Perception Bias Effects on Healthcare Management in COVID-19 Pandemic: An Application of Cumulative Prospect Theory
Abstract
:1. Introduction
2. Literature Review
2.1. Research on the Impact of COVID-19 and Policy Delphi Method
2.2. Cumulative Prospect Theory and Its Applications
2.3. Factors Affecting Healthcare Decisions
3. Methodology
3.1. Decision Task Design and Factors Using Policy Delphi Method
3.2. CPT Decision Model and Measurement of Prospect Values
3.3. Survey Method
4. Results
4.1. Policy Delphi Results
4.2. Estimation Results of Risk Perception and Attitude
4.3. Regression Results for the Effects of Individual and Organizational Factors
5. Discussion
5.1. Risk Perception and Attitude
5.2. Biased Effects of Individual and Organizational Factors
6. Conclusions and Implications
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
- Demographic data: gender, job title, the funding status of the organization, LTCF type, and facility scale.
- Organizational strategy type: On a scale of 1 (strongly disagree) to 7 (strongly agree), please select the option that most nearly corresponds with your organizations’ operations strategies.
- (1)
- My care organization provides innovative, differentiated, diverse, and large-scale care services/programs.
- (2)
- My care organization engages in a cost-efficient analysis of equipment and resources, facilities, the workforce, and care services/programs.
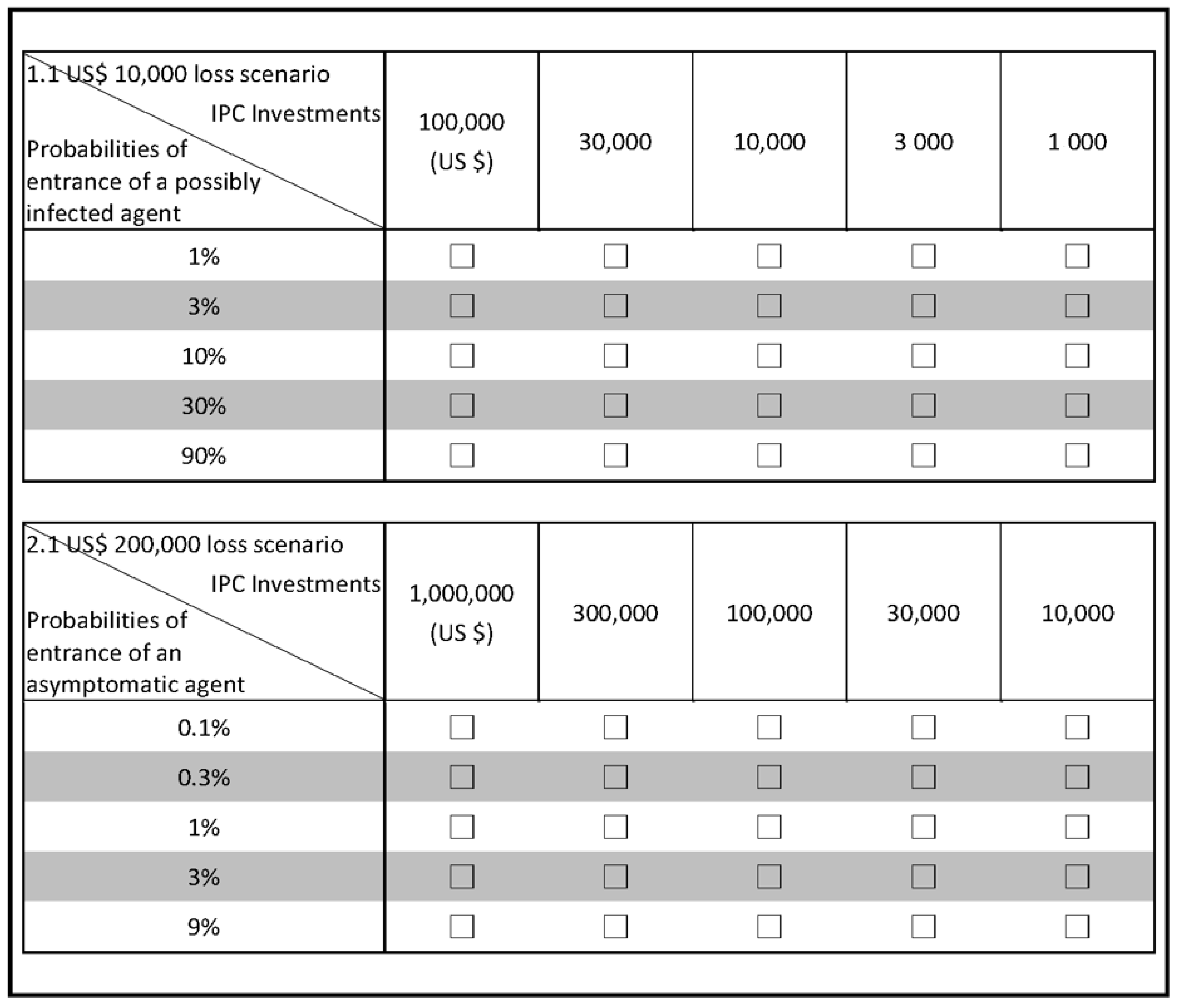
- Decision tasks for investing IPC measures to minimize the damages caused by COVID-19:
- (1)
- Decision Task 1. If a possibly infected stakeholder (i.e., resident, staff member, or visitor) enters the facilities, he/she may be a source of infection risk that causes a facility-wide outbreak. Thus, LTCFs need additional administrative and financial resources to support IPC activities focused on the abovementioned stakeholders to prevent damage. Five financial loss scenarios were presented, namely, USD 10,000, 40,000, 70,000, 