ||
| Ganglion extirpation | 5 (7) | 3 (8) | 2 (6) | ||
| AVF | 4 (6) | 2 (5) | 2 (6) | ||
| Skin lesions | 4 (6) | 3 (5) | 1 (3) |
| Variable | Total (n = 72) | Controls (n = 38) | Cases (n = 34) | p-Value | |
|---|---|---|---|---|---|
| Number of previous punctions + | 2.12 ± 1.24 | 2.92 ± 1.19 | 1.23 ± 0.43 | <0.001 | |
| Time (seconds) + | 385.93 ± 79.58 | 618.34 ± 387.16 | 126.17 ± 101.09 | <0.001 | |
| Pain + | Previous | 6.36 ± 1.87 | 6.65 ± 1.65 | 6.02 ± 2.07 | 0.157 |
| Present | 5.62 ± 2.09 | 6.55 ± 1.70 | 4.58 ± 2.03 | 0.023 | |
| Improvement | 0.74 ± 1.2 | 0.11 ± 0.39 | 1.44 ± 2.12 | <0.001 | |
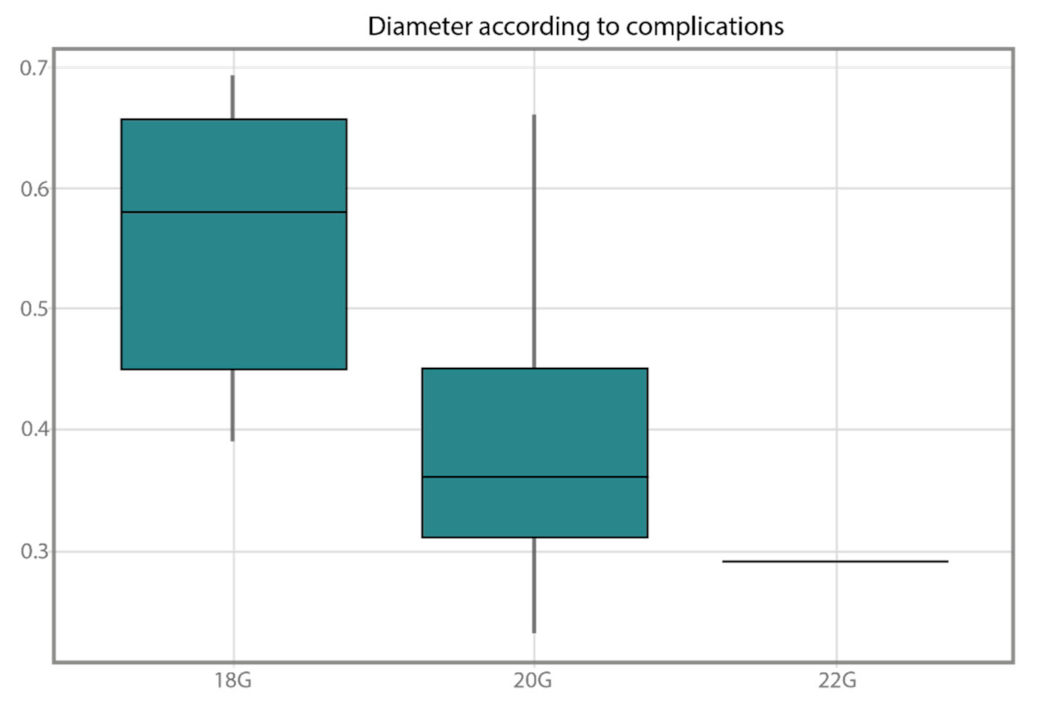
| Complications * | None | 33 | 8 | 25 | <0.001 |
| Ecchymosis | 28 | 26 | 2 | ||
| Hematoma | 11 | 11 | 0 | ||
| Extravasation | 19 | 12 | 7 | ||
| Prior punctures * | 1 | 32 (44) | 6 (16) | 26 (76) | <0.001 |
| 2 | 14 (19) | 6 (16) | 8 (24) | ||
| 3 | 15 (21) | 15 (39) | 0 (0) | ||
| 4 | 7 (1) | 7 (18) | 0 (0) | ||
| 5 | 4 (0.6) | 4 (11) | 0 (0) | ||
| Catheter gauge * | 18G | 14 (19) | 0 (0) | 14 (41) | <0.001 |
| 20G | 26 (36) | 7 (18) | 19 (56) | ||
| 22G | 20 (28) | 19 (50) | 1 (3) | ||
| 24G | 10 (14) | 10 (26) | 0 (0) | ||
| 26G | 2 (3) | 2 (5) | 0 (0) | ||
| Equation Variables | ||||||
|---|---|---|---|---|---|---|
| B | Standard Error | Wald | gl | Sig. | Exp(B) | |
| Technique | 56.674 | 3356.953 | 0.000 | 1 | 0.987 | 4102609739702777600000000.000 |
| BMI | 1.505 | 475.736 | 0.000 | 1 | 0.997 | 4.505 |
| Temperature | 30.429 | 2145.174 | 0.000 | 1 | 0.989 | 16418261462635.236 |
| Impossibility of puncture | 46.219 | 2367.183 | 0.000 | 1 | 0.984 | 118195291007880700000.000 |
| Cytostatic drugs | 14.084 | 4910.388 | 0.000 | 1 | 0.998 | 1307353.215 |
| DM | −0.668 | 13,073.356 | 0.000 | 1 | 1.000 | 0.513 |
| NLIV | −32.661 | 22,003.851 | 0.000 | 1 | 0.999 | 0.000 |
