Efficacy of Different Dosing Regimens of IgE Targeted Biologic Omalizumab for Chronic Spontaneous Urticaria in Adult and Pediatric Populations: A Meta-Analysis
Abstract
1. Introduction
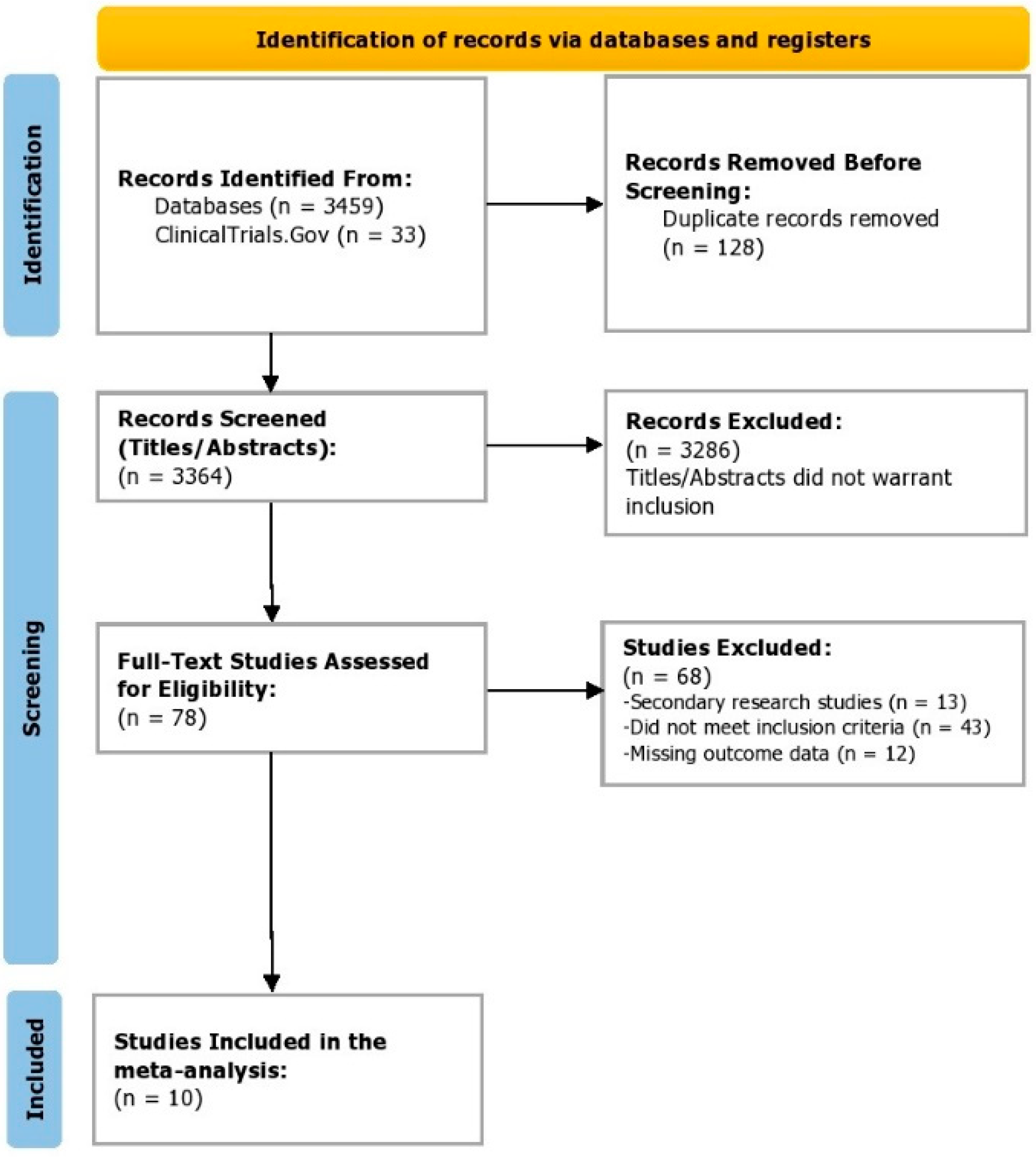
2. Materials and Methods
2.1. Search Strategy and Inclusion Criteria
2.2. Data Extraction (Selection and Coding)
2.3. Data Analysis
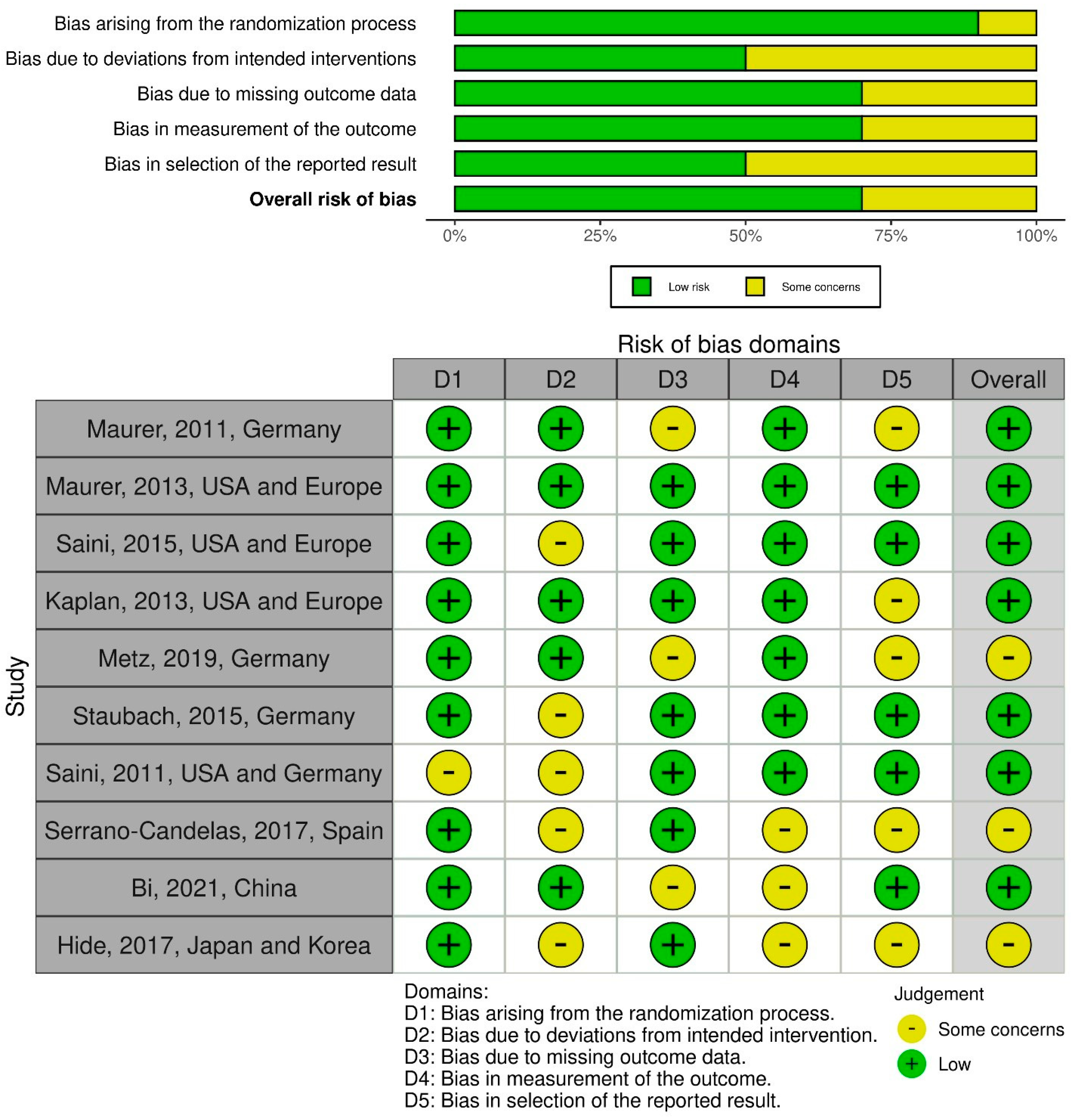
2.4. Risk of Bias (Quality) Assessment
2.5. Protocol Registration and Funding Role
3. Results
3.1. Overview of the Included Studies
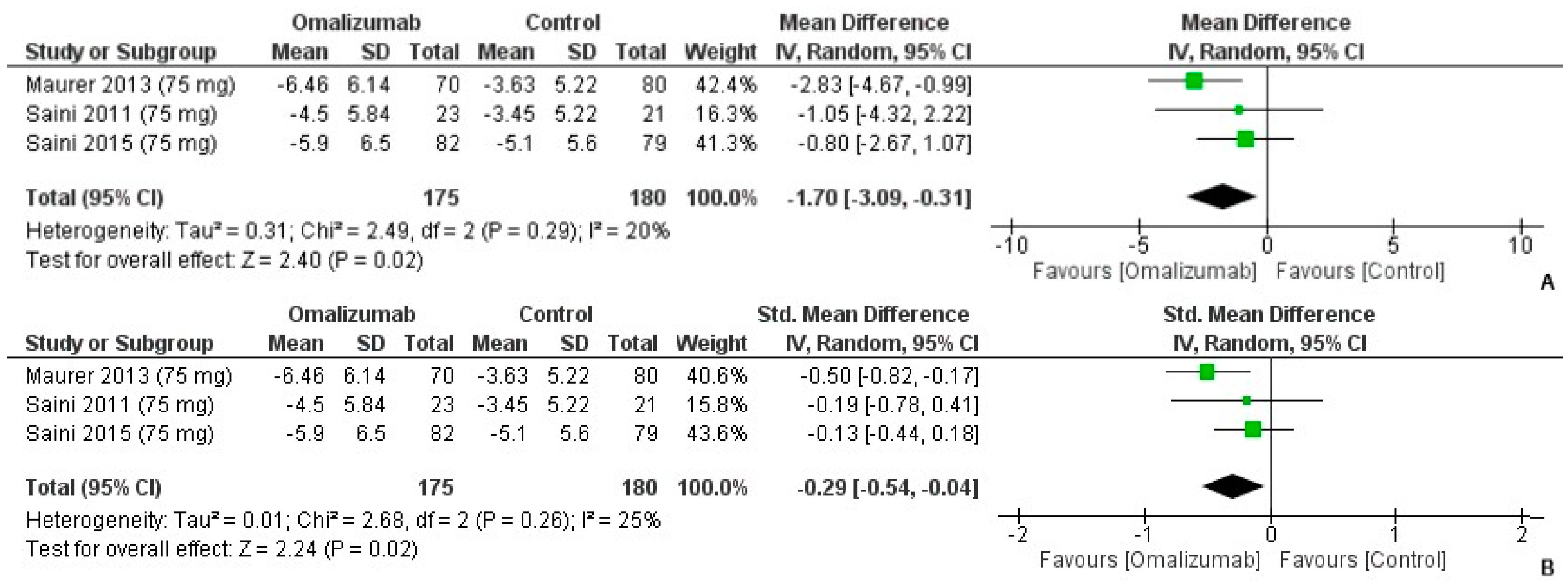
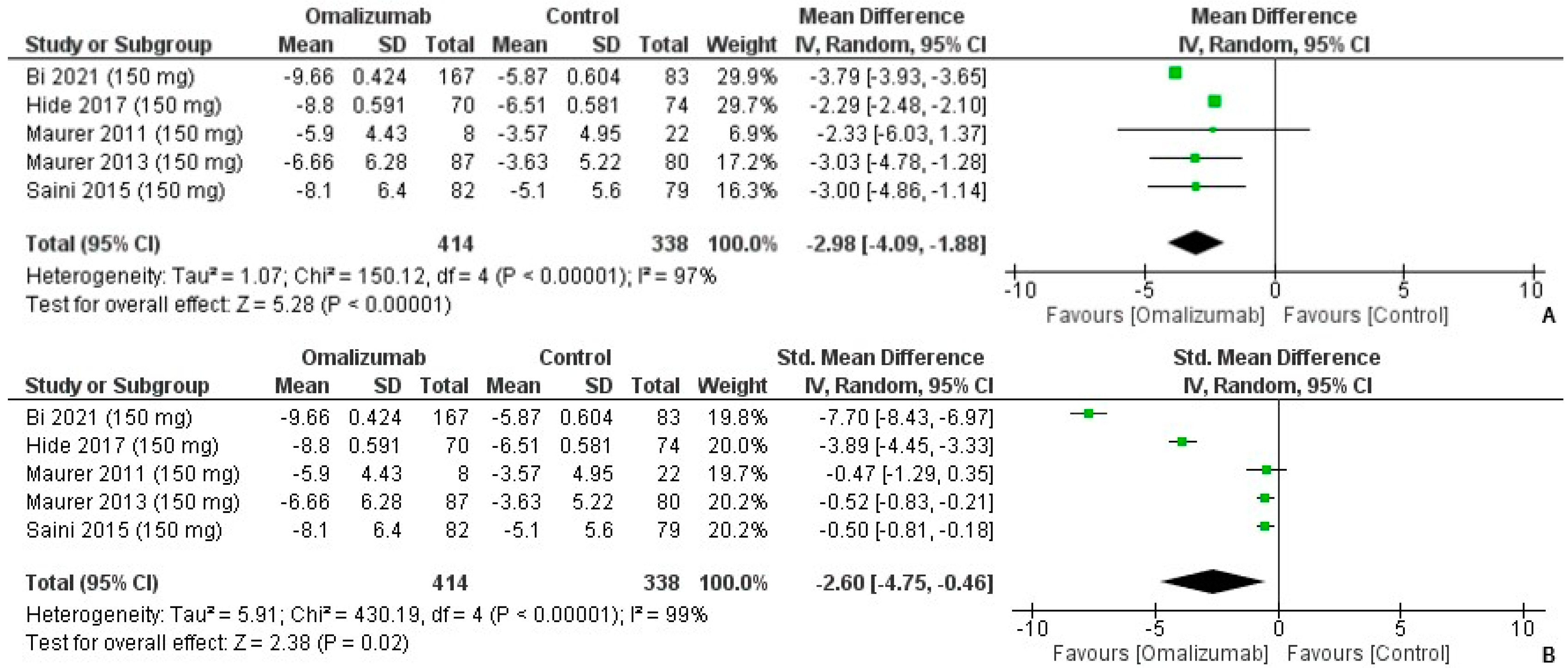
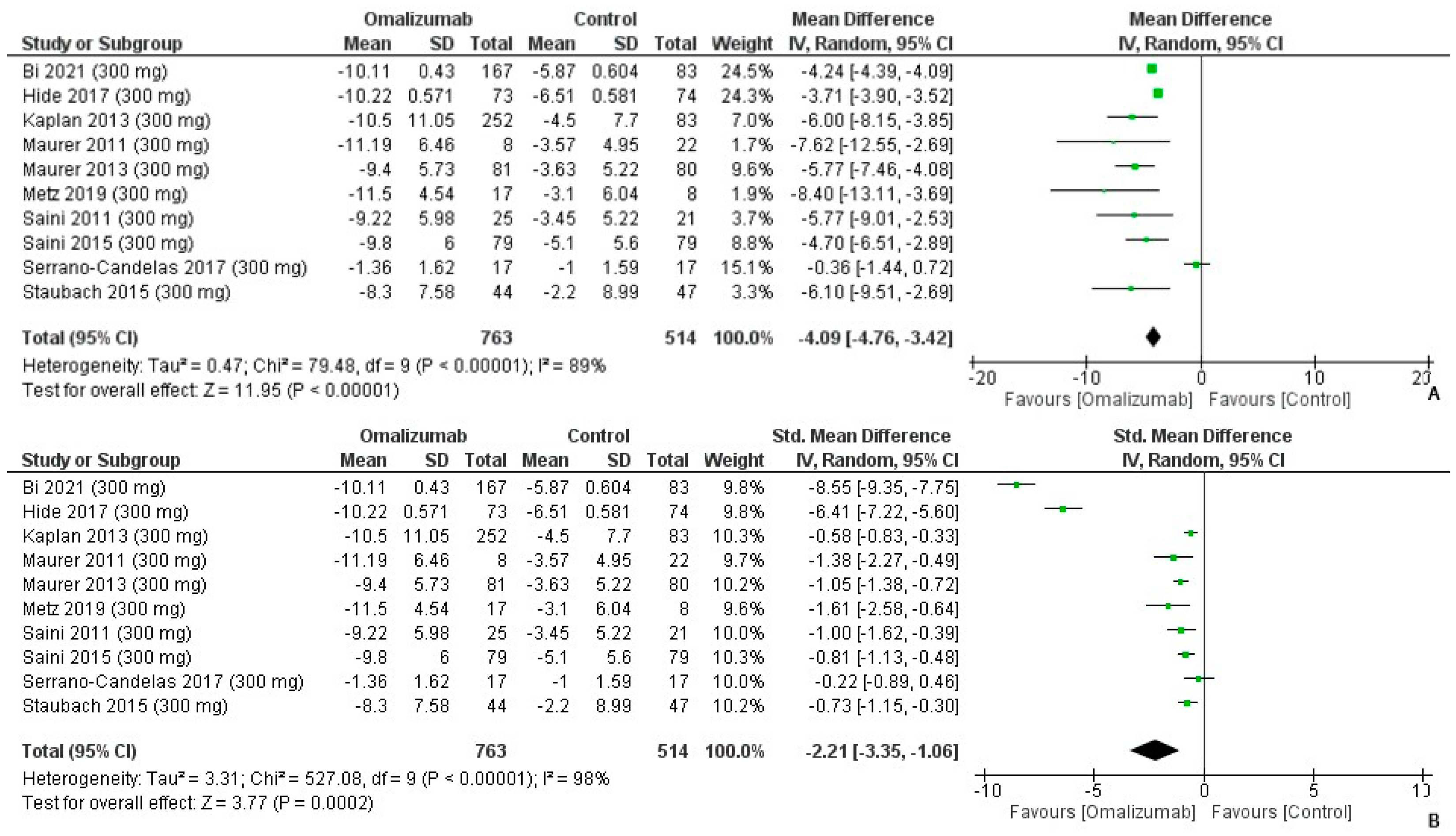
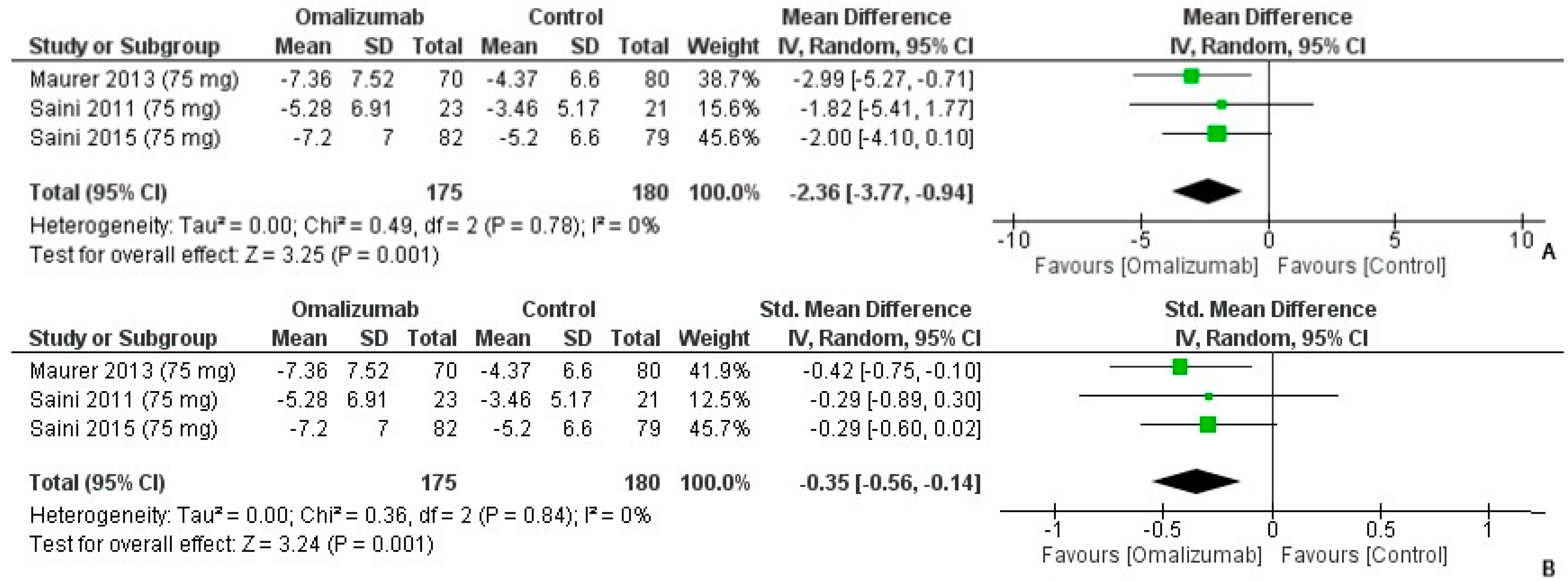
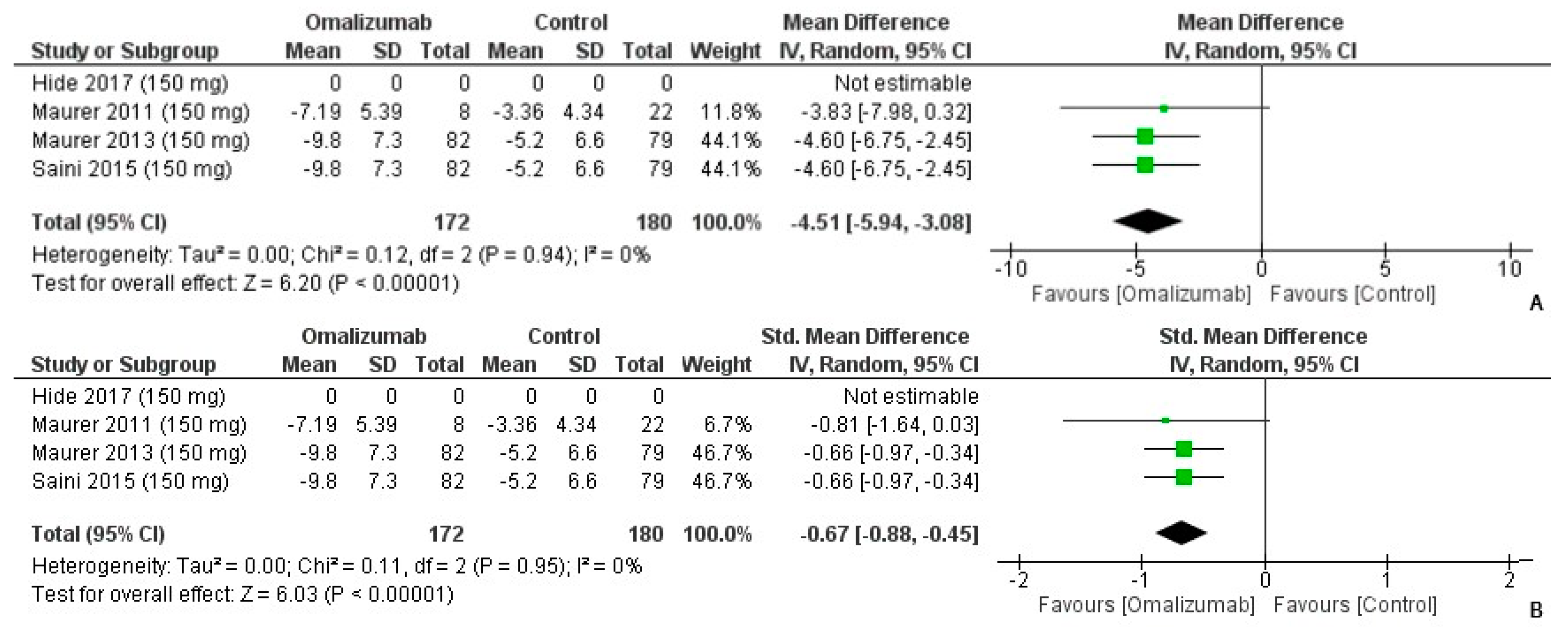
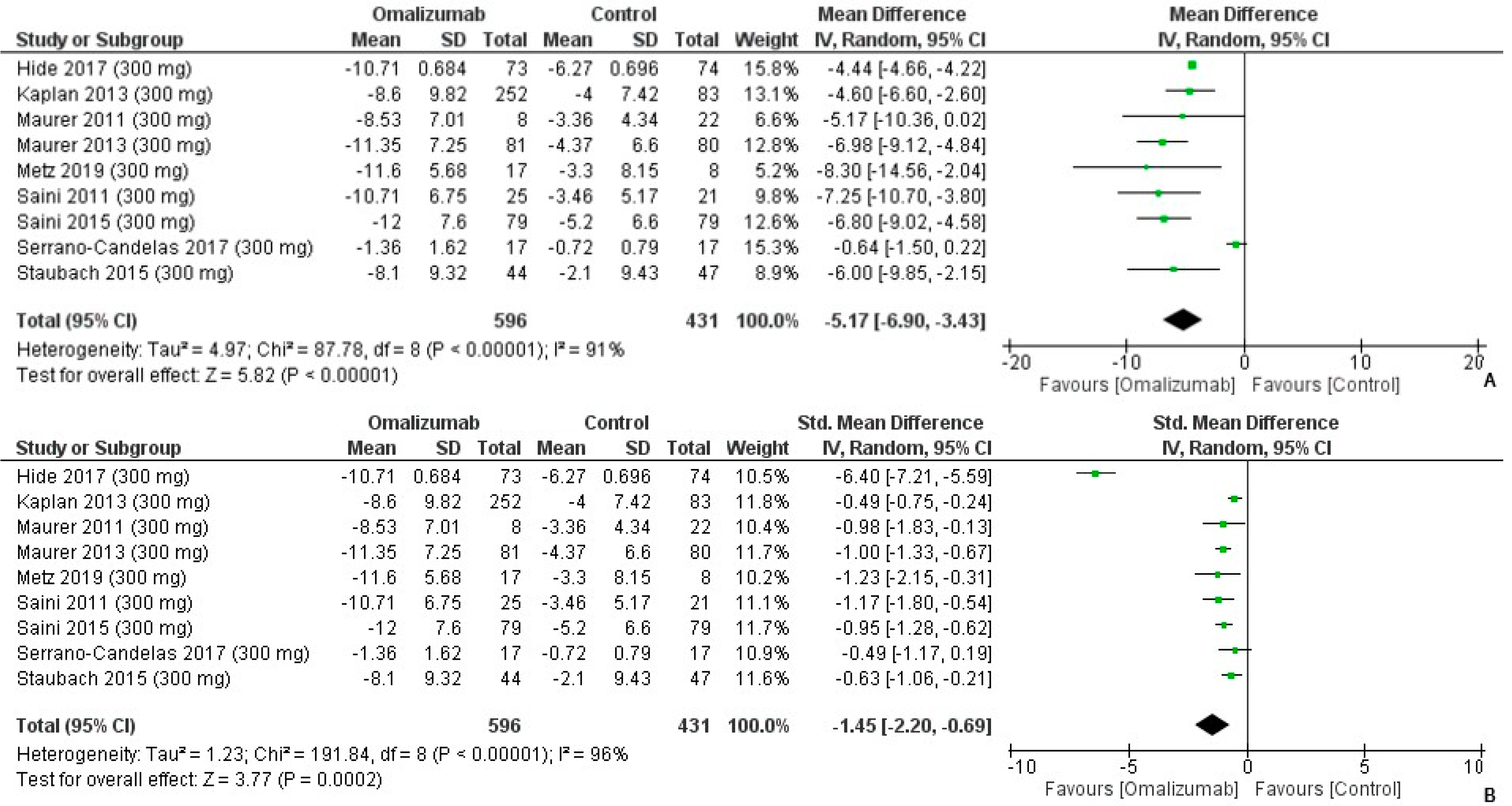
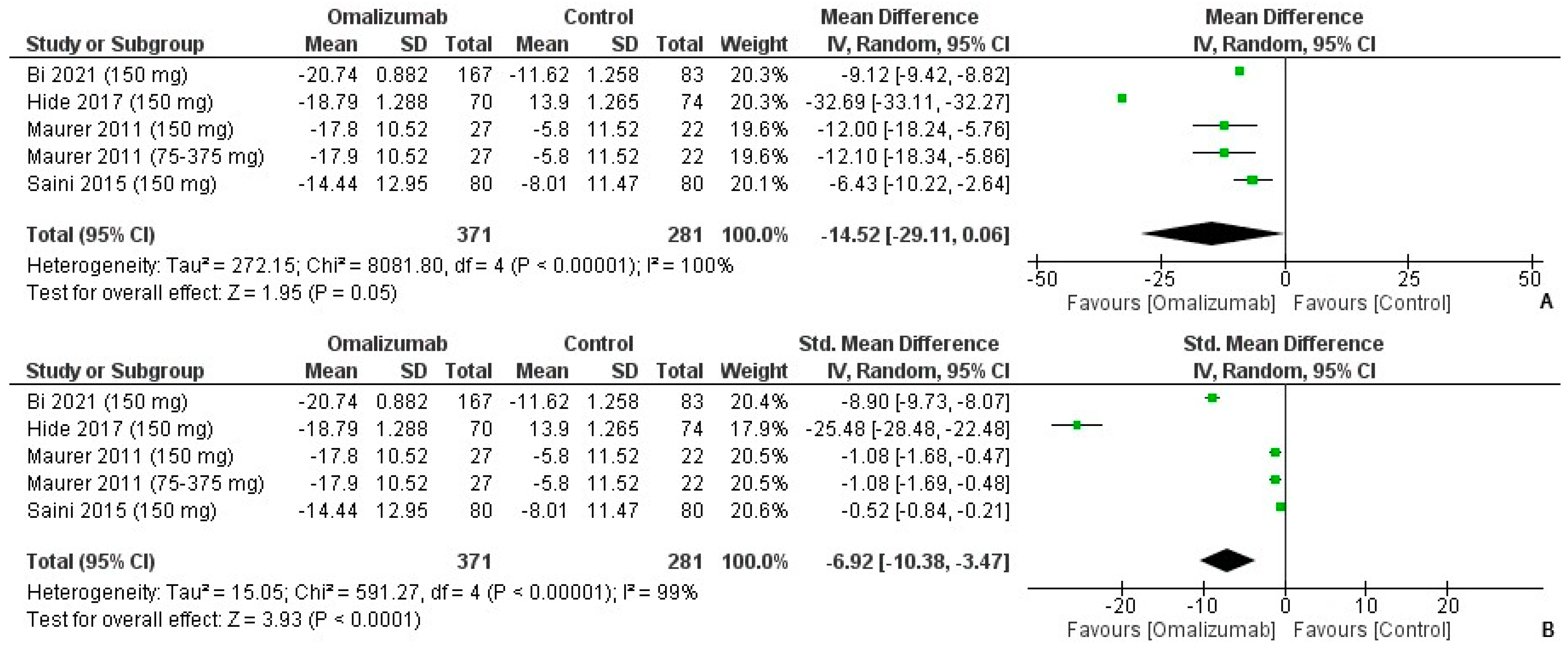
3.2. Weekly Itch Score Outcomes
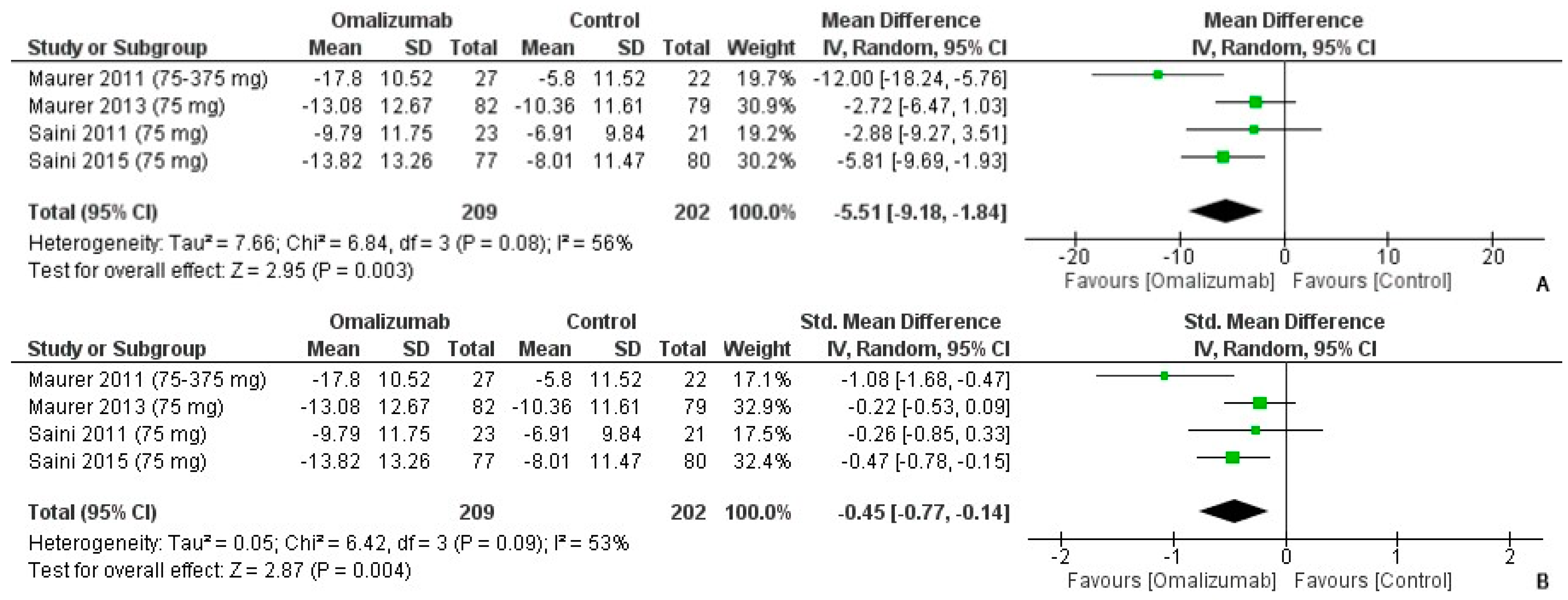
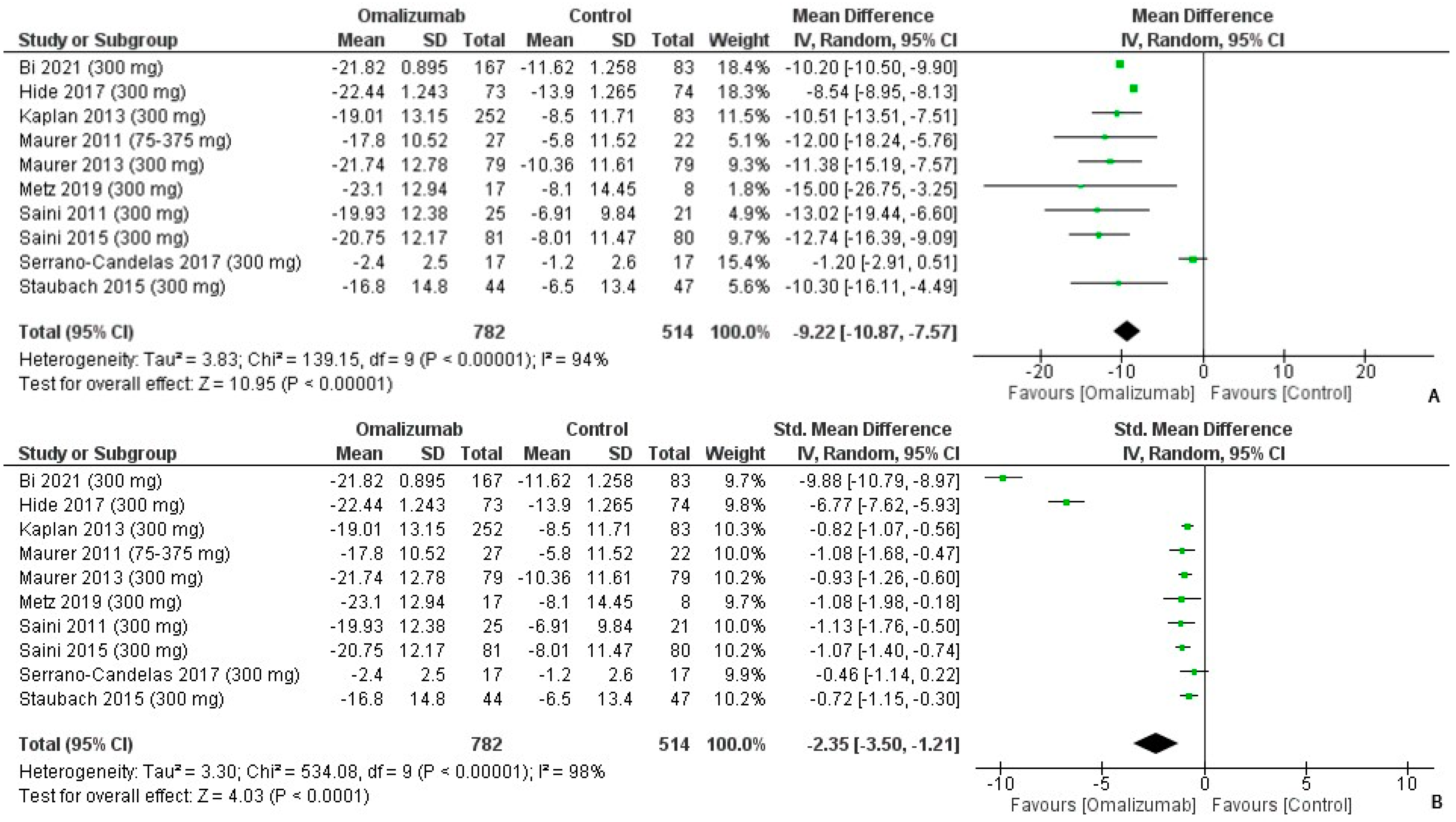
3.3. Weekly Wheal Score Outcomes
3.4. Urticaria Assessment Score 7 (UAS7) Outcomes
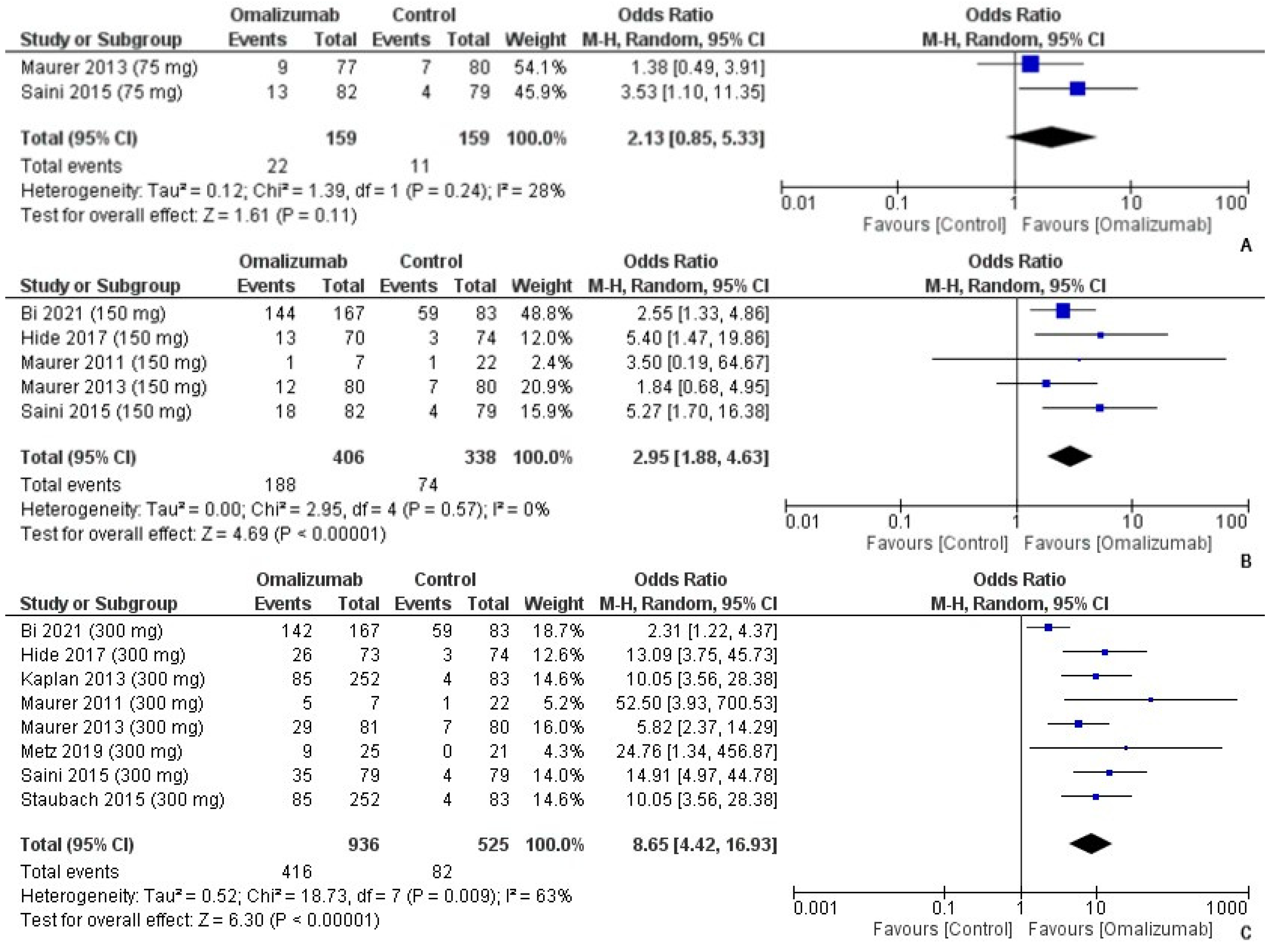
3.5. “Responders” to Omalizumab Treatment
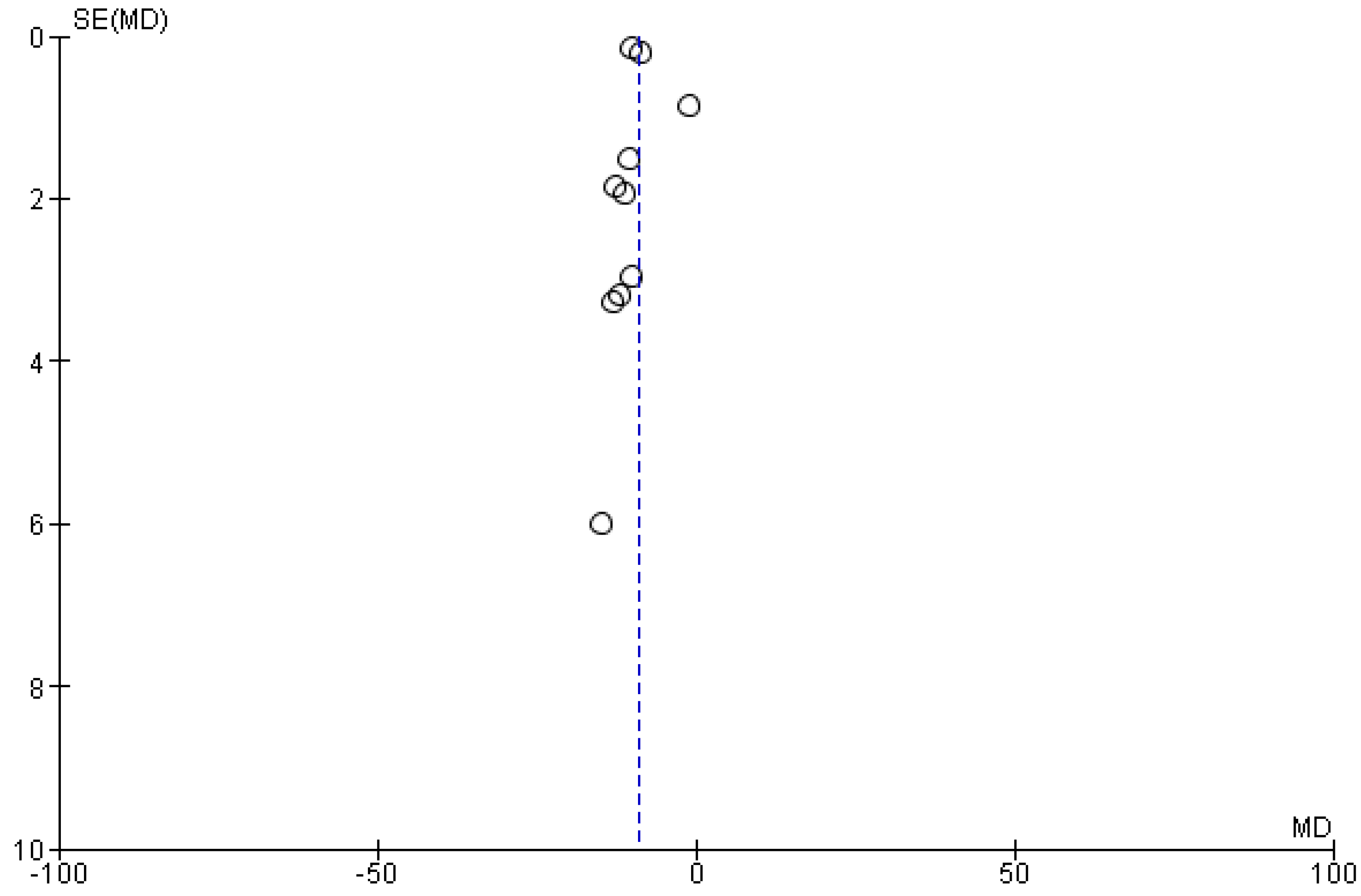
3.6. Funnel Plot and Risk of Bias Synthesis
4. Discussion
4.1. Strengths and Limitations
4.2. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zuberbier, T.; Balke, M.; Worm, M.; Edenharter, G.; Maurer, M. Epidemiology of Urticaria: A Representative Cross-sectional Population Survey. Clin. Exp. Dermatol. Clin. Dermatol. 2010, 35, 869–873. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Borges, M.; Ansotegui, I.J.; Baiardini, I.; Bernstein, J.; Canonica, G.W.; Ebisawa, M.; Gomez, M.; Gonzalez-Diaz, S.N.; Martin, B.; Morais-Almeida, M. The Challenges of Chronic Urticaria Part 1: Epidemiology, Immunopathogenesis, Comorbidities, Quality of Life, and Management. World Allergy Organ. J. 2021, 14, 100533. [Google Scholar] [CrossRef] [PubMed]
- Stepaniuk, P.; Kan, M.; Kanani, A. Natural History, Prognostic Factors and Patient Perceived Response to Treatment in Chronic Spontaneous Urticaria. Allergy Asthma Clin. Immunol. 2020, 16, 63. [Google Scholar] [CrossRef]
- Wertenteil, S.; Strunk, A.; Garg, A. Prevalence Estimates for Chronic Urticaria in the United States: A Sex-and Age-Adjusted Population Analysis. J. Am. Acad. Dermatol. 2019, 81, 152–156. [Google Scholar] [CrossRef]
- Bracken, S.J.; Abraham, S.; MacLeod, A.S. Autoimmune Theories of Chronic Spontaneous Urticaria. Front. Immunol. 2019, 10, 627. [Google Scholar] [CrossRef] [PubMed]
- Ruggeri, R.M.; Imbesi, S.; Saitta, S.; Campennì, A.; Cannavò, S.; Trimarchi, F.; Gangemi, S. Chronic Idiopathic Urticaria and Graves’ Disease. J. Endocrinol. Investig. 2013, 36, 531–536. [Google Scholar]
- Greenberger, P.A. Chronic Urticaria: New Management Options. World Allergy Organ. J. 2014, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, A.P. Treatment of Chronic Spontaneous Urticaria. Allergy Asthma Immunol. Res. 2012, 4, 326–331. [Google Scholar] [CrossRef]
