Immediate Effects of Single-Session High-Velocity Training for Lateral Trunk Movement on Gait Function in Early Postoperative Patients after Total Hip Arthroplasty: A Nonrandomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
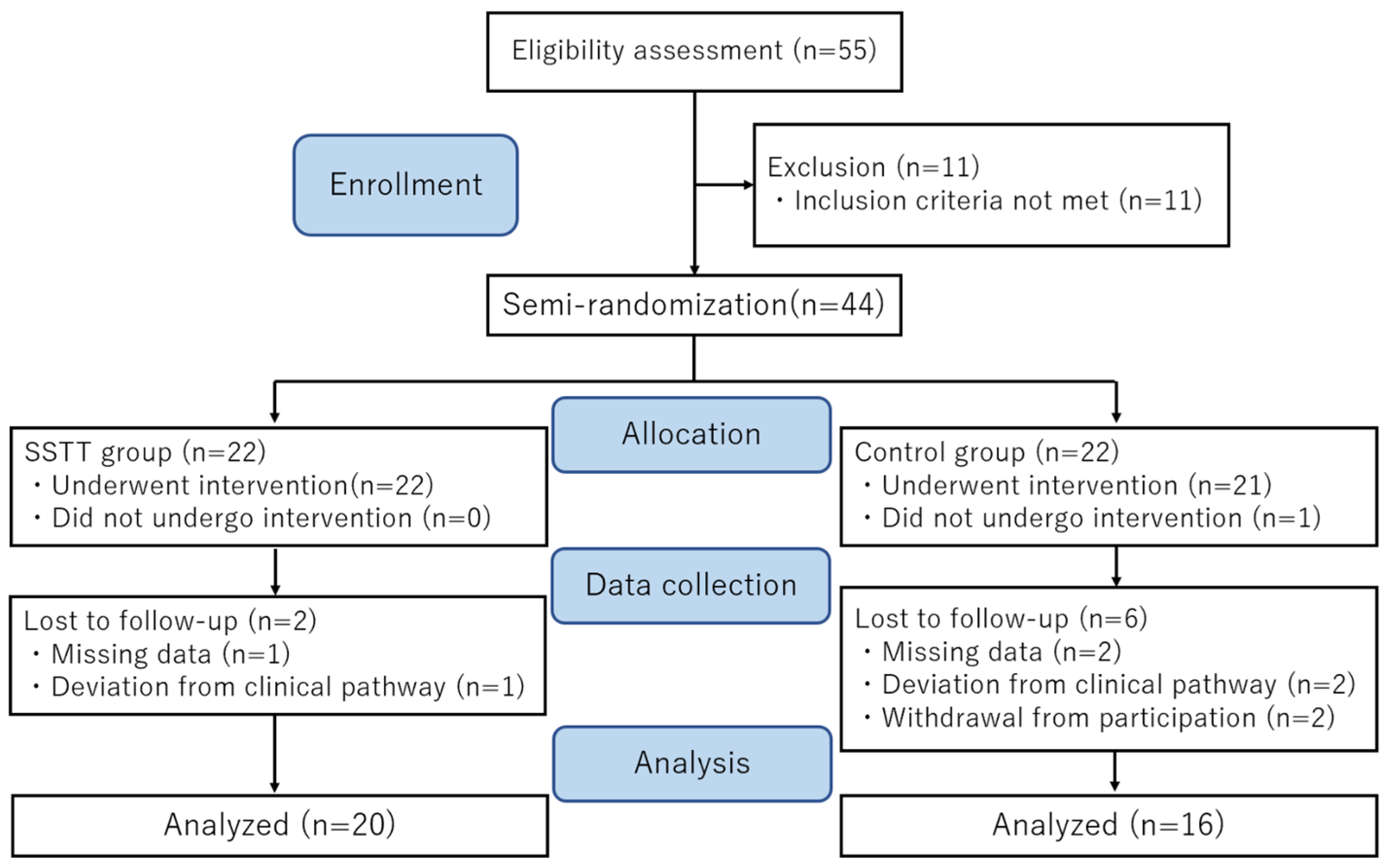
2.1. Participants
2.2. Measurement
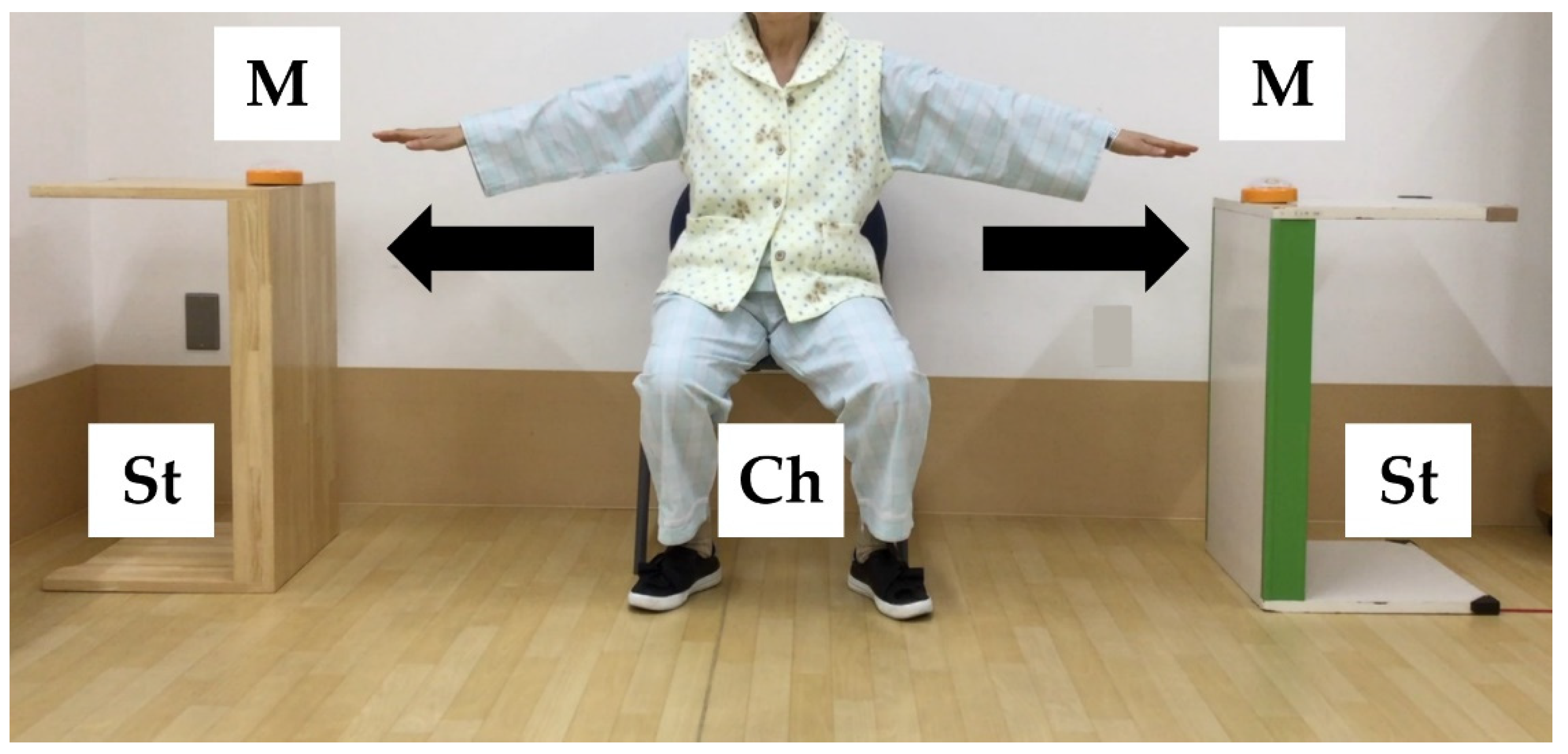
2.3. Interventions
2.4. Statistical Analysis
3. Results
3.1. Basic Characteristics
3.2. Gait Function and Lower Extremity Muscle Strength
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Singh, J.A.; Lewallen, D.G. Patient-level clinically meaningful improvements in activities of daily living and pain after total hip arthroplasty: Data from a large US institutional registry. Rheumatology 2013, 52, 1109–1118. [Google Scholar] [CrossRef] [PubMed]
- Vissers, M.M.; Bussmann, J.B.; Verhaar, J.A.; Arends, L.R.; Furlan, A.D.; Reijman. Recovery of physical functioning after total hip arthroplasty: Systematic review and meta-analysis of the literature. Phys. Ther. 2011, 91, 615–629. [Google Scholar] [CrossRef] [PubMed]
- Zawadsky, M.W.; Paulus, M.C.; Murray, P.J.; Johansen, M.A. Early outcome comparison between the direct anterior approach and the mini-incision posterior approach for primary total hip arthroplasty: 150 consecutive cases. J. Arthroplast. 2014, 29, 1256–1260. [Google Scholar] [CrossRef] [PubMed]
- Stambough, J.B.; Nunley, R.M.; Curry, M.C.; Steger-May, K.; Clohisy, J.C. Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions. J. Arthroplast. 2015, 30, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Morri, M.; Natali, E.; Tosarelli, D. At discharge gait speed and independence of patients provides a challenges for rehabilitation after total joint arthroplasty: An observational study. Arch. Physiother. 2016, 29, 6. [Google Scholar] [CrossRef]
- Mahomed, N.M.; Davis, A.M.; Hawker, G.; Badley, E.; Syed, K.A.; Coyte, P.C.; Gandhi, R.; Wright, J. Inpatient compared with home-based rehabilitation following primary unilateral total hip or knee replacement: A randomized controlled trial. J. Bone Joint Surg. Am. 2008, 90, 1673–1680. [Google Scholar] [CrossRef]