| Time | −0.663 | 33.719 | 0.000 | 1 | 0.984 | 0.515 |
| Difficulty | −9.505 | 1078.693 | 0.000 | 1 | 0.993 | 0.000 |
| Area of puncture | −28.355 | 8800.896 | 0.000 | 1 | 0.997 | 0.000 |
| Constant | −1024.217 | 71,753.598 | 0.000 | 1 | 0.989 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Herrera, Á.; Solaz-García, Á.; Mollá-Olmos, E.; Ferrer-Puchol, D.; Esteve-Claramunt, F.; Trujillo-Barberá, S.; García-Bermejo, P.; Casaña-Mohedo, J. Use of the Ultrasound Technique as Compared to the Standard Technique for the Improvement of Venous Cannulation in Patients with Difficult Access. Healthcare 2022, 10, 261. https://doi.org/10.3390/healthcare10020261
Rodríguez-Herrera Á, Solaz-García Á, Mollá-Olmos E, Ferrer-Puchol D, Esteve-Claramunt F, Trujillo-Barberá S, García-Bermejo P, Casaña-Mohedo J. Use of the Ultrasound Technique as Compared to the Standard Technique for the Improvement of Venous Cannulation in Patients with Difficult Access. Healthcare. 2022; 10(2):261. https://doi.org/10.3390/healthcare10020261
Chicago/Turabian StyleRodríguez-Herrera, Ángeles, Álvaro Solaz-García, Enrique Mollá-Olmos, Dolores Ferrer-Puchol, Francisca Esteve-Claramunt, Silvia Trujillo-Barberá, Pedro García-Bermejo, and Jorge Casaña-Mohedo. 2022. "Use of the Ultrasound Technique as Compared to the Standard Technique for the Improvement of Venous Cannulation in Patients with Difficult Access" Healthcare 10, no. 2: 261. https://doi.org/10.3390/healthcare10020261
APA StyleRodríguez-Herrera, Á., Solaz-García, Á., Mollá-Olmos, E., Ferrer-Puchol, D., Esteve-Claramunt, F., Trujillo-Barberá, S., García-Bermejo, P., & Casaña-Mohedo, J. (2022). Use of the Ultrasound Technique as Compared to the Standard Technique for the Improvement of Venous Cannulation in Patients with Difficult Access. Healthcare, 10(2), 261. https://doi.org/10.3390/healthcare10020261