- Schocket, A.L. Chronic Urticaria: Pathophysiology and Etiology, or the What and Why. In Allergy and Asthma Proceedings; OceanSide Publications, Inc.: Providence, RI, USA, 2006; Volume 27, pp. 90–95. [Google Scholar]
- Konstantinou, G.N.; Asero, R.; Ferrer, M.; Knol, E.F.; Maurer, M.; Raap, U.; Schmid-Grendelmeier, P.; Skol, P.S.; Grattan, C.E.H. EAACI Taskforce Position Paper: Evidence for Autoimmune Urticaria and Proposal for Defining Diagnostic Criteria. Allergy 2013, 68, 27–36. [Google Scholar] [CrossRef]
- Altrichter, S.; Peter, H.-J.; Pisarevskaja, D.; Metz, M.; Martus, P.; Maurer, M. IgE Mediated Autoallergy against Thyroid Peroxidase–a Novel Pathomechanism of Chronic Spontaneous Urticaria? PLoS ONE 2011, 6, e14794. [Google Scholar] [CrossRef]
- Hide, M.; Francis, D.M.; Grattan, C.; Hakimi, J.; Kochan, J.P.; Greaves, M.W. Autoantibodies against the High-Affinity IgE Receptor as a Cause of Histamine Release in Chronic Urticaria. N. Engl. J. Med. 1993, 328, 1599–1604. [Google Scholar] [CrossRef] [PubMed]
- Navinés-Ferrer, A.; Serrano-Candelas, E.; Molina-Molina, G.-J.; Martín, M. IgE-Related Chronic Diseases and Anti-IgE-Based Treatments. J. Immunol. Res. 2016, 2016, 8163803. [Google Scholar] [CrossRef] [PubMed]
- Djukanovic, R.; Wilson, S.J.; Kraft, M.; Jarjour, N.N.; Steel, M.; Chung, K.F.; Bao, W.; Fowler-Taylor, A.; Matthews, J.; Busse, W.W. Effects of Treatment with Anti-Immunoglobulin E Antibody Omalizumab on Airway Inflammation in Allergic Asthma. Am. J. Respir. Crit. Care Med. 2004, 170, 583–593. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Candelas, E.; Martinez-Aranguren, R.; Valero, A.; Bartra, J.; Gastaminza, G.; Goikoetxea, M.J.; Martín, M.; Ferrer, M. Comparable Actions of Omalizumab on Mast Cells and Basophils. Clin. Exp. Allergy 2016, 46, 92–102. [Google Scholar] [CrossRef]
- Kaplan, A.P. Therapy of Chronic Urticaria: A Simple, Modern Approach. Ann. Allergy Asthma Immunol. 2014, 112, 419–425. [Google Scholar] [CrossRef]
- Maurer, M.; Altrichter, S.; Bieber, T.; Biedermann, T.; Bräutigam, M.; Seyfried, S.; Brehler, R.; Grabbe, J.; Hunzelmann, N.; Jakob, T. Efficacy and Safety of Omalizumab in Patients with Chronic Urticaria Who Exhibit IgE against Thyroperoxidase. J. Allergy Clin. Immunol. 2011, 128, 202–209. [Google Scholar] [CrossRef]
- Maurer, M.; Rosén, K.; Hsieh, H.-J.; Saini, S.; Grattan, C.; Gimenéz-Arnau, A.; Agarwal, S.; Doyle, R.; Canvin, J.; Kaplan, A. Omalizumab for the Treatment of Chronic Idiopathic or Spontaneous Urticaria. N. Engl. J. Med. 2013, 368, 924–935. [Google Scholar] [CrossRef]