- Galea, M.P.; Levinger, P.; Lythgo, N.; Cimoli, C.; Weller, R.; Tully, E.; McMeeken, J.; Westh, R. A targeted home- and center-based exercise program for people after total hip replacement: A randomized clinical trial. Arch. Phys. Med. Rehabil. 2008, 89, 1442–1447. [Google Scholar] [CrossRef]
- Jan, M.H.; Hung, J.Y.; Lin, J.C.; Wang, S.F.; Liu, T.K.; Tang, P.F. Effects of a home program on strength, walking speed, and function after total hip replacement. Arch. Phys. Med. Rehabil. 2004, 85, 1943–1951. [Google Scholar] [CrossRef]
- Unlu, E.; Eksioglu, E.; Aydog, E.; Atay, G. The effect of exercise on hip muscle strength, gait speed and cadence in patients with total hip arthroplasty: A randomized controlled study. Clin. Rehabil. 2007, 21, 706–711. [Google Scholar] [CrossRef]
- Rahmann, A.E.; Brauer, S.G.; Nitz, J.C. A specific inpatient aquatic physiotherapy program improves strength after total hip or knee replacement surgery: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2009, 90, 745–755. [Google Scholar] [CrossRef]
- Kyrdalen, I.L.; Thingstad, P.; Sandvik, L.; Ormstad, H. Associations between gait speed and well-knowen fall risk factors among community-dwelling older adults. Physiother. Res. Int. 2019, 24, e1743. [Google Scholar] [CrossRef] [PubMed]
- Cuoco, A.; Callahan, D.M.; Sayers, S.; Frontera, W.R.; Bean, J.; Fielding, B.A. Impact of muscle power and force on gait speed in disabled older men and women. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 1200–1206. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.; Whitehurst, M. The effect of short-term isokinetic training on force and rate of velocity development. J. Strength Cond. Res. 2003, 17, 88–94. [Google Scholar] [PubMed]
- Prevost, M.; Nelson, A.; Maraj, B.K. The effect of two days of velocity-specific isokinetic training on torque production. J. Strength Cond. Res. 1999, 13, 35–39. [Google Scholar]
- Coburn, J.W.; Housh, T.J.; Malek, M.H.; Weir, J.P.; Cramer, J.T.; Bec, T.W.; Johnson, G.O. Neuromuscular responses to three days of velocity-specific isokinetic training. J. Strength Cond. Res. 2006, 20, 892–898. [Google Scholar]