100,000, and 130,000. We assumed five probabilities of a possibly infected stakeholder’s entrance occurrence for each loss scenario, namely, 1% (i.e., one possible agent among 100 agents who entered the facilities), 3%, 10%, 30%, and 90%. This study assumed that LTCFs would invest in the IPC practices suggested by the WHO and CDC to prevent infection risk. The amount of IPC investment included five choices, namely, USD 1000, 3000, 10,000, 30,000, and 100,000. Task 1 included answering the question, “What is the acceptable amount of investment in IPC measures that your organization would choose to minimize the damages caused by COVID-19 under numerous decisions when considering various probabilities and different loss scenarios simultaneously?”
- (2)
- Decision Task 2. If an asymptomatic stakeholder (i.e., resident, staff member, or visitor) enters the facilities, he/she may be a source of infection risk that causes a facility-wide outbreak. Five financial loss scenarios were assumed, namely, USD 200,000, 500,000, 800,000, 1,100,000, and 1,400,000. For each loss scenario of Task 2, we assumed five probabilities of an asymptomatic case entrance occurrence, namely, 0.1% (i.e., one asymptomatic agent among 1000 agents who entered the facilities), 0.3%, 1%, 3%, and 9%. The amount of IPC investment included five choices, namely, USD 10,000, 30,000, 100,000, 300,000, and 1,000,000. Task 2 involved answering the question, “What is the acceptable amount of investment in IPC measures that your organization would choose to minimize the damages caused by COVID-19 under numerous decisions when considering various probabilities and different loss scenarios simultaneously?”
References
- WHO. Infection Prevention and Control Guidance for Long-Term Care Facilities in the Context of COVID-19: Interim Guidance. Available online: https://apps.who.int/iris/bitstream/handle/10665/331508/WHO-2019-nCoV-IPC_long_term_care-2020.1-eng.pdf?sequence=1&isAllowed=y (accessed on 20 June 2021).