- Saini, S.S.; Bindslev-Jensen, C.; Maurer, M.; Grob, J.-J.; Baskan, E.B.; Bradley, M.S.; Canvin, J.; Rahmaoui, A.; Georgiou, P.; Alpan, O. Efficacy and Safety of Omalizumab in Patients with Chronic Idiopathic/Spontaneous Urticaria Who Remain Symptomatic on H1 Antihistamines: A Randomized, Placebo-Controlled Study. J. Investig. Dermatol. 2015, 135, 67–75. [Google Scholar] [CrossRef]
- Kaplan, A.; Ledford, D.; Ashby, M.; Canvin, J.; Zazzali, J.L.; Conner, E.; Veith, J.; Kamath, N.; Staubach, P.; Jakob, T. Omalizumab in Patients with Symptomatic Chronic Idiopathic/Spontaneous Urticaria despite Standard Combination Therapy. J. Allergy Clin. Immunol. 2013, 132, 101–109. [Google Scholar] [CrossRef]
- Metz, M.; Torene, R.; Kaiser, S.; Beste, M.T.; Staubach, P.; Bauer, A.; Brehler, R.; Gericke, J.; Letzkus, M.; Hartmann, N. Omalizumab Normalizes the Gene Expression Signature of Lesional Skin in Patients with Chronic Spontaneous Urticaria: A Randomized, Double-blind, Placebo-controlled Study. Allergy 2019, 74, 141–151. [Google Scholar] [CrossRef]
- Staubach, P.; Metz, M.; Chapman-Rothe, N.; Sieder, C.; Bräutigam, M.; Maurer, M.; Weller, K. Omalizumab Rapidly Improves Angioedema-related Quality of Life in Adult Patients with Chronic Spontaneous Urticaria: X-ACT Study Data. Allergy 2018, 73, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Saini, S.; Rosen, K.E.; Hsieh, H.-J.; Wong, D.A.; Conner, E.; Kaplan, A.; Spector, S.; Maurer, M. A Randomized, Placebo-Controlled, Dose-Ranging Study of Single-Dose Omalizumab in Patients with H1-Antihistamine–Refractory Chronic Idiopathic Urticaria. J. Allergy Clin. Immunol. 2011, 128, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Candelas, E.; Martínez-Aranguren, R.; Vega, O.; Gastaminza, G.; Bartra, J.; Audicana, M.T.; Núñez-Córdoba, J.M.; Algorta, J.; Valero, A.; Martin, M. Omalizumab Efficacy in Cases of Chronic Spontaneous Urticaria Is Not Explained by the Inhibition of Sera Activity in Effector Cells. Sci. Rep. 2017, 7, 8985. [Google Scholar] [CrossRef]
- Bi, X.-D.; Lu, B.-Z.; Pan, X.-X.; Liu, S.; Wang, J.-Y. Adjunct Therapy with Probiotics for Chronic Urticaria in Children: Randomised Placebo-Controlled Trial. Allergy Asthma Clin. Immunol. 2021, 17, 39. [Google Scholar] [CrossRef]
- Hide, M.; Park, H.-S.; Igarashi, A.; Ye, Y.-M.; Kim, T.-B.; Yagami, A.; Roh, J.; Lee, J.-H.; Chinuki, Y.; Youn, S.W. Efficacy and Safety of Omalizumab in Japanese and Korean Patients with Refractory Chronic Spontaneous Urticaria. J. Dermatol. Sci. 2017, 87, 70–78. [Google Scholar] [CrossRef]
- Tharp, M.D.; Bernstein, J.A.; Kavati, A.; Ortiz, B.; MacDonald, K.; Denhaerynck, K.; Abraham, I.; Lee, C.S. Benefits and Harms of Omalizumab Treatment in Adolescent and Adult Patients with Chronic Idiopathic (Spontaneous) Urticaria: A Meta-Analysis of “Real-World” Evidence. JAMA Dermatol. 2019, 155, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Nochaiwong, S.; Chuamanochan, M.; Ruengorn, C.; Awiphan, R.; Tovanabutra, N.; Chiewchanvit, S. Evaluation of Pharmacologic Treatments for H1 Antihistamine–Refractory Chronic Spontaneous Urticaria: A Systematic Review and Network Meta-Analysis. JAMA Dermatol. 2021, 157, 1316–1327. [Google Scholar] [CrossRef]
