Follow-Up Chest X-rays in Minor Chest Trauma with Fewer Than Three Rib Fractures: A Justifiable, Habitual Re-Imaging Industry?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Radiological Fracture Evaluation
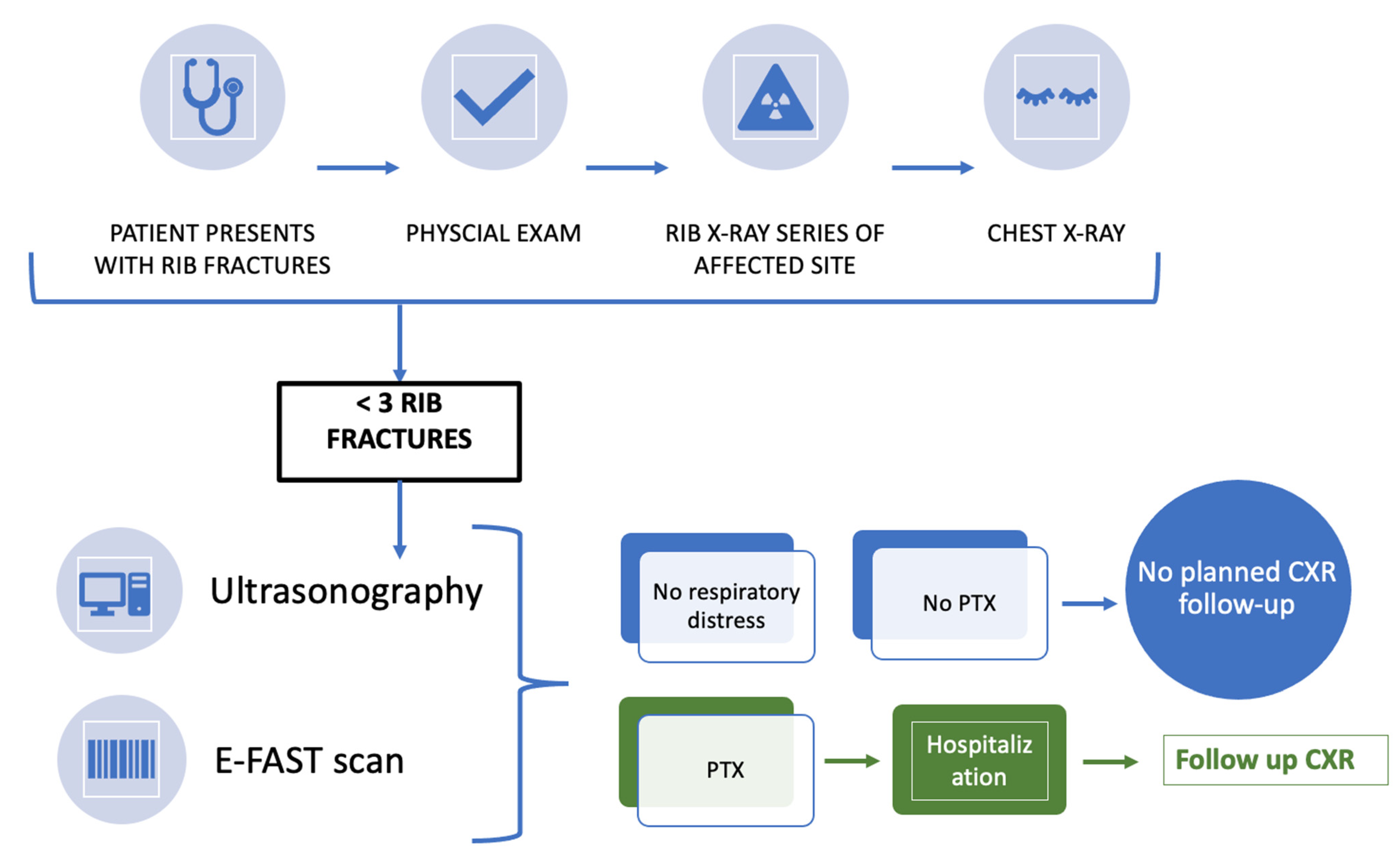
2.4. Treatment Protocol
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bulger, E.M.; Arneson, M.A.; Mock, C.N.; Jurkovich, G.J. Rib fractures in the elderly. J. Trauma 2000, 48, 1040–1047. [Google Scholar] [CrossRef] [PubMed]
- Graeber, G.M.; Nazim, M. The anatomy of the ribs and the sternum and their relationship to chest wall structure and function. Thorac. Surg. Clin. 2007, 17, 473–489. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.-S.; Huang, Y.-K.; Liu, Y.-H.; Liu, H.-P.; Kao, C.-L. Delayed pneumothorax complicating minor rib fracture after chest trauma. Am. J. Emerg. Med. 2008, 26, 551–554. [Google Scholar] [CrossRef] [PubMed]
- Sirmali, M.; Türüt, H.; Topcu, S.; Gülhan, E.; Yazici, Ü.; Kaya, S.; Taştepe, I. A comprehensive analysis of traumatic rib fractures: Morbidity, mortality and management. Eur. J. Cardio-Thorac. Surg. 2003, 24, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Westcott, J.; Davis, S.D.; Fleishon, H.; Gefter, W.B.; Henschke, C.I.; McLoud, T.C.; Pugatch, R.D.; Sostman, H.D.; Tocino, I.; White, C.S.; et al. Rib fractures. American College of Radiology. ACR Appropriateness Criteria. Radiology 2000, 215, 637–639. [Google Scholar] [PubMed]
- Misthos, P.; Kakaris, S.; Sepsas, E.; Athanassiadi, K.; Skottis, I. A prospective analysis of occult pneumothorax, delayed pneumothorax and delayed hemothorax after minor blunt chest trauma. EJCTS 2004, 25, 859–864. [Google Scholar]