- WHO. Strengthening the Health System Response to COVID-19. Maintaining the Delivery of Essential Health Care Services While Mobilizing the Health Workforce for the COVID-19 Response (18 April 2020). Available online: https://apps.who.int/iris/bitstream/handle/10665/332559/WHO-EURO-2020-669-40404-54161-eng.pdf?sequence=1&isAllowed=y (accessed on 20 June 2021).
- WHO. Report Coronavirus Disease 2019 (COVID-19) Situation Report-179. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200717-covid-19-sitrep-179.pdf (accessed on 20 June 2021).
- D’Adamo, H.; Yoshikawa, T.; Ouslander, J.G. Coronavirus disease 2019 in geriatrics and long-term care: The ABCDs of COVID-19. J. Am. Geriatr. Soc. 2020, 68, 912–917. [Google Scholar] [CrossRef] [PubMed]
- Levitt, A.F.; Ling, S.M. COVID-19 in the Long-Term Care Setting: The CMS Perspective. J. Am. Geriatr. Soc. 2020, 68, 1366–1369. [Google Scholar] [CrossRef] [PubMed]
- Yen, M.-Y.; Schwartz, J.; King, C.-C.; Lee, C.-M.; Hsueh, P.-R. Recommendation on protection from and mitigation of COVID-19 pandemic in long-term care facilities. J. Microbiol. Immunol. Infect. 2020, 53, 447–453. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Infection Prevention and Control and Preparedness for COVID-19 in Healthcare Settings—Third Update. 13 May 2020. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/Infection-prevention-control-for-the-care-of-patients-with-2019-nCoV-healthcare-settings_third-update.pdf (accessed on 20 July 2021).
- Kamp, J.; Mathews, A.W. Coronavirus Outbreaks Spreading in Nursing Homes. Available online: https://www.wsj.com/articles/coronavirus-outbreaks-spreading-in-nursing-homes-11584628291 (accessed on 20 June 2020).
- Carter, P.; Anderson, M.; Mossialos, E. Health system, public health, and economic implications of managing COVID-19 from a cardiovascular perspective. Eur. Heart J. 2020, 41, 2516–2518. [Google Scholar] [CrossRef] [Green Version]
- Renda, A.; Castro, R. Towards stronger EU governance of health threats after the COVID-19 pandemic. Eur. J. Risk Regul. 2020, 11, 273–282. [Google Scholar] [CrossRef] [Green Version]
- Sharma, P.; Leung, T.Y.; Kingshott, R.P.; Davcik, N.S.; Cardinali, S. Managing uncertainty during a global pandemic: An international business perspective. J. Bus. Res. 2020, 116, 188–192. [Google Scholar] [CrossRef]
- McAleer, M. Prevention is better than the cure: Risk management of COVID-19. J. Risk Financ. Manag. 2020, 13, 46. [Google Scholar] [CrossRef] [Green Version]
- Bhaskar, S.; Tan, J.; Bogers, M.L.; Minssen, T.; Badaruddin, H.; Israeli-Korn, S.; Chesbrough, H. At the epicenter of COVID-19–the tragic failure of the global supply chain for medical supplies. Front. Public Health 2020, 8, 821. [Google Scholar] [CrossRef]
- Kuo, S.; Ou, H.-T.; Wang, C.J. Managing medication supply chains: Lessons learned from Taiwan during the COVID-19 pandemic and preparedness planning for the future. J. Am. Pharm. Assoc. 2021, 61, e12–e15. [Google Scholar] [CrossRef]