- Maurer, M.; Khan, D.A.; Komi, D.E.A.; Kaplan, A.P. Biologics for the Use in Chronic Spontaneous Urticaria: When and Which. J. Allergy Clin. Immunol. Pract. 2021, 9, 1067–1078. [Google Scholar] [CrossRef]
- Zhao, Z.-T.; Ji, C.-M.; Yu, W.-J.; Meng, L.; Hawro, T.; Wei, J.-F.; Maurer, M. Omalizumab for the Treatment of Chronic Spontaneous Urticaria: A Meta-Analysis of Randomized Clinical Trials. J. Allergy Clin. Immunol. 2016, 137, 1742–1750. [Google Scholar] [CrossRef]
- Rubini, N.P.M.; Ensina, L.F.C.; Silva, E.M.K.; Sano, F.; Solé, D. Effectiveness and Safety of Omalizumab in the Treatment of Chronic Spontaneous Urticaria: Systematic Review and Meta-Analysis. Allergol. Immunopathol. 2019, 47, 515–522. [Google Scholar] [CrossRef]
- Agache, I.; Akdis, C.A.; Akdis, M.; Brockow, K.; Chivato, T.; Del Giacco, S.; Eiwegger, T.; Eyerich, K.; Giménez-Arnau, A.; Gutermuth, J. EAACI Biologicals Guidelines—Omalizumab for the Treatment of Chronic Spontaneous Urticaria in Adults and in the Paediatric Population 12–17 Years Old. Allergy 2022, 77, 17–38. [Google Scholar] [CrossRef] [PubMed]
- Hawro, T.; Ohanyan, T.; Schoepke, N.; Metz, M.; Peveling-Oberhag, A.; Staubach, P.; Maurer, M.; Weller, K. The Urticaria Activity Score—Validity, Reliability, and Responsiveness. J. Allergy Clin. Immunol. Pract. 2018, 6, 1185–1190. [Google Scholar] [CrossRef] [PubMed]
- Zuberbier, T.; Aberer, W.; Asero, R.; Bindslev-Jensen, C.; Brzoza, Z.; Canonica, G.W.; Church, M.K.; Ensina, L.F.; Giménez-Arnau, A.; Godse, K. The EAACI/GA 2 LEN/EDF/WAO Guideline for the Definition, Classification, Diagnosis, and Management of Urticaria: The 2013 Revision and Update. Allergy 2014, 69, 868–887. [Google Scholar] [CrossRef]
- Zuberbier, T.; Abdul Latiff, A.H.; Abuzakouk, M.; Aquilina, S.; Asero, R.; Baker, D.; Ballmer-Weber, B.; Bangert, C.; Ben-Shoshan, M.; Bernstein, J.A. The International EAACI/GA2LEN/EuroGuiDerm/APAAACI Guideline for the Definition, Classification, Diagnosis, and Management of Urticaria. Allergy 2022, 77, 734–766. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, M.; Boccon-Gibod, I.; Gonçalo, M.; İnalöz, H.S.; Knulst, A.; Lapeere, H.; Parthasaradhi, A.; Stingl, G.; Tagka, A.; Valenzuela, F. Expert Opinion: Defining Response to Omalizumab in Patients with Chronic Spontaneous Urticaria. Eur. J. Dermatol. 2017, 27, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Boesel, K.M.; Griffith, D.T.; Prussin, C.; Foster, B.; Romero, F.A.; Townley, R.; Casale, T.B. Omalizumab Rapidly Decreases Nasal Allergic Response and FcεRI on Basophils. J. Allergy Clin. Immunol. 2004, 113, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Sposato, B.; Scalese, M.; Latorre, M.; Novelli, F.; Scichilone, N.; Milanese, M.; Olivieri, C.; Perrella, A.; Paggiaro, P.; Xolair Italian Study Group. Can the Response to Omalizumab Be Influenced by Treatment Duration? A Real-Life Study. Pulm. Pharmacol. Ther. 2017, 44, 38–45. [Google Scholar] [CrossRef]