- Sano, Y.; Iwata, A.; Wanaka, H.; Matsui, M.; Yamamoto, S.; Koyanagi, J.; Iwata, H. An easy and safe training method for trunk function improves mobility in total knee arthroplasty patients: A quasi-randomized controlled trial. PLoS ONE 2018, 13, e0204884. [Google Scholar] [CrossRef]
- Helbostad, J.L.; Moe-Nilssen, R. The effect of gait speed on lateral barance control during walking in healthy elderly. Gait Posture 2003, 18, 27–36. [Google Scholar] [CrossRef]
- Hausdorff, J.M.; Rios, D.A.; Edelberg, H.K. Gait variability and fall risk in community-living older adults: A 1-year prospective study. Arch. Phys. Med. Rehabil. 2001, 82, 1050–1056. [Google Scholar] [CrossRef]
- Lindemann, U.; Becker, C.; Unnewehr, I.; Muche, R.; Aminin, K.; Dejnabadi, H.; Nikolaus, T.; Puhl, W.; Huch, K.; Dreinhöfer, K.E. Gait analysis and WOMAC are complementary in assessing functional outcome in total hip replacement. Clin. Rehabil. 2006, 20, 413–420. [Google Scholar] [CrossRef]
- Ikutomo, H.; Nagai, K.; Nakagawa, N.; Masuhara, K. Falls in patients after total hip arthroplasty in Japan. J. Orthop. Sci. 2015, 20, 663–668. [Google Scholar] [CrossRef]
- Kang, H.G.; Dingwell, J.B. Dynamic stability of superior vs. inferior segments during walking in young and older adults. Gait Posture 2009, 30, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.; Huskisson, E.C. Graphic representation of pain. Pain 1976, 2, 175–184. [Google Scholar] [CrossRef]
- Salarian, A.; Russmann, H.; Vingerhoets, F.J.; Dehollain, C.; Blanc, Y.; Burkhard, P.R.; Aminian, K. Gait assessment in Parkinson’s disease: Toward an ambulatory system for long-term monitoring. IEEE Trans. Biomed. Eng. 2004, 51, 1434–1443. [Google Scholar] [CrossRef] [PubMed]
- Beauchet, O.; Dubost, V.; Aminian, K.; Gonthier, R.; Kressig, R.W. Dual-task-related gait changes in the elderly: Does the type of cognitive task matter? J. Mot. Behav. 2005, 37, 259–264. [Google Scholar]
- Hayashi, K.; Kako, M.; Suzuki, K.; Hattori, K.; Fukuyasu, S.; Sato, K.; Kadono, I.; Sakai, T.; Hasegawa, Y.; Nishida, Y. Associations among pain catastrophizing, muscle strength, and physical performance after total knee and hip arthroplasty. World J. Orthop. 2017, 8, 336–341. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Perera, S.; Mody, S.H.; Woodman, R.C.; Studenski, S.A. Meaningful change and responsiveness in common physical performance measures in older adults. J. Am. Geriatr. Soc. 2006, 54, 743–749. [Google Scholar] [CrossRef]