- Choi, T.-M. Risk analysis in logistics systems: A research agenda during and after the COVID-19 pandemic. Tranportation Res. Part E 2021, 145, 102190. [Google Scholar] [CrossRef]
- Liu, Y.; Fan, Z.-P.; Zhang, Y. Risk decision analysis in emergency response: A method based on cumulative prospect theory. Comput. Oper. Res. 2014, 42, 75–82. [Google Scholar] [CrossRef]
- Bertsimas, D.; Boussioux, L.; Cory-Wright, R.; Delarue, A.; Digalakis, V.; Jacquillat, A.; Kitane, D.L.; Lukin, G.; Li, M.; Mingardi, L.; et al. From predictions to prescriptions: A data-driven response to COVID-19. Health Care Manag. Sci. 2021, 24, 253–272. [Google Scholar] [CrossRef] [PubMed]
- Barberis, N.C. Thirty years of prospect theory in economics: A review and assessment. J. Econ. Perspect. 2013, 27, 173–195. [Google Scholar] [CrossRef] [Green Version]
- Fennema, H.; Wakker, P. Original and cumulative prospect theory: A discussion of empirical differences. J. Behav. Decis. Mak. 1997, 10, 53–64. [Google Scholar] [CrossRef]
- Cagliano, A.C.; Grimaldi, S.; Rafele, C. A systemic methodology for risk management in healthcare sector. Saf. Sci. 2011, 49, 695–708. [Google Scholar] [CrossRef] [Green Version]
- Fraser-Mackenzie, P.; Sung, M.C.; Johnson, J.E. Toward an understanding of the influence of cultural background and domain experience on the effects of risk-pricing formats on risk perception. Risk Anal. 2014, 34, 1846–1869. [Google Scholar] [CrossRef] [Green Version]
- Leung, T.Y.; Sharma, P.; Adithipyangkul, P.; Hosie, P. Gender equity and public health outcomes: The COVID-19 experience. J. Bus. Res. 2020, 116, 193–198. [Google Scholar] [CrossRef]
- March, J.G.; Shapira, Z. Managerial perspectives on risk and risk taking. Manag. Sci. 1987, 33, 1404–1418. [Google Scholar] [CrossRef] [Green Version]
- McNamara, G.; Bromiley, P. Decision making in an organizational setting: Cognitive and organizational influences on risk assessment in commercial lending. Acad. Manag. J. 1997, 40, 1063–1088. [Google Scholar]
- Robinson, P.J.; Botzen, W.W. Determinants of probability neglect and risk attitudes for disaster risk: An online experimental study of flood insurance demand among homeowners. Risk Anal. 2019, 39, 2514–2527. [Google Scholar] [CrossRef] [Green Version]
- Danis, K.; Fonteneau, L.; Georges, S.; Daniau, C.; Bernard-Stoecklin, S.; Domegan, L.; O’Donnell, J.; Hauge, S.H.; Dequeker, S.; Vandael, E.; et al. High impact of COVID-19 in long-term care facilities, suggestion for monitoring in the EU/EEA, May 2020. Eurosurveillance 2020, 25, 2000956. [Google Scholar]
- Comas-Herrera, A.; Zalakaín, J. Mortality associated with COVID-19 outbreaks in care homes: Early international evidence. Int. Long-Term Care Policy Netw. 2020, 12, 1–6. [Google Scholar]
- CDC. Infection Prevention and Control Assessment Tool for Nursing Homes Preparing for COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/downloads/hcp/assessment-tool-nursing-homes.pdf (accessed on 5 July 2020).