- Metz, M.; Ohanyan, T.; Church, M.K.; Maurer, M. Omalizumab Is an Effective and Rapidly Acting Therapy in Difficult-to-Treat Chronic Urticaria: A Retrospective Clinical Analysis. J. Dermatol. Sci. 2014, 73, 57–62. [Google Scholar] [CrossRef]
- MacGlashan, D.W.; Bochner, B.S.; Adelman, D.C.; Jardieu, P.M.; Togias, A.; McKenzie-White, J.; Sterbinsky, S.A.; Hamilton, R.G.; Lichtenstein, L.M. Down-Regulation of Fc (Epsilon) RI Expression on Human Basophils during in Vivo Treatment of Atopic Patients with Anti-IgE Antibody. J. Immunol. 1997, 158, 1438–1445. [Google Scholar]
- Grieco, T.; Porzia, A.; Paolino, G.; Chello, C.; Sernicola, A.; Faina, V.; Carnicelli, G.; Moliterni, E.; Mainiero, F. IFN-γ/IL-6 and Related Cytokines in Chronic Spontaneous Urticaria: Evaluation of Their Pathogenetic Role and Changes during Omalizumab Therapy. Int. J. Dermatol. 2020, 59, 590–594. [Google Scholar] [CrossRef]
- Kolkhir, P.; Church, M.K.; Weller, K.; Metz, M.; Schmetzer, O.; Maurer, M. Autoimmune Chronic Spontaneous Urticaria: What We Know and What We Do Not Know. J. Allergy Clin. Immunol. 2017, 139, 1772–1781. [Google Scholar] [CrossRef] [PubMed]
- De Montjoye, L.; Darrigade, A.-S.; Giménez-Arnau, A.; Herman, A.; Dumoutier, L.; Baeck, M. Correlations between Disease Activity, Autoimmunity and Biological Parameters in Patients with Chronic Spontaneous Urticaria. Eur. Ann. Allergy Clin. Immunol. 2020, 53, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Schoepke, N.; Asero, R.; Ellrich, A.; Ferrer, M.; Gimenez-Arnau, A.; EH Grattan, C.; Jakob, T.; Konstantinou, G.N.; Raap, U.; Skov, P.S. Biomarkers and Clinical Characteristics of Autoimmune Chronic Spontaneous Urticaria: Results of the PURIST Study. Allergy 2019, 74, 2427–2436. [Google Scholar] [CrossRef] [PubMed]
- Antia, C.; Baquerizo, K.; Korman, A.; Alikhan, A.; Bernstein, J.A. Urticaria: A Comprehensive Review: Treatment of Chronic Urticaria, Special Populations, and Disease Outcomes. J. Am. Acad. Dermatol. 2018, 79, 617–633. [Google Scholar] [CrossRef] [PubMed]
- Shahzad Mustafa, S.; Sánchez-Borges, M. Chronic Urticaria: Comparisons of US, European, and Asian Guidelines. Curr. Allergy Asthma Rep. 2018, 18, 36. [Google Scholar] [CrossRef] [PubMed]
- Gaig, P.; Olona, M.; Lejarazu, D.M.; Caballero, M.T.; Domínguez, F.J.; Echechipia, S.; Abujeta, J.L.G.; Gonzalez, M.A.; Lleonart, R.; Cócera, C.M. Epiodemiology of Urticaria in Spain. J. Investig. Allergol. Clin. Immunol. 2004, 14, 214–220. [Google Scholar]