- Iwata, A.; Higuchi, Y.; Kimura, D.; Okamoto, K.; Arai, S.; Iwata, H.; Fuchioka, S. Quick lateral movements of the trunk in a seated position reflect mobility and activities of daily living (ADL) function in frail elderly individuals. Arch. Gerontol. Geriatr. 2013, 56, 482–486. [Google Scholar] [CrossRef]
- Perron, M.; Malouin, F.; Moffet, H.; McFadyen, B.J. Three-dimensional gait analysis in women with a total hip arthroplasty. Clin. Biomech. 2000, 15, 504–515. [Google Scholar] [CrossRef]
- Hodt-Billington, C.; Helbostad, J.L.; Vervaat, W.; Rognsvåg, T.; Moe-Nilssen, R. Changes in gait symmetry, gait velocity and self-reported function following total hip replacement. J. Rehabil. Med. 2011, 43, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.J.; Kim, J.S.; Wang, J.S.; Park, J.H.; Choi, J.H. The effects of isometric trunk exercises and dynamic trunk exercises on gait in elderly people. J. Phys. Ther. Sci. 2015, 27, 1685–1689. [Google Scholar] [CrossRef] [PubMed]
- Karthikbabu, S.; Rao, B.K.; Manikandan, N.; Solomon, J.M.; Chakrapani, M.; Nayak, A. Role of Trunk Rehabilitation on Trunk Control, Balance and Gait in Patients with Chronic Stroke: A Pre-Post Design. Neurosci. Med. 2011, 2, 61–67. [Google Scholar] [CrossRef]
- McKinnon, N.B.; Connelly, D.M.; Rice, C.L.; Hunter, S.W.; Doherty, T.J. Neuromuscular contributions to the age-related reduction in muscle power: Mechanisms and potential role of high velocity power training. Ageing Res. Rev. 2017, 35, 147–154. [Google Scholar] [CrossRef]
- Mosole, S.; Carraro, U.; Kern, H.; Loefler, S.; Fruhmann, H.; Vogelauer, M.; Burggraf, S.; Mayr, W.; Krenn, M.; Paternostro-Sluga, T.L.; et al. Long-term high-level exercise promotes muscle reinnervation with age. J. Neuropathol. Exp. Neurol. 2014, 73, 284–294. [Google Scholar] [CrossRef]
- Friesenbichler, B.; Casartelli, N.C.; Wellauer, V.; Item-Glatthorn, J.F.; Ferguson, S.T.; Leunig, M.; Maffiuletti, N.A. Explosive and maximal strength before and 6 months after total hip arthroplasty. J. Orthop. Res. 2017, 36, 425–431. [Google Scholar]