- Leite, H.; Lindsay, C.; Kumar, M. COVID-19 outbreak: Implications on healthcare operations. TQM J. 2021, 33, 247–256. [Google Scholar] [CrossRef]
- De Loë, R.C.; Melnychuk, N.; Murray, D.; Plummer, R. Advancing the state of policy Delphi practice: A systematic review evaluating methodological evolution, innovation, and opportunities. Technol. Forecast. Soc. Change 2016, 104, 78–88. [Google Scholar] [CrossRef]
- de Meyrick, J. The Delphi method and health research. Health Educ. 2003, 103, 7–16. [Google Scholar] [CrossRef]
- Meskell, P.; Murphy, K.; Shaw, D.G.; Casey, D. Insights into the use and complexities of the Policy Delphi technique. Nurse Res. 2014, 21, 7–16. [Google Scholar] [CrossRef]
- Paraskevas, A.; Saunders, M.N. Beyond consensus: An alternative use of Delphi enquiry in hospitality research. Int. J. Contemp. Hosp. Manag. 2012, 24, 907–924. [Google Scholar] [CrossRef] [Green Version]
- Kahneman, D.; Tversky, A. Prospect theory: An analysis of decision under risk. Econom. J. Econom. society 1979, 47, 263–291. [Google Scholar] [CrossRef] [Green Version]
- Tversky, A.; Kahneman, D. Advances in prospect theory: Cumulative representation of uncertainty. J. Risk Uncertain. 1992, 5, 297–323. [Google Scholar] [CrossRef]
- Levy, J.S. An introduction to prospect theory. Political Psychol. 1992, 13, 171–186. [Google Scholar]
- Booij, A.S.; Van de Kuilen, G. A parameter-free analysis of the utility of money for the general population under prospect theory. J. Econ. Psychol. 2009, 30, 651–666. [Google Scholar] [CrossRef]
- Goda, K.; Hong, H. Implied preference for seismic design level and earthquake insurance. Risk Anal. Int. J. 2008, 28, 523–537. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.-M.; Wu, T.; Chen, Y.J. Over- and under-estimation of risks and counteractive adjustment for cold chain operations: A prospect theory perspective. Int. J. Logist. Manag. 2018, 29, 902–921. [Google Scholar] [CrossRef]
- De La Maza, C.; Davis, A.; Gonzalez, C.; Azevedo, I. Understanding cumulative risk perception from judgments and choices: An application to flood risks. Risk Anal. 2019, 39, 488–504. [Google Scholar] [CrossRef] [PubMed]
- Bern-Klug, M. Considering the CPR decision through the Lens of Prospect theory in the context of advanced chronic illness. Gerontol. 2017, 57, 61–67. [Google Scholar] [CrossRef]