- Yu, M.; Maurer, M.; Chen, Y.; Zhao, Z. Omalizumab in Chronic Inducible Urticaria: A Real-Life Study of Efficacy, Safety, Predictors of Treatment Outcome, Time to Response and Relapse. J. Allergy Clin. Immunol. 2021, 147, AB26. [Google Scholar] [CrossRef]
- Maurer, M.; Metz, M.; Brehler, R.; Hillen, U.; Jakob, T.; Mahler, V.; Pföhler, C.; Staubach, P.; Treudler, R.; Wedi, B. Omalizumab Treatment in Patients with Chronic Inducible Urticaria: A Systematic Review of Published Evidence. J. Allergy Clin. Immunol. 2018, 141, 638–649. [Google Scholar] [CrossRef]
- Kocatürk, E.; Can, P.K.; Akbas, P.E.; Copur, M.; Degirmentepe, E.N.; Kızıltac, K.; Singer, R. Management of Chronic Inducible Urticaria According to the Guidelines: A Prospective Controlled Study. J. Dermatol. Sci. 2017, 87, 60–69. [Google Scholar] [CrossRef]
- Damiani, G.; Diani, M.; Conic, R.R.Z.; Colli, L.; Ferrucci, S.; Martina, E.; Offidani, A.M.; Pigatto, P.D.M. Omalizumab in Chronic Urticaria: An Italian Survey. Int. Arch. Allergy Immunol. 2019, 178, 45–49. [Google Scholar] [CrossRef]
- Bernstein, J.A.; Kavati, A.; Tharp, M.D.; Ortiz, B.; MacDonald, K.; Denhaerynck, K.; Abraham, I. Effectiveness of Omalizumab in Adolescent and Adult Patients with Chronic Idiopathic/Spontaneous Urticaria: A Systematic Review of ‘Real-World’Evidence. Expert Opin. Biol. Ther. 2018, 18, 425–448. [Google Scholar] [CrossRef] [PubMed]
- Dwan, K.; Altman, D.G.; Arnaiz, J.A.; Bloom, J.; Chan, A.-W.; Cronin, E.; Decullier, E.; Easterbrook, P.J.; Von Elm, E.; Gamble, C. Systematic Review of the Empirical Evidence of Study Publication Bias and Outcome Reporting Bias. PLoS ONE 2008, 3, e3081. [Google Scholar] [CrossRef] [PubMed]
- Hollis, K.; Proctor, C.; McBride, D.; Balp, M.-M.; McLeod, L.; Hunter, S.; Tian, H.; Khalil, S.; Maurer, M. Comparison of Urticaria Activity Score over 7 Days (UAS7) Values Obtained from Once-Daily and Twice-Daily Versions: Results from the ASSURE-CSU Study. Am. J. Clin. Dermatol. 2018, 19, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, A.P.; Giménez-Arnau, A.M.; Saini, S.S. Mechanisms of Action That Contribute to Efficacy of Omalizumab in Chronic Spontaneous Urticaria. Allergy 2017, 72, 519–533. [Google Scholar] [CrossRef]
- Kuo, B.-S.; Li, C.-H.; Chen, J.-B.; Shiung, Y.-Y.; Chu, C.-Y.; Lee, C.-H.; Liu, Y.-J.; Kuo, J.-H.; Hsu, C.; Su, H.-W. IgE-Neutralizing UB-221 MAb, Distinct from Omalizumab and Ligelizumab, Exhibits CD23-Mediated IgE Downregulation and Relieves Urticaria Symptoms. J. Clin. Investig. 2022, 132, e157765. [Google Scholar] [CrossRef] [PubMed]
| ID, Name, Citation | Author, Year, Country | Dosage and Time Period | Inclusion | Mean Age | Females (IG vs. CG) | Race (IG vs. CG) |
|---|---|---|---|---|---|---|