- Liu, C.; Chen, Z.; Xu, J.; Wu, G. Diagnostic value and limitations of CT in detecting rib fractures and analysis of missed rib fractures: A study based on early CT and follow-up CT as the reference standard. Clin. Radiol. 2022, 77, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Henry, T.S.; Kirsch, J.; Kanne, J.P.; Chung, J.H.; Donnelly, E.; Ginsburg, M.E.; Heitkamp, D.; Kazerooni, E.A.; Ketai, L.H.; McComb, B.L.; et al. ACR Appropriateness Criteria® Rib Fractures. J. Thorac. Imaging 2014, 29, 364–366. [Google Scholar] [CrossRef] [PubMed]
- Chapman, B.C.; Overbey, D.M.; Tesfalidet, F.; Schramm, K.; Stovall, R.T.; French, A.; Johnson, J.L.; Burlew, C.C.; Barnett, C.; Moore, E.E.; et al. Clinical Utility of Chest Computed Tomography in Patients with Rib Fractures CT Chest and Rib Fractures. Arch. Trauma Res. 2016, 5, e37070. [Google Scholar] [CrossRef] [PubMed]
- Omar, H.R.; Abdelmalak, H.; Mangar, D.; Rashad, R.; Helal, E.; Camporesi, E.M. Occult pneumothorax, revisited. J. Trauma Manag. Outcomes 2010, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Söz, G.; Karakaya, Z. The evaluation of geriatric patients who presented with trauma to the emergency department. Arch. Med Sci. 2019, 15, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Reske-Nielsen, C.; Medzon, R. Geriatric Trauma. Emerg. Med. Clin. North Am. 2016, 34, 483–500. [Google Scholar] [CrossRef] [PubMed]
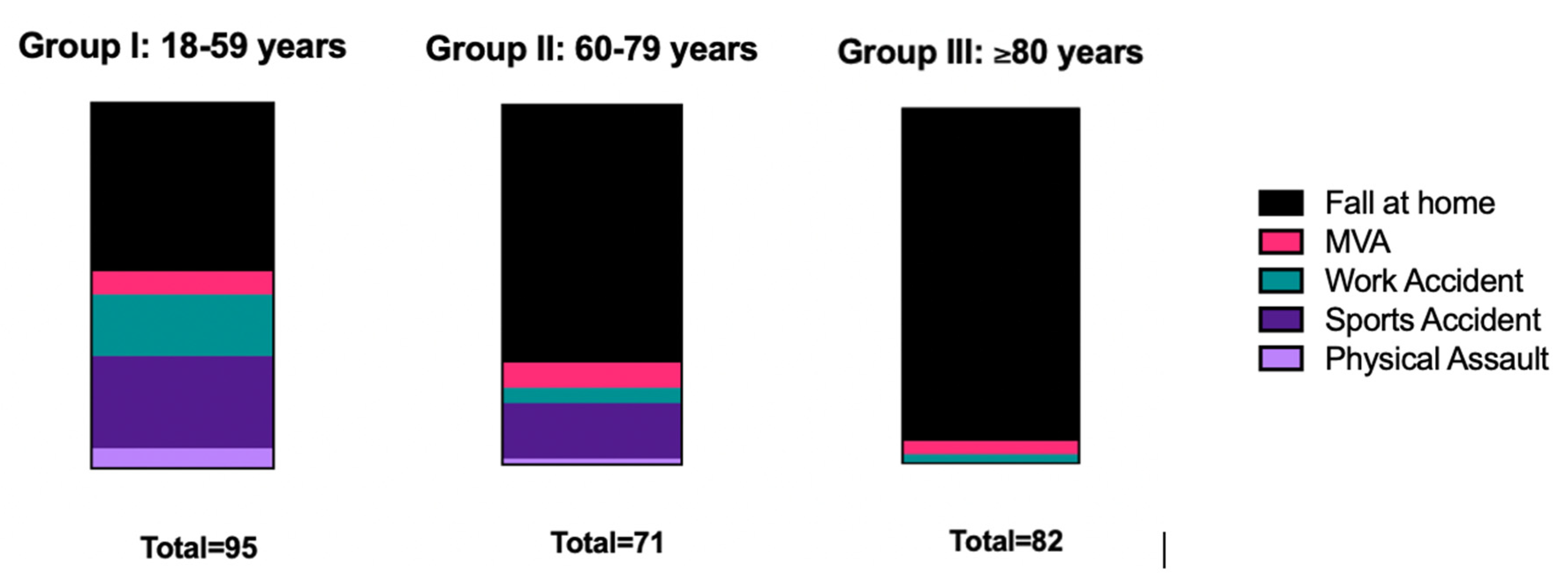
| MECHANISM OF INJURY | N (%) |
|---|---|
| MOTOR VEHICLE ACCIDENT | 30 (12.0) |
| ACCIDENTS AT WORK | 18 (7.2) |
| SPORTS ACCIDENTS | 19 (7.6) |
| PHYSICAL ALTERCATION | 6 (2.4) |
| FALL AT HOME | 176 (70.7) |
| AGE | |
| GROUP I: 18–59 YEARS | 95 (38.2) |