- Winter, L.; Lawton, M.P.; Ruckdeschel, K. Preferences for prolonging life: A prospect theory approach. Int. J. Aging Hum. Dev. 2003, 56, 155–170. [Google Scholar] [CrossRef]
- Winter, L.; Parker, B. Current health and preferences for life-prolonging treatments: An application of prospect theory to end-of-life decision making. Soc. Sci. Med. 2007, 65, 1695–1707. [Google Scholar] [CrossRef]
- ECDC. Surveillance of COVID-19 at Long-Term Care Facilities in the EU/EEA. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-long-term-care-facilities-surveillance-guidance.pdf (accessed on 20 July 2021).
- Ghiasi, A.; Weech-Maldonado, R.; Hearld, L.; Zengul, F.; Rsulnia, M.; Hood, A.; Puro, N. The Moderating Effect of Environmental Instability on the Hospital Strategy-Financial Performance Relationship. J. Health Care Financ. 2019, Fall, 1–18. [Google Scholar]
- Kumar, K.; Subramanian, R. Porters Strategic Types: Differences In Internal Processes and Their Impact on Performance. J. Appl. Bus. Res. (JABR) 1998, 14, 107–124. [Google Scholar] [CrossRef] [Green Version]
- Landry, A.Y.; Hernandez, S.R.; Shewchuk, R.M.; Garman, A.N. A configurational view of executive selection behaviours: A taxonomy of USA acute care hospitals. Health Serv. Manag. Res. 2010, 23, 128–138. [Google Scholar] [CrossRef]
- Ghiasi, A.; Zengul, F.D.; Ozaydin, B.; Oner, N.; Breland, B.K. The impact of hospital competition on strategies and outcomes of hospitals: A systematic review of the US hospitals 1996-2016. J. Health Care Financ. 2018, 44, 2. [Google Scholar]
- Topolyan, I.; Brasington, D.; Xu, X. Assessing the degree of competitiveness in the market for outpatient hospital services. J. Econ. Bus. 2019, 105, 105838. [Google Scholar] [CrossRef]
- Turoff, M.; Linstone, H.A. The Delphi Method-Techniques and Applications; Addison-Wesley: Reading, MA, USA, 2002. [Google Scholar]
- Wolf, L.A.; Delao, A.M. Establishing research priorities for the emergency severity index using a modified Delphi approach. J. Emerg. Nurs. 2021, 47, 50–57. [Google Scholar] [CrossRef] [PubMed]
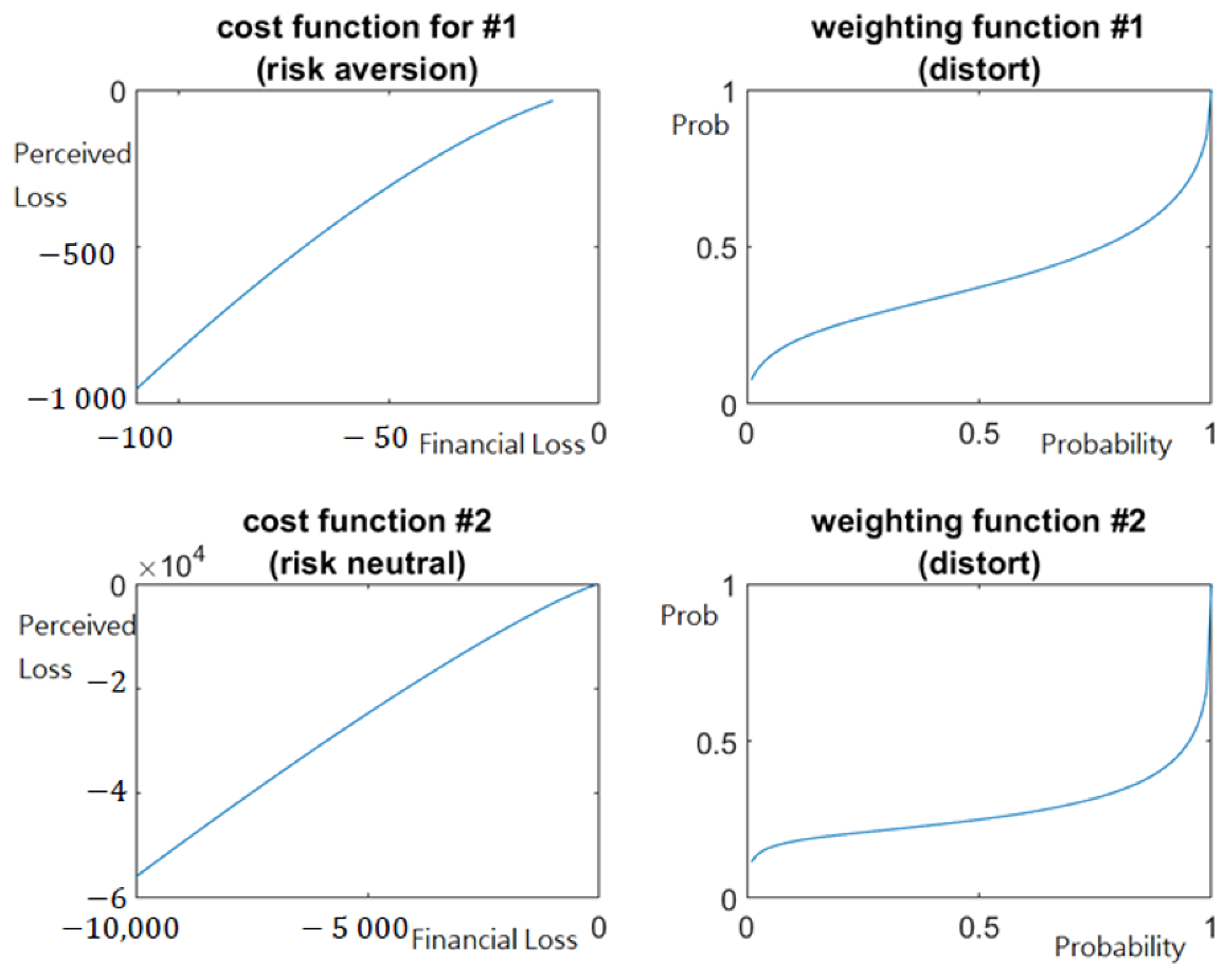
- Gonzalez, R.; Wu, G. On the shape of the probability weighting function. Cogn. Psychol. 1999, 38, 129–166. [Google Scholar] [CrossRef] [Green Version]
- Wu, G.; Gonzalez, R. Curvature of the probability weighting function. Manag. Sci. 1996, 42, 1676–1690. [Google Scholar] [CrossRef] [Green Version]