| NCT00481676, XCUISITE [17] | Maurer, 2011, Germany | Omalizumab, 75 to 375 mg, subcutaneously every 2 or 4 weeks for 24 weeks for a total of 6–12 doses | Individuals between the ages of 18 and 70 years with moderate-to-severe CSU, detected with IgE autoantibodies against autoantigens, who had persistent symptoms (wheals and pruritus) despite standard antihistamine therapy ≥ 6 weeks | 40.5 | 19/27 (70.4%) vs. 19/22 (86.4%) | All White |
| NCT01292473, ASTERIA I [18] | Maurer, 2013, USA and Europe | Omalizumab 75 mg or 150 mg or 300 mg, subcutaneously every 4 weeks till 12 weeks for a total of 3 doses | Individuals between the ages of 12 and 75 years with moderate-to-severe CSU, who remained symptomatic despite H1-antihistamine therapy (licensed doses) ≥ 8 weeks | 42.5 ± 13.7 | 189/243 (77.8%) vs. 55/79 (70%) | White: 202/243 (83.1%) vs. 70/79 (89%) Non-White: 31/243 (12.8%) vs. 6/79 (8%) NA: 10/243 (4.1%) vs. 3/79 (4%) |
| NCT01287117, ASTERIA II [19] | Saini, 2015, USA and Europe | Omalizumab 75 mg or 150 mg or 300 mg, subcutaneously every 4 weeks till 24 weeks for a total of 6 doses | Individuals between the ages of 12–75 years with moderate-to-severe CSU who remained symptomatic despite H1-antihistamine therapy (licensed doses) | 41.15 | 179/238 (75.2%) vs. 52/80 (65%) | White: 199/238 (83.6%) vs. 64/80 (80%) Black: 23/238 (9.7%) vs. 10/80 (12.5%) Other: 16/238 (6.7%) vs. 6/80 (7.5%) |
| NCT01264939, GLACIAL [20] | Kaplan, 2013, USA and Europe | Omalizumab 300 mg subcutaneously every 4 weeks till 24 weeks for a total of 6 doses | Individuals aged 12 to 75 years old with moderate-to-severe CSU; itches and hives for more than 6 consecutive weeks before enrollment despite therapy with H1-antihistamines plus H2-antihistamines, LTRAs, or both; UAS7 ≥ 16 | 43.1 ± 14.1 | 186/252 (73.8%) vs. 55/83 (66.3%) | White: 223/252 (88.5%) vs. 75/83 (90.4%) |
| NCT01599637, MOA [21] | Metz, 2019, Germany | Omalizumab 300 mg, subcutaneously every 4 weeks till 12 weeks for a total of 3 doses | Individuals aged 18–75 years with moderate-to-severe CSU, who remained symptomatic despite H1-antihistamine treatment at approved doses, characterized by the re-occurrence of itch and hives ≥ 6 weeks before baseline; UAS7 ≥ 16; a CSU diagnosis > 6 months; be on an approved dose of an H1-antihistamine for CSU | 39.3 | 18/20 (90%) vs. 8/10 (80%) | All White |
| NCT01723072, X-ACT [22] | Staubach, 2015, Germany | Omalizumab 300 mg, subcutaneously every 4 weeks till 28 weeks for a total of 7 doses | Individuals aged 18–75 years with moderate-to-severe CSU with wheals; > 4 occurrences of angioedema in the last 6 months; symptomatic despite high-dose sg H1- antihistamine treatment (2–4 times the approved dose) | 42.9 ± 12.3 | 30/44 (68.2%) vs. 33/47 (70.2%) | White: 42/44 (95.5%) 46/47 (97.9%) Asian: 1/44 (2.3%) vs. 1/47 (2.1%) Other: 1/44 (2.3%) vs. 0/47 (0%) |