- Glenn, J.M.; Gray, M.; Binns, A. The effects of loaded and unloaded high-velocity resistance training on functional fitness among community-dwelling older adults. Age Ageing 2015, 44, 926–931. [Google Scholar] [CrossRef][Green Version]
- Fukumoto, Y.; Tateuchi, H.; Tsukagoshi, R.; Okita, Y.; Akiyama, H.; So, K.; Kuroda, Y.; Ichihashi, N. Effects of High- and Low-Velocity Resistance Training on Gait Kinematics and Kinetics in Individuals with Hip Osteoarthritis: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2017, 96, 417–423. [Google Scholar] [CrossRef]
- Gabell, A.; Nayak, U.S. The effect of age on variability in gait. J. Gerontol. 1984, 39, 662–666. [Google Scholar] [CrossRef]
- Moe-Nilssen, R.; Helbostad, J.L. Estimation of gait cycle characteristics by trunk accelerometry. J. Biomech. 2004, 37, 121–126. [Google Scholar] [CrossRef]
- Labanca, L.; Ciardulli, F.; Bonsanto, F.; Sommella, N.; Martino, A.D.; Benedetti, M.G. Balance and proprioception impairment, assessment tools, and rehabilitation training in patients with total hip arthroplasty: A systematic review. BMC Musculoskelet. Disord. 2021, 22, 1055. [Google Scholar] [CrossRef] [PubMed]
- Schweigart, G.; Chien, R.D.; Mergner, T. Neck proprioception compensates for age-related deterioration of vestibular self-motion perception. Exp. Brain Res. 2002, 147, 89–97. [Google Scholar] [CrossRef] [PubMed]

| SSTT Group | Control Group | p Value | |
|---|---|---|---|
| n = 20 | n = 16 | ||
| Age (y) | 66.5 ± 7.0 | 62.6 ± 9.1 | 0.156 |
| Height (m) | 1.52 ± 0.05 | 1.55 ± 0.06 | 0.083 |
| Body weight (kg) | 55.0 ± 8.3 | 56.3 ± 9.5 | 0.650 |
| Body mass index (kg/m2) | 23.7 ± 3.7 | 23.1 ± 3.1 | 0.606 |
| Kellgren–Lawrence grade III/IV | 0/20 | 1/15 | 0.256 |
| Visual Analog Scale | 5.4 ± 7.9 | 6.3 ± 10.2 | 0.780 |
| SSTT Group (n = 20) | Control Group (n = 16) | Interaction (Group × Time) | Effect Size (d) | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||
| Gait speed (m/s) | 0.96 ± 0.2 | 1.08 ± 0.2 * | 0.99 ± 0.2 | 1.00 ± 0.2 | 0.000 | 0.810 | |