| GROUP II: 60–79 YEARS | 72 (28.9) |
| GROUP III:≥80 YEARS) | 82 (32.9) |
| NUMBER OF FRACTURED RIBS | |
| 1 | 150 (60.2) |
| 2 | 99 (39.8) |
| LATERALITY | |
| LEFT SIDE | 124 (49.8) |
| RIGHT SIDE | 121 (48.6) |
| BILATERAL | 4 (1.6) |
| LOCATION | |
| TRUE RIBS (I–VII) | 72 (28.9) |
| FALSE RIBS (VIII–XII) | 151 (60.6) |
| BOTH | 26 (10.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deluca, A.; Deininger, S.; Wichlas, F.; Hofmann, V.; Amelunxen, B.; Diepold, J.; Freude, T.; Deininger, C. Follow-Up Chest X-rays in Minor Chest Trauma with Fewer Than Three Rib Fractures: A Justifiable, Habitual Re-Imaging Industry? Healthcare 2022, 10, 2471. https://doi.org/10.3390/healthcare10122471
Deluca A, Deininger S, Wichlas F, Hofmann V, Amelunxen B, Diepold J, Freude T, Deininger C. Follow-Up Chest X-rays in Minor Chest Trauma with Fewer Than Three Rib Fractures: A Justifiable, Habitual Re-Imaging Industry? Healthcare. 2022; 10(12):2471. https://doi.org/10.3390/healthcare10122471
Chicago/Turabian StyleDeluca, Amelie, Susanne Deininger, Florian Wichlas, Valeska Hofmann, Berndt Amelunxen, Julian Diepold, Thomas Freude, and Christian Deininger. 2022. "Follow-Up Chest X-rays in Minor Chest Trauma with Fewer Than Three Rib Fractures: A Justifiable, Habitual Re-Imaging Industry?" Healthcare 10, no. 12: 2471. https://doi.org/10.3390/healthcare10122471
APA StyleDeluca, A., Deininger, S., Wichlas, F., Hofmann, V., Amelunxen, B., Diepold, J., Freude, T., & Deininger, C. (2022). Follow-Up Chest X-rays in Minor Chest Trauma with Fewer Than Three Rib Fractures: A Justifiable, Habitual Re-Imaging Industry? Healthcare, 10(12), 2471. https://doi.org/10.3390/healthcare10122471