| NCT00130234, MYSTIQUE [23] | Saini, 2011, USA and Germany | Omalizumab 75, 300, or 600 mg subcutaneously for a total of 1 dose and followed for 24 weeks | Individuals aged 12 to 75 years with a history of moderate-to-severe CSU ≥ 3 months (pruritus and hives for >3 days in 7 days for >6 consecutive weeks) despite treatment with an approved dose of an H1-antihistamine | 40.8 | 44/69 (63.8%) vs. 17/21 (81%) | White: 57/69 (82.6%) vs. 18/21 (85.7%) Black/African American: 6/69 (8.7%) vs. 2/21 (9.5%) Asian: 4/69 (5.8%) vs. 1/21 (4.8%) American Indian or Alaska Native: 2/69 (2.9%) vs. 0/21 (0%) |
| NCT01713725 [24] | Serrano-Candelas, 2017, Spain | Omalizumab 300 mg, subcutaneously for 14 weeks, with 5 total doses | Individuals with CSU treated with omalizumab, representing a median disease duration of 6.7 years | 44 ± 12.2 | 8/17 (47.1%) vs. 14/22 (63.6%) | NR |
| NCT03328897 [25] | Bi, 2021, China | Omalizumab 150 or 300 mg, injected, every 4 weeks, with 3 total doses | Children aged 6–12 years with CSU, with symptoms at least twice or 2 days per week and duration of each attack within the last 24 h | 8.6 | 62/108 (57.4%) vs. 55/105 (52.4%) | NR |
| NCT02329223, POLARIS [26] | Hide, 2017, Japan and Korea | Omalizumab 150 or 300 mg subcutaneously every 4 weeks for 12 weeks, with 3 total doses | Individuals aged 12 to 75 years, with a CSU diagnosis for 6 months refractory to conventional H1AH at the time of randomization | 43.57 | 83/144 (57.6%) vs. 48/74 (64.9%) | Japanese: 69/144 (47.9%) vs. 36/74 (48.6%) Korean: 75/144 (52.1%) vs. 38/74 (51.4%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manzoor, H.; Razi, F.; Rasheed, A.; Sarfraz, Z.; Sarfraz, A.; Robles-Velasco, K.; Felix, M.; Cherrez-Ojeda, I. Efficacy of Different Dosing Regimens of IgE Targeted Biologic Omalizumab for Chronic Spontaneous Urticaria in Adult and Pediatric Populations: A Meta-Analysis. Healthcare 2022, 10, 2579. https://doi.org/10.3390/healthcare10122579
Manzoor H, Razi F, Rasheed A, Sarfraz Z, Sarfraz A, Robles-Velasco K, Felix M, Cherrez-Ojeda I. Efficacy of Different Dosing Regimens of IgE Targeted Biologic Omalizumab for Chronic Spontaneous Urticaria in Adult and Pediatric Populations: A Meta-Analysis. Healthcare. 2022; 10(12):2579. https://doi.org/10.3390/healthcare10122579
Chicago/Turabian StyleManzoor, Humayun, Foha Razi, Amina Rasheed, Zouina Sarfraz, Azza Sarfraz, Karla Robles-Velasco, Miguel Felix, and Ivan Cherrez-Ojeda. 2022. "Efficacy of Different Dosing Regimens of IgE Targeted Biologic Omalizumab for Chronic Spontaneous Urticaria in Adult and Pediatric Populations: A Meta-Analysis" Healthcare 10, no. 12: 2579. https://doi.org/10.3390/healthcare10122579
APA StyleManzoor, H., Razi, F., Rasheed, A., Sarfraz, Z., Sarfraz, A., Robles-Velasco, K., Felix, M., & Cherrez-Ojeda, I. (2022). Efficacy of Different Dosing Regimens of IgE Targeted Biologic Omalizumab for Chronic Spontaneous Urticaria in Adult and Pediatric Populations: A Meta-Analysis. Healthcare, 10(12), 2579. https://doi.org/10.3390/healthcare10122579