| Stride time (s) | 1.09 ± 0.2 | 1.02 ± 0.1 * | 1.06 ± 0.1 | 1.05 ± 0.1 | 0.000 | 0.900 | |
| CV (%) | 2.29 ± 0.9 | 1.76 ± 0.7 * | 1.99 ± 0.5 | 2.00 ± 0.6 | 0.000 | 0.570 | |
| Hip abductor strength (Nm) | |||||||
| Operation side | 21.4 ± 5.8 | 20.8 ± 6.0 | 19.5 ± 3.9 | 19.4 ± 3.7 | 0.879 | ||
| Non-operation side | 33.3 ± 7.8 | 33.7 ± 8.2 | 32.8 ± 7.4 | 32.7 ± 7.6 | 0.789 | ||
| Knee extensor strength (Nm) | |||||||
| Operation side | 40.6 ± 12.0 | 40.2 ± 12.2 | 39.6 ± 9.3 | 38.8 ± 9.1 | 0.815 | ||
| Non-operation side | 65.6 ± 21.5 | 64.5 ± 20.7 | 64.3 ± 13.6 | 63.8 ± 13.5 | 0.765 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Honma, K.; Yano, Y.; Yamamoto, S.; Ohmine, T.; Wanaka, H.; Senzaki, K.; Kanayama, A.; Oonishi, H.; Iwata, A. Immediate Effects of Single-Session High-Velocity Training for Lateral Trunk Movement on Gait Function in Early Postoperative Patients after Total Hip Arthroplasty: A Nonrandomized Controlled Trial. Healthcare 2022, 10, 256. https://doi.org/10.3390/healthcare10020256
Honma K, Yano Y, Yamamoto S, Ohmine T, Wanaka H, Senzaki K, Kanayama A, Oonishi H, Iwata A. Immediate Effects of Single-Session High-Velocity Training for Lateral Trunk Movement on Gait Function in Early Postoperative Patients after Total Hip Arthroplasty: A Nonrandomized Controlled Trial. Healthcare. 2022; 10(2):256. https://doi.org/10.3390/healthcare10020256
Chicago/Turabian StyleHonma, Keisuke, Yuki Yano, Saki Yamamoto, Toshimitsu Ohmine, Hideyuki Wanaka, Kazuma Senzaki, Atsuki Kanayama, Hiroyuki Oonishi, and Akira Iwata. 2022. "Immediate Effects of Single-Session High-Velocity Training for Lateral Trunk Movement on Gait Function in Early Postoperative Patients after Total Hip Arthroplasty: A Nonrandomized Controlled Trial" Healthcare 10, no. 2: 256. https://doi.org/10.3390/healthcare10020256
APA StyleHonma, K., Yano, Y., Yamamoto, S., Ohmine, T., Wanaka, H., Senzaki, K., Kanayama, A., Oonishi, H., & Iwata, A. (2022). Immediate Effects of Single-Session High-Velocity Training for Lateral Trunk Movement on Gait Function in Early Postoperative Patients after Total Hip Arthroplasty: A Nonrandomized Controlled Trial. Healthcare, 10(2), 256. https://doi.org/10.3390/healthcare10020256