- Windrum, P. Third sector organizations and the co-production of health innovations. Manag. Decis. 2014, 52, 1046–1056. [Google Scholar] [CrossRef]

| Variables | Items | Frequency | Percent |
|---|---|---|---|
| Gender | Male | 123 | 37.6 |
| Female | 204 | 62.4 | |
| Job title | Facility administrator | 102 | 31.2 |
| Healthcare/Medical administrator | 225 | 68.8 | |
| Funding status | Public | 61 | 18.7 |
| For-profit | 266 | 81.3 | |
| LTCF type | General nursing homes | 61 | 18.7 |
| Residential homes | 102 | 31.2 | |
| Mixed LTCFs | 164 | 50.1 | |
| Facility scale | Less than 99 beds | 82 | 25.1 |
| 100~399 beds | 164 | 50.1 | |
| More than 400 beds | 81 | 24.8 |
| Estimated Parameter | Mean | Standard Deviation | MC_Error | Val2.5pc | Median | Val97.5pc | Start | Sample |
|---|---|---|---|---|---|---|---|---|
| 1.091 | 0.336 | 0.010 | 0.510 | 1.255 | 1.388 | 6001 | 320,000 | |
| [Task 1] | 1.433 | 0.802 | 0.024 | 0.937 | 0.980 | 2.879 | 6001 | 320,000 |
| [Task 2] | 1.176 | 0.361 | 0.014 | 0.933 | 0.977 | 1.816 | 6001 | 320,000 |
| [Task 1] | 0.525 | 0.265 | 0.008 | 0.363 | 0.375 | 0.988 | 6001 | 320,000 |
| [Task 2] | 0.382 | 0.045 | 0.001 | 0.351 | 0.356 | 0.462 | 6001 | 320,000 |
| 6001 | 320,000 |
| Estimated Parameter | Gender | Job Title | Funding Status | LTCF Type | Facility Scale | Strategy Type | |
|---|---|---|---|---|---|---|---|
| 0.9 | 0.14 | −0.27 | −0.03 | −0.06 * | 0.1 * | −0.03 ** | |
| 0.9 | 0.09 * | −0.16 ** | −0.27 * | −0.03 * | 0.05 * | 0.14 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, T. Perception Bias Effects on Healthcare Management in COVID-19 Pandemic: An Application of Cumulative Prospect Theory. Healthcare 2022, 10, 226. https://doi.org/10.3390/healthcare10020226
Wu T. Perception Bias Effects on Healthcare Management in COVID-19 Pandemic: An Application of Cumulative Prospect Theory. Healthcare. 2022; 10(2):226. https://doi.org/10.3390/healthcare10020226
Chicago/Turabian StyleWu, Tienhua. 2022. "Perception Bias Effects on Healthcare Management in COVID-19 Pandemic: An Application of Cumulative Prospect Theory" Healthcare 10, no. 2: 226. https://doi.org/10.3390/healthcare10020226
APA StyleWu, T. (2022). Perception Bias Effects on Healthcare Management in COVID-19 Pandemic: An Application of Cumulative Prospect Theory. Healthcare, 10(2), 226. https://doi.org/10.3390/healthcare10020226






